Abstract
Background/Objectives
Eating in the absence of hunger (EAH) has been linked to obesity in adults and children. This study examined the stability of EAH in children between 4.5 and 6 years old, and associations with energy intake and portion selection, as well as cross-sectional and prospective associations with body composition.
Methods
The participants were 158 boys and girls from the Growing Up in Singapore Towards healthy Outcomes cohort. At ages 4.5 and 6 years old children were provided lunch ad libitum, and immediately afterwards were exposed to palatable snacks to measure energy intake in the absence of hunger. At age 6 children completed an additional computer-based task to measure ideal portion size, where they selected pictures of the portions they would like to eat across eight foods. Measures of anthropometry (height/weight/skinfolds) were collected at both ages.
Results
Children who consumed energy during the EAH task at age 4.5 years were 3 times more likely to also do so at age 6 years. Children with high EAH intakes at age 4.5 years had high EAH intakes at age 6, highlighting stability of this behaviour over time. Energy consumed at lunch was unrelated to energy consumed during the EAH task, but children who ate in the absence of hunger cumulatively consumed more energy over lunch and the EAH task. Children who showed EAH tended to select larger ideal portions of foods during the computer task. EAH was not associated with measures of body composition.
Conclusions
EAH is a stable behavioural risk factor for increased energy intake, but was not associated with body composition in this cohort. The majority of children ate in the absence of hunger, suggesting that interventions aimed at reducing responsiveness to external food cues could help to reduce energy intakes.
1.0. Introduction
Increasing rates of obesity observed since the mid-20th century have been partially attributed to changes in the food environment, abundant in affordable, palatable and energy-dense foods, often served in large quantities, that promote greater energy intakes within and around meal times (McAllister et al., 2009, Gill, 2015). Responsiveness to environmental food cues like the sight or smell of foods can be reflected in physiological and behavioural responses. This includes increased salivation and endocrine changes, as well as increases in subjective appetite and selecting and consuming larger quantities of food (Ferriday and Brunstrom, 2008, Oakes and Slotterback, 2000, Nederkoorn et al., 2000, Blundell et al., 2005, Epstein et al., 1996, Fisher et al., 2003). Though the ‘obesogenic environment’ is thought to promote overconsumption, there are individual differences in appetitive traits and responsiveness to environmental food cues, which emerge early in life and stabilise during development, and help to explain why not everybody overconsumes energy and develops obesity (Llewellyn and Wardle, 2015).
Eating despite being full when exposed to palatable foods is a behavioural expression of heightened food responsiveness that could put children at risk of overconsuming calories. This behaviour can be empirically measured by exposing children to freely available snacks immediately after consuming a meal to satiety, in what Fisher and Birch (2002) conceptualised as the ‘Eating in the Absence of Hunger’ (EAH) paradigm. The EAH paradigm is primarily thought to test a child’s responsiveness to external palatable food cues, however increased energy intake during this task might also reflect some aspects of satiety responsiveness (Carnell and Wardle, 2007), disinhibited eating (Tanofsky-Kraff et al., 2008, van Strien and Oosterveld, 2008) and emotional arousal (Wallis and Hetherington, 2004). Moreover, the propensity to eat without hunger has hereditary and genetic components (Fisher et al., 2007a, Wardle et al., 2009) that are likely to be perpetuated by certain parental feeding practices, such as restriction of foods (Cutting et al., 1999, Fisher and Birch, 1999), indicating the potential for large individual differences in this behaviour.
EAH has been shown to be more prevalent among children with overweight/obesity, or at higher familial risk for overweight/obesity (Moens and Braet, 2007, Francis and Birch, 2005, Francis et al., 2007, Faith et al., 2006, Jansen et al., 2003). However, many of the studies examining the link between EAH and obesity in paediatric populations have been conducted only on girls, and those conducted on both boys and girls suggest that this relationship could be dependent on the child’s sex and age (for full review see Lansigan et al., 2015). Studies conducted with girls show that EAH is stable over time (Fisher and Birch, 2002) and is linked to higher adiposity and prospective weight gain (Shunk and Birch, 2004). Among studies which considered both sexes, some showed that EAH is linked to higher adiposity in girls, but not boys (Cutting et al., 1999), while others demonstrated the links with adiposity among boys, but not girls (Hill et al., 2008). Further research is needed to examine the stability of this behaviour among children from both sexes, and the potential links with body composition and weight gain over time.
Children who eat in the absence of hunger may be at risk for overconsuming calories and developing obesity, but it is unclear whether they also demonstrate other behaviours associated with higher energy intakes, such as selecting and consuming larger portions of food. Previous research demonstrated that among 4 year old children EAH was linked with increased intake of foods at lunch, particularly when children were presented with larger portions of food to consume (Fisher et al., 2003). Children, like adults, eat more when they are served larger portions of food (Fisher et al., 2007b, Birch et al., 2000, Steenhuis and Vermeer, 2009, Kling et al., 2016) and it has been suggested that encouraging children to self-serve their food could be a strategy to promote self-regulation and reduce intake (Birch et al., 1991). However, there are individual differences in self-served food portions and not all children eat less when given the opportunity to serve themselves at a meal (Savage et al., 2012, Branen et al., 1997, Fisher, 2007). It is possible that selecting larger portions of food could reflect a similar dimension of food cue responsiveness as that captured by the EAH paradigm, and highly food responsive children may select and consume larger portions of different foods, not just palatable snacks.
To better understand the link between EAH and weight status during childhood, the current study sought to test whether EAH is stable over time and is associated with larger portion selection, increased energy intake and adiposity in children. Specifically, we first examined whether EAH is a stable behaviour between 4.5 and 6 years of age (1). We then investigated the links between EAH and (2) energy consumed during an ad libitum lunchtime meal, (3) child selected ideal portion sizes across a range of foods (4) and child adiposity. We hypothesised that EAH would show stability from 4.5 to 6 years. We further predicted that children who ate in the absence of hunger would consume more energy at lunch, would have higher cumulative energy intakes across the two eating occasions and would select larger portions of foods on a computer based portion selection task. Finally, we predicted that EAH would be associated with higher BMI and higher adiposity at both time points, and children who ate in the absence of hunger at age 4.5 years would have higher BMI and greater increase in BMI between the ages 4.5 and 6 years.
