Abstract
Importance
It is unclear if helping patients meet resource needs, such as difficulty affording food, housing, or medications, improves clinical outcomes.
Objective
To determine the effectiveness of the Health Leads (HL) program on improvement in systolic and diastolic blood pressure (SBP, DBP; units: mm Hg), low-density lipoprotein cholesterol (LDL-C; units: mg/dL), and hemoglobin A1c (HbA1c).
Design
Difference-in-difference evaluation of HL from October 1, 2012 through September 30, 2015. HL consists of screening for unmet needs at clinic visits, and offering those who screen positive to meet with an ‘advocate’ to help obtain resources, or receive brief information provision.
Setting
Three academic primary care practices
Participants
5125 people screened, using a standardized form, for unmet basic resource needs
Main Outcome(s) and Measure(s)
Changes in SBP, DBP, LDL-C, and HbA1c. We compared those who screened positive for unmet basic needs (HL group) to those who screened negative, using intention-to-treat, and, secondarily, between those who did and did not enroll in HL, using linear mixed modeling, examining the period before and after screening.
Results
Of 5125 people screened, 1774 (35%) reported at least one unmet need, and 58% of those enrolled in HL. Median follow-up for those who screened positive and negative was 34 and 32 months, respectively. In unadjusted intention-to-treat analyses of 1998 participants with hypertension, the HL group experienced greater reduction in SBP (differential change −1.2 95% Confidence Interval [CI] −2.1 to −0.4) and DBP (differential change −1.0 95% CI −1.5 to −0.5). For 2281 individuals with an indication for LDL-C lowering, results also favored the HL group (differential change −3.7, 95%CI −6.7 to −0.6). For 774 individuals with diabetes, the HL group did not show HbA1c improvement (differential change −0.04% 95%CI −0.17% to 0.10%). Results adjusted for baseline demographic and clinical differences were not qualitatively different. Among those who enrolled in HL program, there were greater BP and LDL-C improvements then for those who declined (SBP differential change −2.6 95%CI −3.5 to −1.7; SBP differential change −1.4 95%CI −1.9 to −0.9; LDL-C differential change −6.3 95%CI −9.7 to −2.8).
Conclusions and Relevance
Screening for and attempting to address unmet basic resource needs in primary care was associated with modest improvements in blood pressure and lipid, but not blood glucose, levels.
Keywords: Food Insecurity, Health Expenditures, Socioeconomic Status, Diabetes, Cardiovascular Disease, Hypertension
Chronic cardiometabolic diseases, such as hypertension, diabetes, and lipid disorders, are leading causes of morbidity and mortality in the U.S.1, 2 The connection between poor outcomes in these conditions and unmet resource needs, such as difficulty affording food, housing, and medications, has become increasingly clear.3–17 This has led to interest in programs that seek to ‘link’ patients identified in clinical care sites as having unmet basic resource needs to community-based resources.18 This interest is exemplified by the recent Accountable Health Communities (AHC) model proposed by the Centers for Medicare & Medicaid Services (CMS)3. Specifically, interventions to screen for unmet needs and link patients to community resources in order to address them are at the heart of Track 2 and Track 3 of the AHC model.3
Despite growing interest and intuitive appeal, there is as yet scant evidence to support the effectiveness of ‘linkage’ interventions for improving cardiometabolic disease control. To help understand the potential of linkage interventions in chronic cardiometabolic disease management, we conducted a pragmatic evaluation of the Health Leads program in three primary care practices.19 The Health Leads program includes screening for unmet resource needs, an assessment of those who report these needs, and assignment to an ‘advocate’, who then works with a patient to receive resources and benefits to meet those needs.19 For example, a patient who reports difficulty affording food could be assisted with enrollment in the Supplemental Nutrition Assistance Program (SNAP). Conceptually, such assistance could enhance and make more effective the routine care being delivered to patients. For example, addressing transportation issues could enable patients to attend a greater proportion of clinic appointments, and assisting with medication affordability could enable patients to adhere to their treatment plan more closely. Therefore, we hypothesized that participation in the Health Leads program would be associated with improvements in key indicators of cardiometabolic disease management: blood pressure, low density lipoprotein cholesterol (LDL-C) and Hemoglobin A1c (HbA1c) control.
Methods
Setting and Study Participants
We conducted a pragmatic evaluation of the Health Leads program in three academic adult (age > 18 years) internal medicine practices within a primary care network in the Boston metropolitan area. Patients who presented for routine care completed screening for unmet basic resource needs at visit check-in. All who completed screening between October 1, 2013 (when the program began in the clinics) and April 30, 2015 were included in the study. Electronic health record data for participants were obtained from October 1, 2012 (i.e. at least 1 year prior to screening) through September 30, 2015 (i.e. at least 5 months after screening).
The Health Leads program was implemented as the standard of care during the study period, therefore, the Human Research Committee at Partners Health Care approved this analysis of usual care data with a waiver of the informed consent requirement.
