Abstract
Introduction
Although evidence-based, the 5A’s (Ask, Advise, Assess, Assist, and Arrange) for smoking cessation are often incompletely delivered by primary care providers. This study examines whether a computer tablet 5A’s intervention improves primary care provider adherence to the 5A’s.
Study design
Cluster RCT.
Setting/participants
All primary care providers in three urban, adult primary care clinics were randomized for participation. Any English- or Spanish-speaking patient with a primary care appointment who had smoked >100 lifetime cigarettes and at least one cigarette in the past week was eligible.
Intervention
A cluster RCT comparing computer-facilitated 5A’s with usual care assessed effects on provider adherence to each of the 5A’s as determined by patient report. Intervention subjects used a computer tablet to complete the 5A’s immediately before a primary care appointment. A tailored, patient handout and a structured, clinician guide were generated. Data were collected in 2014–2015 and analyzed in 2016–2017.
Main outcome measures
Provider adherence to the 5A’s.
Results
Providers (N=221) saw 961 patients (n=412 intervention, n=549 control) for a total of n=1,340 encounters with n=1,011 completed post-visit interviews (75.4% completion). Intervention providers had significantly higher odds of completing Assess (AOR=1.32, 95% CI=1.02, 1.73) and Assist (AOR=1.45, 95% CI=1.08, 1.94). When looking at first study visits only, intervention providers had higher odds for Arrange (AOR=1.72, 95% CI=1.23, 2.40) and all 5A’s (AOR=2.04, 95% CI=1.35, 3.07) but study visit did not influence receipt of the other 5A’s.
Conclusions
A computer-facilitated 5A’s delivery model was effective in improving the fidelity of provider-delivered 5A’s to diverse primary care patients. This relatively low-cost, time-saving intervention has great potential for smoking cessation and other health behaviors. Future studies should identify ways to promote and sustain technology implementation.
Trial Registration
clinicaltrials.gov identifier NCT02046408.
INTRODUCTION
Despite impressive progress in reducing the rates of adult smoking in the U.S. over the last 50 years, smoking currently accounts for approximately 480,000 U.S. deaths per year and nearly 15% of the population continues to smoke.1 Lower income and more vulnerable populations (e.g., people with severe mental illness or substance use disorders, and people who are uninsured or with Medicaid) smoke at rates exceeding 30%,2 and bear a disproportionate burden of tobacco-related disease.3 The majority of smokers would like to quit, with over half attempting to quit in any given year and 25% wanting to quit in the next 30 days.4,5 Although 70% of smokers have seen a healthcare provider in the past year,6 the large majority are not assessed for readiness to quit and do not receive cessation assistance.7,8
The U.S. Public Health Service recommends the gold-standard 5A’s for smoking cessation, where every medical provider Asks about smoking, Advises cessation, Assesses level of readiness to quit, Assists with motivation or a plan to quit (including use of tobacco cessation medication and counseling), and Arranges a follow-up appointment to review progress and adjust the plan.9 Multiple studies across diverse settings have shown that while most providers Ask and Advise, they often fail to Assess readiness (39%–63.4% prevalence) and Assist patients (38.6%–56.4%) and even more rarely Arrange a follow-up (2%–10.4%).7,8,10–12 The Assist step, with its focus on cessation aids and pharmacotherapy, has been shown to increase the odds of quitting by 40%.8 The Arrange step, which allows for treatment adjustments following relapse, has been associated with a 46% increase in the odds of quitting.8 Competing demands, time limitations, provider attitudes, and lack of self-efficacy are commonly cited reasons for provider nonadherence to the 5A’s.13
Provider training and electronic prompts have shown marginal improvements in 5A’s adherence, but studies have lacked rigor and no conclusive recommendations can be made.14–18 Computer-delivered screening and brief intervention have shown promise for smoking and other health behavior counseling while saving provider time and improving intervention quality,19–21 but technology acceptance and implementation have proven challenging and the impact on provider behavior is uncertain.22–24 Although many interventions can be delivered directly to patients with no provider involvement, sustaining patient adherence is a challenge and clinical outcomes may be less robust.25 Ideally, a technology-enabled intervention would provide evidence-based care while still including the expertise and proven social influence of the provider.26
The current study tests a computer tablet 5A’s intervention for tobacco use disorders delivered in waiting rooms just prior to a primary care appointment. The primary outcomes include provider delivery of each of the 5A’s and delivery of all 5A’s. Secondary outcomes include delivery of the 5A’s from any source (provider or tablet). As an implementation study of an established and effective clinical intervention, this effectiveness study focuses on increasing provider adherence and intervention fidelity rather than cessation outcomes among patients. The authors hypothesize that intervention patients will be more likely to receive Assist and Arrange from their providers and more likely to receive Assess, Assist, Arrange, and the complete 5A’s from either providers or the tablet.
METHODS
This cluster RCT investigated the effect of a computer-facilitated 5A’s program (CF5A’s) on primary care provider (PCP) behavior (see prior manuscript for a detailed description of the development of the CF5A’s intervention).27 Randomization took place at the level of the providers. Patients were assessed for eligibility prior to their PCP appointment and were assigned to CF5A’s or usual care based on their providers’ assignment. CF5A’s patients completed the first four A’s on the computer tablet, generating a tailored health handout for patients and a clinical guide for the provider. Patients were interviewed following their PCP appointment to assess provider adherence to the 5A’s. Data were collected in 2014–2015 and analyzed in 2016– 2017.
