Abstract
The current study examined micro RNA (miRNAs) clusters from the maternal plasma to determine their association with preterm birth (PTB) and infant birth outcomes. A subsample of 42 participants who spontaneously delivered either preterm (≤37 weeks) or term was selected from a parent sample of 515 pregnant Mexican American women. Plasma samples and prenatal data were collected at a single mid-gestation time point (22–24 weeks’ gestation) and birth outcomes were obtained from medical records after delivery. Circulating miRNAs were analyzed by qPCR. When miRNAs were grouped according to chromosomal cluster rather than expression level, individual miRNAs correlated strongly with other individual miRNAs within their respective genomic locus. miRNAs from the c19mc cluster negatively correlated with c14mc miRNAs, and this relationship was more pronounced in PTB. Clusters c14mc was negatively associated with length of gestation; while the c19mc was positively associated with length of gestation and infant head circumference. Together, these findings suggest that groups of miRNAs from common chromosomal clusters, rather than individual miRNAs, operate as co-regulated groups of signaling molecules to coordinate length of gestation and infant outcomes. From this evidence, differences in cluster-wide expression of miRNAs are involved in spontaneous PTB.
Introduction
Preterm birth (PTB), or gestational length ≤37 weeks, is probably the most significant obstetrical problem we currently face. Babies born too soon and too small often have multiple problems such as respiratory problems, intraventricular hemorrhages, necrotizing colitis and neurodevelopmental delays [1]. PTB is currently the primary reason for newborn mortality [2]. The primary monetary costs of PTB total to approximately $26 billion per year in the U.S. [1]. However, the secondary burdens of PTB may be even greater due to the lifelong health impact of premature birth [3]. Thus despite ongoing research, further understanding of the multifactorial etiologies that may affect PTB and related poor birth outcomes is still vitally needed. Scientists need to contemplate multiple risk factors and pathways leading to PTB—as well as their interactions [4]. One particular area of interest related to the etiology of PTB has recently been focused on epigenetics (for which microRNAs are a portion) [4,5]. The origins of PTB may be from complex gene-environment interactions. We present our results using a new methodology to examine microRNAs (miRNAs) as part of a pathway related to gestational age, PTB, and deleterious infant outcomes such as low birth weight and smaller head circumference.
miRNAs are small, non-coding RNAs that post-transcriptionally regulate gene expression that are implicated in numerous biological pathways and pathologies, including those of PTB [6]. A number of studies have focused on the involvement of miRNAs in specific medical conditions that significantly overlap with PTB, including, preeclampsia, intrauterine growth restriction, and fetal alcohol syndrome (FAS-D) [6–9]. Studies focusing specifically on PTB have identified individual miRNAs within the maternal circulation or within specific reproductive tissues such as placenta [5–7, 10]. While promising, the emerging literature on miRNA and pregnancy complications (including PTB) has also produced inconsistent results that can be attributed to differing tissues sources, quantitative methodologies and analytical strategies across studies and between research groups [7].
Another potential source of inconsistent results is due to the preponderance of studies that focus on the analysis of miRNAs as individual elements rather than functional groups. Throughout the genome, individual miRNAs are found as groups or “clusters” that are co-localized within distinct chromosomal loci. As such, miRNA clusters share common regulatory elements, that coordinate the synchronized expression of groups of individual miRNAs [11–12]. Moreover, miRNA clusters often share common target motifs that overlap across other functional gene networks. This enables clusters to influence other biological pathways through post-transcriptional regulation of not just one but several genes within a common network. As such, analytical approaches that represent miRNAs as functional groups of signaling molecules may provide results that reconcile the inconsistencies of previous studies.