Screening and Intervention
The Health Leads program has been described in detail elsewhere.19 In brief, patients complete a standardized screening form that allowed the patient to self-identify unmet resource needs related to food, medications, transportation, utilities, employment, elder care services and housing. Patients who report unmet needs are referred to program staff to complete an assessment and determine if the patient should be enrolled in the program or receive a “rapid resource referral”, which consisted of one-time provision of information. Patients who choose to enroll in the program are assigned to an ‘advocate’, usually an undergraduate student volunteer, operating under the supervision of professional program staff, who works with the patient to prioritize unmet basic resource needs, identify community resources and/or public benefits to meet them, and facilitate receipt of those resources and/or benefits. Each situation had standardized guidelines to indicate when a case could be closed with one of three resolution types: (1) benefits had been received (‘successful’), (2) the need was met elsewhere, could not be met or the advocate lost contact with the patient (‘unsuccessful’), or (3) the patient indicated they were able to move forward without continued assistance (‘equipped’).19 As an example, if a patient reported a food need, and was eligible for but not enrolled in SNAP, the advocate would work with the participant until they were enrolled and benefits were available on an electronic benefit transfer card.19
Outcomes
Our primary outcome was systolic blood pressure (SBP) trend, as it is the most common cardiometabolic risk factor, and is strongly associated with morbidity and mortality.20 Our secondary outcomes were diastolic blood pressure (DBP), LDL-C, and HbA1c. These outcomes are targeted for clinical management in adults with pre-existing cardiometabolic diseases. Therefore, for blood pressure outcomes we included those individuals with a history of hypertension. Similarly, for analyses of LDL-C, participants had a diagnosis of hypertension, coronary heart disease, chronic kidney disease, or diabetes mellitus. For analyses of HbA1c, we included participants with diabetes mellitus. These diagnoses were assessed at time of screening, and were determined using previously validated electronic health record algorithms, which have been used in prior studies (validation documents available upon request).19, 21, 22 Outcome data were collected as part of routine clinical care. Just as patients often qualify for more than one clinical performance metric, participants could be included in the analysis of more than one outcome (e.g. a participant with diabetes and hypertension would be included in the analyses of SBP, DBP, LDL-C, and HbA1c).
We also considered several covariates that may influence the trend in study outcomes. Age, gender, race/ethnicity, educational attainment, health insurance, primary language, clinical conditions, and comorbidity as indicated by the Charlson comorbidity score were abstracted from the electronic health record and adjusted for in our analyses.19
Statistical Analysis
We first performed descriptive statistics. Given that the Health Leads program had adequate capacity to serve all patients identified through screening in the three practices, there was no group of participants who completed screening but were not offered interventional services. Therefore, to test whether program referral was associated with improved health outcomes, we used a difference-in-difference approach. In this design, participants serve as their own controls by comparing trends in outcome before and after the intervention. Simultaneously, those who received care in the same practices during the same time, but screened negative for unmet resource needs, were used to account for ‘secular trends’: other occurrences, aside from the Health Leads program, that may have influenced the outcomes, such as on-going chronic disease management programs in the clinics. Our primary analyses compared those with one of the defined conditions who screened positive (regardless of whether they enrolled in the Health Leads program) to those with one of the defined conditions who screened negative for unmet resource needs. Analogous to an intention-to-treat analysis of a randomized controlled trial, this approach provides the best estimate of the real world effectiveness of the program. As secondary analyses, we also examined change in outcome trend by Health Leads participation category—comparing those who screened negative to those who screened positive but declined a referral to Health Leads, those who declined services after an initial interview with Health Leads, those who received only a ‘rapid resource referral’, and those who fully enrolled in the Health Leads program. The date of screening demarcated the pre- and post-intervention periods for both groups. Participants needed to have at least one outcome measurement in the pre- and post-period in order to be included in the main analyses, but we conducted sensitivity analyses that did not include this requirement. We analyzed the outcomes as continuous variables because blood pressure, LDL-C, and HbA1c have a linear association with poor health outcomes over most of their clinically relevant range23–25. As outcomes could be measured multiple times per participant and were not measured on a fixed schedule (‘unbalanced’ design) we used longitudinal mixed effects linear regression models for hypothesis testing, with patient level random effects to account for repeated measurements within patients. All observations of a particular parameter (e.g. blood pressure) were used for analysis. A p-value < 0.05 indicated statistical significance.
Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC).
Results
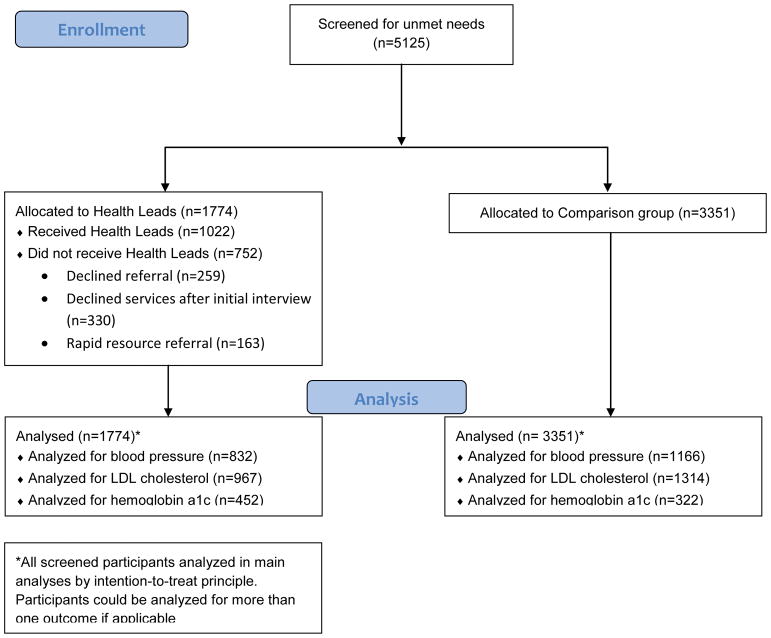
Overall, 5125 people were screened for unmet basic resource needs at the participating practices from October 1, 2013 to April 30, 2015 (Figure 1). Of these, 1774 (35%) screened positive for at least one unmet resource need. Of those who screened positive, they reported a median of 2 (25th percentile: 1; 75th percentile: 3) unmet needs. Overall, those reporting unmet resource needs were more likely to self-identify as a racial/ethnic minority, have less than high school diploma education, speak a primary language other than English, and have Medicaid insurance (Table 1).