2.0. Methods
2.1. Participants
The participants in this study were children from the Growing Up in Singapore Towards healthy Outcomes (GUSTO) cohort (N=1247), who participated in eating behaviour measures (lunch selection and intake, and the EAH task) at 4.5 (± 2 months) and 6 (± 2 months) years of age. Eligibility criteria and recruitment methodology for the GUSTO cohort are described in detail elsewhere (Soh et al., 2014). Pregnant women (18-50 years) were recruited from two major public hospitals in Singapore. Participants had to be Chinese, Malay or Indian with parents of homogenous ethnicity. Written informed consent was collected on recruitment. Selection criteria for participation in this study are described in the participant flowchart (Appendix A). All parents recruited into the cohort were invited to take part in the eating behaviour measures, but participation depended on the family schedules, availability of the test slots in the hospitals involved and attendance at previous eating behaviour tasks. Specific reasons for the lack of participation were not recorded.
Of the 368 children who participated in the eating behaviour tasks at 4.5 years, 242 children attended the follow-up tasks at 6 years. Children who failed to attend the follow-up did not differ from the remaining sample in sex, ethnicity, BMIz, maternal characteristics (age, pre-pregnancy weight, education level) or any anthropometric measures at 4.5 years. Children who consumed less than 50 grams of food at lunch and/or indicated that they were still hungry afterwards were excluded, as absence of hunger could not be assumed for these children (n= 6 at 4.5 years and n= 78 at 6 years; in line with previous approach by Fisher and Birch, 2002). At age 6 years more children were excluded due to insufficient intake, which was probably influenced by only a single food being served, compared to the buffet served at age 4.5 years. The final sample consisted of 158 children.
2.2. Lunchtime meal intake
The lunch took place in the same test room equipped with child appropriate furniture and utensils at both time points. Children were fasted for a minimum of 3 hours before lunch.
At 4.5 years, children consumed lunch with only their mother present in the room. Prior to the meal, mothers were requested to not interfere with children’s food choice and to interact with children in an otherwise usual manner. Participants were told they could eat as much or as little as they wished, and were given up to 30 minutes to consume the meal. Children were served an ad libitum buffet lunch consisting of 9 foods and 3 drinks that had previously been identified as liked and familiar products based on food frequency questionnaires (FFQ) collected from the same cohort at an earlier time point.
The foods and drinks served were: white bread (Gardenia; 2.63 kcal/g; 6 slices), Honey Stars cereal (Nestle; 3.8 kcal/g; 80g), pancakes (Aunty Jemima; 3 kcal/g; 70g), chocolate cake (Sara Lee; 4.3 kcal/g; 80g), cheese (Cowhead; 2.95 kcal/g; 66g), chicken cocktail sausage (Fairprice; 2.95 kcal/g; 192g), chicken nuggets (CP; 2.29 kcal/g; 216g), apple slices (0.44 kcal/g; 204g), canned corn (Hosen; 0.81 kcal/g; 160g), apple juice (Marigold; 0.5 kcal/ml; 6 boxes), full cream milk (Marigold; 0.65 kcal/ml; 6 boxes) and water. Additional portions of each item were also available should any single item have been fully consumed during the meal. Before and after the meal children were given a subjective 5-point picture hunger scale ranging from ‘Hungry’ to ‘Very full’.
At age 6 years, children consumed lunch within a similar time frame, but without their mother present. For this meal, children were presented with a large bowl of fried rice (800g; 1.86 kcal/g) and asked to select their own portion. Children were told that they could eat as much as they wished for their lunch, and they could serve themselves multiple times. The serving bowl was replaced with another 800g if the child required more, although that was never required. Before and after lunch, children’s hunger was assessed using a similar 5-point scale, this time ranging from ‘Very hungry’ to ‘Very full’. At both time points, foods were weighed before and after consumption to estimate energy consumed during lunch.
2.3. Eating in the absence of hunger
The EAH free access protocol was adapted from Fisher & Birch (2002). The EAH task was identical at both time points and took place approximately 20 minutes after lunch. Two sweet (17g M&M, 5.01kcal/g; 30g Hello Panda 5.43kcal/g) and two savoury (6 g Rollercoster, 5.00 kcal/g; 8g Bin Bin, 4.87kcal/g) snacks were placed in small bowls. Children were given access to colouring paper and crayons, and were encouraged to play together with the researcher present in the room. After 5 minutes, the researcher placed the food bowls on the table near the child and told the child that they had to briefly leave the room to prepare the next game, but they were welcome to have the snacks if they wished. The researcher returned after 5 minutes, removed the snacks and took the child to their next activity. Snacks were weighed before and after the task to estimate energy intake.
2.4. Ideal portion selection task
At age 6 years, children participated in an age-appropriate computer-based ideal portion selection task, adapted from a previous method (Brunstrom et al., 2008). The children were presented with high-resolution images of eight different foods representing a variety of common foods available in Singapore and varying in energy density (Rice Porridge, 0.7 kcal/g; Mozzarella Pizza, 2.71kcal/g; Salad, 1.32 kcal/g; Fried Rice, 1.86 kcal/g; Macaroni Cheese, 3.71 kcal/g; Steamed Buns, 2.49 kcal/g; Garlic Bread, 3.48 kcal/g; Roti Prata, 2.46 kcal/g). All foods were presented on the same white plate, under constant lighting conditions and photographed from the same upper viewing angle. The example images are presented elsewhere (McCrickerd and Forde, 2016). Children were asked to imagine that they were going to consume each of the foods for their lunch, followed by the question “how much <food name> would you like to eat for your lunch right now?” Each food was presented in portions ranging from 20 kcal to 900 kcal in 20 kcal steps (44 images in total for each food), and children used designated computer keys to increase or decrease the portion size of the food presented on the plate until they chose their ideal portion. The energy content of the chosen image represented the child’s ideal portion for each of the different food items.
2.5. Anthropometric measures
Anthropometric measures were usually collected on the same day or within one month of participating in the EAH task at both the 4.5 and 6 year time points. This included height, weight, waist and mid-arm circumference, and triceps, biceps, suprailiac and subscapular skinfold thickness (skinfold measurements taken using Holtain Skinfold Caliper (Holtain Ltd, Crymych, UK). All measures were taken in duplicate following the standard guidelines and using the recommended anatomical landmarks for children in this age group (de Onis et al., 2004, Phenxtoolkit). Some data were missing due to lack of assent to individual measurements and these are outlined in the participant flowchart (Appendix A). Height and weight were transformed to BMI z-scores (BMIz) corrected for age and sex according to the WHO child growth standards (WHO, 2003), and later used to classify children’s weight status as with healthy weight (BMIz ≤ 1.04) or with overweight/obesity (BMIz > 1.04; referred to as “with overweight” throughout), equivalent to the 85th percentile (Wang and Chen, 2012, CDC, 2015, Berkowitz et al., 2010). Skinfold thickness measures were used to calculate a body adiposity index (BAi) based on the sum of the suprailiac, subscapular, biceps and triceps skinfold thickness (Nightingale et al., 2011, Berkowitz et al., 2010), and an additional measure of waist-to-height ratio was calculated as an estimate of central adiposity.