Study Population
Providers and patients were recruited from three diverse primary care clinics in the San Francisco Bay Area. Clinic 1 is a mid-size adult primary care clinic within a large academic health center. Clinic 1 follows ≅18,000 patients who make about 40,200 annual visits. Patients are ethnically diverse: 49% white, 24% Asian/Pacific Islander, 15% Latino, 11% African American, and 1% American Indian. The payer mix includes 34% managed care, 32% Medicare, 15% Medicaid, and 19% other. The estimated smoking prevalence is 12%.
Clinic 2 is operated by the City and County of San Francisco, and serves as the primary health care facility for San Francisco’s underserved and uninsured families. Clinic 2 follows ≅6,500 patients who make about 25,000 annual visits. Patients are ethnically diverse: 29% are Asian/Pacific Islander, 28% Latino, 20% white, 19% African American, and 4% other race or ethnicity. Payer mix includes 40% Medicaid, 31% Medicare, and 29% other (local, capitated programs). The estimated smoking prevalence is 17%.
Clinic 3 is an academic, hospital-based HIV primary care clinic also operated in partnership with the City and County of San Francisco. Clinic 3 follows nearly 3,000 people living with HIV/AIDS who make about 14,000 visits. Patients are ethnically diverse: 50.9% are white, 22.5% African American, 19% Latino, 5.4% Asian/Pacific Islander, and 2.2% other races. Payer mix includes: 53% Medicaid (and community capitated programs), 30% Medicare, and 16.5% other. The estimated smoking prevalence is 35%.
Study participants included both PCPs and their patients. All PCPs of any discipline (e.g., MD, DO, NP) and any training level (e.g., faculty, fellows, residents) at all three clinics were enrolled in the study. Providers did not have to provide consent to be enrolled and were randomized into the CF5A’s or usual care conditions. Demographic data on providers were pulled from existing clinic administrative records.
Study staff approached all patients in the waiting room to inform them about the study after they had checked in for their primary care appointment. Study staff screened interested participants for study eligibility and handed them a computer tablet to use in the waiting room. Patients provided informed consent to participate via the tablet. Tablets were returned to the study staff after use. Eligible patients were aged ≥18 years and English- or Spanish-speaking. Patients must have smoked >100 cigarettes in their lifetime and one cigarette in the past 7 days, and could be current daily or non-daily smokers. Patients could participate up to three times during the 12-month study period. This study was approved by the University of California San Francisco IRB. All patient participants were given a $20 gift card after completing each post-PCP visit interview.
Prior to the initiation of the trial, the statistician stratified the list of study providers by clinic site, provider type (attending, nurse practitioner, fellow, resident), provider sex, and provider percentage of effort in primary care. Each combination of strata constituted a block and a computer random number generator implemented block randomization with 1:1 allocation to the CF5A’s and usual care study arms. Just prior to the initiation of the trial, each provider was informed of his or her study arm assignment by the principal investigator. Patients were assigned to a study arm based on the provider they were seeing on the day of study enrollment. Study staff enrolled patients into the study and were blind to the identities of patients’ providers. At the time of enrollment, patients were blind to the study arm assigned to their provider. Randomization of providers was chosen because there were too few sites to randomize and randomization of patients would have resulted in providers treating patients in both study arms, risking intervention contamination.
The CF5A’s intervention followed the accepted protocols for Ask, Advise, Assess, Assist, and Arrange using branching logic to tailor the flow of the interaction based on patient responses. The tablet asked patients about their smoking, advised them to quit, and assessed their level of readiness to quit. Subsequent Assist interventions were based on the patient’s self-reported level of readiness using accepted motivational interviewing techniques. For example, pre-contemplative and contemplative patients completed an importance ruler and were guided through the 5R’s (Relevance, Risks, Rewards, Roadblocks, and Repetition) and decisional balance. Patients who were preparing to quit within the next month were asked about the presence of a plan, plan components, and level of confidence. Past–quit attempts and other successful behavior change examples were explored if confidence was low. If appropriate, patients were encouraged to set a quit date with their provider and to utilize other resources (e.g., quitlines, nicotine replacement therapy). All patients who received the CF5A’s intervention completed the protocols based on their level of readiness to quit and were encouraged to share their specific interests in discussing smoking cessation with their provider that day.
At the end of the tablet intervention, study staff printed out two tailored printouts, one for patients and one for providers. Patients received a summary of their responses, step-by-step instructions on enhancing motivation or promoting cessation, and instructions for follow-up care. Providers received a clinical summary with personalized risk and patient preference information, recommended next steps, and referral resources and pharmacotherapy instructions. These were delivered to the patient and provider in the clinic room prior to the visit. Both providers and patients were encouraged to share and discuss the information on their handouts and to schedule (Arrange) a follow-up visit.
Patients in the usual care condition completed eligibility screening (including being asked about smoking) and consent on the computer tablet. After sharing their contact information and contact preferences, usual care patients returned the computer tablet with no further intervention. An attentional control was not used (e.g., tablet-delivered education about a health concern) due to the potential for biasing the subsequent conversation with their PCP away from smoking.
Measures
Provider adherence to each of the 5A’s steps was the primary outcome. Provider adherence was assessed by asking patients whether they were asked about their tobacco use patterns (Ask), whether they were advised to quit (Advise), whether their willingness to quit was assessed (Assess), whether they were assisted in their quit attempt (if interested) or assisted in building motivation (if not interested in quitting; Assist), and (5) whether follow-up was arranged (Arrange). All questions were binary with yes/no answers (Appendix Table 1). Given the breadth of Assist options, a total of nine questions for Assist were used with any yes response considered as an Assist. An all 5A’s outcome indicated if patients received all five steps of the 5A’s. Patients were also asked whether they received any of the 5A’s intervention by the tablet. Patients were interviewed either in person immediately following their PCP appointment, or by telephone within 72 hours after their PCP appointment, based on their availability. Because patients were allowed to participate up to three times, primary outcomes first reflect all PCP visits and then examination of potential effects by visit number. To minimize attrition, study staff attempted to contact participants by telephone multiple times if they did not complete the post-visit questionnaire within 72 hours.
