Abstract
Purpose:
Antibacterials are commonly prescribed to Pediatric Intensive Care Unit (PICU) patients. However, inappropriate antibacterial prescriptions lead to increases in antibacterial resistance, treatment cost, duration of treatment, and poor clinical outcome. The antibacterial utilization study assesses the prescription patterns and if necessary recommends the interventions to improve antibacterial prescriptions. Hence, the present prospective groundwork was conducted.
Materials and Methods:
The study was conducted over the period of 6 months (April 18 to October 20, 2014). The demographics and drug use details were captured daily from patients admitted to PICU to assess World Health Organization indicators.
Results:
A total of 200 patients enrolled, among them 119 males and 81 females. There were 12.46 (±6.16) drugs prescribed per patient, of which 2.38 (±1.48) were antibacterials. Among the total drug prescribed, 18.49% were antibacterials and 97% patients received at least one antibacterial. Ceftriaxone (49.48%) was the most commonly prescribed antibacterial, while imipenem (2.58%) and colistin (2.06%) use was very low. A total of 80.95% antibacterials were prescribed by generic name, 94.88% were administered intravenously, and 80.76% were prescribed from hospital pharmacy. The average length of PICU stay was 6.15 days (±6.20), the average length of antibacterial treatment was 6.08 days (±6.27), and the average length of empirical antibacterial treatment was 5.50 days (±5.40). The cost of antibacterial therapy per patient was Indian rupees 824.64 (±235.35). In 27 patients, bacterial culture test was positive and of whom 21 received antibacterials as per sensitivity pattern.
Conclusions:
The use of antibacterials was not indiscriminately high but more prescriptions per sensitivity pattern are required.
Keywords: Antibacterials, drug utilization, encounter, indicators, Pediatric Intensive Care Unit
INTRODUCTION
Incidence of infections in patients admitted to Pediatric Intensive Care Unit (PICU) is high due to the presence of critical illness and occurrence of nosocomial infections, which leads to higher use of antibacterial agents.[1,2,3,4] The inappropriate use of antibacterials causes emergence of antibacterial-resistant organisms, resulting in prolonged hospital stay, increased mortality and morbidity, high treatment costs, and increased burden on existing hospital resources.[5,6,7,8]
Drug use studies are more essential in pediatric pharmacotherapy since one-third of the total prescriptions in children are systemic antibacterials such as vancomycin, colistin, meropenem, imipenem, and piperacillin-tazobactam.[9,10,11,12,13,14,15] A prospective drug usage study of antibacterials may serve as an important source of information for the assessment of prescription patterns and formulating future antibacterial usage policies. There is a lack of data on the antibacterial use from our PICU; therefore, the present study was conducted with the aim to evaluate the current prescribing pattern of vancomycin, colistin, meropenem, imipenem, and piperacillin-tazobactam along with other antibacterials and also to assess the antibacterial treatment cost.
MATERIALS AND METHODS
Ethics
The study was initiated after obtaining the Institutional Ethics Committee (IEC) approval. Written informed consent was obtained from the parent and legal guardian of the patient. Assent waiver was sought and granted by the IEC because the patients were critically ill and it would not have been possible to take assent of the patients.
Study design
This was a prospective, cross-sectional, observational antibacterial utilization study.
Study site
This study was conducted at the Department of Pediatrics and Clinical Pharmacology of a Tertiary Care Medical College and Hospital.
Study population
Consecutive patients admitted to the PICU regardless of previous admission history were enrolled in the study with day 1 of admission into PICU being considered as the 1st day of the study. Each admission was considered as a separate patient encounter and all patients were followed up until death, discharge, or transfer to the general ward.
Study procedure
Patient's medical records were scrutinized daily. Demographic details, clinical diagnosis, details of antibacterial use (name, dose, frequency, route and length of treatment, prescribed as generic or brand, change in antibacterial agent, and fixed-dose combination [FDC]), total number of drugs prescribed, culture and sensitivity data, length of stay, and cost of antibacterial treatment were recorded in an online Google spreadsheet.
Calculation of costs
The costs of antibacterials were obtained from hospital pharmacy price list (for those available on hospital schedule) and from the Monthly Index of Medical Specialties (MIMS_ http://www.mims.com/).