Despite the ubiquitous involvement of miRNA in biological and disease pathways, a few miRNA clusters are selectively associated with pregnancy, pregnancy complications, and birth outcomes, most notably the c14mc, c19mc clusters [6,7]. miRNAs from the c14mc and c19mc clusters share a few important characteristics in that they are: 1) predominantly produced by the placenta, 2) detectable in the maternal circulation throughout gestation and 3) rapidly disappear from the maternal circulation following pregnancy termination [6–7, 13–15]. As demonstrated by clinical and in vitro studies, these clusters also show differing temporal expression patterns across pregnancy, wherein c14mc miRNA levels decrease from 1st to 3rd trimester and c19mc miRNA levels increase during this time [13, 16]. As circulating miRNA levels correspond to tissue expression [17], parallel c14mc and c19mc miRNA expression trajectories are likely present in the maternal plasma across pregnancy. Interestingly, c14mc and c19mc are the largest known miRNA clusters in the human genome, each consisting of 46 or more individual miRNAs located in distinct regions (40-100kb segments) on chromosomes 14 and 19, respectively [18–22]. Thereby, circulating c14mc and c19mc miRNAs potentially represent large functional groups of signaling molecules with selective involvement in pregnancy.
Indeed, empirical studies on plasma samples collected during mid-gestation have demonstrated the involvement of individual miRNAs from the c14mc and c19mc clusters in pregnancy outcomes and complications such as PTB or preeclampsia [7]. These effects were observed in plasma samples collected during the 1st trimester [23] as well as mid-gestation [5]. Mid- and late-gestation sampling and analysis of groups circulating miRNAs that included individual members of c14mc and c19mc clusters has also demonstrated altered expression in pregnancies resulting in Fetal Alcohol Syndrome, a behavioral health condition that considerably overlaps with PTB [9].
As, investigations into circulating miRNA and prenatal health have focused primarily on individual miRNAs rather than clusters of miRNAs and have often investigated pathologies that overlap PTB, we propose that cluster-level analysis in pregnancies resulting in spontaneous PTB (without major coinciding complications) will more clearly characterize relationships between circulating miRNA, PTB, and associated infant outcomes. Therefore, the current study sought to 1) investigate cluster-wide associations of pregnancy specific miRNA with length of gestation and birth outcomes and 2) examine whether differences in coordinated expression of circulating miRNA were associated with PTB.
Methods
The current study was conducted in a subset of a parent study (n = 515) on pregnant Hispanic women recruited at two obstetrical clinics in the Houston metropolitan areas from 2008–2012 [24]. The subsample (n = 42) consisted of patients who spontaneously delivered before the completion of 37 gestational weeks (PTB; n = 21) and patients who spontaneously delivered after 37 weeks (Term; n = 21). Selected cases of PTB and term pregnancy were matched for age, gravidity, and BMI. Enrollment criteria included patients who: were between the ages 19 and 39; self-identified as Hispanic; had the ability to read and speak English and/or Spanish; were born in the U.S. or had lived in the U.S. for 10 or more years; were covered by self-pay, state funded or private insurance. Exclusion criteria included: pregnancies with twins or multiple fetuses; medical risk factors such as chronic hypertension, type I or II diabetes, gestational diabetes with insulin treatment, thyroid disorder; major psychiatric disorders (e.g. Bipolar Disorder, Schizophrenia); use of steroids or antidepressants one month prior to enrollment; fetal or uterine anomalies as determined by ultrasound; fetal demise; placenta previa, preeclampsia at time of data collection; cerclage.
Data were collected between 22–24 weeks’ gestation during an appointment with a research nurse separately scheduled from regular prenatal care visits. Venipuncture blood draws (20ml) were collected by between 2 and 4 pm to control for diurnal variation. Immediately following blood collection, all samples were centrifuged and plasma was separated and aliquoted for storage at -80°. Prenatal data was collected from prenatal records for age, gravidity, and BMI and history of PTB. Protocols for this study were approved by the institutional review boards at The University of Texas Medical Branch, Galveston, TX and The University of Texas at Austin.