The secondary outcome examined whether delivery of the 5A’s to the patient took place by either the tablet or the provider. Although the conceptual model27 argues for the importance of including the provider, having the tablet (or any source) deliver the 5A’s could be an improvement over no intervention. Secondary outcomes were also assessed with the post-visit interview, where the authors examined self-reported receipt of the 5A’s from either the provider or the tablet.
Original assumptions included intention-to-treat analyses, 80% power, two-tailed α=0.05, N=1,526 enrolled patients with 80% completing a post-visit interview (n=1,221), an average of B=7.6 enrolled patients per provider with a post-visit interview, and tests of group differences in patient-reported 5A’s delivery at post-visit follow-up. In addition, the authors conservatively assumed one clinic visit per patient and case-wise deletion of missing data. For 5A’s delivery, the authors expected base rates equal to 70% (Advise), 60% (Assess), 50% (any Assist), and 10% (Arrange). The power analysis set-up had a three-level structure: sites, providers, and patients. Intra-site and intra–provider-and-site correlations were assumed to equal 0.05 (ρsite) and 0.10 (ρprov.site), respectively. Providers were the units of randomization and were nested within clinic sites; so, the study arm comparison incorporated both within- and between-cluster elements. The design effect estimate equaled 1.263=(1−ρsite)×(1+[B−1]×[ρprov.site−ρsite]), and the planned effective sample size at post-visit follow-up equaled 1,221/1.263=966, or n=483 per group. Minimum detectable effect sizes ranged from OR=1.44 (any Assist) to 1.72 (Arrange), suggesting good power. Power calculations were confirmed via simulation. Final analyses allowed for multiple visits per patient, which was expected to increase power.
Statistical Analysis
Simple statistics, including means and percentages, were calculated for all provider and patient demographic indicators. Intention-to-treat logistic regression models were fit to all study outcomes and included fixed effects of clinic sites, intervention groups, categorical indicator of patient visit (first, second, third), and a group X visit interaction effect. Preliminary three-level alternating logistic regressions (providers, patients, visits)28 suggested nonsignificant effects of provider-level clusters. Therefore, all final models were fit via generalized estimating equations, specifying patient-level clusters. Nonsignificant interaction effects were dropped and the corresponding models refit. Adjusting for race/ethnicity in the models did not substantively change findings, therefore the authors chose not to adjust for this variable. Each model was fit to 20 multiply imputed data sets created via a Markov chain Monte Carlo method29 using SAS PROC MI, SAS version 9.4. The imputation model included all modeled outcomes and predictors and only outcomes for attended visits were imputed. Imputed values for binary variables were subsequently rounded to the nearest applicable category.29 All parameter and SE estimates were calculated by combining results across the imputed data sets.30,31
RESULTS
A total of 272 PCPs were enrolled and randomized in the study (Clinic 1=124, Clinic 2=105, Clinic 3=43). There were 221 providers that had at least one patient enrolled over the 12-month study period (n=110 CF5A’s, n=111 usual care). There were 961 unique patients consented and seen for a first visit, ≅22.5% of the overall smoking population in the three clinics. A total of 275 patients participated a second time, and 104 participated for a third visit (total N=1,340 PCP visits with n=1,011 completed post-visit interviews [75.4%]; Figure 1 shows the Consort Diagram). Provider and patient demographics can be found in Table 1. Patients were racially diverse, low-income, and had limited educational attainment. Because of the demographic distributions of patients across providers, white patients were overrepresented in the usual care group and Latino/Hispanic and Asian patients were overrepresented in the CF5A’s condition. Providers were more likely to be female and in training.
Figure 1. CF5A’s RCT CONSORT diagram.
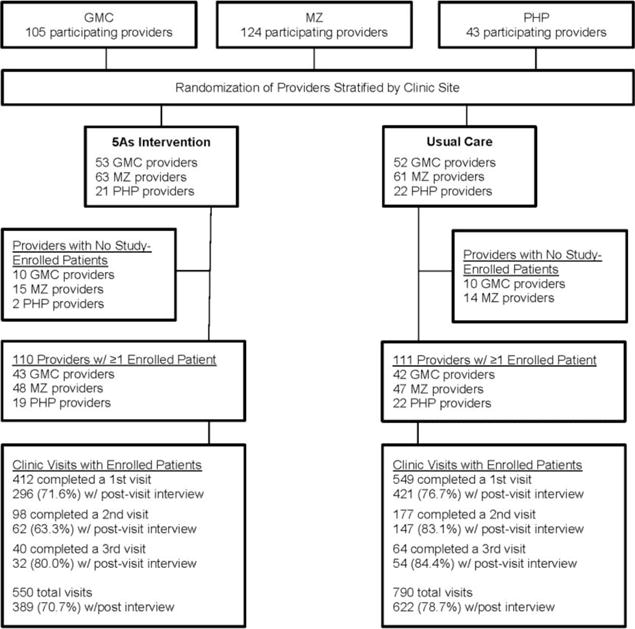
CF5A’s, Computer-facilitated 5A’s; GMC, General Medicine Clinic; MZ, Mount Zion; PHP, Positive Health Program
Table 1.