Definitions
Antibacterial was defined as an agent that interferes with the growth and reproduction of bacteria
-
Antibacterial use was classified into empiric use or definitive use:[16]
- Empiric use of antibacterial agent was defined as administration of an antibacterial agent within 72 h of admission in PICU, while microbiologic cultures' results are pending or use of antibacterial agents in situations after 72 h of admission when microbiologic cultures do not yield a pathogen
- Definitive (therapeutic) use of antibacterial agent was defined as use of any antibacterial agent at a time when microbiologic culture results and susceptibility data are available. This was at the time of initiation of therapy or after empiric antimicrobial use has been initiated once microbiological culture results are available.
World Health Organization indicators
Below mentioned indicators related to antibacterial use are divided into three main sections.[17,18]
Prescribing indicators
Average number of drugs prescribed per patient, percentage of antibacterial agents prescribed, percentage of patients who received an antibacterial agent, average number of antibacterial agents prescribed per patient, percentage of antibacterial agents prescribed by generic name, percentage of antibacterial agents prescribed by intravenous route, percentage of antibacterial agents available in hospital pharmacy, percentage of patients in whom a change of antibacterial agent was required, percentage of antibacterial agents prescribed as FDC, average length of antibacterial treatment, average length of empirical use of antibacterials, percentage of total antibacterial treatment cost, and average antibacterial treatment cost per patient over the study period.
Patient care indicators
Patient care indicators were average length of PICU stay and percentage of mortality during PICU stay.
Supplemental indicators
Supplemental indicators were percentage of patients who received antibacterial treatment as per se nsitivity pattern.
Sample size calculation
No formal sample size calculation was done due to lack of any previous data on the subject, which could be used for the same. A total of 200 patient encounters were enrolled over 6-month period.
Statistical analysis
Descriptive statistics were used and data were expressed using measures of central tendency. Numerical data were tested for normality using the Kolmogorov–Smirnov test. The cost of treatment was compared in patients with infection and without infectious cause of admission using unpaired t-test at 5% significance. The percentage of antibacterials prescribed was compared in patients with infection and without infectious cause of admission using Fisher's exact test. All analyses were done with Statistical Package for the Social Sciences (SPSS) 20 [IBM, Armonk, NY, United States of America].
RESULTS
Demographics
During the 6-month study period (April 18 to October 20, 2014), 200 patients were enrolled (119 male, 81 female) with a median age of 11 months (1, 144) and median weight of 6.4 kg (1.1, 40). There were 188 (94%) patients admitted to PICU only once, 10 (5%) had two admissions, and 2 (1%) had three admissions. Respiratory diseases (28.5%) followed by cardiovascular diseases (21.0%) and central nervous system diseases (11.0%) contributed to most of the PICU admissions. A total of 99 patients were admitted with an infectious disease, whereas 101 patients had a noninfectious cause for admission to the PICU.
Antibacterial use indicators
Table 1 summarizes the antibacterial use indicators. Patients were prescribed (on an average), 12.46 (± 6.16) drugs, of which 2.38 (±1.48) were antibacterial agents. Almost all patients (97%) received at least one antibacterial agent and most of the prescriptions were for intravenous use (94.88%). In all, 63 (32.47%) patients received single antibacterial agent and 131 (67.53%) patients received two or more antibacterial agents. Ceftriaxone (49.48%) was the most commonly prescribed antibacterial agent among patients with both infectious and noninfectious etiology for admission to PICU while imipenem (2.58%) and colistin (2.06%) use was very low. The details of all antibacterials prescribed are presented in Table 2. Meropenem was used more frequently among patients with an infection but vancomycin use was similar in patients with or without an infectious cause for PICU admission.
Table 1.
