Abstract
Prosthetic joint infection due to Salmonella spp is rare. Here we report an acute case of Salmonella enteritidis infection of a total hip arthroplasty in a man taking immunosuppressant medication. He was managed with antibiotics and two-stage revision surgery.
Keywords: bone and joint infections, orthopaedics, salmonella
Background
The number of total hip replacements performed in the UK is increasing every year. In 2016 alone, 64 844 hip replacements were carried out.1 Hip replacement helps to restore quality of life to our ageing population by relieving pain, aiding mobility and restoring independence.2 For these benefits to be experienced by patients, the risk of postoperative complications should be low. Postoperative infection in the replacement joint is one of the most serious complications, and it not only undermines the success of the surgery but also results in additional surgical procedures, healthcare costs and is associated with a significant morbidity and in some cases even mortality.3 Infection rates are now lower than when joint replacement was first introduced but still remain around 1%–2% for elective hip arthroplasties.4
The literature describes two main pathogens as the major contributors of infected hip arthroplasties; Staphylococcus aureus (41% of infections in 2011) and coagulase negative Staphylococci (31% of infections in 2011).3 Others include Enterococcus spp (12%) and Escherichia coli, Enterobacter spp, Pseudomonas spp and Streptococci (7% each).3
The incidence of Salmonella spp infections in a prosthetic joint is less than 1%.3 5 Here we describe a case of early Salmonella enteritidis infection in a prosthetic hip joint. To the best of our knowledge, this is the first case of Salmonella enteritidis infection treated with a two-stage revision in the UK.
Case presentation
A 58-year-old man underwent an uncemented right total hip replacement with a Furlong hydroxyapatite (HA)-coated uncemented stem and acetabular cup (Manufactured by JRI Orthopaedics) with ceramic-on-ceramic bearing surface to treat severe osteoarthritis (figures 1 and 2). Premorbid Oxford Hip Score was 13, and on University of California at Los Angeles (UCLA) Physical Activity Scale, he had fair scores.6 His other comorbidities included multiple sclerosis for which he was taking dimethyl fumarate, an immunosuppressant and disease-modifying drug used in relapsing and remitting multiple sclerosis. His procedure was uneventful, and he was discharged with low molecular weight heparin for deep vein thrombosis prophylaxis. He was fully weight bearing on discharge.
Figure 1.
Plain radiograph of the pelvis showing severe osteoarthritis of the right hip.
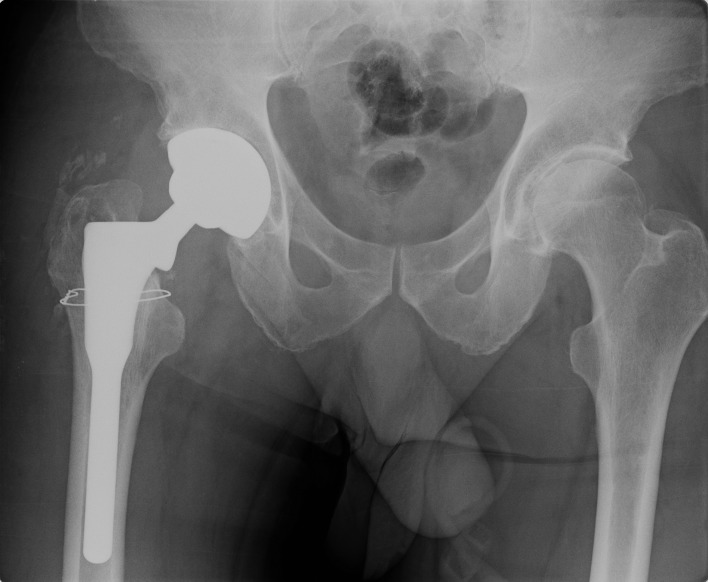
Figure 2.
Plain radiograph of the infected right hip replacement at the time of presentation to hospital.
