Abstract
Background:
Evaluation of late-onset speech and swallowing complications of tracheostomy on neurotrauma cases, as the most common intensive care unit procedure, needs to be evaluated.
Objectives:
A prospective study conducted in a tertiary care teaching hospital to find the late-onset speech and swallowing complications of tracheostomy in neurotrauma cases.
Materials and Methods:
This prospective observational study was conducted in the intensive care unit on intubated patients needing elective tracheostomy at a tertiary care teaching institute in South India with a dedicated referral trauma center. A data collection tool was prepared to find age, gender, date of admission, tracheostomy, and discharge, contact address and number, initial and final diagnosis, initial Glasgow Coma Scale (GCS) on admission and subsequent GCS before and after tracheostomy, ventilator settings before and after the tracheostomy, procedure and intraoperative complications, type of cannula used, details of decannulation, and respiratory difficulties.
Results:
In our study among 69 cases between 16 and 75 years' age range with mean 46.67 ± 16.65, majority were males (75.36%) and 60 were cranial cases (86.96%). Of the alive cases (21 [30.43%]) who underwent tracheostomy; 18 were performed in operation theater and 3 as bedside procedure. Major problems reported were: Speech problems (not able to phonate) (9), feeble voice (6), pain while speaking (6), and reduced loudness (6), frequent throat clearing while speaking (4), cough while speaking (3); breathlessness while speaking (1), gasping while speaking (1) and vocal tiredness (1); aspirations (2) and painful swallowing (1).
Conclusions:
Our study suggested that though, majority of neurotrauma patients require tracheostomy for long term ventilator support and associated speech and swallowing problems are expected.
Keywords: Neurotrauma, tracheostomy, traumatic brain injury
INTRODUCTION
Main cause for mortality in neurotrauma cases is cerebral hypoxia. The mechanical ventilator leads to decrease in intracranial pressure and hypoxia which is also essential due to their lack of ability to protect the airway, pooling up of excessive secretions, and inability to take adequate spontaneous ventilation. Tracheostomy, one of the most common intensive care unit procedures performed on neurotrauma cases, helps in airway management and also lessens the incidence of ventilator-associated pneumonia. The advantages of tracheostomy include patient comfort, better oral hygiene, opportunity for oral feeding, and safe and easier nursing care for airway than translaryngeal intubation.[1] Although patients have shorter days of intensive care, mechanical ventilation, and hospital stays, there are risks in long-term and acute stages for which decision for tracheostomy must be individually considered as the need for prolonged airway access is identified which is generally made within 7–10 days. Bedside techniques allow rapid tracheostomy with low morbidity. The efficacy of tracheostomy teams and tracheostomy hospital services with standardized protocols for tracheostomy insertion and care has been associated with improved outcomes. The clinical studies on late complications of tracheostomy once the patient gets discharged from the hospital are lacking. Most of the patients undergo decannulation of before discharge, yet few patients with excessive secretions and sustained very severe head injury need long-term care before (and after as well) decannulation. Although tracheostomy is part of the standard operative process in the management of neurotrauma cases, literature search showed relatively little data available on the impact and importance of tracheostomy in neurotrauma patients.[2] We report a prospective study conducted in a tertiary care teaching hospital on the late-onset speech and swallowing complications of tracheostomy in neurotrauma cases.
MATERIALS AND METHODS
This prospective observational study was carried out in Intensive Care Unit (ICU) on intubated patients needing elective tracheostomy performed at a tertiary care dedicated referral trauma center of a teaching hospital. A data collection tool was prepared to note down the sociodemographic details about the patients' age, gender, date of admission, date of tracheostomy, date of discharge, contact address and number, initial and final diagnosis, initial Glasgow Coma Scale (GCS) on admission and subsequent GCS before and after tracheostomy, ventilator settings before and after the tracheostomy, procedure and intraoperative complications, type of cannula used, details of decannulation, respiratory difficulties, problems with the wound and associated injuries, swallowing difficulties, and voice difficulties, number of days of ICU stay and hospital stay, and the survival status as well as outcome variables. Details of the clinical profile during hospital stay and after discharge were noted.
