Abstract
Context:
Neuraxial techniques have sedative properties secondary to decreased inputs from sensory and motor afferents. We hypothesized that caudal analgesia decreases the requirement of desflurane as measured by bispectral index (BIS).
Aims:
This study aims to determine the minimum alveolar concentration (MAC) of desflurane for maintaining BIS below 50 (MACBIS50) in children undergoing infraumbilical surgeries with laryngeal mask airway (LMA) and study the effect of caudal analgesia on the same.
Settings and Design:
This is prospective and observational study.
Subjects and Methods:
Thirty-nine American Society of Anesthesiologists physical status Classes I and II children in between 1 and 8 years of age undergoing elective infraumbilical surgery under general anesthesia were allocated randomly into two groups (Group C and Group D) after induction with sevoflurane and LMA insertion. In Group C, caudal block was performed with 0.75 mL/kg of 0.25% bupivacaine and BIS values were recorded after 10 min for 1 min at 10 s intervals. In Group D, BIS was recorded for desflurane for 1 min at 10 s intervals followed by a caudal block with the same dose.
Statistical Analysis Used:
Dixon up-down method with a step size of 0.5%, and probit analysis were used for analysis.
Results:
A total of 39 patients were enrolled. MAC of desflurane for maintaining MACBIS50 was 5.57 (95% confidence interval [CI] 5.22–5.95) in Group D and 4.31 (95% CI 3.12–5.08) in Group C. The use of caudal anesthesia lowered the MAC of desflurane for maintaining MACBIS50 in children by 22.36% (P < 0.001).
Conclusions:
The use of caudal analgesia significantly reduced MAC of desflurane for maintaining MACBIS50 in children undergoing infraumbilical surgeries using LMA.
Keywords: Bispectral index 50, caudal analgesia, desflurane, minimum alveolar concentration, pediatric infraumbilical surgeries
INTRODUCTION
Bispectral index (BIS) is an electroencephalogram (EEG) derived parameter. Anesthetic agents are titrated to a specific BIS value during general anesthesia to allow adjustment of the amount of anesthetic agent required for adequate depth of anesthesia thus resulting in a more rapid emergence. Further, BIS monitoring reduces the incidence of intraoperative awareness under general anesthesia in adults.
Anesthetic agents have a comparable effect on EEG throughout the life.[1] Although conceived as an adult tool, use of BIS for titrating the effect of anesthesia in children has been supported in several studies.[2,3,4,5,6] Further, as in adults, BIS values in pediatric patients inversely correlate with end-tidal concentration of sevoflurane and isoflurane.[3,7] The minimum alveolar concentration (MAC) of sevoflurane for maintaining BIS below 50 (MACBIS50) has been determined to be 2.83% ± 0.16% in children.[4] The MAC of sevoflurane required to prevent purposeful movement in response to noxious stimuli in 50% of patients has been reported to be 2.4% in children.[8] Thus, the ratio of MACBIS50/MAC is 1.18 in pediatric patients. However, there have been no reports investigating these values for desflurane.
Regional techniques have been shown to decrease the requirement of anesthetic agents. There was 34% reduction in MACBIS50 of sevoflurane after administration of epidural lignocaine in adults.[9] No study has evaluated the effect of caudal anesthesia on MACBIS50 of inhalational agent in children.
We hypothesized that caudal block will decrease the MACBIS50 of desflurane. Primary outcome of the study was to determine MACBIS50 of desflurane and effect of caudal block on it. Success rate of laryngeal mask airway (LMA) removal, incidence of coughing and airway complications were the secondary outcomes studied.
SUBJECTS AND METHODS
Ethics approval for the study (Ethical Committee Number NK/1273/Res/259) was provided by Institute Ethics Committee on March 24, 2014. Parents of the children were explained in detail about the study and the parents willing to enroll their children for the study; the written informed consent was obtained from them.
Forty-five children of the American Society of Anaesthesiologists physical status classes I and II between the age group of 1–8 years scheduled for elective infraumbilical surgery under general anesthesia during the study (May 2014–December 2014) were assessed for eligibility. Patients with a history of respiratory or neurological disease were excluded from this study. Parents of three children refused to give the consent. Forty-two children were enrolled after written informed consent in this up-down sequential allocation trial.