Figure 1.
Study Flow Diagram
Table 1.
Patient characteristics
| Screened Negative for Unmet Needs N=3351 |
Screened Positive for Unmet Needs* N=1774 |
|
|---|---|---|
| Age, years (SD) | 56.7 (16.2) | 57.6 (15.5) |
| Female (%) | 56.5 | 55.7 |
| Race/Ethnicity | ||
| Non-Hispanic white (%) | 85.9 | 53.2 |
| Non-Hispanic black (%) | 5.0 | 23.5 |
| Hispanic (%) | 3.2 | 13.7 |
| Asian/Multi/Other (%) | 5.9 | 9.6 |
| Insurance | ||
| Commercial (%) | 64.1 | 38.2 |
| Medicare (%) | 27.4 | 38.0 |
| Medicaid (%) | 4.3 | 15.5 |
| Self-pay (%) | 4.3 | 8.4 |
| ≤High School Diploma Education | 22.1 | 58.3 |
| Non-English Primary Language (%) | 8.3 | 23.8 |
| Charlson Score (SD) | 3.1 (2.4) | 4.0 (2.9) |
| Cardiometabolic disease groups | ||
| Hypertension | 34.8 | 46.9 |
| Indication for LDL lowering | 39.2 | 54.5 |
| Diabetes | 9.6 | 25.5 |
| Program Enrollment Status | ||
| Enrolled | -- | 57.6 |
| Declined Referral | -- | 14.6 |
| Declined Services After Initial Interview | -- | 18.6 |
| Rapid Resource Referral | -- | 9.2 |
LDL = Low Density Lipoprotein Cholesterol
Considered the intervention group for main, intention-to-treat, analyses
Of those who screened positive, 58% (n=1021) enrolled in the Health Leads program, 14.6% (n=259) declined referral, and 17.0% (n=301) declined services after an initial interview. The most commonly reported needs were in the areas of healthcare, including medication affordability, utilities, and food. For those enrolled in Health Leads, cases were open for a median 42 days (25th percentile: 24; 75th percentile: 71), and participants received a median 5 (25th percentile: 3; 75th percentile: 9) contacts from their advocate. Of those who discussed their needs with Health Leads, 29.7% of reported needs were closed as ‘successful’, 27.9% as ‘equipped’, 34.9% as ‘unsuccessful’ and 7.1% handled with a rapid resource referral. Almost all (93%) of the ‘unsuccessful’ category involved participants who stopped responding to attempts to contact them from Health Leads advocates.
For blood pressure analyses, 832 participants who screened positive and 1166 participants who screened negative met inclusion criteria (eTable 1). For LDL-C analyses, 967 participants who screened positive and 1314 participants who screened negative were included. For HbA1c analyses, 452 participants who screened positive and 322 who screened negative were included. Those who screened positive represent the Health Leads group for the following analyses. Median time studied was 34 (25th percentile: 25; 75th percentile: 36) months for those who screened positive and 32 (25th percentile: 26; 75th percentile: 36) months for those who screened negative. Those who screened positive had a median time studied prior to screening of 17 (25th percentile: 11; 75th percentile: 26) months, and median time followed after screening of 12 (25th percentile: 7; 75th percentile: 19) months. Those who screened negative had a median time studied prior to screening of 25 (25th percentile: 18; 75th percentile: 28) months, and median time followed after screening of 6 (25th percentile: 6; 75th percentile: 8) months (eTable 2).
Of those with hypertension, baseline systolic blood pressure was slightly higher (133.1 mm Hg vs. 131.8 mm Hg, p=0.04) in the Health Leads group, but diastolic blood pressure was similar (76.6 mm Hg vs. 76.3 mm Hg, p =0.35) (Table 2). In unadjusted difference-in-difference analyses, the differential change after screening favored the Health Leads group, with greater reduction in SBP (differential change −1.2 mm Hg 95% Confidence Interval [CI] −2.1 to −0.4 mm Hg) and DBP (differential change −1.0 mm/Hg 95% CI −1.5 to −0.5 mm Hg) (Figure 2). In models adjusted for age, gender, race/ethnicity, educational attainment, primary language, health insurance, clinical conditions (diabetes, chronic kidney disease, coronary heart disease, cerebrovascular disease, and depression), and comorbidity score, the differential change again favored the Health Leads group (differential change in SBP −1.6 mm Hg 95% CI −2.5 1 to −0.6 mm Hg; differential change in DBP −1.1 mm Hg 95% CI −1.61 to −0.6 mm Hg).
Table 2.