Provider and Patient Demographics
| Demographic variables | Intervention (%) n=110 |
Usual care (%) n=111 |
Total (%) N=221 |
|---|---|---|---|
| Provider | |||
| Female | 65 (59.1) | 66 (59.5) | 131 (59.3) |
| Male | 45 (40.9) | 45 (40.5) | 90 (40.7) |
| Faculty | 35 (31.8) | 40 (36) | 75 (33.9) |
| Resident/Fellow | 69 (62.7) | 65 (58.6) | 134 (60.6) |
| Other (NP) | 9 (8.2) | 6 (5.4) | 15 (6.8) |
| Mean % clinical effort | 11.5 | 13.5 | 12.5 |
| Patient | n=412 | n=549 | N=961a |
| Age, years (Mean) | 51 | 50 | 50.4 |
| Female | 139 (33.9) | 195 (35.7) | 334 (34.9) |
| Race/Ethnicityb | |||
| White | 118 (28.1) | 202 (37.2) | 320 (33.5) |
| African American | 160 (38.9) | 216 (39.7) | 376 (39.4) |
| Hispanic/Latino | 89 (21.6) | 81(14.9) | 170 (17.8) |
| Asian/PI | 24 (5.8) | 17 (3.1) | 41 (4.3) |
| Native American | 4 (1.0) | 9 (1.6) | 13 (1.4) |
| Other | 16 (3.9) | 18 (3.3) | 34 (3.6) |
| Education | |||
| High school or less | 195 (48.3) | 274 (51.2) | 469 (49.9) |
| Some college | 136 (33.7) | 176 (32.9) | 312 (33.2) |
| College degree | 73 (18.1) | 85 (15.9) | 158 (16.8) |
| Health insurance type | |||
| HMO/PPO | 30 (7.4) | 27 (5.0) | 57 (6.0) |
| Medicaid | 234 (58.1) | 330 (60.1) | 564 (59.6) |
| Medicare | 80 (19.8) | 118 (21.7) | 198 (20.9) |
| Uninsured | 4 (1.0) | 3 (0.6) | 7 (0.7) |
| Other | 55 (13.6) | 65 (12.0) | 120 (12.7) |
| Smoking status, Mean (SD) | |||
| Current cigarettes daily | 10.7 (8.4) | 10.2 (9.6) | 10.4 |
| Number of years smoked in lifetime | 27.7 (14.4) | 28 (14.2) | 27.9 |
| Time to first cigarette (%)c | |||
| <30 minutes | 165 (55.9) | 251 (59.6) | 416 (58.1) |
| Readiness to quit (%) | |||
| Pre-contemplation | 46 (15.6) | 70 (16.6) | 116 (12.1) |
| Contemplation | 131 (44.4) | 184 (43.7) | 315 (44.0) |
| Preparation | 88 (29.8) | 110 (26.1) | 198 (27.6) |
| Action | 12 (4.1) | 24 (5.7) | 36 (5.0) |
| Don’t know/Refused | 18 (6.1) | 33 (7.8) | 51 (7.1) |
Sample size varied slightly per item due to missing data.
No significant differences between intervention and usual care after adjusting for provider clusters. Wald Chi square test: F(5, 205)=1.98, p=0.0829.
Assessed after the primary care visit for the usual care group.
PPO, Preferred provider organization
After adjusting for clustering effects across all study visits, there were no significant group differences in PCP 5A’s behavior for Ask, Advise, Arrange, or for the complete 5A’s. CF5A’s patients had 32% higher odds of receiving Assess (AOR=1.32, 95% CI=1.02, 1.72) and 45% higher odds of receiving any Assist (AOR=1.45, 95% CI=1.08, 1.94) from their PCP (Table 2). When looking at first study visits only, CF5A’s patients had 72% higher odds of receiving Arrange (AOR=1.72, 95% CI=1.23, 2.40) and 104% higher odds of receiving all 5A’s (AOR=2.04, 95% CI=1.35, 3.07) compared with usual care. Visit number was not a significant predictor for any other outcomes.
Table 2.
GEE Analysis of Patient-Reported Outcomes Describing Provider-Delivery of 5A’s
| Intervention vs usual carea | Intervention % | Usual care % | AOR (95% CI) | p-value |
|---|---|---|---|---|
| ASK-Prov | 59.7 | 55.0 | 1.21 (0.93, 1.57) | 0.156 |
| ADVISE-Prov | 57.0 | 51.1 | 1.26 (0.96, 1.66) | 0.091 |
| ASSESS-Prov | 56.8 | 49.9 | 1.32 (1.01, 1.72) | 0.037 |
| ASSIST-Prov | 62.9 | 53.9 | 1.45 (1.08, 1.93) | 0.012 |
| ARRANGEb-Prov (visit-averaged) | 20.0 | 22.2 | 0.87 (0.53, 1.44) | 0.596 |
| Visit 1 | 28.2 | 18.6 | 1.72 (1.23, 2.40) | 0.002 |
| Visit 2 | 20.8 | 20.9 | 0.99 (0.50, 1.97) | 0.981 |
| Visit 3 | 13.2 | 28.0 | 0.39 (0.12, 1.31) | 0.127 |
| All 5A’sc – Prov (visit-averaged) | 12.0 | 13.6 | 0.86 (0.47, 1.59) | 0.641 |
| Visit 1 | 17.9 | 9.7 | 2.04 (1.35, 3.07) | 0.001 |
| Visit 2 | 12.2 | 13.9 | 0.86 (0.39, 1.89) | 0.701 |
| Visit 3 | 7.8 | 18.6 | 0.37 (0.09, 1.53) | 0.169 |
Note: Boldface indicates statistical significance (p<0.05). N=961 patients with n=1,340 visits.