The patient presented to the accident and emergency department on ninth postoperative day with 2-day history of severe right hip pain, fever and rigors. On examination, he was feverish with a temperature of 38.6°C and tachycardic with a heart rate of 102 beats per minute. His right hip surgical wound was erythematous with serosanguinous ooze. Blood tests showed C-reactive protein (CRP) of 287 mg/L and a white cell count (WCC) of 14.2×109/L. Antibiotic treatment was not started until after intraoperative specimens could be taken. His dimethyl fumarate was stopped.
He underwent debridement, antibiotics and implant retention (DAIR procedure) of his right hip on the 10th day after primary surgery. Intraoperative findings included 10 mL of haematoma collection between the subcutaneous fat and fascia lata which was communicating to hip. A wound swab from the collection and five tissue specimens from hip were collected for culture and sensitivity testing. The fascia lata was opened to ensure there was no distal communication of the haematoma, and this region was thoroughly debrided and washed out with 6 L of saline. Following discussion with microbiologist while awaiting culture and sensitivity reports, it was decided to commence intravenous gentamicin (5 mg/kg) once daily dose alongside intravenous teicoplanin (400 mg/12 hours). Patient developed a subtle sensorineural hearing loss during this intravenous antibiotic treatment. After discussion with microbiologist and patient the risks of persistant infection while avoiding hearing loss, a consensus was arrived to discontinue gentamicin after 5 days.
Following hip DAIR procedure, the patient did not improve. He continued to be feverish, and the wound was still discharging. He was discussed at the multidisciplinary meeting involving the microbiologist and other orthopaedic surgeons. Prior to his DAIR procedure, the patient was on dimethyl fumarate which might have probably caused him not to respond. On seventh day after his DAIR procedure, the patient underwent a first-stage revision of his right hip. Significant necrosis of the tissue with serosanguinous collection between subcutaneous fat and fascia lata and also between the fascia lata and muscle layer was found. A radical debridement was performed, and a size 54 spacer containing vancomycin and gentamicin was inserted (figure 3).
Figure 3.
Plain radiographs of the right hip after first-stage revision with removal of implants and insertion of a cement spacer.
All five tissue samples from the right hip taken during the DAIR procedure grew Salmonella enteritidis- subspecies I. The results were derived by whole genome sequencing. The isolated organism demonstrated sensitivity to amoxicillin/ampicillin, ciprofloxacin and gentamicin. All blood culture samples taken yielded no growth after 5 days of incubation, and three stool samples were taken which were all negative for Salmonella spp.
Multidisciplinary team meeting consisting of consultant microbiologist, community nurses, physiotherapists and consultant orthopaedic surgeons was held. Patient’s comorbidities and microbiology sample sensitivities were discussed. He was commenced on oral ciprofloxacin (500 mg/12 hours) for a total of 6 weeks as per microbiologist’s advice.
Following positive tissue cultures, the patient was further enquired about any recent gastrointestinal symptoms. He revealed that 2 months prior to surgery he had been on holiday to Indonesia where he experienced 5 days of abdominal pain and diarrhoea and treated himself with two doses of oral ciprofloxacin 500 mg. He also reported that his chronic right hip pain had worsened throughout his holiday. None of this was known prior to his hip replacement, and he was completely asymptomatic at the time of his elective surgery. During preoperative assessment prior to surgery, his inflammatory markers—CRP level was 2 mg/L and WCC was 4.6×109/L, which were all within the normal range.
Outcome and follow-up
Three months later, the patient finally underwent a second-stage revision for his right hip with Furlong HA-coated uncemented stem and acetabular cup (figure 4). During the second stage of revision surgery, there was minimal loss of metaphyseal cancellous bone and an intact femur diaphysis, so a primary design stem providing good primary stability was used.7 8 The procedure was uneventful, and intraoperatively, the tissues were found to be very healthy and vascular. Five repeat tissue specimens were sent for culture and sensitivity from various sites. None of these repeat samples showed any sign of residual infection. He went on to make a good recovery with no further evidence of infection. At the 8-month follow-up, his Oxford Hip Score was 39. On UCLA Activity Scale, he had an excellent score, and his Harris Hip Score was 100%. At the 18-month follow-up, he continued to have good outcome with an Oxford Hip Score of 48. On the UCLA Activity Scale, he had an excellent score, and his Harris Hip Score was 100%. There were no concerns of infection, and the radiograph of the hip was satisfactory (figure 5).