miRNA analysis
Plasma samples were thawed and centrifuged at 3000 x g for 5 minutes. For each sample, a 200μl aliquot was transferred to a microtube and combined with a lysis buffer containing 1μg carrier RNA per 60μl buffer. Total RNA was extracted using miRCury RNA isolation kit (Exiqon, Woburn, MA). Each miRNA sample was reverse transcribed into cDNA and run on miRCURY LNATM Universal RT microRNA PCR Human Panels 1&2 (Exiqon, Woburn, MA). Raw CT values were subject to quality control checks for hemolysis [9]. Cycle thresholds (CTs) were considered un-amplified if CT values > 50. -∆CTs for each individual miRNA in each sample was normalized to the mean CT for all miRNAs in that particular sample (e.g. globalized miRNA expression) and calculated as (CTmiRNA_x-CTAverage_miRNA_Expression). In a previous study, we demonstrated that globalized miRNA expression within maternal plasma is unaffected by experimental condition [9].
miRNA clusters
miRNA clusters were classified as groups of individual miRNAs within 10kb on the same chromosome via mirbase.org [25]. Specifically, miRNAs from the c14mc cluster were defined as individual miRNA located at position 14q32. on chromosome 14, and c19mc miRNAs were selected from position 19q13.41 on chromosome 19. miRNAs from the family cluster miR-17/92 were located within a 10kb proximity on chromosome 13, position 13q31.1 and another group of these miRNA were chromosomally co-localized on the X chromosome, position Xq26.2 [26]. For inclusion in statistical analysis, individual miRNAs had to be detected in a minimum of 30/42 patient samples; miRNAs that fell below this threshold were excluded from the present analyses. A list of each individual miRNA used for cluster variables is provided in S1 Table.
Statistical analysis
Initial analysis compared individual miRNAs expressed as -∆CTs between term and PTB pregnancies by t-test. Additionally, correlational analysis for individual miRNAs within and between chromosomal clusters was conducted using Pearson’s.
To examine potential differences in cluster-wide expression patterns between term and PTB samples we compared correlation matrices of individual miRNA expression levels grouped by genomic location. For each chromosomal cluster, we created a correlation matrix of the -∆CTs between each miRNA within that particular genomic location using values from only term or only PTB samples. Correlation coefficients from term or PTB samples were compared statistically by the Jennrich test [27], which tests the equality of two matrices. As the sets of coefficients followed normal distributions, we also used one-way ANOVA with pairwise comparisons to determine if a significant difference existed between the two groups.
Factor analysis using minimum residual exploratory factor analysis (EFA) was performed in R (R Core Team (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/)., using the psych package (Revelle, W. (2017) psych: Procedures for Personality and Psychological Research, Northwestern University, Evanston, Illinois, USA, https://CRAN.R-project.org/package=psych Version = 1.7.5). The number of dimensions to extract was determined by examining Bayesian Information Criteria (BIC) and with parallel analysis, which compares the observed eigenvalues of the correlation matrix with those from simulated data with similar properties to the actual data [28]. The factor solution was rotated into an oblique solution using the oblimin transformation to simplify interpretation while preserving correlation structure (S2 Table). Factor variables were constructed by row means for each miRNA from a respective cluster. miRNA Factor variables were then used to assess differences in gestational age at birth between term and preterm deliveries. Each matched pair of women was assigned an ID number which was used as a random factor in linear or logistic mixed regression models. Fixed factors in these models included gestational age at birth, and miRNA cluster variables. Additionally, fetal sex, history of PTB, gravida, and pre-pregnancy BMI, factors known to pregnancy outcomes, were included as covariates. Results were considered significant if the p-value for the interaction between the acculturation measure and cluster variable were below 0.05.
Each t-test, ANOVA, linear mixed-effects model, and Pearson’s correlation was assessed with the significance level at 0.05. Data were analyzed using Stata 14 Software (StataCorp 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).
Results
Sample characteristics
Table 1 illustrates that differences in length of gestation between term and PTB cases were unlikely due to medical complications (e.g. preeclampsia) that are often factors for PTB. Additionally, term and PTB cases did not significantly differ in demographic characteristics (e.g. age, pre-pregnancy BMI, income). While the parent sample included patients from Houston and Austin, the subsample selected for this study only included patients from the Houston area to avoid confounding factors possibly associated with geographic region. Patients who had a history of PTB were in both the term and PTB groups, however, none of these patients received progesterone treatment during their prenatal care.