3.0. Statistical Analysis
Children’s energy intake during the EAH task was treated as a continuous variable, but was also converted into categorical variables to differentiate children who did not consume any food during the EAH task from those who consumed some energy, and who were further split to low vs high EAH intake using a median split (adapted after (Fisher and Birch, 2002). All study aims were tested comparing children who did not show EAH and those who did (binary variable), and those with no EAH, low EAH and high EAH, to reduce the impact of unbalanced sample sizes, as the majority of children showed some EAH. Energy consumed during lunch was added to the energy consumed during the EAH task as a measure of cumulative energy consumed over the two eating occasions (referred to as “cumulative intake” throughout). For the computer task, the ideal portion of the eight foods (in kcal) was averaged to provide a mean ideal portion (kcal) as an estimate of children’s portion selection, independent of food type.
Preliminary regression analyses were conducted to identify potential independent covariates of EAH (from sex, ethnicity, BMI, birth weight, gestational age, maternal education and household income) and adiposity (the same covariates, without BMI). There were no significant links between these variables and EAH (p>0.40), but sex and BMI were still controlled for in the analyses focused on EAH, as these have been identified by past research summarised in the introduction as potential confounders. Conversely, sex and birth weight were identified as significant covariates of adiposity (p<0.05), and were therefore controlled for in all analyses focused on adiposity.
To examine the stability of EAH between 4.5 and 6 years (1), hierarchical logistic regressions were conducted with EAH at 6 years as a binary outcome variable, adjusted for sex and BMI. Additional chi-squared analyses examined whether children who showed no intake during the EAH task or low vs high EAH at 4.5 years tended to stay in the same intake category at age 6 years. ANCOVAs (adjusted for sex and BMI) were conducted to examine if children who showed EAH (and those with lower vs higher EAH intake) differed from those who did not eat in the absence of hunger, in (2) energy consumed at lunch and cumulatively, at both time points and (3) in ideal portion size selected at age 6 years. ANCOVAs (adjusted for sex and birth weight) were used to examine the links between EAH and (4) children’s body composition. Additional logistic regressions (adjusted for sex and birth weight) were conducted to test if children of different weight status (healthy weight vs overweight) differed in their likelihood to show EAH, at both ages. Finally, hierarchical linear regression analysis adjusted for sex, birth weight and baseline BMI was conducted to test if EAH at age 4.5 years predicted BMI at age 6 years, and change in BMI between 4.5 and 6 years (Time 2 - Time 1). Bonferroni corrected post-hoc comparisons are reported throughout. For sensitivity testing, all study aims were re-examined using hierarchical regression models with continuous predictors and outcomes, adjusted for covariates. Unadjusted analyses yielded virtually identical results to those reported (unreported). All analyses were conducted in SPSS version 23.0 (IBM), and an alpha level of 0.05 was considered statistically significant.
4.0. Results
4.1. Sample characteristics
There sample consisted of 84 boys and 74 girls, who were of Chinese (n= 94), Malay (n= 32) or Indian (n= 32) ethnicity. The highest educational achievement reported by the mothers at recruitment was primary education (5.6%), secondary education (60.3%) or university education (31.6%; 2.5% unreported). The mean birth weight was 3137 g ± 450 and the majority of the sample had the gestational age above 37 weeks (94.4%).
Energy intake during lunch and the EAH task at both ages, presented for the total sample are described in Table 1. The proportion of children who consumed some energy during the EAH task and the amount of energy consumed in the absence of hunger was higher at age 6 years, potentially due to the different energy content of foods served at lunch. Mean BMIz decreased, while the adiposity levels (across all indices) increased from 4.5 to 6 years.
Table 1.
Eating in the absence of hunger (% of sample and energy intake), lunch intake and anthropometry1 at ages 4.5 and 6 years.
| Age 4.5 years | Age 6 years | |
|---|---|---|
| Energy intake | ||
| % No intake (kcal ± SD) | 27.2% (0) | 12.5% (0) |
| % EAH (kcal ± SD) | 73.0 % (40.4 ± 34.3) | 87.5% (53.4 ± 36.4 kcal) |
| Low intake (kcal ± SD) | 36.1% (15.0, ± 8.4) | 43.8% (27.8, ± 12.0) |
| % High intake (kcal ± SD) | 36.7% (65.4, ±31.8) | 43.8% (79.1, ±34.4) |
| Lunch intake (kcal ± SD) | 319.4 ± 150.2 | 226.3 ± 117.5 |
| Cumulative intake (kcal ± SD) | 347.0 ± 155.2 | 273.0 ± 122.5 |
| Anthropometry | ||
| BMIz | 0.15 ± 1.26 | 0.04 ± 1.52 |
| Biceps (mm) | 6.62 ± 2.44 | 6.66 ± 3.01 |
| Triceps (mm) | 10.27 ± 3.53 | 10.75 ± 4.58 |
| Suprailiac (mm) | 6.99 ± 3.64 | 7.22 ± 5.38 |
| Subscapular (mm) | 7.56 ± 3.68 | 8.08 ± 5.87 |
| BAi | 31.87 ± 12.34 | 32.66 ± 17.88 |
| Mid-arm (cm) | 16.90 ± 3.41 | 17.74 ± 2.66 |
| Waist (cm) | 51.63 ± 5.25 | 54.29 ± 7.85 |
| Waist-to-height ratio | 0.49 ± 0.05 | 0.47 ± 0.05 |
There were no sex differences in likelihood to show EAH at 4.5 (χ<2.0, p>0.31) or 6 years (χ<2.4, p>0.12), or in energy consumed during the EAH task at 4.5 (t=1.54, p=0.12) or 6 years (t=1.62, p=0.11). At 4.5 years boys consumed more energy at lunch (t=2.74, p=0.007, Δ64.0, CI95% [17.9, 110.0]) and more energy cumulatively (t=2.95, p=0.004, Δ71.2, CI95% [23.5, 119.0]). Similarly, at 6 years boys consumed more energy at lunch (t= 2.10, p=0.037, Δ38.9, CI95% [2.45, 75.3]), and cumulatively (t=2.28, p=0.026, Δ43.2, CI95% [5.33, 81.1]). Boys and girls did not differ in BMI or waist circumference at either age (t<1.0, p>0.3), but girls tended to have higher body adiposity index (4.5 years: t=2.45, p=0.015, Δ4.83, CI95% [0.94, 8.72]; 6 years: t=2.24, p=0.026, Δ6.83, CI95% [8.09, 12.86]) and across all indices (p<0.05).