Figure 4.
Plain radiographs of the right hip after second-stage revision with Furlong hydroxyapatite-coated uncemented prosthesis.
Figure 5.
Plain radiographs of the right hip at 18 months’ follow-up.
Discussion
Salmonella is a genus of rod-shaped (bacillus) gram-negative bacteria of the Enterobacteriaceae family. Salmonella spp are one of the most common causes of food poisoning worldwide.9 10 Symptoms include abdominal pain and diarrhoea and last between 4 and 7 days.10 Although the most common presentation of salmonellosis is gastroenteritis, a bacteraemia may occur with this pathogen. Septic arthritis following Salmonella bacteraemia is rare and is usually seen in immune-compromised patients or patients with pre-existing significant underlying medical conditions; in this case report, the patient was on immunosuppressant drug to treat multiple sclerosis.10–12 Salmonella enteritidis described in this case is a non-typhoid serovar of Salmonella enterica and was the most common strain of Salmonella in UK between 2000 and 2010.12 13
Salmonellosis in humans is generally contracted through the consumption of contaminated food of animal origin; however, person to person transmission can also occur through the faecal–oral route.10 Countries have seen rates of infection rise over the last decade, likely due to increased global travel, and Salmonella enteritidis is the most commonly reported serotype among travel-associated non-typhoid Salmonella infections.13–15
Salmonella prosthetic joint infections are extremely rare. A recent review of the literature in 2012 reported only 29 cases of infection in prosthetic hip and knee joints worldwide.9 The majority of cases found in the literature were late infections in patients with significant underlying disease or risk factors, although Salmonella enteritidis was the most commonly reported strain.9 To the best of our knowledge, we present the only case of early Salmonella enteritidis infection in a total hip arthroplasty reported in the UK.
Existing literature explains how prosthetic joint infections can occur via direct inoculation during surgery (usually Staphylococcus and Streptococcus infections); however, Salmonella is not considered to be an intraoperative contaminant during joint replacement surgery.14 15 Salmonella joint infections usually occur via haematological seeding into the vulnerable joint, in this case a total hip arthroplasty.14 15 The clinical history of our patient supports the theory of haematogenous spread (along with negative stool cultures on more than one occasion); however, this case is slightly unusual in that the patient suffered gastroenteritis weeks prior to surgery and not postoperatively. This suggests that despite taking a course of antibiotics while on holiday in an attempt to treat his diarrhoea, he had either seeding in his arthritic hip prior to surgery or subclinical Salmonella bacteraemia at the time of surgery. The majority of these infections are in patients who suffer a gastrointestinal infection postoperatively which can lead to seeding into the new prosthetic joint.15 This case highlights the importance of preoperative consultation and fully exploring any recent illness or foreign travel. Our hospital has now added questions regarding recent travel or gastrointestinal illness to their preoperative questionnaire for total hip replacement surgery.
Lymphopenia is a known and common adverse effect with dimethyl fumarate.16 The patient was on dimethyl fumarate for management of his multiple sclerosis. Lymphopenia was ruled out prior to his primary total hip replacement.