Antibacterial use indicators
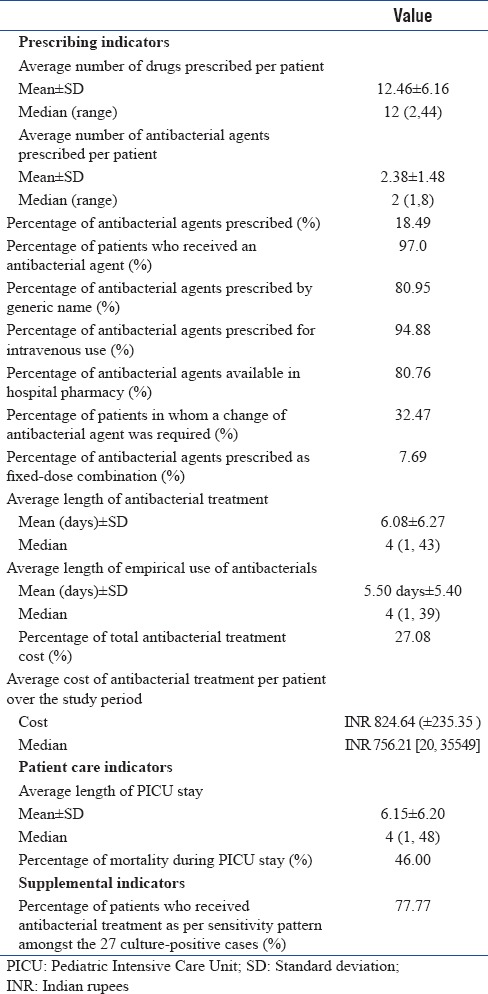
Table 2.
Frequency of antibacterial prescribed in patients admitted to Pediatric Intensive Care Unit
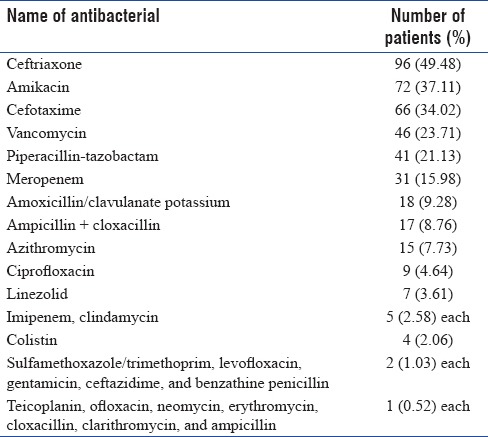
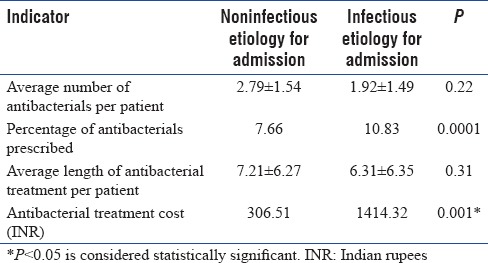
Majority of the antibacterials prescribed were available in hospital pharmacy (80.76%), they were prescribed by generic name (80.95%), and only 7.69% were FDCs. A total of 27.08% cost incurred for antibacterial treatment, where per-patient antibacterial cost was Indian rupees (INR) 824.64. The average length of PICU stay was 6.15 days, the average length of antibacterial treatment was 6.08 days, the average length of empirical antibacterial treatment was 5.50 days and during their PICU stay, change of antibacterial agent was required in 32.47% patients. Of the 27 bacterial culture-positive patients, 21 received antibacterials as per se nsitivity pattern. Acinetobacter baumannii (22.58%) was the most isolated organism followed by Klebsiella pneumoniae (16.13%) and Burkholderia cepacia (12.90%) and details of all isolated organisms are listed in Table 3. The difference in number of antibacterials used and their duration of use between patients with infectious and noninfectious cause of admission was not statistically significant (P = 0.22 and 0.31, respectively) as shown in Table 4. The difference in the cost of treatment among the two groups was statistically significant (P = 0.001). The percentage of antibacterials (10.83%) prescribed in patients with infectious etiology was significantly (P = 0.0001) higher than the patients with noninfectious etiology (7.66%).
Table 3.
Details of isolated organisms
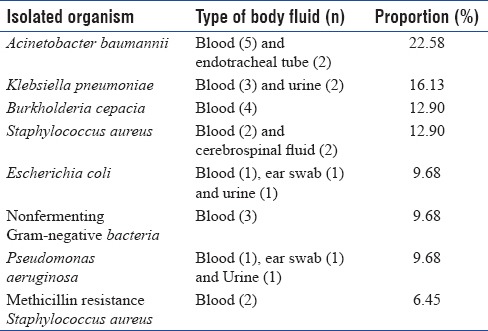
Table 4.