Table 1. Sample characteristics (frequency or mean ± SD).
| Total (n = 42) | Term (n = 21) | Preterm (n = 21) | |
|---|---|---|---|
| Demographics | |||
| Age | 26.25 ± 5.05 | 26.3 ± 4.8 | 26.2 ± 5.3 |
| Pre-Pregnancy BMI | 25.7 ± 5.35 | 25.8 ± 5.5 | 25.6 ± 5.2 |
| Cotinine Positive | 2 | 1 | 1 |
| Pregnancy Outcomes | |||
| Spontaneous Delivery | 42 | 21 | 21 |
| Gestational Age at Birth (Weeks) | 36.9 ± 1.6 | 38.6 ± 0.7 | 35.3 ± 2.4 |
| Birthweight (g) | 2852 ± 410.1 | 3114 ± 286.5 | 2590 ± 533.6 |
| Infant Head Circumference (cm) | 32.6±1.8 | 33.1±1.2 | 32.1±2.2 |
| Preeclampsia | 0 | 0 | 0 |
| Chorioamnionitis | 0 | 0 | 0 |
| Preterm PROM | 0 | 0 | 0 |
| Diabetes (GDM or PGDM) | 0 | 0 | 0 |
| Placental Abruption | 0 | 0 | 0 |
| Maternal History | |||
| Gravida | |||
| 1 Pregnancy | 7 | 3 | 4 |
| 2 Pregnancies | 7 | 3 | 4 |
| 3 Pregnancies | 16 | 10 | 6 |
| 4+ Pregnancies | 12 | 5 | 7 |
| History of PTB | 10 | 3 | 7 |
| Progesterone Treatment | 0 | 0 | 0 |
miRNA
Individual expression
Initial comparisons of individual miRNA expression showed differences between term and PTB compared by t-test (S1 Table) for three miRNAs from c14mc: miRNAs hsa-mir-127-3p and hsa-mir-136-5p from the RTL subregion of c14mc and hsa-mir-543 located in a broader region of the c14mc cluster. No other group differences were observed between term and PTB samples for any other individual miRNAs from the c14mc cluster; nor were any group difference observed between individual miRNAs from the c19mc or miR-17/92 cluster. Total miRNA expression did not differ between term and PTB samples [t(39) = 0.09; p = 0.9]
Expression by chromosomal clusters
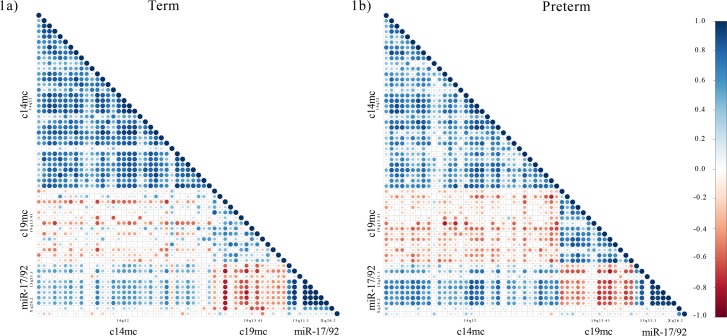
To examine the relationship between expression levels of miRNAs within chromosomal clusters and between miRNAs from separate genomic loci, we performed correlational analysis using Pearson’s correlation. Consistently positive correlations were observed between miRNAs and the other miRNAs from the same chromosomal clusters. Negative correlations were observed in expression levels between c19mc miRNA and miRNAs from all other clusters (c14mc, and miR-17/92 located on chromosome 13 and the X chromosome). The positive correlations of miRNA with other miRNAs from the same chromosomal cluster is most apparent when a correlation matrix was organized according to genomic location (Fig 1). A correlation matrix that organized miRNA expression levels from highest to lowest, regardless, of genomic location, revealed no specific pattern of expression.
Fig 1. Correlations plots of individual miRNAs (-∆CTs) from clusters c14mc, c19mc, and miR-17/92.
Individual miRNAs were grouped according to cluster and ordered within according to genomic position clusters. Pearson’s correlation analysis was performed for individual miRNAs -∆CTs for term (A) and preterm (B) separately. Positive and negative Pearson’s r coefficients are represented by blue and red dots, respectively.