4.2. Stability of eating in the absence of hunger over time
Eating in the absence of hunger showed stability between the two time points, and children who ate in the absence of hunger at 4.5 years were 3 times more likely to also do so at age 6 years (χ2 =4.04, p=0.045; Wald criterion 4.17, p=0.041; Odds Ratio 3.01, 95% CI [1.04, 8.67]; Nagelkerke R2= 0.087).
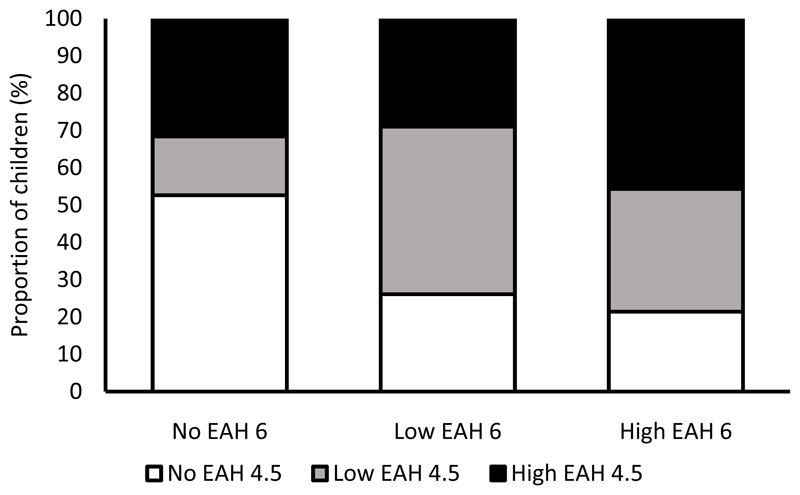
Although the proportion of children who consumed some energy during the EAH task increased at age 6 years, when split to three EAH groups, children with no intake, low or high EAH intake at 4.5 years tended to stay in the same category of intake at age 6 years (χ=12.1, p=0.017). Figure 1 illustrates the percentage of children who showed no EAH, low and high EAH at age 6 years, and their EAH classification at age 4.5 years. Among children who did not eat in the absence of hunger at age 6 years, over 50% also did not consume any snacks at age 4.5 years. Among those who showed high EAH intake at age 6 years, over 45% were also classified as high EAH intake at age 4.5 years, demonstrating stability of this behaviour over time. Additional regression analyses confirmed that energy consumed in the absence of hunger at age 4.5 years predicted energy consumed during the EAH task at 6 years (B=0.19, p=0.036).
Figure 1.
Percentage of children classified according to their intake during the EAH task at ages 4.5 and 6 years.
4.3. Eating in the absence of hunger and energy intake
There were no differences in energy consumed at lunch between children who ate in the absence of hunger, compared to those who did not eat in the absence of hunger at age 4.5 years (F(1, 151)= 1.94, p=0.17) and 6 years (F(1, 140)= 0.12, p=0.73). Similarly, no differences in energy intake at lunch were observed when children were split into three EAH groups at age 4.5 years (F(2, 150)= 2.50, p=0.086, pη2= 0.03) and 6 years (F(2, 139)= 0.10, p=0.90, pη2= 0.002), or in regression models that used continuous data at 4.5 (β<0.01, p=0.95) and 6 years (β=-0.04, p=0.68), indicating that children’s intake during EAH task was unrelated to their energy intake at lunch.
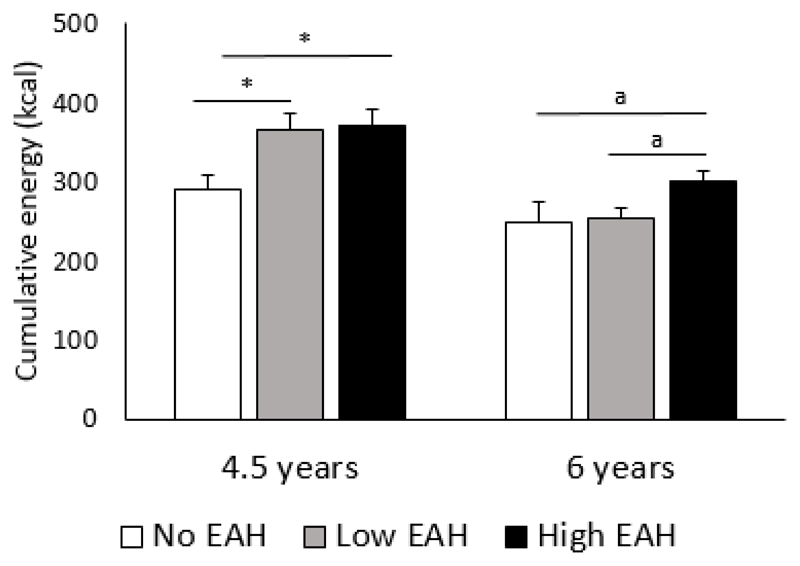
Though EAH was independent from children’s energy intake at lunch, children who showed EAH at 4.5 years cumulatively consumed more energy over the two eating occasions (M=368.7, SE=14.9; (F(1,151)= 8.67, p=0.004, pη2= 0.054), compared to children who did not show EAH (M=289.2, SE=19.2). However, this was not observed at age 6 years (F(1,140)= 2.42, p=0.12, pη2= 0.017). When three EAH groups were considered, the pattern remained the same at 4.5 years old - children who did not eat in the absence of hunger consumed cumulatively less energy than children who showed EAH intake (F(2, 150)= 4.35, p=0.015, pη2= 0.055). However, at age 6 years children who had high energy intake during the EAH task cumulatively consumed more energy than children with no EAH intake or low EAH intake (F(2, 139)= 3.70, p=0.027, pη2= 0.051). Figure 2 illustrates group differences in mean cumulative energy intakes at both time points. These patterns remained similar in linear regression models at ages 4.5 (β=0.23, p=0.003) and 6 years (β=.29, p<0.001).
Figure 2.
