Abstract
Background:
Several video laryngoscopes had demonstrated their superiority over conventional oral and nasal intubation techniques. King Vision video laryngoscope has fewer studies supporting its suitability for oral intubations. However, its suitability as a nasal intubating device has not been yet evaluated. We evaluated the suitability of King Vision video laryngoscope for nasotracheal intubation comparing with TruviewPCD.
Methods:
Eighty American Society of Anesthesiologists Grade I and II elective surgical patients were studied. After meeting the inclusion criteria, 80 study subjects were randomized into two groups. Group T were intubated using TruviewPCD and Group K were intubated with the nonchanneled King Vision video laryngoscope. Our primary outcome was single successful nasotracheal intubation without use of any additional maneuvers. The time taken for intubation, use of additional maneuverers, Cormack-Lehane grading, and hemodynamics were also analyzed.
Results:
Seventy-one patients (88.75%) were successfully intubated in a single attempt, i.e. 35 patients (90%) in Group K and 36 patients (87.5%) in Group T. Intubation time (mean ± standard deviation) was 67.9 ± 24.1 s in Group T and 64.9 ± 20.0 s in Group K where comparison was not statistically significant (P = 0.5). The additional maneuvers (P = 0.2) and hemodynamic changes were not clinically significant. There were no associated serious complications.
Conclusion:
King Vision video laryngoscope is just as effective as TruviewPCD video laryngoscope for successful nasotracheal intubation.
Keywords: King Vision video laryngoscope, nasotracheal intubation, TruviewPCD
INTRODUCTION
Conventionally nasotracheal intubation is usually done by Macintosh-assisted Magill forceps. It is usually associated with trauma, hemodynamic stress response while negotiating the tube into trachea. There is a need for video laryngoscope device that reduces trauma during nasotracheal intubation. Use of video laryngoscopes is becoming popular nowadays for both oral and nasotracheal intubation.[1,2] Studies on video laryngoscopes such as C-MAC have reported requiring less force on the maxillary incisors to negotiate into trachea and provide a better visualization of the glottis.[3] This may also explain how recent studies performed by Raveendra et al.[4] and Patil Archita et al.[5] required less manipulation during nasal intubation with Truview. Various studies comparing individual video laryngoscopes for nasotracheal intubation have been studied using Truview, C-MAC, GlideScope, and McGrath video laryngoscope.[6] TruviewPCD video laryngoscope is a device with a narrow-angulated blade and connecting camera and stylet for using nasotracheal intubation. King Vision is a lightweight ergonomically designed device with a camera at the distal tip of the blade along with a light source to provide minimal lifting of soft tissue and impact on the dentition. To the best of our knowledge, no studies are available supporting King Vision video laryngoscope and TruviewPCD video laryngoscope for success of nasotracheal intubation. Hence, with research supporting the superiority of Truview video laryngoscope over conventional direct laryngoscopy techniques, we designed the study to compare King Vision and TruviewPCD video laryngoscopes for ease of nasotracheal intubation.
METHODS
After approval from our Institutional Ethics Committee and written informed consent taken, 80 American Society of Anesthesiologists (ASA) physical status I and II adult patients were randomly divided into two groups of 40 each through a sequential sampling method. They were randomized into two groups by sealed envelope technique. In Group K, intubation was performed using King Vision video laryngoscope, and in Group T, intubation was performed using TruviewPCD video laryngoscope. All patients received a standardized anesthetic protocol. Patients were advised a fasting period of at least 8 h. They were premedicated with tablet diazepam 10 mg and tablet ranitidine 150 mg orally the night before surgery and the morning of surgery. ASA physical status III and IV, Le-fort Type 2 and Type 3 fracture, anticipated difficult airway, patients with basilar skull fracture and cerebrospinal fluid rhinorrhea were excluded from the study. In the preoperative holding area, an 18-gauge intravenous cannula was secured and injection glycopyrrolate 0.2 mg and injection midazolam 0.03 mg/kg were administered intravenously. Nasal cavity preparation was done 20 min before intubation by decongestant drops. In the operating theater, standard monitoring such as pulse oximetry, electrocardiogram, and noninvasive blood pressure monitoring were used, and baseline values were recorded before intubation and at 1 min intervals for next 5 min after intubation. All patients were preoxygenated with 100% oxygen for 3 min; anesthesia was induced with 0.1 mg/kg morphine and 2 mg/kg propofol. After the confirmation of bag and mask ventilation, injection vecuronium 0.08 mg/kg was administered intravenously and ventilation continued with oxygen and isoflurane at 1.5%. At the end of 3 min, a well-lubricated PVC tube of appropriate size was negotiated through a selected nostril until it advanced into the nasopharynx. Once the tube was successfully advanced into the nasopharynx, respective video laryngoscope was performed.
