Abstract
Perinatal regionalization, or risk-appropriate care, is an approach that classifies facilities based on capabilities to ensure women and infants receive care at a facility that aligns with their risk. The CDC designed the Levels of Care Assessment Tool (LOCATe) to assist jurisdictions working in risk-appropriate care in assessing a facility’s level of maternal and neonatal care aligned with the most current American College of Obstetricians and Gynecologists/Society for Maternal-Fetal Medicine (ACOG/SMFM) and American Academy of Pediatrics (AAP) guidelines. LOCATe produces standardized assessments for each hospital that participates and facilitates conversations among stakeholders in risk-appropriate care. This article describes how public health departments implement and use LOCATe in their jurisdictions.
Keywords: perinatal regionalization, risk-appropriate care, levels of neonatal care, levels of maternal care, CDC LOCATe, levels of care assessment tool
Introduction
Perinatal regionalization, also referred to as risk-appropriate care, is a strategy for improving maternal and neonatal health outcomes that the March of Dimes initially proposed in the 1976 report, toward improving the outcome of pregnancy (TIOP I).1 Risk-appropriate care provisions support women and infants receiving care in a facility staffed with personnel and equipment that matches their risk. Facilities are classified into levels based on functional capabilities and organized within a tiered, regionalized system of perinatal care.2 In response to TIOP I, states began to develop coordinated regional systems for perinatal care. In addition to facilities with a range of capabilities, these systems may include a regional (or tertiary) care center. Regional centers provide both the highest level of perinatal care and support lower level facilities with education, outreach, and maternal and neonatal transport.
Subsequent versions of TIOP and editions of the Guidelines for Perinatal Care broadened the focus beyond neonatal care to include comprehensive perinatal care and definitions for levels of care based on the most recent published evidence.3,4 Improved outcomes have been demonstrated for high-risk infants (e.g., very preterm or with serious medical and/or surgical conditions) when delivered at higher level facilities equipped to manage their conditions, with a meta-analysis in 2010 concluding that very low birthweight (<1500 g) and very preterm (<32 weeks gestational age) infants born in level III or higher facilities experience decreased mortality.5 These findings further highlight the importance of coordinated systems of risk-appropriate care.
In 2012, the American Academy of Pediatrics (AAP) published an updated policy statement on Levels of Neonatal Care.2 The 2012 statement updates recommendations for designation of levels of newborn care (levels I–IV) based on specific facility capabilities. While studies have found that units with a lower volume of deliveries are associated with higher mortality, evidence remains insufficient to support specific volume recommendations, and so remain absent from the 2012 AAP guidance.6,7 The policy statement discusses the importance of using standardized terminology to encourage comparison across facilities and regions and to improve accuracy and reporting of statistics and performance measures.
While the initial development of levels of care included maternal and neonatal provisions, the framework of perinatal regions and systems has generally focused on the neonate. In response to increasing levels of maternal morbidity and mortality in the United States,8,9 the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) published the Obstetric Care Consensus: Levels of Maternal Care, in 2015.10 The structure of the newly developed maternal levels of care recommendations is similar to the neonatal levels; each level (I–IV, plus birth centers) describes minimum capabilities related to facility staffing and equipment. Furthermore, the publication provides guidance that congruency between maternal and neonatal level is not the goal, but rather that a pregnant woman receives care in a facility that best meets her needs and those of the neonate. Both maternal guidance and neonatal guidance place importance on measurement and evaluation of health outcomes by reviewing facility data, as well as the role that regional centers play in coordinating transport and outreach education within their area.
While almost half of states currently have levels of neonatal care criteria defined in policy, definitions and monitoring vary widely. The specific criteria and monitoring mechanisms used for level designation can include functional criteria, utilization criteria, compliance mechanisms, regulatory sources, or a combination of these. A systematic web search in 2008 found that 22 states reference or cite AAP documents as part of their designation process. Some states choose to develop legislation that supports perinatal levels of care for regulatory and reimbursement purposes, while other states do not designate levels of care.11 This wide range of mechanisms results in a lack of consistency and presents a challenge for national efforts focused on increasing opportunities for collaboration and improvement of maternal and neonatal care.
States and jurisdictions engaged in the Collaborative Improvement and Innovation Network to Reduce Infant Mortality (IM CoIIN) identified maternal and neonatal risk-appropriate care as one of six priority strategies. This multiyear national movement engages federal, state, and local leaders, as well as public and private agencies, professionals, and communities to use quality improvement, innovation, and collaborative learning for reducing infant mortality and improving birth outcomes.12 Specifically, this strategy team aims to increase the delivery of higher risk infants and mothers at an appropriate level facility. The IM CoIIN risk-appropriate care strategy teams expressed difficulty in monitoring levels of care among facilities and highlighted the importance of developing a consistent and uniform method for assessing levels of care. We describe here how the CDC and jurisdictions developed a tool that addresses the need identified for a user-friendly and standardized approach that states can use to assess maternal and neonatal care capabilities of facilities.