Group differences in cumulative intake of energy at 4.5 and 6 years old, adjusted for sex and BMI. Bonferroni corrected post hoc group comparisons: *p<0.05; a indicates p<0.09
4.4. Eating in the absence of hunger and ideal portion size
There were no differences in mean ideal portion selected on the computer task at age 6 years between children who consumed some energy during the EAH task and those who did not (F(1,127)= 0.90, p=0.35; pη2= 0.01). However, when the eight foods were assessed separately it was clear that children who ate during the EAH task at 4.5 and 6 years old consistently chose larger ideal portion sizes of the foods presented, but the majority of these comparisons did not reach significance (results presented in Table 2). These patterns remained similar when three EAH groups were compared (F(2,126)= 0.51, p=0.60, pη2= 0.01) and when data were assessed continuously, highlighting non-significant trends for children who ate more during the EAH task to select larger mean ideal portions of foods (β=0.12, p=0.17), larger portions of garlic bread (β=0.15, p=0.09) and pizza (β=0.15, p=0.19) and significantly larger portions of Bao (β=0.19, p=0.026).
Table 2.
Group differences1 in ideal portion size (Mean kcal ± SEM) selected by children at age 6 years, and differences in measures2 of anthropometry, stratified by EAH intake at ages 4.5 and 6 years.
| Ideal portion size (kcal) | Age 4.5 years | Age 6 years | ||
|---|---|---|---|---|
| No EAH | EAH | No EAH | EAH | |
| Bao | 231.4 ± 37.3 | 395.9 ± 31.9*** | 266.0 ± 58.8 | 359.7 ± 28.2 |
| Rice porridge | 215.7 ± 36.0 | 288.6 ± 25.6 | 224.2 ± 51.5 | 272.8 ± 22.8 |
| Garlic bread | 286.8 ± 42.4 | 300.0 ± 27.7 | 277.8 ± 73.2 | 297.1 ± 24.4 |
| Mac & Cheese | 288.8 ± 35.0 | 379.3 ± 29.6a | 407.0 ± 63.7 | 348.5 ± 25.3 |
| Salad | 124.6 ± 25.9 | 161.9 ± 19.4 | 123.0 ± 26.0 | 154.5 ± 17.4 |
| Pizza | 325.2 ± 48.4 | 441.6 ± 31.1* | 390. 0 ± 69.9 | 418.7 ± 28.5 |
| Prata | 259.5 ± 29.2 | 294.7 ± 21.4 | 275.0 ± 34.6 | 286.2 ± 19.1 |
| Fried rice | 208.4 ± 31.7 | 302.2 ± 24.9* | 268.0 ± 45.2 | 278.5 ± 22.1 |
| Mean portion | 244.0 ± 22.1 | 329.7 ± 16.8** | 275.9 ± 32.6 | 310.4 ± 15.1 |
| Anthropometry | ||||
| BMIz | 0.18 ± 0.16 | 0.15 ±0.13 | -0.28 ± 0.51 | 0.08 ± 0.13 |
| Biceps (mm) | 7.1 ± 0.2 | 6.5 ± 0.4 | 6.1 ± 0.65 | 6.7 ± 0.28 |
| Triceps (mm) | 10.3 ± 0.5 | 10.3 ± 0.3 | 9.4 ± 1.1 | 10.9 ± 0.41 |
| Suprailiac (mm) | 6.8 ± 0.5 | 7.1 ± 0.4 | 6.4 ± 1.4 | 7.3 ± 0.49 |
| Subscapular (mm) | 7.6 ± 0.6 | 7.6 ± 0.3 | 7.8 ± 1.9 | 8.1 ± 0.5 |
| BAi | 31.6 ± 1.9 | 31.4 ± 1.2 | 29.3 ± 4.9 | 33.1 ± 1.6 |
| Mid-arm (cm) | 16.6 ± 0.3 | 17.1 ± 0.4 | 17.3 ± 0.6 | 17.8 ± 0.2 |
| Waist (cm) | 51.3 ± 0.5 | 51.8 ± 0.7 | 53.4 ± 2.0 | 54.4 ± 0.7 |
| Waist-to-height ratio | 0.49 ± 0.01 | 0.49 ±0.01 | 0.47 ± 0.01 | 0.47 ± 0.01 |
EAH: Eating in the absence of hunger; a=0.051; (t-tests)*p<0.05; **p<0.01, ***p<0.001
ANCOVA analyses adjusted for sex and BMI for group differences in ideal portion sizes and adjusted for sex and birth weight in analyses focused on child anthropometry collected at the same time-point as the EAH task.
All non-significant
4.4. Eating in the absence of hunger and body composition
There were no significant differences in BMI or body composition between children who ate in the absence of hunger and those who did not, at ages 4.5 (F<0.7, p>0.41) or 6 years (F<0.7, p>0.40). Group differences in indices of adiposity are presented in Table 2. Similarly, no differences in BMI or body composition were observed when three categories of EAH were considered, at age 4.5 years (F<1.0, p>0.48) or 6 years (F<1.0, p>0.57).
The likelihood to eat in the absence of hunger was the same among children with healthy weight and with overweight, at age 4.5 years (B= 0.78 95% CI [0.20, 2.99], Wald criterion 0.14, p=0.71, Nagelkerke R2=0.01) and 6 years (B=1.35 95% CI [0.36, 5.09], Wald criterion 0.19, p=0.66, Nagelkerke R2=0.04). These patterns were supported by the models that used continuous data, highlighting that EAH at 4.5 or 6 years did not predict child BMIz (4.5 years: F(3, 151)= 2.06, p=0.11, β<0.01, p=0.91; 6 years: F(3, 140)= 1.67, p=0.18, β<0.01, p=0.96), or measures of adiposity at either time point (β<0.30, p>0.5).
In prospective analyses, energy consumed in the absence of hunger at age 4.5 years did not predict child BMI at age 6 years (β= 0.02, p=0.67; F(4, 134)= 72.3, p<.32) or change in BMI between the ages 4.5 and 6 years (β= 0.04, p=0.67; F(4, 134)= 0.13, p<0.97).
5.0. Discussion
The current study examined the stability of eating in the absence of hunger between 4.5 and 6 years, as well as the relationship between this behaviour and children’s intake of energy, self-selected ideal portion sizes, and their body weight and composition. Children who showed EAH consumed cumulatively more energy over the two eating occasions (2), and tended to select larger ideal portions of foods (3). Importantly, children who showed EAH at 4.5 years were 3 times more likely to eat in the absence of hunger at 6 years, highlighting stability of this behaviour over time (1). Nevertheless, EAH was not linked to children’s BMI or body composition, and did not predict future BMI (4).