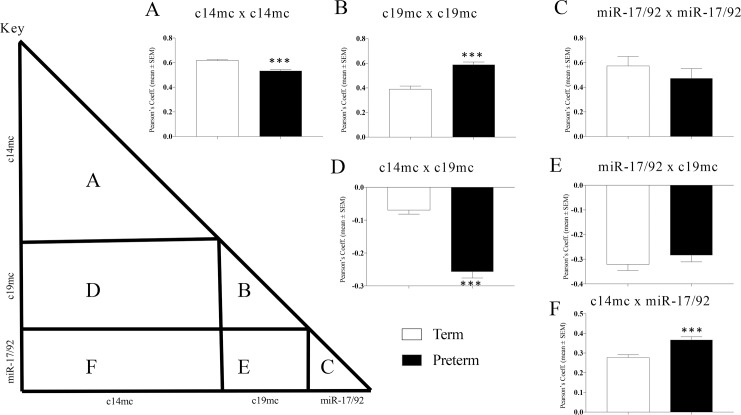
To further investigate patterns of co-expression, correlation matrices were created using either samples only from term (Fig 1A) or PTB (Fig 1B) deliveries. For within cluster correlations, c14mc miRNA were significantly more positively correlated with each other in plasma collected in term pregnancies than in PTB samples [F(1,1188) = 45.96; p<0.001] (Fig 2A). Co-expression of c19mc miRNAs with each other was significantly more positively correlated in PTB samples than in term samples [F(1,208) = 37.83; p<0.001] (Fig 2B). We observed no differences in the average correlation between miR-17/92 between term and PTB samples [F(1,88) = 2.95; p = 0.09] (Fig 2C). For between cluster comparisons, the mean negative correlation between c14mc and c19mc miRNA was significantly greater in PTB as compared to term samples [F(1,1019) = 160.24; p<0.001] (Fig 2D). Correlations between c19mc and miR-17/92 miRNAs did not differ between term and PTB [F(1,310) = 1.12; p = 0.29] (Fig 2E). However, higher correlations between c14mc miRNAs and miR-17/92 miRNAs located were detected in PTB samples [F(1,678) = 19.22; p>0.001] (Fig 2F).
Fig 2. miRNA correlation comparisons between PTB and term cases.
Average correlations between individual miRNAs were compared between term and PTB to evaluate differences in coordinated expression of miRNA clusters c14mc, c19mc, and miR-17/92. Regions of each respective term and PTB correlation matrices that corresponded to within cluster correlations (A-C) and between clusters correlations (D-F) were compared by ANOVA (Fig 2 key provides a visual guide for which areas of the matrices were compared between term and PTB). (A) PTB showed lower correlated expression of c14mc miRNAs and (B) higher correlated expression of c19mc miRNAs. (C) Within cluster correlations for miR-17/92 miRNAs did not differ between term and PTB. (D) Negative correlations between c14mc and c19mc miRNAs was stronger in PTB, while (E) the negative correlations between miR-17/92 and c19mc miRNAs did not differ between term and PTB. (F) PTB showed stronger correlations between c14mc and miR-17/92 miRNAs. Correlations were calculated using Pearson’s correlation coefficient. *** = p<0.001; ANOVA.
Factor analysis and miRNA cluster variables
Correlation plots using all miRNAs from c14mc, c19mc and miR-17/92 for each patient (Term or PTB) indicated that miRNA expression was coordinated by genomic location (Fig 1). We also observed consistent positive correlations between individual miRNAs from the c14mc and miR-17/92 clusters and birth outcomes (length of pregnancy, birth weight, and infant head circumference) (Table 2). Similarly, we observed consistent negative correlations between c19mc miRNAs and birth outcomes, indicating that high c19mc expression is related to pregnancies that are longer in duration as well as greater infant birth weight head circumference. A separate correlation matrix that ranked miRNA from high to low expression, regardless of genomic location, showed no distinct patterns (S1 Fig). In this correlation plot, individual c14mc miRNAs that were more highly expressed in PTB samples (hsa-mir-127-3p, hsa-mir-136-5p, and hsa-mir-543) were randomly interspersed between miRNAs from clusters c19mc and miR-17/92. A correlation matrix consisting of miRNA grouped by expression rank rather than genomic location revealed no cohesive pattern or relationship with any other birth outcomes.