Comparison between patients with infectious and noninfectious etiology for admission to Pediatric Intensive Care Unit
DISCUSSION
Descriptive data on antibacterial use are important because it would reveal the extent of use and temporal trends of antibacterial use. The majority of patients were male as was also seen in study conducted by Kanish et al. and Thiruthopu et al.[19,20] The present study has six major findings. First, a high percentage of patients (97%) received antibacterial agents during their PICU stay. Second, the empirical use of antibacterial agents is high due to low culture yield and a total of 21 (77.77%) among 27 patients whom the culture tests positive received antibacterials as per se nsitivity pattern; since the antibacterials were not changed if patient is recovering, i.e., when there is complete resolution of clinical findings (signs and symptoms and leukocytosis) and clinical improvement when there is a partial resolution of clinical findings. Third, in 94.88% patients, the antibacterials were administered intravenously and a large number of prescriptions (80.95%) were by generic name. Fourth, the presence of Gram-negative bacteria (80.65%) was higher compared to Gram-positive bacteria in the samples tested for culture and sensitivity analysis. Fifth, a low antibacterial treatment cost (INR 824.64) per patient over the study period and sixth, a short average duration of PICU stay (6.15 days).
There are various studies which have reported that between 36% and 97% patients received antimicrobial treatment during their stay in the PICU.[1,5,19,21,22,23,24,25] In India, study conducted by Kanish et al.[19] reported that the 91.6% patients received antibiotics, while the study conducted in Europe [5,22,24] found lowest percentages of patients exposed to antimicrobial (36%–67%) compared with studies conducted in the US (71%–97%)[23,25] and a study conducted in China (95%).[21] Thus, the percentage of patients in our PICU who received at least one antibacterial agent was high as like the US and China studies. This may be due to perceived high bacterial infections in developing country like India, nature of the illness, and poor hygiene in socioeconomically poor populations. The average number of antibacterials prescribed per patient (2.38) was found to be similar with the study conducted by Kanish et al. (1.917) and Abbas et al. (3.00).[2,19] The prescription by generic name varies from 13.3% to 93% across the globe, and in our study, we found a high number of prescriptions by generic name (80.95%) and high use of generics which may have led to low treatment costs.[26,27,28,29] A total of 27% cost was spent on antibacterial agents (INR 824) which was low compared to a study conducted in another part of India by Kanish et al. (INR 3338). A reason for the low cost was probably due to availability of medicines in the hospital pharmacy which provides medicines at a subsidized cost. There was a significantly higher cost incurred by patients with an infectious cause of admission (INR 1414) as compared to those who were admitted for a noninfectious disease (INR 306), indicating the use of higher antibiotics for a longer duration. In our study, we found that the majority of antibacterials were given intravenously (94.88%) possibly to reduce the mortality and morbidity in an emergent situation since this is a tertiary referral center and most of the patients come with a fairly advanced disease requiring emergent action. The average length of stay (6.15 days) and the average length of antibacterial treatment (6.08 days) were similar indicating that on each day of admission patient received antibacterial.
Among 200 patients, only 27 patients had positive cultures and of these 21 received antibacterials as per se nsitivity pattern. The low culture yield was probably due to receipt of antibacterials before PICU admission. Other studies have also found higher percentages of empiric antimicrobial treatment (58% and 72%) in PICUs.[20,25] Ceftriaxone was the most commonly prescribed antibacterial as also seen in other Indian studies.[19,29] In our study, we found that the use of imipenem (2.58%) and colistin (2.0%) was minimal, indicating that higher antibacterials were being used only in resistant cases or because of nonavailability in hospital pharmacy, while the use of vancomycin, piperacillin-tazobactam, and meropenem was adequate. The percentages of death (46%) were found to be higher, and this may be because of only critically ill patients were admitted to PICU of this tertiary referral center and because of late referral from other hospitals.
CONCLUSIONS
The study concludes that the average number of antibacterials prescribed per patient was not indiscriminately high. The empirical use of antibacterials was found to be high. The present study on antibacterial prescribing patterns provides a framework for future continuous prescription audit in the PICU and interventions to change practice (if necessary).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors thank Dr. Avinash Supe, Director - Medical Education and Major Hospitals and Dean, Seth G.S. Medical College and KEM Hospital, Mumbai, for granting permission to publish this manuscript.