Odds of self-reported receipt of 5A’s in the intervention group compared to usual care group.
Group-by-visit interaction p-value=0.023.
Group-by-visit interaction p-value=0.021.
GEE, generalized estimating equation; 5A’s, Ask, Advise, Assess, Assist, and Arrange; Prov, Provider
Across all study visits, patients in the CF5A’s condition were significantly more likely to receive Ask, Advise, Assess, and Assist from either their PCP or the computer tablet in comparison with usual care group patients. CF5A’s patients were also more likely to receive all 5A’s from any source compared with usual care, but only for the first visit (Table 3).
Table 3.
GEE Analysis of Patient-Reported Outcomes Describing Provider and/or Tablet-Delivery of 5A’sa
| Intervention vs usual careb | Intervention % | Usual care % | AOR (95% CI) |
p-value |
|---|---|---|---|---|
| ASK-P/T | 83.7 | 76.6 | 1.57 (1.07, 2.31) | 0.021 |
| ADVISE-P/T | 69.8 | 57.2 | 1.73 (1.30, 2.30) | 0.0002 |
| ASSESS-P/T | 78.9 | 61.0 | 2.39 (1.82, 3.14) | <0.0001 |
| ASSIST-P/T | 83.6 | 59.8 | 3.43 (2.43, 4.84) | <0.0001 |
| All 5A’s c- P/T (visit-averaged) | 13.2 | 14.4 | 0.90 (0.47, 1.70) | 0.739 |
| Visit 1 | 21.7 | 10.9 | 2.26 (1.52, 3.36) | <0.0001 |
| Visit 2 | 12.3 | 14.1 | 0.85 (0.36, 2.02) | 0.719 |
| Visit 3 | 8.2 | 19.2 | 0.38 (0.09, 1.59) | 0.182 |
Note: Boldface indicates statistical significance (p<0.05). N=961 patients with n=1,340 visits.
ARRANGE outcomes were not included as the tablet was not programmed to perform an ARRANGE step.
Odds of self-reported receipt of 5A’s by either the provider and/or tablet in the intervention group compared to provider-delivered 5A’s in the usual care group.
Group-by-visit interaction p-value=0.011.
GEE, generalized estimating equation; 5A’s, Ask, Advise, Assess, Assist, and Arrange; P/T, Provider and/or tablet
DISCUSSION
A CF5A’s intervention increased provider adherence to the 5A’s clinical guideline for tobacco use disorders in the intervention compared with the usual group. Rates of receipt of the 5A’s were within the ranges observed in previous studies, with the exception of the Arrange intervention, which was much higher in this study in both intervention and control groups than what has been previously reported.8 Across all visits, intervention providers were more likely to Assess and Assist their patients with smoking cessation when compared with usual care providers. For first visits, intervention providers were also more likely to Arrange a follow-up and to deliver all 5A’s. Not surprisingly, more dramatic and consistent differences were seen between intervention and usual care conditions when the source of the 5A’s was expanded to include either providers or the computer tablets. This study differs from prior 5A’s intervention studies by creating a hybrid, digital delivery system and tailored clinical decision aid rather than relying on more traditional continuing education interventions or reminders,14,15,18 and by its focus on provider behavior rather than clinical outcomes.21 Moreover, patients were actively engaged and empowered by the technology and the personalized report they received prior to their PCP appointment.
Given the established body of evidence in support of the 5A’s8–10 for smoking cessation, provider adherence to these guidelines was the focus of the present study. The 5A’s intervention was a known clinical guideline in each of the study clinics, suggesting it had been partially implemented already.11,32 Prior work in the same clinics demonstrated that provider adherence to the 5A’s was poor, suggesting suboptimal care for patients who smoke.11 Both providers and staff expressed a lack of confidence in their ability to provide behavior change counseling and expressed an interest in additional training and clinical decision tools that could be used at the point of care. Clinicians noted a perceived lack of smoking cessation resources and indicated that referral assistance and resource recommendations would be helpful.32 The CF5A’s intervention was specifically designed to address some of these barriers. The provider handout had information that was specific to the needs of the patient based on his or her motivation to quit. The handout also had readily accessible information on referral resources and guidance on prescribing pharmacotherapy, intended to guide patient–provider discussion around smoking cessation.
The CF5A’s intervention was iteratively developed using provider and patient needs and preferences.27,32,33 Although the tablets were successful in delivering the 5A’s and in improving provider adherence, the implementation of the technology was challenging, and ongoing support was needed from research staff. In a related study, the authors elicited attitudes and preferences regarding technology adoption in the same clinics where they conducted the intervention and found that, perceived ease of use of technology was dependent on the clinic’s ability to accommodate a digital intervention.32,33 Interruptions to clinic workflow, heavy patient volume, perceived importance of smoking cessation relative to patients’ other priorities, and implementing digital technology interventions that are unlinked with the electronic health records were some of the factors that influenced perceptions around the use of digital technology interventions. Other digital health reviews have focused on similar factors.34–36 Further research is needed on how to best promote the adoption and sustained implementation of digital health technologies, particularly in overburdened health care systems. Future studies might also explore the integration of digital health interventions in situations within existing hardware and digital workflows (e.g., electronic health records, clinical dashboards) that have already been established and proven effective in other studies.37,38
The limited but significant findings with visit number raise important possibilities when considering longitudinal behavior change interventions. Stronger results (more Arrange and more complete 5A’s delivered by the provider) were seen in the first primary care visit only. Although the lower provider 5A’s adherence in the second and third visits could be because of random factors or a smaller sample size, it could also reflect the challenges of repeating interventions in a primary care setting already overloaded with clinical tasks. In reality, behavior change is often slow and requires multiple repetitions and ongoing support in order to be successful.39 Although cessation success is enhanced with provider involvement,9,40 it is probably not realistic to expect all follow-up and continuing support to come only from the provider. Redesigning clinical workflows for behavior change interventions using team-based practice and newer integrated behavioral health models could improve and extend the behavior change gains made in earlier visits.41 Digital tools employed by and coordinated across the healthcare team warrant further attention and research.