No premedication was given. Monitoring consisted of a five-lead electrocardiogram, noninvasive measurement of blood pressure, pulse oximetry (SpO2), and BIS. All children were induced with 8% sevoflurane in oxygen. An intravenous access was secured after induction. BIS sensor probe Xp (Aspect systems, Norwood, USA) was placed on frontotemporal region as per manufacturer's instructions. BIS values were recorded using Datex Ohmeds S/5 monitor after assessing for adequate depth of anesthesia by checking jaw relaxation; an appropriate sized LMA was inserted. Controlled ventilation was then started using circle system with a tidal volume of 6–8 ml/kg at a rate to maintain end-tidal carbon dioxide (EtCO2) concentration between 35 and 45 mm Hg.
Patients were randomly allocated into two groups (Group C and Group D) using computer-generated random numbers. Children in Group C were placed in the left lateral position. Caudal block was performed with short beveled 23G needle using 0.75 mL/kg of 0.25% bupivacaine. Children were then turned supine, and desflurane was administered in 100% oxygen at a predetermined concentration. We waited for 10 min for the onset of caudal block. Thereafter, on attaining the same exhaled end-tidal desflurane concentration with the aim to achieve equilibrium between the alveolar and brain concentration, BIS was recorded at an interval of 10 s for 1 min.
Children in Group D after LMA insertion were administered desflurane in 100% oxygen. We waited until the exhaled end-tidal desflurane concentration attained the inspired desflurane concentration. BIS values were then recorded at an interval of 10 s for 1 min. Children in this group were then turned lateral and given caudal block for the purpose of intraoperative analgesia. Data recording for primary outcome was completed before the start of surgery.
Inspired and end-tidal desflurane concentration were measured using Datex Ohmeda M CAiOV gas analyzer software version 3.2 with automatic agent identifi cation using the Datex Ohmeda S/5 monitor (Datex-Ohmeda, GE Medical systems Pudong, Shanghai, China). Circle system was used, and end-tidal desflurane concentration was measured by placing a gas analyzer port between the LMA and the breathing circuit. Infrared analyzer was calibrated before the start of every case using Datex-Ohmeda airway module calibration gas stock number 755583.
The dial settings were adjusted to attain an end-tidal desflurane concentration of 5% in the first patient. This starting point taken corresponds to 0.75 MAC according to the previously reported MACBIS50 of sevoflurane.[4] If a given patient had an average BIS of <50, the desflurane concentration was reduced by 0.5% in the subsequent patient, whereas if a given patient had a BIS >50, the desflurane concentration was increased by 0.5% in the next patient.
For the purpose of blinding, data collection was done by an independent investigator who was called to the operation room (OR) after the patient had been anesthetized by the attending anesthesiologist. This investigator left the OR after data collection and was not involved in the subsequent management of the patient.
Anesthesia was then maintained with 4%–6% desflurane in oxygen and nitrous oxide (50:50). Total flow was kept at 2 L/min with a cumulative MAC of 1–1.3. Increase of >20% of preincision baseline heart rate or mean arterial pressure was defined as inadequate analgesia in both groups and treated with boluses of 0.5 μg/kg of fentanyl. After the surgery, the dial settings were set at 5%, and LMA removed once exhaled end-tidal desflurane concentration was also 5%. All the patients received 100% oxygen with face mask after LMA removal.
Statistical analysis
Demographic data were collected and presented as mean ± standard deviation. The Dixon's up-and-down method needs six pairs of failure-success for statistical analysis. We assessed and enrolled patients until we had the required number of pair for both groups and this formed the basis for sample size calculation.[10] MACBIS50 was calculated using the midpoint concentration of patients involving a crossover (i.e., BIS ≤ or > 50) according to the up-down method. Average of the crossover midpoints in each pair defined ED50. The up-and-down sequences were also analyzed by the probit test, which enabled us to derive the desflurane concentration for maintaining BIS of 50, with 95% confidence limits of the mean. Data were also analyzed by a logistic regression test to obtain the probability of BIS <50 versus end-tidal desflurane concentration, the maximum likelihood estimators of the model variables, and a goodness of fit. Calculated MACBIS50 of desflurane between the two groups were compared using Student's t-test. P < 0.05 was considered statistically significant. The analysis was performed using Microsoft Excel (2007) and Stat plus.