CDC LOCATe Development and Implementation
The CDC Levels of Care Assessment Tool (LOCATe) was developed to provide standardized assessments that align with the 2015 ACOG/SMFM11 and 2012 AAP6 guidance and encourage conversations among stakeholders in the provision of risk-appropriate care. The CDC developed a web-based assessment tool with sections specific to both maternal and neonatal care capabilities of the responding facility (www.cdc.gov/reproductivehealth/maternalinfanthealth/LOCATe.html). To keep respondent burden to a minimum, the assessment focuses on collecting information necessary to distinguish between levels of care. The content of CDC LOCATe primarily came from the 2015 ACOG/SMFM Levels of Maternal Care and 2012 AAP Levels of Neonatal Care guidance, and can be divided into four categories. The first group of questions corresponds directly to criteria in the guidance and used to assess levels. The second group also corresponds with the criteria, but the response options have greater specificity than the guidance. There are places in the guidance where the wording is insufficient to support specificity, accommodating a variety of interpretations by respondents. For example, the ACOG/SMFM Levels of Maternal Care guidance categorizes access to a maternal-fetal medicine specialist on-site, by phone or by telemedicine equally, while CDC LOCATe separates these availability options. This approach allows responses to be assessed consistently with the guidance, while simultaneously collecting data for stakeholder analysis on possible differences in outcomes based on the type of availability of a maternal-fetal medicine specialist.
The third group of questions does not directly come from existing criteria, but rather from gaps identified by stakeholders in the evidence used to inform the development of criteria. For example, LOCATe includes questions about the volume of procedures (e.g., pediatric surgery) and volume of high-risk patients (e.g., very preterm deliveries). This information is not used for assessing levels, but to support stakeholders in developing the evidence they may need to best inform risk-appropriate care activities.
The fourth grouping of information gathered by LOCATe is based on language included in the AAP and ACOG/SMFM levels of care guidance but is not used in assessing levels of care. This information is collected to inform stakeholder conversations. Among these expanded questions is a series related to level of care self-designation and the source of that designation. The maternal section includes questions on a facility’s current protocols and drills performed for three major maternal events: obstetric hemorrhage, hypertensive emergency, and thromboembolism. LOCATe ends with a section that includes different statistics about the hospital. The neonatal section includes numbers of total live births and number of live births less than 1500 g and less than 32 weeks of gestation. The maternal section includes number of maternal deaths before discharge and women who were admitted to the intensive care unit or received four or more units of blood, the standard criteria used to estimate severe maternal morbidity. This information can be useful for the jurisdiction implementation team and their stakeholders in identifying quality improvement opportunities outside of the guidelines or generating measures used for monitoring performance of risk-appropriate care systems.
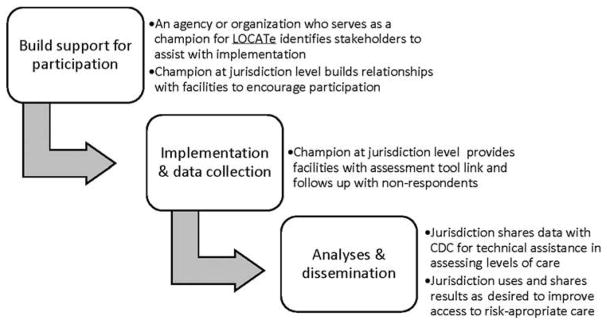
A small group of states that had participated in the IM CoIIN risk-appropriate care strategy team piloted LOCATe, first among a sample of facilities in five states, and then among all facilities in two states. The implementation process has become more refined with each additional state’s participation (Fig. 1). An agency, or champion, that has an existing relationship with the hospitals in the area, such as the public health department or the state perinatal quality collaborative, leads the implementation effort. This implementation team communicated the purpose of LOCATe with all birthing facilities in the area and may partner with the local hospital association in this effort. Following data collection, CDC provided technical assistance by applying an algorithm developed to assess a maternal and neonatal level of care for each facility. The algorithm utilized a scoring system for each of the questions that refer directly to staffing and equipment specifications in the ACOG/SMFM and AAP guidance. Each question was scored with equal weight and a maternal and neonatal level of care was assigned based on the overall score. The preliminary results were then shared back with the jurisdiction’s implementation team. The preliminary results included highlighting facilities with inconsistent responses, which required active follow-up by the implementation team to confirm responses. Together, CDC and the jurisdiction implementation team collaborated to finalize the LOCATe results, which the jurisdiction then used and disseminated in ways they determined appropriate for their setting. Access and improvements to risk-appropriate care are driven by states and jurisdictions; CDC does not retain or otherwise use jurisdictions’ LOCATe data for its own purposes.
