Abstract
Background:
Peri-operative incentive spirometry (IS) helps in improving pulmonary function, facilitates sputum clearance and prevents unwanted postoperative pulmonary complications after major abdominal and thoracic surgery. In our hospital, all patients are instructed to practice IS before abdominal and thoracic surgeries so that they can perform it in the postoperative period effectively. However, many patients do not follow our advice. A few unfortunate patients land up with pulmonary complications as it becomes difficult to train them after surgery.
Aims:
To determine the compliance rate of patients who were instructed to perform incentive spirometry preoperatively.
Study design and settings:
Observational, single arm study in a single speciality centre.
Materials and Methods:
After approval from hospital ethics committee the study was registered with Clinical Trials Registry of India (CTRI). 100 patients posted for major abdominal or thoracic cancer surgery were enrolled in the study. They were instructed to perform incentive spirometry(IS) in front of relatives, an information leaflet was provided to them and the spirometry effort was noted in ‘ml’. The effort was crossed checked on the day of surgery. Patients performing IS correctly with effort more or equal to that noted earlier were labelled as compliant. Others were labelled as non-compliant. The reason of non-compliance was to be determined using a questionnaire meant for patient and the accompanying family member.
Results:
Out of 100, 26 patients were found to be non-compliant out of which 10 were males and 16 were female patients. 15 patients did not understand the instructions properly, 8 patients did not get enough time to practice, family members of 10 patients could not help the patient in performing and understanding IS, family members of 8 patients did not have adequate time for the patient.
Conclusion:
A non-compliance rate of 26% could be because patients and family members did not understand the seriousness of preoperative IS in spite of explaining and giving an information leaflet. The surgeries planned were major ones which require arrangement of finances, abstinence from work and other social issues like not having anybody at home with other family members, location of hospital far from the place they live. Involving respiratory therapist and nursing staff early during pre-anaesthesia check up could help in better understanding of the patient and family regarding benefits of IS.
Keywords: Incentive spirometry, infection, patient education, postoperative pulmonary complications, surgery
INTRODUCTION
Incentive spirometer is a hand-held device that helps patients in achieving effective inspirations. Preoperative incentive spirometry (IS) is useful for patients posted for major abdominal and thoracic surgeries as it helps in improving lung function, facilitates sputum clearance, and also helps in educating the patient how to perform IS correctly and effectively. This education helps the patient in performing IS during postoperatively for better rehabilitation. The incidence of postoperative pulmonary complications (POPCs) is in the range of 2%–39%.[1,2] Basal atelectasis, pneumonia, and hypoxic respiratory failure are the commonly encountered POPCs. IS, deep-breathing exercises, directed coughing, early mobilization, and multimodal analgesia can help in preventing or reducing the severity of POPCs. IS is similar to a sigh or yawning which decreases pleural pressure and facilitates better lung expansion and mucociliary clearance, thereby promoting better gas exchange. If IS is performed using the correct technique, it can reduce the possibility of POPCs. This was highlighted by the study published by Westwood et al.[3] Several studies highlighted the importance of preoperative IS and deep-breathing exercises in preserving postoperative lung function leading to lesser POPCs.[4,5] There are no studies in the literature where the compliance of surgical patients who were trained to perform IS was assessed. The aim of our study was to find the compliance rate and the reason for noncompliance in patients who did not perform IS as instructed on the day of surgery.
MATERIALS AND METHODS
We conducted an observational, follow-up, prospective, single-arm study in our institute by recruiting 100 patients of both sexes who were posted for major abdominal and thoracic cancer surgeries over a period of 4 months (from March 2017 to June 2017).
Patients coming for emergency and urgent surgeries were not recruited. Patients with preexisting tracheostomy, on home continuous positive airway pressure machine, having intercostal drains in situ, who are mentally incompetent, who are not able to communicate in either of three languages (Telugu, Hindi, and English), and who are not willing to give consent were excluded from the study. Patients were instructed how to perform IS properly (holding the mouthpiece, achieving a slow rise, holding the small ball in the center, and raising the larger one as high as possible). A verbal confirmation that the patient had understood the IS technique was taken. Once satisfied with the technique, the preoperative IS effort in “ml” was noted in the preanesthesia checkup (PAC) form and labeled “baseline” effort. An information leaflet was provided to the patient in the language they understand and were asked to refer if required. We also confirmed that the patient or his/her family member could read the information leaflet. The IS effort on the day of surgery was also noted and labeled “optimal” effort. The baseline and optimal effort (at PAC and on the day of surgery) along with other data such as age, gender, weight, body mass index (BMI), and abdominal/thoracic surgery were entered in a Microsoft Excel sheet. We compared demographic data of all included patients (age, weight, gender, and BMI) and expressed it as mean ± standard deviation. The value of P < 0.05 was considered to be statistically significant. Statistical analysis was performed using Microsoft Excel 2011 (Microsoft Corporation, Redmond, WA, USA).