Unadjusted and Adjusted Difference-in-Difference results for Blood Pressure, LDL-Cholesterol, and Hemoglobin A1c, by Screening Status
| Unadjusted | Adjusted* | ||||||
|---|---|---|---|---|---|---|---|
| SBP (mm Hg) | |||||||
| Baseline SBP (95% CI) | p | Differential Change (95% CI) | P | Differential Change (95% CI) | P | ||
| Screened Positive | 133.1 (132.2 to 134.0) | 0.04 | −1.2 (−2.1 to −0.4) | 0.006 | −1.6 (−2.5 1 to −0.6) | 0.001 | |
| Screened Negative | 131.8 (130.9 to 132.7) | -- | -- | -- | -- | -- | |
|
| |||||||
| DBP (mm Hg) | |||||||
| Baseline DBP (95% CI) | p | Differential Change | P | Differential Change | P | ||
| Screened Positive | 76.6 (76.1 to 77.1) | 0.35 | −1.0 (−1.5 to −0.5) | <.0001 | −1.1 (−1.61 to −0.6) | <.0001 | |
| Screened Negative | 76.3 (75.8 to 76.8) | -- | -- | -- | -- | -- | |
|
| |||||||
| LDL (mg/dL) | |||||||
| Baseline LDL (95% CI) | p | Differential Change | P | Differential Change | P | ||
| Screened Positive | 103.0 (100.1 to 105.9) | 0.14 | −3.7 (−6.7 to −0.6) | 0.02 | −3.9 (−7.2 to −0.6) | 0.02 | |
| Screened Negative | 100.2 (97.7 to 102.6) | -- | -- | -- | -- | -- | |
|
| |||||||
| HbA1c (%) | |||||||
| Baseline HbA1c (95% CI) | p | Differential Change | P | Differential Change | P | ||
| Screened Positive | 7.53 (7.39 to 7.66) | 0.002 | −0.04 (−0.17 to 0.10) | 0.59 | 0.03 (−0.12 to 0.17) | 0.72 | |
| Screened Negative | 7.19 (7.03 to 7.35) | -- | -- | -- | -- | -- | |
SBP = systolic Blood Pressure; DBP=Diastolic Blood Pressure; LDL = Low-density lipoprotein cholesterol; HbA1c = Hemoglobin A1c.
Adjusted for age, gender, race/ethnicity, educational attainment, primary language, health insurance, comorbidity score, and presence of diabetes, chronic kidney disease, coronary heart disease, cerebrovascular disease, and depression
A negative value for ‘differential change’ represents a greater decrease, compared with the referent category
Figure 2.
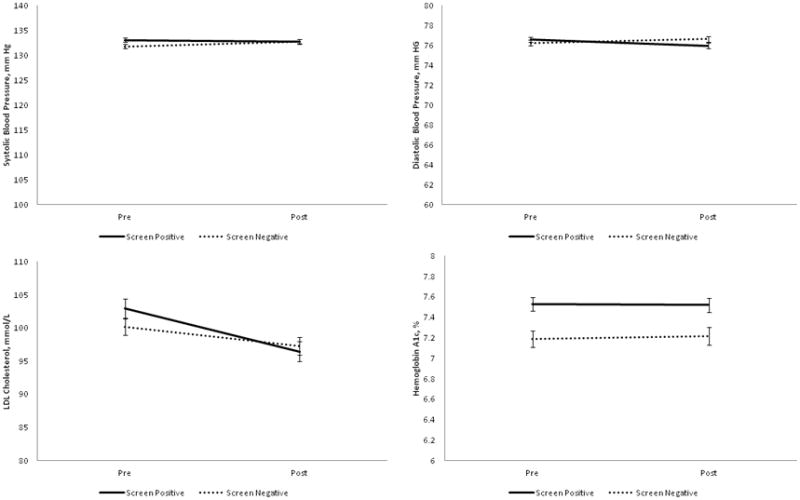
Change from pre-intervention to post-intervention, with error bars, comparing those who screened positive to those who screened negative for unmet needs, for systolic blood pressure (upper left), diastolic blood pressure (upper right), low density lipoprotein cholesterol (lower left) and hemoglobin A1c (lower right).
For those with an indication for LDL-C lowering, baseline LDL-C was similar comparing the Health Leads group (103.0 mg/dL) to those who screened negative (100.2 mg/dL), p =0.14. Unadjusted difference-in-difference results again favored the Health Leads group (differential change −3.7 mg/dL, 95%CI −6.7 to −0.6 mg/dL) (Figure 2). Adjusted results were similar (differential change −3.9 mg/dL, 95%CI −7.2 to −0.6 mg/dL).
For those with diabetes, baseline HbA1c was greater in the Health Leads group compared with those who screened negative (7.53% vs. 7.19%, p=0.002). However, the Health Leads group did not see HbA1c improvement (differential change −0.04% 95%CI −0.17% to 0.10%) (Figure 3). Adjusted results also revealed no differential improvement (0.03%, 95%CI −0.12 to 0.17).
In secondary analyses based on program enrollment, rather than just screening positive for unmet needs, enrollment in Health Leads was associated with statistically significant benefit in SBP, DBP, and LDL-C reduction (Table 3). There remained no benefit for HbA1c reduction. The magnitude of these benefits was greater than the magnitude seen in the intention-to-treat analyses. Declining services, being lost to contact, or receiving a one-time referral to a resource were generally not associated with benefit.
Table 3.