Ciprofloxacin is effective for the treatment of Salmonella prosthetic joint infection, due to the ability of this class of drugs to kill not only rapidly growing bacteria, but also those bacteria that are in a stationary phase and adherent to the prosthetic material.11 17 Orally administered ciprofloxacin has high bioavailability and provides adequate concentrations in bones and soft tissues comparable with intravenous ciprofloxacin.18 19
There is evidence that fluoroquinolone is effective in treating Salmonella prosthetic joint infection in a patient on immunosuppressive medication.20 21
Currently more than one treatment option exists for prosthetic hip joint infections from debridement with prosthesis retention and long-term antibiotic treatment, to one-stage or two-stage revisions to excision arthroplasty. The risk of failure with DAIR procedure rises after stopping oral antibiotics, but lengthening antibiotic therapy may simply postpone, rather than prevent, failure.22 The best treatment option remains unclear, and currently surgeons perform both one-stage and two-stage revisions.23 24 In the UK in 2013, 36% were one-stage revisions, 60% were two-stage revisions and 4% of patients underwent an excision.23 There is no specific evidence at present to recommend a particular treatment, and the INfection ORthopaedic Management (INFORM) trial was commenced in 2016 with the intention of comparing one-stage versus two-stage revisions.23 In our patient, the DAIR procedure was not successful. Dimethyl fumerate he was taking might have contributed to his immunosupressed state. Both single-stage and two-stage revision options were discussed with the patient and in a multidisciplinary meeting. The consensus was to do a two-stage procedure.
Given the nature of the organism isolated and the relatively young age and good functional status of our patient, we performed a two-stage revision.
Learning points.
Salmonella infection should be suspected in those with a prosthetic joint infection if they are immune-suppressed, suffered a recent diarrhoeal illness or recent foreign travel.
The most common route of spread for Salmonella is haematogenous spread from a distant focus. This case is even more unusual as gastrointestinal infection and seeding in to joint has probably occurred preoperatively. Preoperative assessment should also explore all of these risk factors.
Treatment involves both antibiotic therapy and surgery, and two-stage revision may be preferable to allow for extended antibiotic therapy.
Footnotes
Contributors: CMRD: writing and revision of the manuscript. JSH: data collection and writing the article. PD: data collection and interpretation. NNS: supervision and final approval. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.National Joint Registry. NJR StatsOnline. Njrcentre.org.uk. http://www.njrcentre.org.uk/njrcentre/Healthcareproviders/Accessingthedata/StatsOnline/NJRStatsOnline/tabid/179/Default.aspx (accessed 6 Jan 2017).
- 2.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. The Lancet 2007;370:1508–19. 10.1016/S0140-6736(07)60457-7 [DOI] [PubMed] [Google Scholar]
- 3.Lamagni T. Epidemiology and burden of prosthetic joint infections. J Antimicrob Chemother 2014;69 Suppl 1:i5–i10. 10.1093/jac/dku247 [DOI] [PubMed] [Google Scholar]
- 4.Public Health England. UK Standards for microbiology investigations, Investigation of orthopaedic implant associated infections. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/504319/B_44i2.pdf (accessed 6 Jul 2017).
- 5.Kobayashi H, Hall GS, Tuohy MJ, et al. Bilateral periprosthetic joint infection caused by Salmonella enterica serotype Enteritidis, and identification of Salmonella sp using molecular techniques. Int J Infect Dis 2009;13:e463–e466. 10.1016/j.ijid.2008.12.015 [DOI] [PubMed] [Google Scholar]
- 6.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res 2009;467:958–65. 10.1007/s11999-008-0358-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Della Valle CJ, Paprosky WG. Paprosky Femoral Classification. J Bone Joint Surg [American volume] 2003;85:1–6. [DOI] [PubMed] [Google Scholar]
- 8.Pinaroli A, Lavoie F, Cartillier JC, et al. Conservative femoral stem revision: avoiding therapeutic escalation. J Arthroplasty 2009;24:365–73. 10.1016/j.arth.2007.12.002 [DOI] [PubMed] [Google Scholar]
- 9.Gupta A, Berbari EF, Osmon DR, et al. Prosthetic joint infection due to Salmonella species: a case series. BMC Infect Dis 2014;14:633 10.1186/s12879-014-0633-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organisation Media Centre. Salmonella (non typhoidal) fact sheet. http://www.who.int/mediacentre/factsheets/fs139/en/ (accessed 6 Jan 2017).