Patients were declared compliant if the optimal IS effort was same or better than baseline along with a correct technique. The patients who were not performing correctly, not holding mouthpiece correctly, hyperventilating while performing IS, or exhaling instead of inhaling were declared as noncompliant (NC). The NC patient and the family members were asked five questions with responses YES or NO as the answers to know the cause of NC [Table 1]. These data were also used for analysis.
Table 1.
Questions which would be asked to the non-compliant patients and the family members
Ethical consideration, trial registration, and protocol publication
Hospital Ethics Committee approval was taken to conduct this observational study (EC Reference No. IEC/2017/28, dated February 23, 2017). We registered our study with the Clinical Trials Registry of India (CTRI). The registration number is CTRI/2017/03/008122, registered on March 16, 2017. We prepared our protocol using the Standard Protocol Items for Randomized Trials recommendations (http://www.spiritstatement.org/).[6] The study protocol is published with the Digital Object Identifier: 10.20900/mo. 20170013.[7]
RESULTS
We recruited 100 patients over a span of 4 months. The mean age was 54.03 years (range: 25–75 years). Total male (M) and female (F) patients who were studied were 39 and 61, respectively. Average weight of the patients was 62.3 kg (F = 63.75 kg, M = 59.85 kg, P value = 0.1598, confidence interval of 95%), average age was 54.03 years (F = 53.39, M = 55.03, P = 0.5456, confidence interval of 95%), and average BMI was 25.45 kg/m2 (F = 27.25, M = 22.65, P = 0.0002, confidence interval of 95%) [Figure 1]. Ninety-one patients were posted for abdominal surgeries and nine patients were posted for thoracic surgeries. Noncompliance was seen in 26 patients, of whom 10 were male and 16 were female patients, which means that a total of 26 patients out of 100 recruited did not perform IS as instructed. Twenty-two patients in the abdominal surgery group and four patients in the thoracic surgery group were NC.
Figure 1.
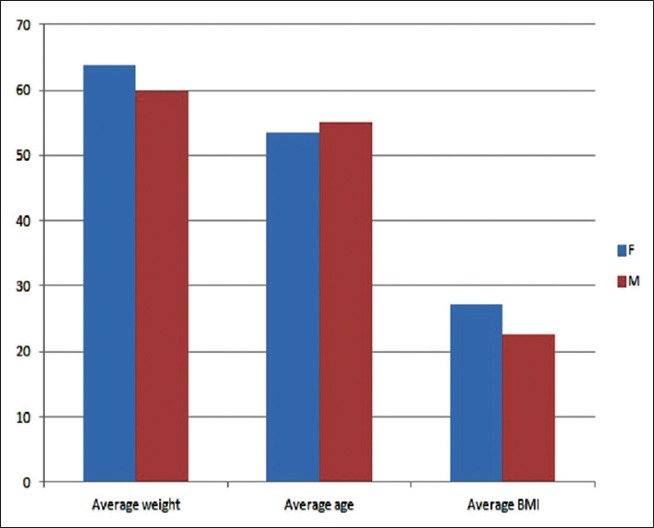
Comparison of age, weight, and body mass index between female and male patients who were recruited in the study
On analyzing the responses to the questionnaire, we found that 15 patients did not understand the instructions even after giving a leaflet with printed instructions in the language they understood (M = 5, F = 10). Eight patients (M = 4, F = 4) mentioned that they did not get enough time to practice. Ten patients (M = 3, F = 7) said that the family members did not or could not help them preoperatively in practicing IS. Family members of 12 (M = 3, F = 9) patients did not or could not help the patient in understanding and performing IS. Family members of seven patients (M = 2, F = 5) did not have adequate time for attending the patient. Figure 2 represents a bar diagram showing comparison between female and male patients who were asked five questions to know the cause of NC.
Figure 2.