FIG. 1.
LOCATe process diagram. LOCATe, Levels of Care Assessment Tool.
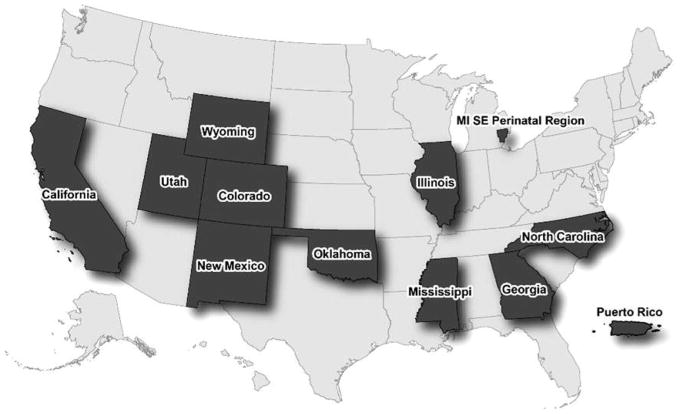
As awareness of the tool has increased—through webinars, presentations, and partnerships—additional states, perinatal regions within states, and U.S. territories outside of the IM CoIIN strategy team have shown interest in implementing CDC LOCATe. As of June 2017, 12 jurisdictions have implemented CDC LOCATe (Fig. 2).
FIG. 2.
Map of LOCATe jurisdictions.
Discussion
A myriad of factors should be considered by a jurisdiction when developing an implementation and dissemination strategy for CDC LOCATe, including existing legislation, public health agency structure, and political climate. Jurisdictions interested in implementing LOCATe are advised that the time dedicated to preparation for distribution of the tool is equally as vital as the data collection itself. Full participation from all birthing facilities in the jurisdiction is encouraged, as this approach allows a comprehensive understanding of maternal and neonatal care capabilities in their area. Implementation and use of LOCATe data vary with the resources, opportunities, and needs specific to the jurisdiction. Illinois, the Southeast Michigan Perinatal Quality Improvement Coalition (SEMP QIC), and Wyoming, are three illustrative examples of how LOCATe supports stakeholders in risk-appropriate care.
Illinois’ initial goals in implementing LOCATe were to obtain data that would enable an assessment of statewide policies and systems related to risk-appropriate care. Illinois linked LOCATe data to vital records (infant birth and death certificates) to enable detailed comparisons of patient demographics and outcomes across facilities. The Illinois analyses have revolved around answering questions related to four main topics: (1) describing the AAP and ACOG/SMFM levels of care as a statewide system and highlighting gaps in services, (2) comparing the current regionalized perinatal system to the estimated AAP and ACOG/SMFM levels of care, (3) estimating potential changes in patient volumes and geographic access to higher level facilities that might occur if the AAP levels of care were adopted, and (4) assessing between-level and within-level variation in neonatal mortality. The results of these analyses were compiled into a 25-page data report that was provided to the state Levels of Care Task Force and Perinatal Advisory Committee. Based on the information provided by the LOCATe analyses, these statewide committees recommended that Illinois revises the state perinatal code to adopt the current ACOG/SMFM and AAP level of care guidelines. Work is now underway in the state to begin the process of revising the administrative code that governs the regionalized perinatal system. In the future, Illinois plans to link the LOCATe data to the hospital discharge data to further analyze infant and maternal morbidities in relation to levels of care, seeking to strengthen the evidence supporting perinatal regionalization.
The SEMP QIC includes a membership of perinatal providers from three highly populated counties in southeast Michigan. The births in these three counties (Wayne, Oakland, and Macomb) represent 41% of the total births in Michigan and 68% of the African American births in the state. Michigan’s 3-year average (2009–2013) infant mortality rate (IMR) is 7.0 and areas in the SEMP QIC region have 3-year average IMR ranging from 11.8 to 16.1. CDC LOCATe was used as a consistent method to assess the hospital level of care available in 96% of the birthing hospitals of SEMP QIC. In-person hospital meetings occurred to confirm responses from the assessment and collect qualitative data on the patient population of each hospital. Aggregate LOCATe results were shared with SEMP QIC participating hospitals in a 1-hour webinar and at a scheduled SEMP QIC membership meeting. The hospital-specific results were shared with responding hospital for internal use and quality improvement efforts. The data collected from the use of LOCATe and the in-person visits are being used to inform the gap analysis work of SEMP QIC and guide priority areas of focus for improvements in the regions’ perinatal system of care.