Unadjusted and Adjusted Difference-in-Difference results for Blood Pressure, LDL-Cholesterol, and Hemoglobin A1c, by Health Leads Enrollment Status
| Unadjusted | Adjusted* | ||||||
|---|---|---|---|---|---|---|---|
| SBP (mm Hg) | Baseline SBP (95% CI) | p | Differential Change (95% CI) | P | Differential Change (95% CI) | P | |
| Enrolled | 132.4 (131.6 to 133.1) | 0.50 | −2.6 (−3.5 to −1.7) | <.0001 | −2.7 (−3.7 to −1.7) | <.0001 | |
| Declined Referral | 131.8 (130.4 to 133.2) | 0.26 | −0.2 (−2.1 to 1.7) | 0.82 | −0.4 (−2.4 to 1.6) | 0.69 | |
| Declined Services After Initial Interview | 132.8 (131.4 to 134.1) | 0.72 | −0.7 (−2.6 to 1.1) | 0.44 | −0.7 (−2.7 to 1.4) | 0.51 | |
| RRR | 133.2 (131.2 to 135.2) | 0.50 | −2.2 (−5.3 to 1.0) | 0.18 | −4.0 (−8.1 to 0.1) | 0.06 | |
| Screened Negative | 132.6 (131.9 to 133.2) | -- | -- | -- | -- | -- | |
|
| |||||||
| DBP (mm Hg) | Baseline DBP (95% CI) | p | Differential Change | P | Differential Change | P | |
| Enrolled | 76.4 (75.9 to 76.8) | 0.18 | −1.4 (−1.9 to −0.9) | <.0001 | −1.5 (−2.1 to −0.98) | <.0001 | |
| Declined Referral | 75.9 (75.1 to 76.7) | 0.07 | −0.2 (−1.2 to 0.9) | 0.75 | 0.0 (−1.1 to 1.2) | 0.96 | |
| Declined Services After Initial Interview | 76.6 (75.8 to 77.4) | 0.99 | −1.1 (−2.2 to −0.1) | 0.03 | −1.1 (−2.3 to 0.0) | 0.06 | |
| RRR | 75.7 (74.6 to 76.8) | 0.11 | 0.4 (−1.4 to 2.2) | 0.65 | 0.0 (−2.4 to 2.3) | 0.97 | |
| Screened Negative | 76.6 (76.2 to 77.0) | -- | -- | -- | -- | -- | |
|
| |||||||
| LDL (mg/dL) | Baseline LDL (95% CI) | p | Differential Change | P | Differential Change | P | |
| Enrolled | 105.0 (101.5 to 108.6) | 0.02 | −6.3 (−9.7 to −2.8) | 0.0003 | −7.0 (−10.7 to −3.3) | 0.0002 | |
| Declined Referral | 96.5 (88.8 to 104.2) | 0.40 | 1.9 (−4.8 to 8.6) | 0.58 | 1.7 (−5.4 to 8.8) | 0.63 | |
| Declined Services After Initial Interview | 104.2 (96.5 to 111.8) | 0.31 | −0.6 (−7.0 to 5.8) | 0.85 | 2.5 (−4.6 to 9.6) | 0.49 | |
| RRR | 92.1 (81.0 to 103.1) | 0.17 | 4.5 (−4.6 to 13.6) | 0.33 | 3.9 (−7.6 to 15.4) | 0.50 | |
| Screened Negative | 100.0 (97.6 to 102.5) | -- | -- | -- | -- | -- | |
|
| |||||||
| HbA1c (%) | Baseline HbA1c (95% CI) | p | Differential Change | P | Differential Change | P | |
| Enrolled | 7.55 (7.39 to 7.72) | 0.002 | −0.07 (−0.21 to 0.07) | 0.34 | −0.02 (−0.17 to 0.13) | 0.81 | |
| Declined Referral | 7.15 (6.79 to 7.50) | 0.85 | 0.04 (−0.22 to 0.29) | 0.77 | 0.16 (−0.12 to 0.44) | 0.26 | |
| Declined Services After Initial Interview | 7.73 (7.35 to 8.12) | 0.01 | −0.07 (−0.31 to 0.18) | 0.61 | −0.02 (−0.27 to 0.24) | 0.90 | |
| RRR | 7.49 (6.95 to 8.03) | 0.29 | 0.08 (−0.25 to 0.41) | 0.64 | 0.06 (−0.31 to 0.43) | 0.76 | |
| Screened Negative | 7.19 (7.02 to 7.35) | -- | -- | -- | -- | -- | |
RRR = Rapid Resource Referral SBP = systolic Blood Pressure; DBP=Diastolic Blood Pressure; LDL = Low-density lipoprotein cholesterol; HbA1c = Hemoglobin A1c.
Adjusted for age, gender, race/ethnicity, educational attainment, primary language, health insurance, comorbidity score, and presence of diabetes, chronic kidney disease, coronary heart disease, cerebrovascular disease, and depression
Enrollment Categories: Enrolled = enrolled in Health Leads program. Declined Services = Screened positive for unmet needs, but did not contact Health Leads program. Lost From Triage = Screened positive for unmet needs, made contact with Health Leads but did not complete enrollment. Rapid Referral = Screened positive for unmet needs, received one-time information or advice, did not enroll in Health Leads program. Screened negative = screened negative for unmet needs.
A negative value for ‘differential change’ represents a greater decrease, compared with the referent category
Sensitivity analyses that did not require participants to have an outcome measurement in both the pre- and post-screening period were not substantially different from the main analyses (eTable 3). Information on health related quality of life in a subset of randomly selected participants (eTable 4), a ‘responder’ analysis of those with ‘out-of-control’ parameters that came under control in the post-intervention period (eTable 5), and a more detailed breakdown of presenting needs (eTable 6) is available in the supplemental material.
Discussion
In this study, we found that screening for unmet basic needs coupled with referral to a program that helped link patients to community resources and public benefits to meet those needs resulted in modest improvements in blood pressure and LDL-cholesterol, but not Hemoglobin A1c. These findings persisted even after adjustment for potential confounders. The association between intervention and blood pressure and cholesterol improvement was stronger for those who enrolled in the program, although this study cannot demonstrate causality.