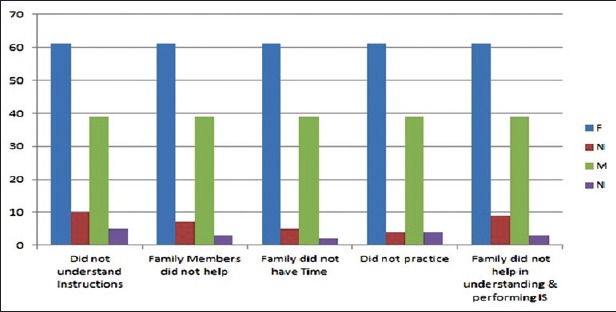
The comparison between male and female noncompliant patients who along with the family members were questioned to know the cause of noncompliance. Five questions were asked to these patients which had responses as YES or NO
DISCUSSION
The purpose of starting preoperative IS is to train the patients in performing correctly, to promote mucociliary clearance of sputum, and to improve pulmonary function. The patients who were included in the study were cancer patients of varying stage and grade. The diagnosis of cancer per se is alarming for patients and family members. They want to get the proposed surgery done as early as possible so as to prevent spread of malignancy which is a common notion among cancer patients.
Despite confirming verbally during PAC that the patient and family members had understood the instructions, a noncompliance rate of 26% suggests that either they did not read and followed the instructions properly or they did not understand the importance of IS which was explained to them in detail. The reason for less involvement of family members during the preoperative period could be because of issues such as arranging finances, completing formalities for medical insurance, work pressure, difficulty in availing leave from workplace, and other psychosocial issues.
The reason for more NC in female patients could be because of more family responsibilities and household work compared to their male counterpart. The limitations of our study were that we did not follow the patients who were NC to see whether they developed serious POPCs after surgery as compared to those who were compliant. The average length of stay in hospital was also not followed up. We did not compare the socioeconomic and educational status of the patients. Few patients who were included in the study were illiterate, but the accompanying family was literate and could read the instructions leaflet. Therefore, we assumed that they would help the patient by reading out the instructions in case there is a problem. Future studies which compare postoperative outcomes in NC patients to compliant patients can establish evidence, suggesting the importance of optimal IS before elective major abdominal and thoracic surgery.
CONCLUSION
Inability to understand the instructions, inadequate time to practice, and inadequate support from patient's family members were the reasons depicted for NC. The socioeconomic status or inability to understand the seriousness of POPCs could be the reason for NC with preoperative IS. Patients who have poor effort in baseline IS could be called more frequently to PAC clinic to monitor if they are performing IS appropriately. Such patients could be sent to a respiratory therapist for a detailed session on explaining the technique of IS. The family members should be counseled in detail and advised to get involved in preoperative optimization of the patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Mr. Gopal, our respiratory therapist, and Mrs. Hazra, our assistant at the preanesthesia clinic, for explaining and training all the patients with IS. Mr. Chaitanya, secretary, at PAC clinic helped in organizing and analyzing the Microsoft Excel sheet.
REFERENCES
- 1.Fisher BW, Majumdar SR, McAlister FA. Predicting pulmonary complications after nonthoracic surgery: A systematic review of blinded studies. Am J Med. 2002;112:219–25. doi: 10.1016/s0002-9343(01)01082-8. [DOI] [PubMed] [Google Scholar]
- 2.Gatti G, Cardu G, Lusa AM, Pugliese P. Predictors of postoperative complications in high-risk octogenarians undergoing cardiac operations. Ann Thorac Surg. 2002;74:671–7. doi: 10.1016/s0003-4975(02)03741-4. [DOI] [PubMed] [Google Scholar]
- 3.Westwood K, Griffin M, Roberts K, Williams M, Yoong K, Digger T, et al. Incentive spirometry decreases respiratory complications following major abdominal surgery. Surgeon. 2007;5:339–42. doi: 10.1016/s1479-666x(07)80086-2. [DOI] [PubMed] [Google Scholar]
- 4.Kundra P, Vitheeswaran M, Nagappa M, Sistla S. Effect of preoperative and postoperative incentive spirometry on lung functions after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:170–2. doi: 10.1097/SLE.0b013e3181db81ce. [DOI] [PubMed] [Google Scholar]
- 5.Kulkarni SR, Fletcher E, McConnell AK, Poskitt KR, Whyman MR. Pre-operative inspiratory muscle training preserves postoperative inspiratory muscle strength following major abdominal surgery – A randomised pilot study. Ann R Coll Surg Engl. 2010;92:700–7. doi: 10.1308/003588410X12771863936648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nair AS, Seelam S, Bharuka A, Nayak PP, Saifuddin MS, Rayani BK. Protocol of an observational, follow up, single arm study for knowing the compliance of patients scheduled for major abdominal and thoracic surgeries who were instructed to perform spirometry in a single specialty centre. Med One. 2017;2:e170013. [Google Scholar]