RESULTS
Parents of 42 patients consented to participate in the study. The study protocol could not be followed in three patients [Figure 1]. These three children were excluded before the inclusion of next patient. Table 1 shows the baseline patient characteristics of children in two groups. Figure 2 shows the sequences of individual patients in both groups using up-and-down method. The mean MACBIS50 values calculated with the Dixon's up-and-down method was significantly higher (P = 0.0007) in Group D (5.75% [0.288]) than Group C (4.5% [0.381]). Mean EtCO2 was comparable in both groups.
Figure 1.
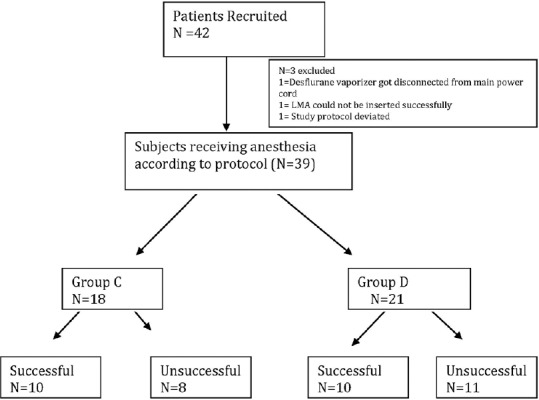
Subject cohort flow diagram
Table 1.
Demographic and intraoperative data of the patient
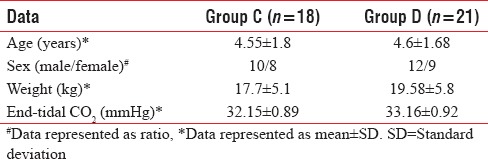
Figure 2.
Sequence of desflurane concentration for maintaining MACBIS50 in both groups. Hollow shape represents average bispectral index value >50, filled shape indicates average bispectral index value <50. X axis denotes number of patients and Y axis denotes concentration of desflurane
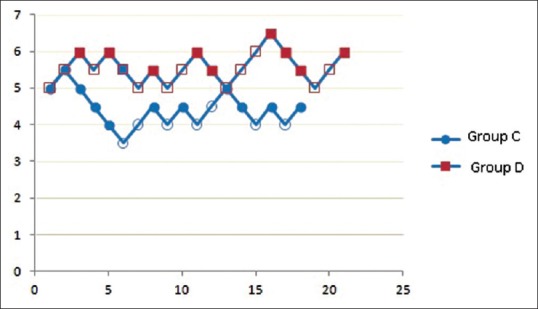
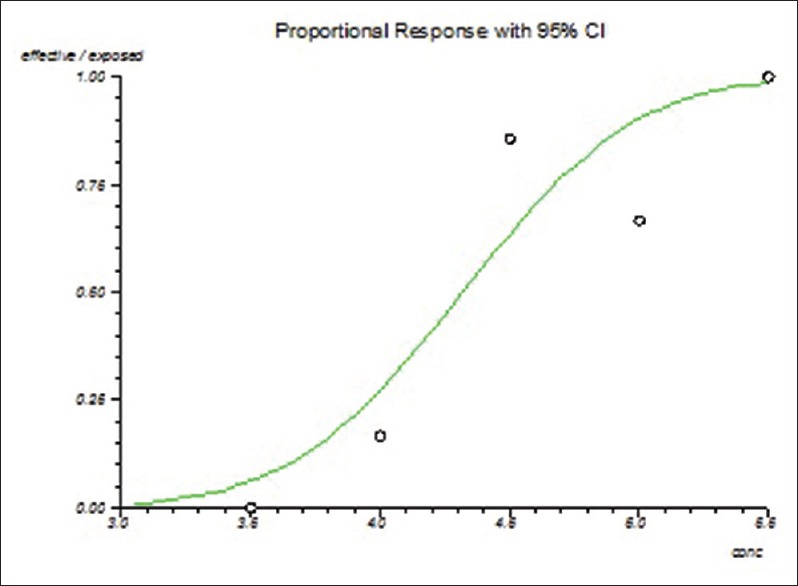
A logistic regression curve of the probability of attaining BIS50 is shown in Figures 3 and 4 and is illustrated by the dose-response curve constructed for both groups using probit test data The MACBIS50 values estimated by probit analysis were 5.57% (95% confidence interval [CI] 5.22–5.95) in Group D and 4.32% (95% CI 3.12–5.08) in Group C. Values were similar to those obtained with Dixon up-down method. Corresponding ED95 values, i.e., minimum concentration of desflurane required for maintaining BIS value <50 in 95% subjects was 6.158 (5.85–8.04) for Group D and 5.18 (4.7–6.6) for Group C.