Laryngoscopy for patients in both groups was performed by inserting the respective video laryngoscope blades in the midline of the oral cavity. The Cormack and Lehane (CL) scoring of laryngeal view as seen on the monitor was noted. After visualizing the larynx, the nasotracheal tube was advanced into the trachea. Primary outcome was the rate of success of nasotracheal intubation with or without any added maneuvers. Secondary outcome was the time taken for intubation, nasotracheal intubation aided with head and neck manipulation, BURP or use of the Magill forceps, CL grading, hemodynamic changes, and complications such as trauma, bleeding, and sore throat.
A successful intubation was defined as a single passage of the device into the glottis with or without assistance of additional maneuvers such as head and neck manipulation/BURP or with the use of Magill forceps. Time for intubation was defined as the time from after introduction of the endotracheal tube through the nostril into nasopharynx until the appearance of capnograph trace. A failed intubation was defined as one where the patient was not intubated in the first attempt within 90 s or when oxygen saturation fell below 95%, whichever occurred first. Inability to successfully intubate the patient in the first attempt was addressed by oxygenating the patient for 3 min followed by intubation using conventional Macintosh laryngoscope assisted with Magill forceps. Systolic blood pressure, diastolic blood pressure, mean arterial pressure (MAP), oxygen saturation, and heart rate (HR) were recorded at the baseline, 3 min after induction (before intubation), and five successive recordings at 1-min interval after intubation.
Statistical analysis
The sample size was calculated based on previous study by Raveendra et al.[4] using the formula n = 4pq/L2. With a power of 80% and alpha of 0.01, we calculated a sample size of 40 in each group. Data were entered into Microsoft Excel 2013 and analyzed by SPSS v 21 (IBM Corporation, Armonk, New York, USA).
Descriptive analysis was reported as mean and standard deviation and median and range of continuous variables, and P < 0.05 was considered statistically significant. The demographics were analyzed by Student's t-test. ASA, use of additional maneuvers, and success of intubation were analyzed by Chi-square test. The time taken for intubation (not normally distributed data) and glottis visualization using CL grading score were analyzed by Mann–Whitney U-test.
RESULTS
Demographic data such as age, sex, ASA status, body mass index, and Mallampati class between two groups were statistically comparable. Success rate was comparable between the two groups with 87.5% in Group T and 90% in Group K (P = 0.7) [Figure 1]. Thirty-five patients were successfully intubated within 90 s in Group T and 36 patients were successfully intubated in Group K within 90 s. The median intubation time was 66 s in Group T and 61 s in Group K (P = 0.5). Assisted maneuvers between the two groups were comparable (P = 0.4) [Figure 2]. CL grade (CLG) was comparable between two groups with P = 0.3 [Figure 3]. Rise in HR from baseline values was noted in all patients of both groups. However, there was no statistically significant difference between the two groups [Figure 4]. A rise in MAP from baseline values after intubation was noted in all patients of both groups [Figure 5]. Patients belonging to Group K demonstrated a higher MAP value in the 2 and 3 min postintubation; however, the difference between the two groups was not statistically significant in relation to HR changes and MAP.
Figure 1.

Comparison of success rate between the two groups
Figure 2.
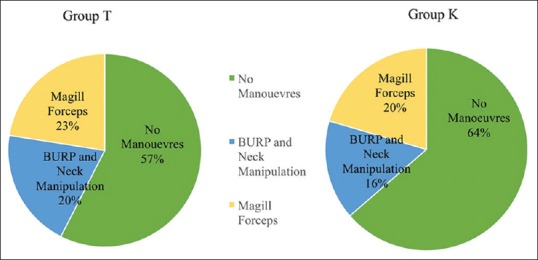
Comparison of assisted maneuvers between the two groups
Figure 3.

Comparison of Cormack-Lehane grading between the two groups
Figure 4.

Heart rate variation between the two groups
Figure 5.