Limitations
The present study has several limitations. First, the primary outcome was patient-reported receipt of the 5A’s rather than an audio recording of each primary care conversation, potentially leading to recall bias. Given the impracticality of recording so many primary care visits, the remaining possible data sources were patient self-report, provider report, and chart review. Provider reports have been shown to overestimate adherence to practice guidelines and have little correlation to electronic health record documentation.42,43 Chart reviews have been seen as the least reliable given inconsistencies in charting, which often underestimate provider behaviors.43,44 Although patient report is also imperfect, comparisons of direct observations with patient report show that most smokers correctly recall smoking cessation advice45 and a systematic review comparing chart review, provider report, and patient report found the strongest support for the use of patient report as a proxy for clinical behavior.44
Although the patient sample was highly diverse, and many were from traditionally underserved populations, white patients were overrepresented in the usual care condition and Hispanic and Asian patients were overrepresented in the intervention condition. Racial/ethnic minority groups are less likely to report receipt of cessation counseling; thus, intervention effects could potentially be attenuated.46 The findings are more generalizable to urban, low-income populations that carry a disproportionate burden of tobacco use. Furthermore, despite aggressive attempts at follow-up, nearly a quarter of the sample did not complete a post-visit interview. Common reasons included disconnected phones, missed calls, and unanswered voicemails. Patients were given the option of an in-person interview immediately after their PCP visit, but many had subsequent visits or other commitments.
CONCLUSIONS
Using a “clinician–extender” technology model, a CF5A’s intervention was effective in increasing 5A’s delivery to patients and provider behavior in the intervention group compared with the usual care group. Although the adoption and sustainability of digital tools remains a challenge, the clinician–extender approach offers promise in effectively and efficiently delivering a large number of behavioral health interventions. A conceptual framework has been proposed consisting of four steps along a continuum of using digital tools for health care to improve provider delivery of and patient receipt of the intervention: (1) provider interventions alone; (2) provider interventions with digital adjuncts; (3) digital tools with human guidance, not necessarily from professional providers; and (4) totally automated digital tools with no human guidance.47 The current study illustrates the second of these steps. Adding Steps 3 and 4, that is, evidence-based smoking cessation digital tools,48 to the list of potential smoking cessation services suggested to smokers could provide a seamless extension of computer-facilitated services to patients. Future scale-up studies should address technical and implementation obstacles to reach larger populations more quickly and improve clinical care.
Supplementary Material
Acknowledgments
We would like to acknowledge the clinical and administrative staff in each of our study clinics, our research coordinators, and our many volunteer assistants and clinic staff who worked so diligently supporting patient engagement and the investigative process. Phreesia, Inc. generously contributed tablet hardware, programming, and ongoing technical support. Project funding provided by NIH/National Institute for Drug Abuse grant R01DA034253.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults – United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65(44):1205–1211. doi: 10.15585/mmwr.mm6544a2. https://doi.org/10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- 2.Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults – United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2015;64(44):1233–1240. doi: 10.15585/mmwr.mm6444a2. https://doi.org/10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- 3.CDC. Smoking rates for uninsured and adults on Medicaid more than twice those for adults with private health insurance. www.cdc.gov/media/releases/2015/p1112-smoking-rates.html. Accessed August 23, 2016.