Table 2. Correlations between individual miRNAs birth outcomes.
| miRNA | Cluster | Pregnancy Duration | Birth Weight | Infant Head Size |
|---|---|---|---|---|
| hsamir4935p | c14mc | 0.1494 | 0.1916 | 0.3751* |
| hsamir3373p | c14mc | 0.3281* | 0.3486* | 0.2178 |
| hsamir3375p | c14mc | 0.1995 | 0.2899 | 0.1657 |
| hsamir4315p | c14mc | 0.2927 | 0.31* | 0.2913 |
| hsamir4333p | c14mc | 0.2480 | 0.1654 | 0.1561 |
| hsamir1273p | c14mc | 0.471* | 0.3522* | 0.3159 |
| hsamir4325p | c14mc | 0.2294 | 0.2739 | 0.3748* |
| hsamir1363p | c14mc | 0.2975 | 0.3458* | 0.1760 |
| hsamir1365p | c14mc | 0.4058* | 0.3574* | 0.2689 |
| hsamir3793p | c14mc | 0.3024 | 0.3190 | 0.1204 |
| hsamir3795p | c14mc | 0.1462 | 0.1145 | 0.2870 |
| hsamir3803p | c14mc | 0.3409 | 0.4181* | 0.4425* |
| hsamir323a3p | c14mc | 0.323* | 0.3335* | 0.1944 |
| hsamir3293p | c14mc | 0.1518 | 0.1969 | 0.0764 |
| hsamir4943p | c14mc | 0.1201 | 0.2690 | 0.3952* |
| hsamir543 | c14mc | 0.3476* | 0.379* | 0.2961 |
| hsamir4953p | c14mc | 0.3496* | 0.2913 | 0.3197* |
| hsamir376c3p | c14mc | 0.3074* | 0.2860 | 0.3002 |
| hsamir376a3p | c14mc | 0.2851 | 0.2930 | 0.2769 |
| hsamir376a5p | c14mc | 0.3339* | 0.2600 | 0.1940 |
| hsamir6543p | c14mc | 0.2114 | 0.2860 | 0.2169 |
| hsamir376b3p | c14mc | 0.2694 | 0.2561 | 0.2458 |
| hsamir3813p | c14mc | 0.1016 | 0.2328 | 0.0182 |
| hsamir487b3p | c14mc | 0.2511 | 0.2374 | 0.2072 |
| hsamir8893p | c14mc | 0.2071 | 0.2439 | 0.3329 |
| hsamir3823p | c14mc | 0.1295 | 0.2353 | 0.1619 |
| hsamir1345p | c14mc | 0.2274 | 0.2117 | 0.2027 |
| hsamir496 | c14mc | 0.3629 | 0.2826 | 0.1404 |
| hsamir3773p | c14mc | 0.2303 | 0.2813 | 0.1999 |
| hsamir4093p | c14mc | 0.2637 | 0.2649 | 0.2713 |
| hsamir3693p | c14mc | 0.2028 | 0.2489 | 0.2080 |
| hsamir3695p | c14mc | 0.2608 | 0.3352 | 0.1564 |
| hsamir4103p | c14mc | 0.2520 | 0.1924 | 0.1176 |
| hsamir5153p | c19mc | -0.0583 | -0.0541 | -0.2190 |
| hsamir5155p | c19mc | -0.1079 | -0.0454 | -0.1140 |
| hsamir520a5p | c19mc | -0.1380 | -0.2998 | -0.4409* |
| hsamir5255p | c19mc | -0.0995 | -0.1893 | -0.3597* |
| hsamir518f5p | c19mc | -0.2525 | -0.2322 | -0.3668* |
| hsamir520c3p | c19mc | -0.1809 | -0.0622 | -0.2170 |
| hsamir518c3p | c19mc | -0.0860 | -0.0833 | -0.2413 |
| hsamir518c5p | c19mc | -0.0499 | -0.1059 | -0.2282 |
| hsamir5243p | c19mc | -0.3067 | -0.2615 | -0.5219** |
| hsamir5245p | c19mc | -0.2000 | -0.2513 | -0.3533* |
| hsamir517a3p | c19mc | -0.0828 | -0.1044 | -0.2788 |
| hsamir519d3p | c19mc | -0.1789 | -0.1978 | -0.1910 |
| hsamir518d5p | c19mc | -0.1760 | -0.1988 | -0.4283** |
| hsamir519a3p | c19mc | -0.1913 | -0.2221 | -0.4493** |
| hsamir173p | miR-17/92 | -0.1043 | -0.1378 | 0.0817 |
| hsamir175p | miR-17/92 | 0.0675 | 0.0655 | 0.2355 |
| hsamir18a3p | miR-17/92 | -0.0933 | -0.1150 | 0.0010 |
| hsamir18a5p | miR-17/92 | 0.1267 | 0.0728 | 0.341* |
| hsamir19a3p | miR-17/92 | 0.1181 | 0.1077 | 0.3347* |