REFERENCES
- 1.Sodhi J, Satpathy S, Sharma DK, Lodha R, Kapil A, Wadhwa N, et al. Healthcare associated infections in Paediatric Intensive Care Unit of a tertiary care hospital in India: Hospital stay & extra costs. Indian J Med Res. 2016;143:502–6. doi: 10.4103/0971-5916.184306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abbas Q, Ul Haq A, Kumar R, Ali SA, Hussain K, Shakoor S, et al. Evaluation of antibiotic use in Pediatric Intensive Care Unit of a developing country. Indian J Crit Care Med. 2016;20:291–4. doi: 10.4103/0972-5229.182197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ding H, Yang Y, Chen Y, Wang Y, Fan S, Shen X, et al. Antimicrobial usage in paediatric Intensive Care Units in China. Acta Paediatr. 2008;97:100–4. doi: 10.1111/j.1651-2227.2007.00580.x. [DOI] [PubMed] [Google Scholar]
- 4.Bidone N, Giglio N, Bakir J, Sheehan MG, Arias López MP, Rosin M, et al. Prescription and use of antibiotics at a pediatric Intensive Care Unit in Buenos Aires city. Arch Argent Pediatr. 2008;106:409–15. doi: 10.1590/S0325-00752008000500007. [DOI] [PubMed] [Google Scholar]
- 5.Van Houten MA, Luinge K, Laseur M, Kimpen JL. Antibiotic utilization for hospitalized paediatric patients. Int J Antimicrob Agents. 1998;10:161–4. doi: 10.1016/s0924-8579(98)00022-3. [DOI] [PubMed] [Google Scholar]
- 6.Bhullar HS, Shaikh FA, Deepak R, Poddutoor PK, Chirla D. Antimicrobial justification form for restricting antibiotic use in a pediatric Intensive Care Unit. Indian Pediatr. 2016;53:304–6. doi: 10.1007/s13312-016-0841-0. [DOI] [PubMed] [Google Scholar]
- 7.Niederman MS. Appropriate use of antimicrobial agents: Challenges and strategies for improvement. Crit Care Med. 2003;31:608–16. doi: 10.1097/01.CCM.0000050464.70382.D6. [DOI] [PubMed] [Google Scholar]
- 8.Pulcini C, Pradier C, Samat-Long C, Hyvernat H, Bernardin G, Ichai C, et al. Factors associated with adherence to infectious diseases advice in two Intensive Care Units. J Antimicrob Chemother. 2006;57:546–50. doi: 10.1093/jac/dki483. [DOI] [PubMed] [Google Scholar]
- 9.Kanish R, Gupta K, Juneja S, Bains HS, Kaushal S. Prescribing pattern and pharmacoeconomics of antibiotic use in the department of pediatrics of a tertiary care medical college hospital in Northern India. Ann Trop Med Public Health. 2015;8:101–4. [Google Scholar]
- 10.Kaur S, Gupta K, Bains HS, Kaushal S. Prescribing pattern & cost-identification analysis of antimicrobial use in respiratory tract infections. JK Sci. 2013;15:19–23. [Google Scholar]
- 11.Thrane N, Olesen C, Schønheyder HC, Sørensen HT. Socioeconomic factors and prescription of antibiotics in 0- to 2-year-old Danish children. J Antimicrob Chemother. 2003;51:683–9. doi: 10.1093/jac/dkg118. [DOI] [PubMed] [Google Scholar]
- 12.Majeed A, Moser K. Age- and sex-specific antibiotic prescribing patterns in general practice in England and Wales in 1996. Br J Gen Pract. 1999;49:735–6. [PMC free article] [PubMed] [Google Scholar]
- 13.Shamshy K, Begum IM, Perumal P. Drug utilization of antimicrobial drug in pediatrics population in a tertiary care hospital in Erode, Tamilnadu, India. Int J Pharm Tech Res. 2011;3:1530–6. [Google Scholar]
- 14.Shankar PR, Upadhyay DK, Subish P, Dubey AK, Mishra P. Prescribing patterns among paediatric inpatients in a teaching hospital in Western Nepal. Singapore Med J. 2006;47:261–5. [PubMed] [Google Scholar]
- 15.Ghai OP, Paul VK, Bagga A. Essential Pediatrics. 7th ed. New Delhi: CBS; 2009. Disorders of respiratory system; pp. 351–2. [Google Scholar]