EAH showed stability over an 18 month period and children tended to consume similar amounts of energy during this task at both times, confirming the stability of the behaviour among boys and girls and the impact on energy intake. These results are consistent with Fisher and Birch (2002), who demonstrated stability of this behaviour among girls of a similar age. In the current study, both boys and girls who showed higher intake in the absence of hunger at a younger age, and had a higher risk for overeating, tended to also show higher intake at the later time point, indicating that EAH is a relatively stable behaviour among both sexes. Future studies are needed to examine the emergence of this behaviour among younger children.
The amount consumed during the EAH task was not linked to how much children ate during lunch, indicating that intake during the EAH task was not simply a compensatory mechanism among children who consumed less at lunch. Instead, children who ate in the absence of hunger, particularly in the high EAH group, consumed cumulatively more energy over the two eating occasions, compared to children who did not eat in the absence of hunger. This was true at both time points and indicates that free access to palatable foods outside of the main mealtimes could be a risk factor for increased energy intake, especially since the majority of children showed susceptibility to this food cue. In this instance, parents may be inclined to use methods of restriction as a means to limit intake of such snacks, which could be problematic because previous research suggests that these strategies are more likely to exacerbate EAH than to reduce it (Johnson and Birch, 1994, Birch et al., 2003, Fisher and Birch, 2002). One strategy to limit EAH could be to covertly restrict access to palatable foods by managing the child’s food environment and in this way reduce potential temptation. Parents could also be given guidance on appropriate techniques to reduce children’s food responsiveness, which have been shown to be effective in reducing EAH in school-age children with overweight and obesity (Boutelle et al., 2011).
In the current study children who consumed some food during the EAH task tended to choose larger ideal portions for seven out of eight foods presented in the computer-based task. While these differences were small and not statistically significant, they were consistent across foods, and the unbalanced sample sizes may have limited the power of these comparisons. At age 4.5 years the group of children who did not eat in the absence of hunger was larger, compared to at age 6 years, when the sample was more balanced. When the ideal portion selections were examined among children stratified by the EAH intake at age 4.5 years the differences showed statistical significance, suggesting that the trends observed at age 6 years could be meaningful. Ideal portions selected on a computer have been shown to predict the actual portions selected and consumed at a later meal (Wilkinson et al., 2012), and among children larger portions have been linked with increased meal size and energy intake (Fisher et al., 2007b, Birch et al., 2000, Steenhuis and Vermeer, 2009, Kling et al., 2016, Fisher et al., 2003). It is possible that EAH and selection of larger ideal portion sizes in the computer-based task reflect a similar dimension of children’s responsiveness to external food cues. An alternative interpretation of these findings might be that children who did not eat in the absence of hunger selected smaller portions of foods in the computer-task, perhaps because they have a smaller appetite.
Contrary to the past findings, EAH was not linked to children’s body composition, which was true for both boys and girls. Previous studies that have examined EAH and adiposity were mainly conducted on either boys or girls, and those that considered both sexes tended to report sex-specific differences and focus primarily on BMI (Cutting et al., 1999, Fisher et al., 2007a, Moens and Braet, 2007, Hill et al., 2008, Kral et al., 2012). Our findings suggest that most children in this age group, independent of their weight status and sex, are susceptible to show EAH when given access to palatable snack-foods. Previous research suggests that parental feeding practices, particularly restriction, can independently contribute to and moderate the link between children’s EAH and adiposity (Birch et al., 2003, Cutting et al., 1999, Fisher and Birch, 2002), but parental behaviours can also be a consequence of the child’s weight status (Costanzo and Woody, 1985). A recent study from our GUSTO cohort also showed that the relationship between parental feeding practices and children’s weight gain between 4-6 years is bi-directional (Quah et al., Under review). Children who show EAH in the laboratory setting may be at risk of weight gain if they have opportunities to habitually express this behaviour in their usual environment, and that will be affected by parenting style and feeding practices.
The strength of the current study was in the multi-ethnic sample of boys and girls of the same age, who participated in a variety of behavioural and anthropometric measurements at two time points over an 18 month period. However, there are several limitations worth highlighting. Firstly, there was a relatively small sample of children who did not consume any energy during the EAH task which limited the comparisons, although similar numbers have been reported in other studies (Hill et al., 2008, Moens and Braet, 2007). This was somewhat controlled by comparing three groups of children and conducting analyses on continuous data. Secondly, children with overweight were underrepresented, which limited the comparisons with body composition, although these numbers were representative of the Singaporean population. Another limitation was the lack of data on children’s ideal portion size at age 4.5 years. There were also some methodological differences in the meals between the two time points. At age 6 years children were served fried rice, which is a common local mealtime food. However, there were many children who did not consume enough of the meal and reported feeling hungry afterwards, and thus had to be excluded from the analyses. Finally, the findings of this study suggest that unrestricted access to palatable foods outside of main mealtimes may contribute to greater cumulative energy intakes, particularly among children with heightened susceptibility to external food cues. Nevertheless, the measure of cumulative intake included also the energy consumed during the EAH task, and as such the EAH intake (predictor) and the cumulative energy intake (outcome) were not independent of one another. Future studies should test this association in more strict experimental designs. Despite these limitations, our study demonstrated that EAH is stable over time and contributes to increased energy intakes among children who are more susceptible to external food cues.
In summary, EAH is a stable (1) behavioural risk factor for increased intake of energy (2), independently of sex or weight status. Our findings show that 4.5 year old children who consumed energy in the absence of hunger were 3 times more likely to exhibit the same behaviour 18 months later. Responsiveness to external food cues, as captured by the EAH paradigm, may also manifest in other eating behaviours, such as selecting larger food portions (3). Portion selection data in the current study was only available at age 6 years and further research is needed to examine the trends observed in the current study among younger children. Though EAH was not linked with measures of body composition in this sample (4), potential moderating effects of parental feeding practices and the child’s environment require further investigation. Given the prevalence of this behaviour, future research should examine strategies to minimise children’s responsiveness to external food cues and provide parents with appropriate guidelines to reduce EAH.
Supplementary Material
Acknowledgements
The GUSTO study group includes: Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Chung Ning Law, Evelyn Xiu Ling Loo, Fabian Yap, Falk Mueller-Riemenschneider, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P S van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira., Jonathan Tze Liang Choo, Jonathan Y. Bernard, Joshua J. Gooley, Keith M. Godfrey, Kenneth Kwek, Kok Hian Tan, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Lourdes Mary Daniel, Lynette P Shek, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Peter D. Gluckman, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, Seang-Mei Saw, See Ling Loy, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shirong Cai, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yap-Seng Chong, Yin Bun Cheung, Yiong Huak Chan and Yung Seng Lee.