- 4.Burris JL, Wahlquist AE, Carpenter MJ. Characteristics of cigarette smokers who want to quit now versus quit later. Addict Behav. 2013;38(6):2257–2260. doi: 10.1016/j.addbeh.2013.02.008. https://doi.org/10.1016/j.addbeh.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babb S, Malarcher A, Schauer G, Asman K, Jamal A. Quitting smoking among adults – United States, 2000–2015. MMWR Morb Mortal Wkly Rep. 2017;65(52):1457–1464. doi: 10.15585/mmwr.mm6552a1. https://doi.org/10.15585/mmwr.mm6552a1. [DOI] [PubMed] [Google Scholar]
- 6.Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev Chronic Dis. 2014;11:E131. doi: 10.5888/pcd11.140053. https://doi.org/10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruger J, O’Halloran A, Rosenthal AC, Babb SD, Fiore MC. Receipt of evidence-based brief cessation interventions by health professionals and use of cessation assisted treatments among current adult cigarette-only smokers: National Adult Tobacco Survey, 2009–2010. BMC Public Health. 2016;16:141. doi: 10.1186/s12889-016-2798-2. https://doi.org/10.1186/s12889-016-2798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park ER, Gareen IF, Japuntich S, et al. Primary care provider-delivered smoking cessation interventions and smoking cessation among participants in the National Lung Screening Trial. JAMA Intern Med. 2015;175(9):1509–1516. doi: 10.1001/jamainternmed.2015.2391. https://doi.org/10.1001/jamainternmed.2015.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fiore MC, Jaén CR, Baker T, et al. Clinical Practice Guideline. Rockville, MD: U.S DHHS, Public Health Service; 2008. Treating Tobacco Use and Dependence: 2008 Update. Published. [Google Scholar]
- 10.Quinn VP, Hollis JF, Smith KS, et al. Effectiveness of the 5-As tobacco cessation treatments in nine HMOs. J Gen Intern Med. 2009;24(2):149–154. doi: 10.1007/s11606-008-0865-9. https://doi.org/10.1007/s11606-008-0865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vijayaraghavan M, Yuan P, Gregorich S, et al. Disparities in receipt of 5As for smoking cessation in diverse primary care and HIV clinics. Prev Med Rep. 2017;6:80–87. doi: 10.1016/j.pmedr.2017.02.012. https://doi.org/10.1016/j.pmedr.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams RJ, Masica AL, McBurnie MA, et al. Documentation of the 5As for smoking cessation by PCPs across distinct health systems. Am J Manag Care. 2014;20(3):e82–e89. [PMC free article] [PubMed] [Google Scholar]
- 13.Marcy TW, Skelly J, Shiffman RN, Flynn BS. Facilitating adherence to the tobacco use treatment guideline with computer-mediated decision support systems: Physician and clinic office manager perspectives. Prev Med. 2005;41(2):479–487. doi: 10.1016/j.ypmed.2004.11.026. https://doi.org/10.1016/j.ypmed.2004.11.026. [DOI] [PubMed] [Google Scholar]
- 14.McCullough A, Fisher M, Goldstein AO, Kramer KD, Ripley-Moffitt C. Smoking as a vital sign: Prompts to ask and assess increase cessation counseling. J Am Board Fam Med. 2009;22(6):625–632. doi: 10.3122/jabfm.2009.06.080211. https://doi.org/10.3122/jabfm.2009.06.080211. [DOI] [PubMed] [Google Scholar]
- 15.Caplan L, Stout C, Blumenthal DS. Training physicians to do office-based smoking cessation increases adherence to PHS guidelines. J Community Health. 2011;36(2):238–243. doi: 10.1007/s10900-010-9303-0. https://doi.org/10.1007/s10900-010-9303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McElwaine KM, Freund M, Campbell EM, Bartlem KM, Wye PM, Wiggers JH. Systematic review of interventions to increase the delivery of preventive care by primary care nurses and allied health clinicians. Implement Sci. 2016;11:50. doi: 10.1186/s13012-016-0409-3. https://doi.org/10.1186/s13012-016-0409-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Strayer SM, Heim SW, Rollins LK, et al. Improving smoking cessation counseling using a point-of-care health Intervention Tool (IT): From the Virginia Practice Support and Research Network (VaPSRN) J Am Board Fam Med. 2013;26(2):116–125. doi: 10.3122/jabfm.2013.02.110078. https://doi.org/10.3122/jabfm.2013.02.110078. [DOI] [PubMed] [Google Scholar]
- 18.Payne TJ, Gaughf NW, Sutton MJ, et al. The impact of brief tobacco treatment training on practice behaviours, self-efficacy and attitudes among healthcare providers. Int J Clin Pract. 2014;68(7):882–889. doi: 10.1111/ijcp.12386. https://doi.org/10.1111/ijcp.12386. [DOI] [PubMed] [Google Scholar]
- 19.Ondersma SJ, Grekin ER, Svikis D. The potential for technology in brief interventions for substance use, and during-session prediction of computer-delivered brief intervention response. Subst Use Misuse. 2011;46(1):77–86. doi: 10.3109/10826084.2011.521372. https://doi.org/10.3109/10826084.2011.521372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Portnoy DB, Scott-Sheldon LAJ, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: A meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47(1):3–16. doi: 10.1016/j.ypmed.2008.02.014. https://doi.org/10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unrod M, Smith M, Spring B, DePue J, Redd W, Winkel G. Randomized controlled trial of a computer-based, tailored intervention to increase smoking cessation counseling by primary care physicians. J Gen Intern Med. 2007;22(4):478–484. doi: 10.1007/s11606-006-0069-0. https://doi.org/10.1007/s11606-006-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garavand A, Mohseni M, Asadi H, Etemadi M, Moradi-Joo M, Moosavi A. Factors influencing the adoption of health information technologies: A systematic review. Electron Physician. 2016;8(8):2713–2718. doi: 10.19082/2713. https://doi.org/10.19082/2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ketikidis P, Dimitrovski T, Lazuras L, Bath PA. Acceptance of health information technology in health professionals: An application of the revised technology acceptance model. Health Informatics J. 2012;18(2):124–134. doi: 10.1177/1460458211435425. https://doi.org/10.1177/1460458211435425. [DOI] [PubMed] [Google Scholar]