- 16.Camins BC, King MD, Wells JB, Googe HL, Patel M, Kourbatova EV, et al. Impact of an antimicrobial utilization program on antimicrobial use at a large teaching hospital: A randomized controlled trial. Infect Control Hosp Epidemiol. 2009;30:931–8. doi: 10.1086/605924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. How to investigate drug use in health facilities: Selected drug use indicators. Geneva: World Health Organization; 1993. [Last accessed on 2014 Jan 08]. Available from: http://www.apps.who.int/medicinedocs/en/d/Js2289e/ [Google Scholar]
- 18.World Health Organization. How to investigate antimicrobial use in hospitals: Selected indicators. Geneva: World Health Organization; 2012. [Last accessed on 2014 Jan 08]. Available from: http://www.apps.who.int/medicinedocs/documents/s21031en/s21031en.pdf . [Google Scholar]
- 19.Kanish R, Gupta K, Juneja S, Bains HS, Kaushal S. Prescribing pattern of antibiotics in the department of pediatrics in a tertiary care medical college hospital in Northern India. Asian J Med Sci. 2014;5:69–72. [Google Scholar]
- 20.Thiruthopu NS, Mateti UV, Bairi R, Sivva D, Martha S. Drug utilization pattern in South Indian pediatric population: A prospective study. Perspect Clin Res. 2014;5:178–83. doi: 10.4103/2229-3485.140558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ding H, Yang Y, Wei J, Fan S, Yu S, Yao K, et al. Influencing the use of antibiotics in a Chinese pediatric Intensive Care Unit. Pharm World Sci. 2008;30:787–93. doi: 10.1007/s11096-008-9220-9. [DOI] [PubMed] [Google Scholar]
- 22.Fischer JE, Ramser M, Fanconi S. Use of antibiotics in pediatric intensive care and potential savings. Intensive Care Med. 2000;26:959–66. doi: 10.1007/s001340051288. [DOI] [PubMed] [Google Scholar]
- 23.Toltzis P, Rosolowski B, Salvator A. Etiology of fever and opportunities for reduction of antibiotic use in a pediatric Intensive Care Unit. Infect Control Hosp Epidemiol. 2001;22:499–504. doi: 10.1086/501940. [DOI] [PubMed] [Google Scholar]
- 24.Briassoulis G, Natsi L, Tsorva A, Hatzis T. Prior antimicrobial therapy in the hospital and other predisposing factors influencing the usage of antibiotics in a pediatric critical care unit. Ann Clin Microbiol Antimicrob. 2004;3:4. doi: 10.1186/1476-0711-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grohskopf LA, Huskins WC, Sinkowitz-Cochran RL, Levine GL, Goldmann DA, Jarvis WR, et al. Use of antimicrobial agents in United States neonatal and pediatric intensive care patients. Pediatr Infect Dis J. 2005;24:766–73. doi: 10.1097/01.inf.0000178064.55193.1c. [DOI] [PubMed] [Google Scholar]
- 26.Dimri S, Tiwari P, Basu S, Parmar VR. Drug use pattern in children at a teaching hospital. Indian Pediatr. 2009;46:165–7. [PubMed] [Google Scholar]
- 27.Nsimba SE. Assessing prescribing and patient care indicators for children under five years old with malaria and other disease conditions in public primary health care facilities. Southeast Asian J Trop Med Public Health. 2006;37:206–14. [PubMed] [Google Scholar]
- 28.Hyam E, Brawer M, Herman J, Zvieli S. What's in a teaspoon? Underdosing with acetaminophen in family practice. Fam Pract. 1989;6:221–3. doi: 10.1093/fampra/6.3.221. [DOI] [PubMed] [Google Scholar]
- 29.Venkateswaramurthy N, Murali R, Sampath Kumar R. The study of drug utilization pattern in pediatric patients. Int J Pharm Pharm Sci. 2013;5:140–4. [Google Scholar]