Figure 3.
Dose response curve of desflurane for probability of maintaining bispectral index below 50 in Group C; 4.32% (95% confidence interval 3.12–5.08). X axis denotes end tidal desflurane concentration and Y axis denotes probability of bispectral index below 50
Figure 4.
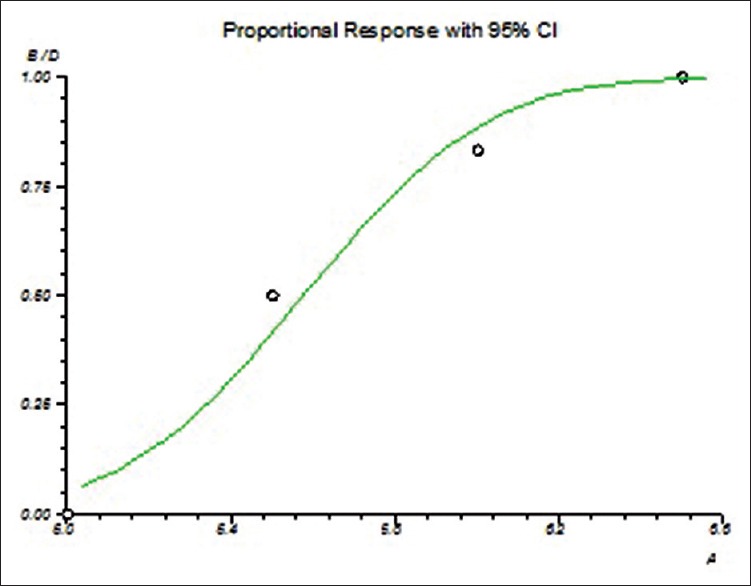
Dose response curve of desflurane for probability of maintaining bispectral index below 50 in Group D; 5.57% (95% confidence interval 5.22–5.95). X axis denotes end tidal desflurane concentration and Y axis denotes probability of bispectral index below 50
We observed movement in three patients and incomplete laryngospasm in two patients at the time of LMA removal. Laryngospasm responded to positive pressure ventilation. Desaturation (defined as SpO2< 90%) was not noticed in any of the children.
DISCUSSION
Anesthesia depth depends on a triad of good hypnosis, adequate analgesia, and abolition of reflex muscle activity. Balanced anesthesia aims to maintain adequate depth of anesthesia by preventing the awareness and its physiological effects. The depth of anesthesia monitor like BIS utilizes the EEG signals recorded from forehead which are amplified and processed through various algorithm and converted to a digital value.[11] A value of BIS index between 40 and 60 corresponds to optimal depth of anesthesia which has been validated. BIS index can have erroneous reading in number of situations like two different BIS monitors of the same make when applied on the same patient can cause 10% variation in reading, reduced adherence of electrode can cause false elevated value, and electromyography activity can superimpose on the frequency band of EEG leading to low-BIS value. Other factors include the drugs, pacemakers, peritoneal irrigation, and hypovolemia. Nevertheless, it remains an important monitoring tool for assessing the depth of anesthesia.[12]
No study till date has defined the MACBIS50 of desflurane in children. EEG bispectrum for both sevoflurane and desflurane were found to be similar to one another in terms of their respective positions in the structured model of the multiple correspondence analysis at MAC of 2, 1, and 0.5.[13] It is therefore expected that MACBIS50 for desflurane should be similar to that for sevoflurane. Tsuruta, et al. determined 2.83% (95% CI 2.70–3.14) as MACBIS50 of sevoflurane in children with a MACBIS50/MAC ratio of 1.19.[4] In our study, we found a MACBIS50/MAC of 0.69 for desflurane. The values are less than that reported for sevoflurane by Tsuruta et al. WWe can attribute lower value of MACBIS50/MAC ratio in our study to use of different airway device. Tsuruta et al. defined MACBIS50 in intubated children. The use of LMA to secure the airway is associated with less hemodynamic changes at the time of insertion and needs lesser depth anesthetics of anesthesia for maintenance of patient during the surgical procedure. ED50 of sevoflurane for both insertion and removal of LMA is less than that for endotracheal tube in any intubated patient. In a study by Aantaa et al., it was found that ED50 of sevoflurane for LMA insertion (1.57 [0.33] %) was significantly less than that for laryngoscopy and tracheal tube insertion (2.2 [0.31] %).[14] Similarly, ED50/MAC ratio for desflurane has also been studied both for removal of endotracheal tube and LMA. Cranfield and Bromley reported that ED50 for extubation with desflurane was 7.7% and ED50/MAC ratio 0.88.[15] Makkar et al. found that the ED50/MAC ratio of desflurane for LMA removal was 0.41.[16] The results of these studies show that ED50/MAC values for both insertion and removal of LMA with either sevoflurane or desflurane are 30%–40% less than that for endotracheal tube. Hence, the ratio of MACBIS50/MAC may also differ depending on the device used to secure airway.