| hsamir20a5p | miR-17/92 | 0.0769 | 0.0180 | 0.3375* |
| hsamir106a5p | miR-17/92 | 0.1036 | 0.0360 | 0.348* |
| hsamir18b5p | miR-17/92 | 0.1591 | 0.0931 | 0.3647* |
| hsamir20b5p | miR-17/92 | 0.0091 | 0.0846 | 0.2117 |
| hsamir3633p | miR-17/92 | -0.0637 | -0.0048 | 0.1495 |
Pearson's Correlation
* = p<0.05
** = p<0.01
Factor analysis confirmed observation miRNAs are better grouped by cluster than by up- or down-regulation, as individual miRNAs loaded on to latent variables that corresponded to genomic location rather than expression level (S2 Table). Individual miRNAs from c14mc, c19mc, and miR-17/92 loaded onto factors consisting of primarily miRNAs from the same respective cluster. We then created three factor variables for miRNA clusters using row means of the -∆CT for individual miRNAs within a respective chromosomal cluster: c14mc c19mc and miR-17/92. This approach accounted for any potential missing values resulting from miRNAs that were undetectable in a given patient’s sample. For c14mc, a cluster variable was created that consisted of each miRNA from c14mc, genomic location 14q32. For c19mc, a whole cluster variable was created that included all miRNAs from c19mc, genomic location 19q13.41. For the miR-17/92, a variable was created that included all miRNAs from this sequence-based cluster either 13q31.3 or Xq26.2 [26].
We then tested the ability of each factor variable cluster of miRNAs for association with birth outcomes (length of gestation, birth weight, and infant head circumference) in mixed model regressions with paired cases set as a random factor (Results summarized in Table 3). We controlled for pre-pregnancy BMI, gravida, history of PTB, and fetal sex by using these variables as covariates in each regression model. The c14mc cluster positively predicted length of gestation at birth with positive regression coefficients. Because miRNA expression was expressed as -∆CT, the positive coefficient indicates that high c14mc expression is predictive of early spontaneous delivery and is consistent with correlational analysis. Regression models using each of the miR-17/92 and c19mc clusters variables were not statistically significant. The correlation coefficient between c19mc and length of gestation was negative, suggesting that low expression of individual c19mc miRNAs is associated with PTB. For infant birth outcomes, we did not find a significant relationship between the c14mc or miR-17/92 clusters with either birth weight or infant head circumference. A positive relationship between c19mc and infant head circumference, however, was detected. An additional linear regression model using only samples from term deliveries showed that the relationship between c19mc and head circumference was independent in differences in length of gestation or infant birthweight (R2 = 0.584, F(5,14) = 3.93, p<0.05).