This study is consistent with and extends our knowledge of healthcare interventions to address basic resource needs. While few other programs have focused specifically on unmet needs, several other strategies to address social determinants of health in clinic care have been tried, with variations in workforce (lay vs. professional), setting (clinic vs. community based), and on-going interaction (longitudinal empanelment vs. episodic engagement).26–36 For example, community health worker programs often use a ‘lay’ workforce, based outside of the clinic, who work with specific patients over a long period of time.29 Alternatively, care coordination and case management programs are often based in clinics or healthcare systems, and use professional staff, such as registered nurses or licensed clinical social workers.32, 35 Case management programs often feature longitudinal panels, while some social work referrals are more episodic in nature. Several of these approaches have achieved success for chronic disease management, although none focus specifically on unmet basic needs. This study presents an alternative model—lay clinic-based undergraduate volunteers, trained and equipped with tools to address episodic issues with basic resource needs—and finds that this approach can be successful.
The magnitude of the benefits in blood pressure and LDL-C improvement seen in this study may not be important clinically to an individual but are likely important at the population level, particularly considering that the results occurred in patient populations that typically benefit less from usual medical care, and that there is unlikely to be substantial harm from participation in the program. The reductions in blood pressure and LDL cholesterol seen in patients who enrolled in Health Leads are similar to those seen in a recent successful randomized control trial of a multi-faceted quality improvement intervention that did not focus on unmet basic resource needs.26 Further, a 2 mm Hg reduction in systolic blood pressure or a 1 mm Hg reduction in diastolic blood pressure is associated with an approximately 5% reduction in relative risk for coronary heart disease events.24 Similarly, a 4 mmol/L reduction in LDL is associated with a 4% reduction in relative risk for coronary heart disease events.23
An unanswered question resulting from this study is why BP and LDL improved, while HbA1c did not. At this time, we are not sure why we observed this. Prior studies have established the importance of improving dietary quality, in addition to medication, in controlling hyperglycemia.37 The data in this study suggest that connections to resources to meet various needs (e.g. medication affordability and food) occur with equal success. However, the result of that connection may vary depending on the adequacy and efficacy of the ‘resource landscape’ available. For example, reducing financial barriers to medications (such as may occur if patients enroll in a pharmacy assistance program), is closely linked to improved adherence and improved health.12 However, connection to food resources, such as enrollment in SNAP or receipt of food from a food pantry, while effective for improving food insecurity, may not support the changes in dietary quality necessary to improve HbA1c. The CMS’ AHC model, which seeks to test linkage interventions to improve health, acknowledges the important role of the resource landscape.3 In the AHC’s ‘Track 3’—Engagement—CMS calls upon healthcare delivery organizations to partner with social service providers in the same community in order to help tailor the resources available both to meet basic resource needs and to improve health.3
An important strength of this study is its pragmatic design. Compared with a highly selected population in a randomized-controlled trial, this study evaluated program operation in ‘real-world’ conditions, and with the intention-to-treat analytic approach, the estimates of effects are likely generalizable to other primary-care settings serving populations that are underrepresented in randomized control trials. We should note, however, that clinic-based interventions such as this one do not reach those who are out of care. Although participants chose whether to enroll in the program after screening, we do not believe that differences in engagement with care or self-efficacy among those who enrolled are likely to have influenced improvement in the study outcomes. The difference-in-difference design helps account for these unmeasured differences in participant characteristics by comparing participants to their own pre-intervention results. Further, the lack of benefit observed with regard to HbA1c suggests enrollment is not synonymous with improvement. However, without randomization it is impossible to exclude these differences as possible contributors to the findings observed. Finally, because program entry was not predicated on having elevated values of the study outcomes, but rather on unmet needs, regression to the mean is unlikely to explain the observed differences between the groups.
Despite these strengths, the results of this study should be interpreted in the light of several limitations. First, the three practices in this study already had advanced population health management programs that focused on blood pressure, cholesterol, and HbA1c. How these results would generalize to practices without such programs is unclear; it is possible that other settings could see larger reductions. Nevertheless, the results help understand what can be gained by adding programs that address unmet basic needs to current chronic disease management efforts. Second, the study was set in Massachusetts, where health insurance coverage is high.38 However, because national health insurance rates are, after the implementation of the Affordable Care Act, rising to the level of Massachusetts, the results are likely relevant in many settings.38 Other limitations include lack of information on those who did not complete screening, lack of information on duration of diabetes and tobacco use, and that the study analyst was not blinded to the exposure groups.
This study has several implications for the future study and use of linkage interventions. First, the “rapid resource referral” used in this study is similar to what is proposed in Track 1 of the AHC model, and did not show benefit.3 Second, because 40% of our participants reporting unmet needs had commercial insurance, linkage programs may be worthwhile in a broad array of clinical settings. It will be important to determine whether linkage programs can be combined with ongoing population management efforts, such as identifying patients overdue for visits or not meeting clinical goals. Additionally, future work should focus on improvements to the program that may increase the benefits seen, and increase the conversion rate between those reporting needs and ultimate linkage to resources. Additionally, studies of linkage interventions incorporating randomized designs, particularly with cluster-randomization above the level of the participant (in order to include a more ‘real-world’ selection of participants compared with participant-level randomization), would provide important complementary information. Finally, while this study focused on indicators of cardiometabolic control, there are several other potentially important outcomes for a linkage intervention that should be considered when evaluating its impact. Health related quality of life, reduction in stress and depressive symptoms, along with other indicators of mental well being, engagement with care, and the cost-effectiveness of the intervention are all important areas for future studies to investigate.