Wyoming implemented LOCATe to learn about the perinatal care system in the state. LOCATe offered a standardized, relatively simple tool to capture the resources and capabilities at each Wyoming facility. State Maternal and Child Health staff are meeting with each Wyoming facility to confirm their results, and learn how levels of care are operationalized in a rural/frontier setting. A statewide perinatal level of care report will be released, which will share the assessed level of each facility. Results from LOCATe identified that several Wyoming facilities did not have specific maternal care protocols in place. As a result, Wyoming facilities are participating in the Utah Department of Health’s Extension for Community Healthcare Outcomes (ECHO) for hypertension in pregnancy. The ECHO provides a continuous learning system and connects facilities to specialist mentors at the University of Utah’s medical center. It is expected that the number of Wyoming facilities that have developed a hypertension protocol will increase through participation in the ECHO. In addition, the information gleaned from LOCATe will be used to develop program activities around risk-appropriate care, which was selected by Wyoming’s Maternal and Child Health Unit as a Title V Priority under the umbrella of prevention of infant mortality. In the future, Wyoming will include the data from LOCATe in its analyses of maternal and infant morbidities, and in an analysis of perinatal transport practices.
These examples demonstrate the flexibility of LOCATe across diverse settings as each implementation team utilized the results in alignment with needs and priorities. CDC LOCATe provides a standardized assessment of facility levels of care, supporting collaborative approaches within and between jurisdictions to strengthen systems of risk-appropriate care. Implementation of CDC LOCATe helps place an equal importance on levels of maternal and neonatal care and allows an agency to measure a facility’s capabilities in an unbiased way, anchored to national guidelines. As the number of jurisdictions that prioritize provision of risk-appropriate care systems continues to grow, adoption of CDC LOCATe may encourage collaboration at regional levels. Forging collaborations among stakeholders within and between jurisdictions will maximize the impacts of systems of risk-appropriate care and ultimately improve systems of care for women and infants.
Acknowledgments
We thank the 12 jurisdictions (California, Colorado, Georgia, Illinois, Michigan Southeast Perinatal Region, Mississippi, New Mexico, North Carolina, Oklahoma, Puerto Rico, Utah, and Wyoming) who have implemented CDC LOCATe for their collaboration and continued efforts to improve the outcomes for mothers and infants.
Footnotes
Author Disclosure Statement
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. No competing financial interests exist.
References
- 1.March of Dimes, Committee on Perinatal Health. Toward improving the outcome of pregnancy: Recommendations for the regional development of maternal and perinatal health services. White Plains, NY: March of Dimes National Foundation; 1976. [Google Scholar]
- 2.American Academy of Pediatrics Committee on Fetus and Newborn. Levels of neonatal care. Pediatrics. 2012;130:587. [Google Scholar]
- 3.American Academy of Pediatrics, American College of Obstetrics and Gynecology. Guidelines for perinatal care. 7. Elk Grove Village (IL): AAP; Washington, DC: American College of Obstetricians and Gynecologists; 2012. [Google Scholar]
- 4.March of Dimes. Towards improving the outcome of pregnancy III: Enhancing perinatal health through quality, safety, and performance initiatives (TIOP3) White Plains, NY: March of Dimes Foundation; 2010. [Google Scholar]
- 5.Lasswell SM, Barfield WD, Rochat RW, Blackmon L. Perinatal regionalization for very low-birth-weight and very preterm infants: A meta-analysis. JAMA. 2010;304:992–1000. doi: 10.1001/jama.2010.1226. [DOI] [PubMed] [Google Scholar]
- 6.Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356:2165–2175. doi: 10.1056/NEJMsa065029. [DOI] [PubMed] [Google Scholar]
- 7.Chung JH, Phibbs CS, Boscardin WJ, Kominski GF, Ortega AN, Needleman J. The effect of neonatal intensive care level and hospital volume on mortality of very low birth weight infants. Med Care. 2010;48:635–644. doi: 10.1097/MLR.0b013e3181dbe887. [DOI] [PubMed] [Google Scholar]
- 8.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among deliver and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120:1029–1036. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 10.American College of Obstetricians and Gynecologists. Levels of maternal care. Obstetric Care Consensus No. 2. Obstet Gynecol. 2015;125:502–515. doi: 10.1097/01.AOG.0000460770.99574.9f. [DOI] [PubMed] [Google Scholar]
- 11.Blackmon LR, Barfield WD, Stark AR. Hospital neonatal services in the United States: Variation in definitions, criteria, and regulatory status, 2008. J Perinatal. 2009;29:788–794. doi: 10.1038/jp.2009.148. [DOI] [PubMed] [Google Scholar]
- 12. [Accessed June 19, 2017];NICHQ Website. Available at: www.nichq.org/childrens-health/infant-health/CoIIN-to-reduce-infant-mortality.