The Institutional Ethical Committee approved the study protocol. All the consecutive patients who underwent percutaneous tracheostomy (PCT) and 69 intubated patients in ICU on mechanical ventilation needing elective tracheostomy were enrolled for the study irrespective of gender or age were included in this study. Pediatric patients, patients with distorted neck anatomy with unidentifiable anatomic landmarks and coagulopathy, patients requiring emergency airway access, and patients coming from outside hospital with tracheostomy in situ were excluded from the study. The study was conducted by a team which included neuroanesthesia and neurosurgery residents and consultants. This study comprised cohort of all patients admitted to neurosurgery ICU with head injury/spinal injury/intracerebral hematomas/acute large infarcts requiring decompressive craniectomies/evacuation of intracerebral hematomas and others such as head injury with maxillofacial injuries, if needed or in neurosurgery ICU by neuroanesthetist at any time before the decision to perform tracheostomy. Acute physiology and GCS score were used to define the severity of illness. All patients with a head injury underwent noncontrast computed tomography brain to rule out intracranial hemorrhage. In this study, the patients were managed as per ICU protocol, the decision for intubation was taken by emergency physician in casualty, and the decision of tracheostomy was done by primary consultant or neurosurgeon/neurophysician.
Those patients with a low GCS score and spinal injury with tachypnea and inadequate oxygen saturation (SPO2) after initial mechanical ventilation undergone tracheostomy with a standardized open technique either in ICU bedside or in operation theater (OT) if it was available by the neurosurgical resident/consultant. After the tracheostomy, a patient was shifted to ICU for monitoring and regular suctioning of the tracheal secretions by staff nurse as well as other ancillary care with nurse-patient ratio in ICU as 1:2–3. When the patient was stabilized and able to maintain SPO2 on T-piece ventilation/on room air, the patient was shifted to neurosurgery ward with a nurse-patient ratio of 1:10. The caregivers of the patients were trained in the nursing care of tracheostomy gradually and optimal as well as critical precautions to be undertaken regarding hygiene and feeding. Daily tracheostomy care was provided by the staff nurse, and patients were discharged after regaining adequate consciousness and after decannulation of the tracheostomy tube. The patients who were discharged with tracheostomy tube, their caregivers were given adequate training regarding tracheostomy casre. They were also asked to buy foot operated or electric suction apparatus and were trained in sucking off the excess-pooled secretions and then the patient gets discharged. Patients were followed till discharge from hospital or death due to any cause during hospital stay. After discharge, patients were also followed about complications during follow-up visits and on telephonic conversation up to 6 months after discharge.
Statistical analysis
Data were entered on Excel and were analyzed using IBM SPSS Statistics, Version 24.0. (Armonk, NY: IBM Corp USA). Continuous variables were summarized with standard descriptive statistics.
RESULTS
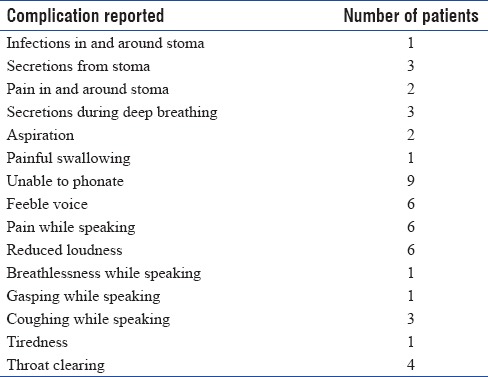
In our study, the patients who had undergone tracheostomy 69 were between 16 and 75 years' age range with mean 46.67 ± 16.65, three-fourths majority were males (n = 52, 75.36%). Out of 69 patients taken with this study, 60 (86.96%) were cranial cases and 9 were spinal cases; 22 were dead in the follow-up, 21 are alive, and 26 patients could not be contacted. Among 21 cases, 18 had undergone tracheostomy in OT and 3 had bedside procedure. Problems with wound: Out of 21 patients, one had infections in and around stoma, three had secretions from stoma, and two had pain in around stoma. Breathing difficulties: Out of 21 patients, three had secretions from stoma during deep breathing and no other difficulty was reported. Problems in swallowing: Out of 21 patients, two reported aspirations while swallowing and one reported painful swallowing. Speech problems: many patients reported problems related to voice. Nine patients were not able to phonate; Six each reported feeble voice, pain while speaking, and reduced loudness; four reported frequent throat clearing while speaking, three reported cough while speaking, while one each reported breathlessness while speaking, gasping while speaking, and vocal tiredness [Table 1].