Caudal analgesia causes the peripheral input deafferentation and the local anesthetic by its effect on the central nervous system due to its rostral spread and its systemic absorption, presumed to affect the arousal due to the intrinsic sedative activity. Davidson et al. and Banerjee et al. in their studies on pediatric population concluded that caudal analgesia decreases the arousal as determined by the BIS index monitoring during general anesthesia.[17,18] Hodgson and Liu found 34% reduction in the end-tidal sevoflurane concentration required for maintaining BIS <50 in lidocaine epidural anesthesia compared with general anesthesia alone group in adult patients.[9] Authors concluded that epidural anesthesia markedly reduced the amount of volatile general anesthetic required for adequate depth of anesthesia. Kim et al. have demonstrated that caudal analgesia reduces the sevoflurane concentration required for the LMA removal.[19]
We also observed that use of caudal analgesia was associated with significant reduction in MACBIS50 of desflurane in children. The use of caudal analgesia significantly decreased MACBIS50 values to 4.32% (95% CI 3.12–5.08) as compared to MACBIS50 of desflurane with LMA (5.57% [95% CI 5.22–5.95]).
In a single study conducted in children to see the effect of combined anesthesia (local plus general) or balanced anesthesia (intravenous analgesia plus inhalational anesthetics) to see maintenance requirement of sevoflurane using BIS, authors found a significant decrease in sevoflurane requirements to maintain BIS <50 in combined anesthesia group.[20]
Several factors such as the use of propofol, N2O, opioids, and success of caudal block can influence the BIS values. We have used operator's clinical impression of successful needle placement based on four predictors, i.e., ability to locate sacral hiatus, “pop off” on piercing the ligament, lack of resistance to injection and lack of subcutaneous swelling.[21] If three or all four predictors were positive, clinical impression was recorded as successful. Operator's impression of unsuccessful block was the reason for exclusion of one of the three patients excluded from the study. Further, no child required intraoperative rescue analgesia indicating effective caudal block in enrolled children. None of the children received propofol or N2O. Therefore, we believe that we followed a protocol that did not involve any other factor that might have affected BIS.
All the LMAs were removed in a deep plane in our study. Lerman et al. showed that incidence of airway events with LMA removal at a MAC of 1.3 (≈9%) using desflurane anesthesia was 15%.[22] Authors attributed this to inadequate depth of desflurane anesthesia at the time of removal of the LMA. However, data indicates that for each anesthetic there is a threshold below which no airway irritation develops. TerRiet et al. observed that 75% of adult patients found desflurane irritating at a MAC of 2.[23] On the other hand, volunteers given desflurane up to 1 MAC did not report any coughing, breath holding, or laryngospasm.[24] Hence, higher incidence of airway events after desflurane in the study conducted by Lerman et al. might have been due to exposure to higher concentration of the desflurane. In another study, Makkar et al. found ED95 of desflurane for LMA removal to be 4.13%.[25] Hence, we chose to remove LMA at end-tidal desflurane concentration of 5% and found the incidence of airway events to be <1%.