- 11.Day LJ, Qayyum QJ, Kauffman CA. Salmonella prosthetic joint septic arthritis. Clin Microbiol Infect 2002;8:427–30. 10.1046/j.1469-0691.2002.00466.x [DOI] [PubMed] [Google Scholar]
- 12.Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev 2014;27:302–45. 10.1128/CMR.00111-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Public Health England Research and Analysis. Salmonella by Serotype 2000 to 2010. 2007. https://www.gov.uk/government/publications/salmonella-by-serotype/salmonella-by-serotype-2000-to-2010 (accessed 6 Jan 2017).
- 14.Chai SJ, White PL, Lathrop SL, et al. Salmonella enterica serotype Enteritidis: increasing incidence of domestically acquired infections. Clin Infect Dis 2012;54 Suppl 5:S488–S497. 10.1093/cid/cis231 [DOI] [PubMed] [Google Scholar]
- 15.de la Torre B, Tena D, Arias M, et al. Recurrent prosthetic joint infection due to Salmonella enteritidis: case report and literature review. Eur J Orthop Surg Traumatol 2012;22 Suppl 1:89–97. 10.1007/s00590-012-0955-6 [DOI] [PubMed] [Google Scholar]
- 16.Dimethyl fumarate (Tecfidera): updated advice on risk of progressive multifocal leukoencephalopathy - GOV. UK, Medicines and Healthcare products Regulatory Agency. 2016. https://www.gov.uk/drug-safety-update/dimethyl-fumarate-tecfidera-updated-advice-on-risk-of-progressive-multifocal-leukoencephalopathy (accessed 8 Apr 2018).
- 17.Widmer AF, Colombo VE, Gächter A, et al. Salmonella infection in total hip replacement: tests to predict the outcome of antimicrobial therapy. Scand J Infect Dis 1990;22:611–8. 10.3109/00365549009027105 [DOI] [PubMed] [Google Scholar]
- 18.Fong IW, Ledbetter WH, Vandenbroucke AC, et al. Ciprofloxacin concentrations in bone and muscle after oral dosing. Antimicrob Agents Chemother 1986;29:405–8. 10.1128/AAC.29.3.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gentry LO, Rodriguez GG. Oral ciprofloxacin compared with parenteral antibiotics in the treatment of osteomyelitis. Antimicrob Agents Chemother 1990;34:40–3. 10.1128/AAC.34.1.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oe K, Wada T, Ohno H, et al. Salmonella septic arthritis following total knee arthroplasty for rheumatoid arthritis in a patient receiving etanercept. J Orthop Sci 2011;16:258–62. 10.1007/s00776-011-0023-9 [DOI] [PubMed] [Google Scholar]
- 21.Ekinci M, Bayram S, Akgül T, et al. Periprostetic Joint Infection Caused by Salmonella: Case Reports of Two Azathioprine and Prednisolone Induced-immunocompromised Patients. Hip Pelvis 2017;29:139–44. 10.5371/hp.2017.29.2.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byren I, Bejon P, Atkins BL, et al. One hundred and twelve infected arthroplasties treated with ’DAIR' (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother 2009;63:1264–71. 10.1093/jac/dkp107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strange S, Whitehouse MR, Beswick AD, et al. One-stage or two-stage revision surgery for prosthetic hip joint infection-the INFORM trial: a study protocol for a randomised controlled trial. Trials 2016;17:90 10.1186/s13063-016-1213-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beswick AD, Elvers KT, Smith AJ, et al. What is the evidence base to guide surgical treatment of infected hip prostheses? systematic review of longitudinal studies in unselected patients. BMC Med 2012;10:18 10.1186/1741-7015-10-18 [DOI] [PMC free article] [PubMed] [Google Scholar]