Mean arterial blood pressure variation between the two groups
DISCUSSION
In our study, 87.5% of the patients were successfully intubated nasally with a TruviewPCD laryngoscope and 90% patients with King Vision. The study results were dissimilar to studies conducted by Raveendra et al., who had a 94% success rate.[4] In our study, the performers were any anesthesiologist with expertise of >30 video laryngoscopy-assisted intubations. Each successful intubation was performed in a single attempt and within 90 s and/or before the oxygen saturation fell below 95% with or without additional maneuvers such as head and neck manipulation/BURP or with the use of Magill forceps. The difference in results could be attributed due to differences in methodology and due to learning curve as described by them. Similarly, Patil Archita et al. with Truview video laryngoscope demonstrated 100% success rate where a single anesthesiologist had performed the study.[5]
We defined intubation time as the time taken from after introduction of the endotracheal tube through the nostril into nasopharynx until the passage of nasotracheal tube through the glottis and appearance of capnography trace. Usually, nasal intubation takes longer time than orotracheal intubation. Intubation time was comparable with both groups. Defining intubation time was different in different studies. Patil Archita et al., Raveendra et al., and Tseng et al. defined intubation time as measure of time taken from removal of face mask till the appearance of a capnography waveform and a failed attempt, if tracheal intubation took >60 s. They measured a total intubation time with three parts, i.e. time taken for introduction of the nasal tube from the selected nostril to the oropharynx, time from use of intubating device, and the time for passing the nasotracheal tube through the trachea till the removal of the intubating device. Intubation time was measured in three parts, respectively.[2,4,5]
Use of additional maneuvers was predefined in the methodology. Fifty-seven percent in Group T and 64% in Group K did not require any additional maneuvers. Our results have shown similarities to Hirabayashi.[7] 20% in Group T and 16% in Group K required external maneuvers. Twenty-three percent in Group T and 20% in Group K required use of Magill forceps. This was similar to Raveendra et al., who had reported a requirement of head position manipulation in 20% cases, external laryngeal maneuvers in 28% cases, and use of both maneuvers in 18% patients.[4] The use of cuff inflation as an additional maneuver was described by Baddoo and Philips in a case series for nasal intubations using the C-MAC laryngoscope.[8] On this basis, this technique was added as an additional maneuver by Patil et al. in the event of inability to intubate even despite the use of BURP (Backwards Upwards Rightwards Pressure) or external head and neck manipulation. However, it was not useful in assisting in nasal intubations in their study.[9] Considering the previous study, this technique was not incorporated in our methodology.
In our study, we obtained CLG 1 view in 24 (60%) cases in Group T and 28 (70%) cases in Group K. Arora et al. showed better glottis view with Truview compared to Macintosh.[10] Bharti et al. showed similar results with respects to glottic view with Truview.[11] Our study results were similar to Priyanka et al.[12] Improved glottis visualization was observed by Raveendra et al. (CLG 1%–86%) and Patil Archita et al. (CLG 1%–76.66%) with the Truview video laryngoscope.[4,5]
We had noted and evaluated hemodynamic changes to be comparable between the two groups with respect to HR and MAP. HR changes are not significant in Truview and King Vision video laryngoscopy within the respective groups. Similarly, MAP changes are not significant in both the groups compared to baseline and postintubation response and between the groups also. This can be explained by the limited force required for video laryngoscope-guided nasotracheal intubation. Previous studies have also shown similar results with the use of video laryngoscope to be not significant with changes in hemodynamics as was observed by Patil Archita et al.[5]
Intubation device that requires lesser manipulation of the airway would significantly reduce the sympathetic stimulation and thereby affecting the hemodynamics less as was noted by Bag et al. in their comparison of TruviewPCD and the Macintosh laryngoscope for glottic view and ease of intubation where they noted a significant rise from baseline HR with the Macintosh laryngoscope than with the TruviewPCD laryngoscope.[13] Cierniak et al. observed that King Vision had comparative hemodynamic parameters with other video laryngoscopes.[14]
Minimal bleeding was noted while passing the nasotracheal tube through the nasopharynx in 11 cases and 12 cases in Group T and Group K, respectively, which was self-limiting. Postoperative sore throat was observed in four cases in Group T and three cases in Group K in patients where video laryngoscopy-assisted intubation had failed. This finding could be attributable to the use of conventional Macintosh laryngoscope assisted with the Magill forceps for nasal intubation.
The limitations of our study were (1) this was not a crossover study, (2) due to technical impossibility, the intubation device could not be blinded from the performer, and (3) performer variation could have influenced the primary outcome of the study. However, multiple performers were utilized to avoid study bias.