Limitations of our study are that we enrolled children over a wide range of age. As MAC is significantly influenced by age, slightly different values might be expected on stratification of children in 2–4 and 4–8 years of age group.[2] Further studies with narrower age groups may be undertaken using desflurane. Second, ED95, which is more important clinically, was calculated by extrapolation from ED50 and so maybe it is less precise. Third, younger children have larger spread when the same weight base-dosage of local anesthetics is administered for caudal block. Effect of caudal block on BIS can be different between children even though dose of bupivacaine is same. Finally, we could have used a more valid method like ultrasound to confirm the success of caudal block.
CONCLUSIONS
MACBIS50 of desflurane with LMA is 5.57% (95% CI 5.22–5.95) in children. Use of caudal analgesia significantly decreases MACBIS50 values to 4.32% (95% CI 3.12–5.08).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Murat I, Constant I. BIS in pediatrics: Fashion or new tool? Paediatr Anaesth. 2005;15:177–80. doi: 10.1111/j.1460-9592.2004.01564.x. [DOI] [PubMed] [Google Scholar]
- 2.Tokuwaka J, Satsumae T, Mizutani T, Yamada K, Inomata S, Tanaka M, et al. The relationship between age and minimum alveolar concentration of sevoflurane for maintaining bispectral index below 50 in children. Anaesthesia. 2015;70:318–22. doi: 10.1111/anae.12890. [DOI] [PubMed] [Google Scholar]
- 3.Degoute CS, Macabeo C, Dubreuil C, Duclaux R, Banssillon V. EEG bispectral index and hypnotic component of anaesthesia induced by sevoflurane: Comparison between children and adults. Br J Anaesth. 2001;86:209–12. doi: 10.1093/bja/86.2.209. [DOI] [PubMed] [Google Scholar]
- 4.Tsuruta S, Satsumae T, Mizutani T, Inomata S, Shimizu T, Takahashi S, et al. Minimum alveolar concentrations of sevoflurane for maintaining bispectral index below 50 in children. Paediatr Anaesth. 2011;21:1124 7. doi: 10.1111/j.1460-9592.2011.03602.x. [DOI] [PubMed] [Google Scholar]
- 5.Kim HS, Oh AY, Kim CS, Kim SD, Seo KS, Kim JH, et al. Correlation of bispectral index with end-tidal sevoflurane concentration and age in infants and children. Br J Anaesth. 2005;95:362–6. doi: 10.1093/bja/aei196. [DOI] [PubMed] [Google Scholar]
- 6.Davidson AJ, Huang GH, Rebmann CS, Ellery C. Performance of entropy and bispectral index as measures of anaesthesia effect in children of different ages. Br J Anaesth. 2005;95:674–9. doi: 10.1093/bja/aei247. [DOI] [PubMed] [Google Scholar]
- 7.Whyte SD, Booker PD. Bispectral index during isoflurane anesthesia in pediatric patients. Anesth Analg. 2004;98:1644–9. doi: 10.1213/01.ANE.0000117223.84646.36. [DOI] [PubMed] [Google Scholar]
- 8.Lerman J, Sikich N, Kleinman S, Yentis S. The pharmacology of sevoflurane in infants and children. Anesthesiology. 1994;80:814–24. doi: 10.1097/00000542-199404000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Hodgson PS, Liu SS. Epidural lidocaine decreases sevoflurane requirement for adequate depth of anesthesia as measured by the bispectral index monitor. Anesthesiology. 2001;94:799–803. doi: 10.1097/00000542-200105000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Dixon WJ, Massey FJ. Introduction to Statistical Analysis. 4th ed. New York: McGraw-Hill; 1983. pp. 426–41. [Google Scholar]
- 11.Rani DD, Harsoor S. Depth of general anaesthesia monitors. Indian J Anaesth. 2012;56:437–41. doi: 10.4103/0019-5049.103956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duarte LT, Saraiva RA. When the bispectral index (BIS) can give false results. Rev Bras Anestesiol. 2009;59:99–109. doi: 10.1590/s0034-70942009000100013. [DOI] [PubMed] [Google Scholar]