Sources of Support: This work is supported by the Translational Clinical Research (TCR) Flagship Program on Developmental Pathways to Metabolic Disease funded by the National Research Foundation (NRF) and administered by the National Medical Research Council (NMRC), Singapore-NMRC/TCR/004-NUS/2008. Additional funding is provided by the Singapore Institute for Clinical Sciences, A*STAR and Nestec SA. KMG is supported by the National Institute for Health Research through the NIHR Southampton Biomedical Research Centre and by the European Union's Seventh Framework Programme (FP7/2007-2013), project Early Nutrition under grant agreement n°289346.
Abbreviations
- EAH
Eating in the absence of hunger
- BMIz
Body Mass Index z-score
Footnotes
Clinical Trial Registry Number: NCT01174875; https://clinicaltrials.gov/
Authors' contributions
This study was conceived and designed by CGF, AF, KMC, MFFC and LRF. Analyses were performed and interpreted by AF, KMC and CGF. ATG, JYT and MJC were involved in data collection. AF, KMC and CGF prepared the draft manuscript with input from LRF, QPL and MFFC. YSC, KHT, FY, LPS, MJM, BFPB, YSL and KMG were responsible for conception and recruitment for the GUSTO cohort. All authors reviewed and approved the final draft.
Competing interests
K. M. G., Y. S. L., C.G.F. and Y.-S. C. have received reimbursement for speaking at conferences sponsored by companies selling nutritional products. They are part of an academic consortium that has received research funding from Abbott Nutrition, Nestec and Danone. L.R.F. is an employee of Nestec SA, working at the Nestlé Research Center. The other authors have no financial or personal conflict of interests.
Ethics approval and consent to participate
Informed written consent was obtained from participants, and the study was approved by the National Healthcare Group Domain Specific Review Board and SingHealth Centralized Institutional Review Board.
References
- Berkowitz RI, Moore RH, Faith MS, Stallings VA, Kral TV, Stunkard AJ. Identification of an obese eating style in 4-year-old children born at high and low risk for obesity. Obesity. 2010;18:505–512. doi: 10.1038/oby.2009.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Engell D, Rolls BJ. Serving portion size influences 5-year-old but not 3-year-old children’s food intakes. Journal of the American Dietetic Association. 2000;100:232–234. doi: 10.1016/S0002-8223(00)00070-5. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. The American Journal of Clinical Nutrition. 2003;78:215–220. doi: 10.1093/ajcn/78.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birch LL, Johnson SL, Andresen G, Peters JC, Schulte MC. The variability of young children's energy intake. New England Journal of Medicine. 1991;324:232–235. doi: 10.1056/NEJM199101243240405. [DOI] [PubMed] [Google Scholar]
- Blundell JE, Stubbs RJ, Golding C, Croden F, Alam R, Whybrow S, Le Noury J, Lawton CL. Resistance and susceptibility to weight gain: Individual variability in response to a high-fat diet. Physiology & Behavior. 2005;86:614–622. doi: 10.1016/j.physbeh.2005.08.052. [DOI] [PubMed] [Google Scholar]
- Boutelle KN, Zucker NL, Peterson CB, Rydell SA, Cafri G, Harnack L. Two novel treatments to reduce overeating in overweight children: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79:759. doi: 10.1037/a0025713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branen L, Fletcher J, Myers L. Effects of pre-portioned and family-style food service on preschool children's food intake and waste at snacktime. Journal of Research in Childhood Education. 1997;12:88–95. [Google Scholar]
- Brunstrom JM, Shakeshaft NG, Scott-Samuel NE. Measuring 'expected satiety' in a range of common foods using a method of constant stimuli. Appetite. 2008;51:604–614. doi: 10.1016/j.appet.2008.04.017. [DOI] [PubMed] [Google Scholar]
- Carnell S, Wardle J. Measuring behavioural susceptibility to obesity: validation of the child eating behaviour questionnaire. Appetite. 2007;48:104–13. doi: 10.1016/j.appet.2006.07.075. [DOI] [PubMed] [Google Scholar]
- CDC. Defining Childhood Obesity. [Accessed 01.03.2016];2015 [Online]. Available: https://www.cdc.gov/obesity/childhood/defining.html.
- Costanzo PR, Woody EZ. Domain-specific parenting styles and their impact on the child's development of particular deviance: the example of obesity proneness. Journal of Social and Clinical Psychology. 1985;3:425–445. [Google Scholar]
- Cutting TM, Fisher JO, Grimm-Thomas K, Birch LL. Like mother, like daughter: familial patterns of overweight are mediated by mothers' dietary disinhibition. The American Journal of Clinical Nutrition. 1999;69:608–613. doi: 10.1093/ajcn/69.4.608. [DOI] [PubMed] [Google Scholar]
- De Onis M, Onyango AW, Van Den Broeck J, Chumlea CW, Martorell R. Measurement and standardization protocols for anthropometry used in the construction of a new international growth reference. Food and Nutrition Bulletin. 2004;25:S27–S36. doi: 10.1177/15648265040251S104. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch R, Coleman KJ. Differences in salivation to repeated food cues in obese and nonobese women. Psychosomatic Medicine. 1996;58:160–4. doi: 10.1097/00006842-199603000-00011. [DOI] [PubMed] [Google Scholar]
- Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Eating in the absence of hunger: a genetic marker for childhood obesity in prepubertal boys? Obesity. 2006;14:131–138. doi: 10.1038/oby.2006.16. [DOI] [PubMed] [Google Scholar]
- Ferriday D, Brunstrom JM. How does food-cue exposure lead to larger meal sizes? British Journal of Nutrition. 2008;100:1325–32. doi: 10.1017/S0007114508978296. [DOI] [PubMed] [Google Scholar]
- Fisher JO. Effects of Age on Children's Intake of Large and Self-selected Food Portions. Obesity. 2007;15:403–412. doi: 10.1038/oby.2007.549. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Restricting Access to Foods and Children's Eating. Appetite. 1999;32:405–419. doi: 10.1006/appe.1999.0231. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. The American Journal of Clinical Nutrition. 2002;76:226–231. doi: 10.1093/ajcn/76.1.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Cai G, Jaramillo SJ, Cole SA, Comuzzie AG, Butte NF. Heritability of Hyperphagic Eating Behavior and Appetite-Related Hormones among Hispanic Children. Obesity. 2007a;15:1484–1495. doi: 10.1038/oby.2007.177. [DOI] [PubMed] [Google Scholar]