Conclusion
An intervention program that screens for unmet basic needs and attempts to link patients with these needs to community resources improved blood pressure and LDL-cholesterol, but not HbA1c. Further refinement of these types of interventions, and their dissemination, holds promise for improving the health of vulnerable populations.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the assistance of Carine Y. Yelibi, who was employed at Massachusetts General Hospital during the time of the study, in formatting the data for analysis. The authors also gratefully acknowledge Hilary Placzek, who is an employee of Health Leads, for assistance with obtaining data on program use, and Anya Dangora, who was employed by Health Leads during part of the study, for assistance in obtaining data on patient health status.
Funding Support: Seth A. Berkowitz was supported by the Division of General Internal Medicine and the Diabetes Population Health Research Center at Massachusetts General Hospital.
Biographies
Seth A. Berkowitz conceived of the study and drafted the manuscript. Steven J. Atlas conceived of the study and revised the manuscript critically for important intellectual content. Amy Catherine Hulberg, Sara Standish, and Gally Reznor made substantial contributions to the design of the study and revised the manuscript critically for important intellectual content. All authors give final approval of the version to be published and agree to accountability. An earlier version of these analyses, containing only 6 months of results data, was presented at the Society for General Internal Medicine meeting on April 23, 2015.
Seth A. Berkowitz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Prior Presentation: An earlier version of these analyses, with only 6 months of data, was presented at the Society for General Internal Medicine meeting on April 23rd, 2015.
Conflict of Interest Disclosures: Seth A. Berkowitz, Steven J. Atlas, and Gally Reznor declare they have no conflicts of interest to report. Amy Catherine Hulberg and Sara Standish are employees of Health Leads. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; or preparation, review, decision to submit for publication, or approval of the manuscript.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Judd SE, Kissela BM, Lackland DT, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Willey JZ, Woo D, Yeh RW, Turner MB. Heart disease and stroke statistics--2015 update: A report from the american heart association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Murphy SL, Xu J, Kochanek KD, Bastian BA. Deaths: Final data for 2013. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2016;64:1–119. [PubMed] [Google Scholar]
- 3.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities--addressing social needs through medicare and medicaid. N Engl J Med. 2016;374:8–11. doi: 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
- 4.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among u.S. Adults with diabetes. Diabetes care. 2013;36:3093–3099. doi: 10.2337/dc13-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berkowitz SA, Gao X, Tucker KL. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: Results from the boston puerto rican health study. Diabetes care. 2014;37:2587–2592. doi: 10.2337/dc14-0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, Schow M, Atlas SJ, Wexler DJ. Material need insecurities, control of diabetes mellitus, and use of health care resources: Results of the measuring economic insecurity in diabetes study. JAMA Intern Med. 2015;175:257–265. doi: 10.1001/jamainternmed.2014.6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castillo DC, Ramsey NL, Yu SS, Ricks M, Courville AB, Sumner AE. Inconsistent access to food and cardiometabolic disease: The effect of food insecurity. Current cardiovascular risk reports. 2012;6:245–250. doi: 10.1007/s12170-012-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ford ES. Food security and cardiovascular disease risk among adults in the united states: Findings from the national health and nutrition examination survey, 2003–2008. Preventing chronic disease. 2013;10:E202. doi: 10.5888/pcd10.130244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health affairs (Project Hope) 2015;34:1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 10.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income nhanes participants. J Nutr. 2010;140:304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363:6–9. doi: 10.1056/NEJMp1000072. [DOI] [PubMed] [Google Scholar]
- 12.Choudhry NK, Avorn J, Glynn RJ, Antman EM, Schneeweiss S, Toscano M, Reisman L, Fernandes J, Spettell C, Lee JL, Levin R, Brennan T, Shrank WH. Full coverage for preventive medications after myocardial infarction. N Engl J Med. 2011;365:2088–2097. doi: 10.1056/NEJMsa1107913. [DOI] [PubMed] [Google Scholar]
- 13.Choudhry NK, Fischer MA, Avorn JL, Lee JL, Schneeweiss S, Solomon DH, Berman C, Jan S, Lii J, Mahoney JJ, Shrank WH. The impact of reducing cardiovascular medication copayments on health spending and resource utilization. Journal of the American College of Cardiology. 2012;60:1817–1824. doi: 10.1016/j.jacc.2012.06.050. [DOI] [PubMed] [Google Scholar]
- 14.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the american heart association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 15.Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. The Canadian journal of cardiology. 2010;26(Suppl C):8C–13C. doi: 10.1016/s0828-282x(10)71075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel MR, Piette JD, Resnicow K, Kowalski-Dobson T, Heisler M. Social determinants of health, cost-related nonadherence, and cost-reducing behaviors among adults with diabetes: Findings from the national health interview survey. Medical care. 2016;54:796–803. doi: 10.1097/MLR.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: Food insecurity, cost-related medication underuse, and unmet needs. The American journal of medicine. 2014;127:303–310 e303. doi: 10.1016/j.amjmed.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Peek ME, Ferguson M, Bergeron N, Maltby D, Chin MH. Integrated community-healthcare diabetes interventions to reduce disparities. Current diabetes reports. 