- 13.Tirel O, Wodey E, Harris R, Bansard JY, Ecoffey C, Senhadji L, et al. The impact of age on bispectral index values and EEG bispectrum during anaesthesia with desflurane and halothane in children. Br J Anaesth. 2006;96:480–5. doi: 10.1093/bja/ael034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aantaa R, Takala R, Muittari P. Sevoflurane EC50 and EC95 values for laryngeal mask insertion and tracheal intubation in children. Br J Anaesth. 2001;86:213–6. doi: 10.1093/bja/86.2.213. [DOI] [PubMed] [Google Scholar]
- 15.Cranfield KA, Bromley LM. Minimum alveolar concentration of desflurane for tracheal extubation in deeply anaesthetized, unpremedicated children. Br J Anaesth. 1997;78:370–1. doi: 10.1093/bja/78.4.370. [DOI] [PubMed] [Google Scholar]
- 16.Makkar JK, Ghai B, Bhardwaj N, Wig J. Minimum alveolar concentration of desflurane with fentanyl for laryngeal mask airway removal in anesthetized children. Paediatr Anaesth. 2012;22:335–40. doi: 10.1111/j.1460-9592.2011.03712.x. [DOI] [PubMed] [Google Scholar]
- 17.Davidson AJ, Ironfield CM, Skinner AV, Frawley GP. The effects of caudal local anesthesia blockade on the bispectral index during general anesthesia in children. Paediatr Anaesth. 2006;16:828–33. doi: 10.1111/j.1460-9592.2006.01868.x. [DOI] [PubMed] [Google Scholar]
- 18.Banerjee A, Das B, Mukherjee D, Khanra M. A study of the effect of caudal epidural block on bispectral index targeted propofol requirement in children: A comparative study. J Indian Assoc Pediatr Surg. 2015;20:77–81. doi: 10.4103/0971-9261.151551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim JS, Park WK, Lee MH, Hwang KH, Kim HS, Lee JR, et al. Caudal analgesia reduces the sevoflurane requirement for LMA removal in anesthetized children. Korean J Anesthesiol. 2010;58:527–31. doi: 10.4097/kjae.2010.58.6.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reinoso-Barbero F, Martínez-García E, Hernández-Gancedo MC, Simon AM. The effect of epidural bupivacaine on maintenance requirements of sevoflurane evaluated by bispectral index in children. Eur J Anaesthesiol. 2006;23:460–4. doi: 10.1017/S0265021506000330. [DOI] [PubMed] [Google Scholar]
- 21.Orme RM, Berg SJ. The ‘swoosh’ test – An evaluation of a modified ‘whoosh' test in children. Br J Anaesth. 2003;90:62–5. [PubMed] [Google Scholar]
- 22.Lerman J, Hammer GB, Verghese S, Ehlers M, Khalil SN, Betts E, et al. Airway responses to desflurane during maintenance of anesthesia and recovery in children with laryngeal mask airways. Paediatr Anaesth. 2010;20:495–505. doi: 10.1111/j.1460-9592.2010.03305.x. [DOI] [PubMed] [Google Scholar]
- 23.TerRiet MF, DeSouza GJ, Jacobs JS, Young D, Lewis MC, Herrington C, et al. Which is most pungent: Isoflurane, sevoflurane or desflurane? Br J Anaesth. 2000;85:305–7. doi: 10.1093/bja/85.2.305. [DOI] [PubMed] [Google Scholar]
- 24.Jones RM, Cashman JN, Mant TG. Clinical impressions and cardiorespiratory effects of a new fluorinated inhalation anaesthetic, desflurane (I-653), in volunteers. Br J Anaesth. 1990;64:11–5. doi: 10.1093/bja/64.1.11. [DOI] [PubMed] [Google Scholar]
- 25.Makkar JK, Ghai B, Wig J. Minimum alveolar concentration of desflurane with caudal analgesia for laryngeal mask airway removal in anesthetized children. Paediatr Anaesth. 2013;23:1010–4. doi: 10.1111/pan.12226. [DOI] [PubMed] [Google Scholar]