CONCLUSION
Based on the results and methodology employed, we have concluded that both Truview and King Vision video laryngoscopes are equally successful for nasotracheal intubation. Supporting our hypothesis, King Vision video laryngoscope is just as effective as TruviewPCD video laryngoscope for nasotracheal intubation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Sarkılar G, Sargın M, Sarıtaş TB, Borazan H, Gök F, Kılıçaslan A, et al. Hemodynamic responses to endotracheal intubation performed with video and direct laryngoscopy in patients scheduled for major cardiac surgery. Int J Clin Exp Med. 2015;8:11477–83. [PMC free article] [PubMed] [Google Scholar]
- 2.Tseng KY, Lu IC, Shen YC, Lin CH, Chen PN, Cheng KI, et al. A comparison of the video laryngoscopes with Macintosh laryngoscope for nasotracheal intubation. Asian J Anesthesiol. 2017;55:17–21. doi: 10.1016/j.aja.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 3.Lee RA, van Zundert AA, Maassen RL, Willems RJ, Beeke LP, Schaaper JN, et al. Forces applied to the maxillary incisors during video-assisted intubation. Anesth Analg. 2009;108:187–91. doi: 10.1213/ane.0b013e31818d1904. [DOI] [PubMed] [Google Scholar]
- 4.Raveendra US, Mehandale SG, Shetty SR, Kamath MR. Evaluation of the Truview EVO2 laryngoscope for nasotracheal intubation. Saudi J Anaesth. 2012;6:398–402. doi: 10.4103/1658-354X.105882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patil Archita R, Sahni Saloni C, Patil Rajaram S, Veer T. Nasotracheal intubation using two laryngoscope blades Truview and Mccoy: A comparative study to evaluate a videolaryngoscope for cases of orofacial malignancies. Int J Med Res Prof. 2016;2:40–4. [Google Scholar]
- 6.Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–61. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 7.Hirabayashi Y. GlideScope ® videolaryngoscope facilitates nasotracheal intubation. Can J Anaesth. 2006;53:1163. doi: 10.1007/BF03022888. [DOI] [PubMed] [Google Scholar]
- 8.Baddoo HK, Phillips BJ. Cuff inflation to aid nasotracheal intubation using the C-MAC videolaryngoscope. Ghana Med J. 2011;45:84–6. doi: 10.4314/gmj.v45i2.68934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patil VV, Subramanya BH, Kiranchand N, Bhaskar SB, Dammur S. Does C-MAC ® video laryngoscope improve the nasotracheal intubating conditions compared to Macintosh direct laryngoscope in paediatric patients posted for tonsillectomy surgeries? Indian J Anaesth. 2016;60:732–6. doi: 10.4103/0019-5049.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arora S, Sayeed H, Bhardwaj N. A comparison of truview EVO2 laryngoscope with Macintosh laryngoscope in routine airway management: A randomized crossover clinical trial. Saudi J Anaesth. 2013;7:244–8. doi: 10.4103/1658-354X.115322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bharti N, Arora S, Panda NB. A comparison of McCoy, TruView, and Macintosh laryngoscopes for tracheal intubation in patients with immobilized cervical spine. Saudi J Anaesth. 2014;8:188–92. doi: 10.4103/1658-354X.130705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Priyanka AS, Nag K, Hemanth Kumar VR, Singh DR, Kumar S, Sivashanmugam T, et al. Comparison of king vision and truview laryngoscope for postextubation visualization of vocal cord mobility in patients undergoing thyroid and major neck surgeries: A randomized clinical trial. Anesth Essays Res. 2017;11:238–42. doi: 10.4103/0259-1162.200240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bag SK, Kumar VR, Krishnaveni N, Ravishankar M, Velraj J, Aruloli M, et al. Acomparative study between Truview (PCD) laryngoscope and Macintosh laryngoscope in viewing glottic opening and ease of intubation: A crossover study. Anesth Essays Res. 2014;8:372–6. doi: 10.4103/0259-1162.143152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cierniak M, Timler D, Wieczorek A, Sekalski P, Borkowska N, Gaszynski T, et al. The comparison of the technical parameters in endotracheal intubation devices: The Cmac, the Vividtrac, the McGrath Mac and the Kingvision. J Clin Monit Comput. 2016;30:379–87. doi: 10.1007/s10877-015-9727-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