- Fisher JO, Liu Y, Birch LL, Rolls BJ. Effects of portion size and energy density on young children's intake at a meal. The American Journal of Clinical Nutrition. 2007b;86:174–179. doi: 10.1093/ajcn/86.1.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JO, Rolls BJ, Birch LL. Children’s bite size and intake of an entrée are greater with large portions than with age-appropriate or self-selected portions. The American Journal of Clinical Nutrition. 2003;77:1164–1170. doi: 10.1093/ajcn/77.5.1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis L, Birch L. Maternal weight status modulates the effects of restriction on daughters' eating and weight. International Journal of Obesity (2005) 2005;29:942. doi: 10.1038/sj.ijo.0802935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis LA, Ventura AK, Marini M, Birch LL. Parent overweight predicts daughters’ increase in BMI and disinhibited overeating from 5 to 13 years. Obesity. 2007;15:1544–1553. doi: 10.1038/oby.2007.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill TP. Introduction: an overview of the key drivers of obesity and their influence on diet. In: Gill T, editor. Managing and Preventing Obesity. Woodhead Publishing; 2015. [Google Scholar]
- Hill C, Llewellyn CH, Saxton J, Webber L, Semmler C, Carnell S, Van Jaarsveld C, Boniface D, Wardle J. Adiposity and'eating in the absence of hunger'in children. International Journal of Obesity. 2008;32:1499. doi: 10.1038/ijo.2008.113. [DOI] [PubMed] [Google Scholar]
- Jansen A, Theunissen N, Slechten K, Nederkoorn C, Boon B, Mulkens S, Roefs A. Overweight children overeat after exposure to food cues. Eating Behaviors. 2003;4:197–209. doi: 10.1016/S1471-0153(03)00011-4. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Birch LL. Parents' and children's adiposity and eating style. Pediatrics. 1994;94:653–61. [PubMed] [Google Scholar]
- Kling SM, Roe LS, Sanchez CE, Rolls BJ. Does milk matter: Is children’s intake affected by the type or amount of milk served at a meal? Appetite. 2016;105:509–518. doi: 10.1016/j.appet.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral TV, Allison DB, Birch LL, Stallings VA, Moore RH, Faith MS. Caloric compensation and eating in the absence of hunger in 5-to 12-y-old weight-discordant siblings. The American Journal of Clinical Nutrition. 2012;96:574–583. doi: 10.3945/ajcn.112.037952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansigan RK, Emond JA, Gilbert-Diamond D. Understanding eating in the absence of hunger among young children: A systematic review of existing studies. Appetite. 2015;85:36–47. doi: 10.1016/j.appet.2014.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Llewellyn C, Wardle J. Behavioral susceptibility to obesity: Gene-environment interplay in the development of weight. Physiology & Behavior. 2015;152:494–501. doi: 10.1016/j.physbeh.2015.07.006. [DOI] [PubMed] [Google Scholar]
- Mcallister EJ, Dhurandhar NV, Keith SW, Aronne LJ, Barger J, Baskin M, Benca RM, Biggio J, Boggiano MM, Eisenmann JC, Elobeid M, et al. Ten putative contributors to the obesity epidemic. Critical Reviews in Food Science and Nutrition. 2009;49:868–913. doi: 10.1080/10408390903372599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mccrickerd K, Forde CG. Parents, portions and potential distortions: Unpicking children's meal size. Nutrition Bulletin. 2016;41:67–71. [Google Scholar]
- Moens E, Braet C. Predictors of disinhibited eating in children with and without overweight. Behaviour Research and Therapy. 2007;45:1357–1368. doi: 10.1016/j.brat.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Nederkoorn C, Smulders F, Jansen A. Cephalic phase responses, craving and food intake in normal subjects. Appetite. 2000;35:45–55. doi: 10.1006/appe.2000.0328. [DOI] [PubMed] [Google Scholar]
- Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH. Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study) International Journal of Epidemiology. 2011;40:33–44. doi: 10.1093/ije/dyq180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakes ME, Slotterback CS. Self-reported measures of appetite in relation to verbal cues about many foods. Current Psychology. 2000;19:137. [Google Scholar]
- Phenxtoolkit. https://www.phenxtoolkit.org.
- Quah PL, Ng C, Fries LR, Chan MJ, Aris IB, Lee YS, Yap F, Godfrey KM, Gluckman PD, Chong Y, Shek LPC, et al. Bidirectional associations between maternal feeding practices and body mass index (BMI): a study in Asian Singaporean preschoolers. doi: 10.3389/fnut.2019.00032. Under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage JS, Haisfield L, Fisher JO, Marini M, Birch LL. Do children eat less at meals when allowed to serve themselves? American Journal of Clinical Nutrition. 2012;96:36–43. doi: 10.3945/ajcn.112.035261. [DOI] [PubMed] [Google Scholar]
- Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. Journal of the American Dietetic Association. 2004;104:1120–1126. doi: 10.1016/j.jada.2004.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh SE, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, Stunkel W, Holbrook JD, Kwek K, Chong YS, Saw SM. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. International Journal of Epidemiology. 2014;43:1401–9. doi: 10.1093/ije/dyt125. [DOI] [PubMed] [Google Scholar]
- Steenhuis IH, Vermeer WM. Portion size: review and framework for interventions. International Journal of Behavioral Nutrition and Physical Activity. 2009;6:58. doi: 10.1186/1479-5868-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, Yanovski JA. Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite. 2008;51:148–155. doi: 10.1016/j.appet.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Strien T, Oosterveld P. The children's DEBQ for assessment of restrained, emotional, and external eating in 7- to 12-year-old children. International Journal of Eating Disorders. 2008;41:72–81. doi: 10.1002/eat.20424. [DOI] [PubMed] [Google Scholar]
- Wallis DJ, Hetherington MM. Stress and eating: the effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite. 2004;43:39–46. doi: 10.1016/j.appet.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Wang Y, Chen H-J. Handbook of anthropometry. Springer; 2012. Use of percentiles and z-scores in anthropometry. [Google Scholar]
- Wardle J, Llewellyn C, Sanderson S, Plomin R. The FTO gene and measured food intake in children. International Journal of Obesity. 2009;33:42–5. doi: 10.1038/ijo.2008.174. [DOI] [PubMed] [Google Scholar]
- WHO. Child Growth Standards. [Accessed 01.06.2016];2003 [Online]. Available: http://www.who.int/childgrowth/standards/Technical_report.pdf.
- Wilkinson LL, Hinton EC, Fay SH, Ferriday D, Rogers PJ, Brunstrom JM. Computer-based assessments of expected satiety predict behavioural measures of portion-size selection and food intake. Appetite. 2012;59:933–938. doi: 10.1016/j.appet.2012.09.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.