2014;14:467. doi: 10.1007/s11892-013-0467-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz SA, Hulberg AC, Hong C, Stowell BJ, Tirozzi KJ, Traore CY, Atlas SJ. Addressing basic resource needs to improve primary care quality: A community collaboration programme. BMJ quality & safety. 2016;25:164–172. doi: 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 20.Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, Nonas CA, Sacks FM, Smith SC, Jr, Svetkey LP, Wadden TA, Yanovski SZ, Kendall KA, Morgan LC, Trisolini MG, Velasco G, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC, Jr, Tomaselli GF. 2013 aha/acc guideline on lifestyle management to reduce cardiovascular risk: A report of the american college of cardiology/american heart association task force on practice guidelines. Circulation. 2014;129:S76–99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 21.Berkowitz SA, Atlas SJ, Grant RW, Wexler DJ. Individualizing hba1c targets for patients with diabetes: Impact of an automated algorithm within a primary care network. Diabetic medicine : a journal of the British Diabetic Association. 2014;31:839–846. doi: 10.1111/dme.12427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grant RW, Wexler DJ, Ashburner JM, Hong CS, Atlas SJ. Characteristics of “complex” patients with type 2 diabetes mellitus according to their primary care physicians. Archives of internal medicine. 2012;172:821–823. doi: 10.1001/archinternmed.2012.1229. [DOI] [PubMed] [Google Scholar]
- 23.Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Jr, Stone NJ. Implications of recent clinical trials for the national cholesterol education program adult treatment panel iii guidelines. Circulation. 2004;110:227–239. doi: 10.1161/01.CIR.0000133317.49796.0E. [DOI] [PubMed] [Google Scholar]
- 24.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ (Clinical research ed) 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yudkin JS, Richter B, Gale EA. Intensified glucose lowering in type 2 diabetes: Time for a reappraisal. Diabetologia. 2010;53:2079–2085. doi: 10.1007/s00125-010-1864-z. [DOI] [PubMed] [Google Scholar]
- 26.Ali MK, Singh K, Kondal D, Devarajan R, Patel SA, Shivashankar R, Ajay VS, Unnikrishnan AG, Menon VU, Varthakavi PK, Viswanathan V, Dharmalingam M, Bantwal G, Sahay RK, Masood MQ, Khadgawat R, Desai A, Sethi B, Prabhakaran D, Narayan KM, Tandon N. Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals: A randomized, controlled trial. Annals of internal medicine. 2016 doi: 10.7326/M15-2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Freund T, Peters-Klimm F, Boyd CM, Mahler C, Gensichen J, Erler A, Beyer M, Gondan M, Rochon J, Gerlach FM, Szecsenyi J. Medical assistant-based care management for high-risk patients in small primary care practices: A cluster randomized clinical trial. Annals of internal medicine. 2016;164:323–330. doi: 10.7326/M14-2403. [DOI] [PubMed] [Google Scholar]
- 28.Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A, Montori VM, Spencer M, An LC. Comparison of community health worker-led diabetes medication decision-making support for low-income latino and african american adults with diabetes using e-health tools versus print materials: A randomized, controlled trial. Annals of internal medicine. 2014;161:S13–22. doi: 10.7326/M13-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kangovi S, Mitra N, Grande D, White ML, McCollum S, Sellman J, Shannon RP, Long JA. Patient-centered community health worker intervention to improve posthospital outcomes: A randomized clinical trial. JAMA Intern Med. 2014;174:535–543. doi: 10.1001/jamainternmed.2013.14327. [DOI] [PubMed] [Google Scholar]
- 30.Long JA, Jahnle EC, Richardson DM, Loewenstein G, Volpp KG. Peer mentoring and financial incentives to improve glucose control in african american veterans: A randomized trial. Annals of internal medicine. 2012;156:416–424. doi: 10.1059/0003-4819-156-6-201203200-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Margolius D, Bodenheimer T, Bennett H, Wong J, Ngo V, Padilla G, Thom DH. Health coaching to improve hypertension treatment in a low-income, minority population. Annals of family medicine. 2012;10:199–205. doi: 10.1370/afm.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among medicare beneficiaries: 15 randomized trials. Jama. 2009;301:603–618. doi: 10.1001/jama.2009.126. [DOI] [PubMed] [Google Scholar]
- 33.Perez-Escamilla R, Damio G, Chhabra J, Fernandez ML, Segura-Perez S, Vega-Lopez S, Kollannor-Samuel G, Calle M, Shebl FM, D’Agostino D. Impact of a community health workers-led structured program on blood glucose control among latinos with type 2 diabetes: The dialbest trial. Diabetes Care. 2015;38:197–205. doi: 10.2337/dc14-0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-led diabetes education programs in high-risk mexican americans improve glycemic control compared with standard approaches: A project dulce promotora randomized trial. Diabetes Care. 2011;34:1926–1931. doi: 10.2337/dc10-2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stone RA, Rao RH, Sevick MA, Cheng C, Hough LJ, Macpherson DS, Franko CM, Anglin RA, Obrosky DS, Derubertis FR. Active care management supported by home telemonitoring in veterans with type 2 diabetes: The diatel randomized controlled trial. Diabetes Care. 2010;33:478–484. doi: 10.2337/dc09-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang TS, Funnell M, Sinco B, Piatt G, Palmisano G, Spencer MS, Kieffer EC, Heisler M. Comparative effectiveness of peer leaders and community health workers in diabetes self-management support: Results of a randomized controlled trial. Diabetes Care. 2014;37:1525–1534. doi: 10.2337/dc13-2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coppell KJ, Kataoka M, Williams SM, Chisholm AW, Vorgers SM, Mann JI. Nutritional intervention in patients with type 2 diabetes who are hyperglycaemic despite optimised drug treatment--lifestyle over and above drugs in diabetes (loadd) study: Randomised controlled trial. BMJ (Clinical research ed) 2010;341:c3337. doi: 10.1136/bmj.c3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sommers BD, Musco T, Finegold K, Gunja MZ, Burke A, McDowell AM. Health reform and changes in health insurance coverage in 2014. N Engl J Med. 2014;371:867–874. doi: 10.1056/NEJMsr1406753. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.