Table 1.
Long-term profile of tracheostomy (n=69)
DISCUSSION
Prolonged endotracheal (ET) intubation in neurotrauma is associated with injury to the larynx and trachea and also leads to more discomfort of the patient and irritability which requires the use of sedatives. Once these people get discharged, the feedback on the problems faced at later time at home is lacking. Against this background, a prospective study was done to assess the late-onset speech and swallowing complications of tracheostomy in neurotrauma cases.
Most of the patients undergo decannulation of tracheostomy tube before discharge. Yet, in cases of excessive secretions in very severe head injury, when it took prolonged decannulation and hospital stay with financial constraints of patients, the domiciliary caregivers were provided adequate training in tracheostomy as well as nursing care. Further, they were asked to procure a small foot operated or electric suction apparatus with capacity building in sucking off the excess pooled secretions before the patient were discharged. A study from Pune, India, however, reported that among their road traffic accident group, cases showed benefits of early tracheostomy in neurotrauma cases with severely impaired consciousness.[2] A study on nonneurosurgical cases revealed that early tracheostomy patients tend to have shorter stay of ICU and hospital compared to late tracheostomy patients, and early or late tracheostomy showed no significant effect on mortality.[3] In neurosurgical cases, secondary trauma can worsen chances of mortality irrespective of tracheostomy timing. In neurological disorders and head injury cases, mortality rate was high as reported by Aass.[4]
Short-term complication may include pneumothorax, damage to trachea and other adjacent organs, bleeding, and infections, and long-term complications may arise relating to long-standing artificial airway.[5] Early tracheostomy and late tracheostomy did not show much difference in terms of complications, but early tracheostomy reduces number of ICU days and duration of sedation. In critically ill patients, death would not be caused by tracheostomy alone. A systemic review reported by Siempos et al. also mentioned the same thing. Mortality rate in ICU reduced in early tracheostomy cases contrary to some studies.[6] Early tracheostomy can reduce respiratory problems such as ventilator-associated pneumonia and sepsis.[6,7] There is a decline in rate of complication with PCT.[6] In a retrospective study of large sample size, results showed increased mortality rate in late tracheostomy cases (>10 days) followed by intermediate tracheostomy [5–9 days] followed by early tracheostomy (<4 days).[7] Late tracheostomy cases can have more complications – bleeding, stoma infections, granuloma, and tracheal stenosis.[8] These, in turn, can cause more damage to swallowing and speaking. As reported by Durbin et al.,[1] tracheostomy causes less damage to the larynx, communication ability, and swallowing. Furthermore, they suggested better preservation of glottis competence which is essential in reducing aspiration and for phonation. In the present study, only 3 out of 21 cases reported swallowing difficulties, thus indicating advantage of tracheostomy than prolonged mechanical ventilation. However, speech complaints were more but they could be treated in following visits. Norwood et al reported that in long-term follow-up after tracheostomy, subjective voice changes were reported in 27% patients while two cases had major voice changes with persistent hoarseness.[9]
In our study, 29% of patients reported speech problems and 10% reported respiratory problems. Similar finding was reported by Aass – 17 out of 43 patients reported laryngeal problems.[4] In conventional tracheostomy cases, often, a single patient may present with multiple complaints than percutaneous tracheostomy cases.[10] Similar findings were noted in our present study, where few patients reported three complaints. A study from Kolkata, India, reported that late complications such as left-sided vocal cord paralysis, hoarseness of voice, and voice change were checked for at 1 month but were absent in all cases.[11] Further, the published literatures do not provide evidence of consistent advantages of tracheostomy across the dissimilar diagnoses.[12,13]
Strengths and limitations
The strengths of the study are that little data have been available in the published literature to assess the late-onset speech and swallowing complications of tracheostomy in neurotrauma cases. We had few limitations as well; first, the inclusion of patients with different diagnoses and diverse indications for ventilatory support has been a major limitation of these studies in estimating the complications of tracheostomy in neurotrauma cases. Further, a small number of patients were also a limitation of our study.