- 24.Trick WE, Deamant C, Smith J, Garcia D, Angulo F. Implementation of an Audio Computer- Assisted Self-Interview (ACASI) system in a general medicine clinic patient response burden. Appl Clin Inform. 2015;6(1):148–162. doi: 10.4338/ACI-2014-09-RA-0073. https://doi.org/10.4338/ACI-2014-09-RA-0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dickinson WP, Glasgow RE, Fisher L, et al. Use of a website to accomplish health behavior change: If you build it, will they come? And will it work if they do? J Am Board Fam Med. 2013;26:168–176. doi: 10.3122/jabfm.2013.02.110344. https://doi.org/10.3122/jabfm.2013.02.110344. [DOI] [PubMed] [Google Scholar]
- 26.Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2008;(2):CD000165. doi: 10.1002/14651858.CD000165.pub3. https://doi.org/10.1002/14651858.CD000165.pub3. [DOI] [PubMed]
- 27.Kalkhoran S, Appelle NA, Napoles AM, et al. Beyond the Ask and Advise: Implementation of a computer tablet intervention to enhance provider adherence to the 5As for smoking cessation. J Subst Abuse Treat. 2016;60:91–100. doi: 10.1016/j.jsat.2015.05.009. https://doi.org/10.1016/j.jsat.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carey V, Zeger SL, Diggle P. Modelling multivariate binary data with alternating logistic regressions. Biometrika. 1993;80(3):517–526. https://doi.org/10.1093/biomet/80.3.517. [Google Scholar]
- 29.Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. https://doi.org/10.1201/9781439821862. [Google Scholar]
- 30.Meng XL, Rubin DB. Performing likelihood ratio tests with multiply-imputed data sets. Biometrika. 1992;79(1):103–111. https://doi.org/10.1093/biomet/79.1.103. [Google Scholar]
- 31.Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987. https://doi.org/10.1002/9780470316696. [Google Scholar]
- 32.Nápoles AM, Appelle N, Kalkhoran S, Vijayarghavan M, Alvarado N, Satterfield J. Perceptions of clinicians and staff about the use of digital technology in primary care: Qualitative interviews prior to implementation of a computer-facilitated 5A’s intervention. BMC Med Inform Decis Mak. 2016;16:44–57. doi: 10.1186/s12911-016-0284-5. https://doi.org/10.1186/s12911-016-0284-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Holden RJ, Karsh BT. The Technology Acceptance Model: Its past and its future in health care. J Biomed Inform. 2010;43(1):159–172. doi: 10.1016/j.jbi.2009.07.002. https://doi.org/10.1016/j.jbi.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: Evidence review and recommendations for future research in mental health. Gen Hosp Psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. https://doi.org/10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsey A. Integration of technology-based behavioral health interventions in substance abuse and addiction services. Int J Ment Health Addict. 2015;13(4):470–480. doi: 10.1007/s11469-015-9551-4. https://doi.org/10.1007/s11469-015-9551-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sciamanna CN, Marcus BH, Goldstein MG, et al. Feasibility of incorporating computer-tailored health behaviour communications in primary care settings. Inform Prim Care. 2004;12(1):40–48. doi: 10.14236/jhi.v12i1.107. [DOI] [PubMed] [Google Scholar]
- 37.Smith BK, Adsit RT, Jorenby DE, Matsumura JS, Fiore MC. Utilization of the electronic health record to improve provision of smoking cessation resources for vascular surgery inpatients. Int J Cardiovasc Res. 2015;4(5) doi: 10.4172/2324-8602.1000231. https://doi.org/10.4172/2324-8602.1000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levine LD, Chang J, Merkatz IR, Bernstein PS. Enhanced physician prompts in prenatal electronic medical records impact documentation on smoking cessation. Open J Obstet Gynecol. 2013;3(10):717–721. doi: 10.4236/ojog.2013.310132. https://doi.org/10.4236/ojog.2013.310132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6(6):e011045. doi: 10.1136/bmjopen-2016-011045. https://doi.org/10.1136/bmjopen-2016-011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stead LF, Perera R, Lancaster T. A systematic review of interventions for smokers who contact quitlines. Tob Control. 2007;16(suppl 1):i3–i8. doi: 10.1136/tc.2006.019737. https://doi.org/10.1136/tc.2006.019737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crowley RA, Kirschner N. The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: Executive summary of an American College of Physicians position paper. Ann Intern Med. 2015;163(4):298–299. doi: 10.7326/M15-0510. https://doi.org/10.7326/M15-0510. [DOI] [PubMed] [Google Scholar]
- 42.Adams AS, Soumerai SB, Lomas J, Ross-Degnan D. Evidence of self-report bias in assessing adherence to guidelines. Int J Qual Health Care. 1999;11(3):187–192. doi: 10.1093/intqhc/11.3.187. https://doi.org/10.1093/intqhc/11.3.187. [DOI] [PubMed] [Google Scholar]
- 43.Conroy MB, Majchrzak NE, Silverman CB, et al. Measuring provider adherence to tobacco treatment guidelines: A comparison of electronic medical record review, patient survey, and provider survey. Nicotine Tob Res. 2005;7(suppl 1):S35–S43. doi: 10.1080/14622200500078089. https://doi.org/10.1080/14622200500078089. [DOI] [PubMed] [Google Scholar]
- 44.Hrisos S, Eccles MP, Francis JJ, et al. Are there valid proxy measures of clinical behaviour? A systematic review. Implement Sci. 2009;4:37. doi: 10.1186/1748-5908-4-37. https://doi.org/10.1186/1748-5908-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flocke SA, Stange KC. Direct observation and patient recall of health behavior advice. Prev Med. 2004;38(3):343–349. doi: 10.1016/j.ypmed.2003.11.004. https://doi.org/10.1016/j.ypmed.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 46.Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev Chronic Dis. 2014;11:140053. doi: 10.5888/pcd11.140053. https://doi.org/10.5888/pcd11.140053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Muñoz R. The efficiency model of support and the creation of digital apothecaries. Clin Psychol Sci Pract. 2017;24(1):46–49. https://doi.org/10.1111/cpsp.12174. [Google Scholar]
- 48.Muñoz RF, Bunge EL, Chen K, et al. Massive open online interventions: A novel model for delivering behavioral-health services worldwide. Clin Psychol Sci. 2016;4(2):194–205. https://doi.org/10.1177/2167702615583840. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