CONCLUSIONS
The finding of our study showed that majority of neurotrauma patients require tracheostomy for long-term ventilator support, and these issues may be complicated with late-onset speech troubles in good number of cases while swallowing-related problems were negligible.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Durbin CG, Jr, Perkins Mp, Moores LK. Should tracheostomy be performed as early as 72 hours in patients requiring prolonged mechanical ventilation? Respir Care. 2010;55:76–87. [PubMed] [Google Scholar]
- 2.Zirpe KG, Tambe DV, Deshmukh AM, Gurav SK. The impact of early tracheostomy in neurotrauma patients: A Retrospective study. Indian J Crit Care Med. 2017;21:6–10. doi: 10.4103/0972-5229.198309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Puentes W, Jerath A, Djaiani G, Cabrerizo Sanchez R, Wąsowicz M. Early versus late tracheostomy in cardiovascular intensive care patients. Anaesthesiol Intensive Ther. 2016;48:89–94. doi: 10.5603/AIT.a2016.0016. [DOI] [PubMed] [Google Scholar]
- 4.Aass AS. Complications to tracheostomy and long-term intubation: A follow-up study. Acta Anaesthesiol Scand. 1975;19:127–33. doi: 10.1111/j.1399-6576.1975.tb05232.x. [DOI] [PubMed] [Google Scholar]
- 5.Bösel J, Schiller P, Hook Y, Andes M, Neumann JO, Poli S, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): A randomized pilot trial. Stroke. 2013;44:21–8. doi: 10.1161/STROKEAHA.112.669895. [DOI] [PubMed] [Google Scholar]
- 6.Siempos II, Ntaidou TK, Filippidis FT, Choi AM. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: A systematic review and meta-analysis. Lancet Respir Med. 2015;3:150–8. doi: 10.1016/S2213-2600(15)00007-7. [DOI] [PubMed] [Google Scholar]
- 7.Bickenbach J, Fries M, Offermanns V, Von Stillfried R, Rossaint R, Marx G, et al. Impact of early vs. Late tracheostomy on weaning: A retrospective analysis. Minerva Anestesiol. 2011;77:1176–83. [PubMed] [Google Scholar]
- 8.Romero J, Vari A, Gambarrutta C, Oliviero A. Tracheostomy timing in traumatic spinal cord injury. Eur Spine J. 2009;18:1452–7. doi: 10.1007/s00586-009-1097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norwood S, Vallina VL, Short K, Saigusa M, Fernandez LG, McLarty JW, et al. Incidence of tracheal stenosis and other late complications after percutaneous tracheostomy. Ann Surg. 2000;232:233–41. doi: 10.1097/00000658-200008000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hazard P, Jones C, Benitone J. Comparative clinical trial of standard operative tracheostomy with percutaneous tracheostomy. Crit Care Med. 1991;19:1018–24. doi: 10.1097/00003246-199108000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kiran S, Eapen S, Chopra V. A comparative study of complications and long term outcomes of surgical tracheostomy and two techniques of percutaneous tracheostomy. Indian J Crit Care Med. 2015;19:82–6. doi: 10.4103/0972-5229.151015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung NH, Napolitano LM. Tracheostomy: Epidemiology, indications, timing, technique, and outcomes. Respir Care. 2014;59:895–915. doi: 10.4187/respcare.02971. [DOI] [PubMed] [Google Scholar]
- 13.Pinheiro Bdo V, Tostes Rde O, Brum CI, Carvalho EV, Pinto SP, Oliveira JC, et al. Early versus late tracheostomy in patients with acute severe brain injury. J Bras Pneumol. 2010;36:84–91. doi: 10.1590/s1806-37132010000100014. [DOI] [PubMed] [Google Scholar]