Table 3. Summary Relationships between miRNA clusters, length of Gestation and Infant Outcomes.
| Mixed Model Regression for miRNA Clusters and Birth Outcomes | |||||
|---|---|---|---|---|---|
| Outcome | miRNA Cluster | Estimate | Std. Err | z | 95% C.I. |
| Length of Gestation | c14mc | 0.83* | 0.39 | 2.11 | 0.06–1.60 |
| c19mc | -0.66 | 0.4 | -1.64 | -1.30–0.13 | |
| miR-17/92 | 0.79 | 0.69 | 1.16 | -0.55–2.15 | |
| Infant Birthweight | c14mc | 189.21 | 86.25 | 2.19 | 20.16–358.25 |
| c19mc | -144.46 | 88.07 | -1.64 | -317.07–28.15 | |
| miR-17/92 | 106.25 | 153.73 | 0.69 | -195.05–407.55 | |
| Infant Head Circumference | c14mc | 0.62 | 0.32 | 1.99 | 0.008–1.25 |
| c19mc | -0.87* | 0.29 | -3.05 | -1.43–-0.31 | |
| miR-17/92 | 1.14 | 0.52 | 2.21 | 0.127–2.16 | |
Cluster variables based on chromosomal location were tested as predictors of birth outcomes (pregnancy duration, infant birth weight, and infant head circumference) by mixed model regression with pre-pregnancy BMI, infant sex, gravida, and history of PTB as control covariates. Statistical significance * = p<0.05 (bold).
Discussion
The first major finding of our current study is that pregnancy specific miRNAs within the maternal plasma are co-regulated based on chromosomal clustering at distinct genomic loci. Previous studies into PTB and other prenatal medical complications that focused on individual miRNAs or groups of miRNAs sorted by expression levels rather than genomic location have produced disparate results. Findings from the current study provide a novel perspective by examining cluster-wide associations between circulating miRNAs and birth outcomes. Still, our results are consistent with previous studies that have identified individual miRNAs or groups of miRNAs from the c14mc, c19mc, and miR-17/92 chromosomal clusters that are associated with pregnancies disorders, including PTB [5], pre-eclampsia [8, 23], and FAS-D [9].
The second major finding from our study is that differential expression of miRNA clusters c14mc and c19mc are predictive of PTB. Both correlational analysis and mixed model, multivariate regressions demonstrated that pregnancy duration is predicted by c14mc and c19mc miRNA expression patterns. In both term and PTB pregnancies, c14mc and c19mc expression are inversely related. This negative correlation between these miRNA clusters is most pronounced in pregnancies that resulted in spontaneous PTB. As such, these findings indicate the difference in pregnancies resulting in term or PTB may be related to an imbalance in c19mc and c14mc expression. It is important to note, that none of the patients in the current study developed preeclampsia or gestational hypertension or gave birth to infants with symptoms of FAS-D. As such, differential expression of c19mc miRNAs in our study is most likely due to decreased pregnancy duration, and not a result of overlapping pathologies.
The results that various clusters of miRNAs analyzed here are highly related to the infant birth outcomes of birth weight and head circumference is important. Several of the miRNAs are highly related to head circumference, especially in the c19mc cluster. These findings are not necessarily in concert with birth weight and gestational length, which is intriguing. This is potentially an important finding, considering that the relationship between c19mc miRNAs and head circumference is independent of length of gestation and is definitely worthy of follow up with the infants to see if this is then related to their future neurodevelopment.
In the current study, we included clinically-based observations known to influence prematurity (history of PTB, gravida, BMI and fetal sex) as covariates in regression models analyzing the relationship between miRNA clusters and PTB. Importantly, none of these clinical observations significantly influenced the statistical models used to analyze the relationship between c14mc and c19mc clusters and length of gestation. Further investigations are needed to address potential relationships between circulating miRNAs and previously identified biological and/or sociocultural risk factors for PTB.
The c14mc and c19mc miRNAs are groups of biomarkers that share several key characteristics. Due to genomic co-localization, c14mc and c19mc miRNAs share regulatory mechanisms intrinsic to their respective cluster. Consequently, these common regulatory elements may selectively influence the conditions under which c14mc and c19mc miRNAs are expressed as groups, specifically where (e.g. tissue or cell type) and when (e.g. developmental period). For example, both clusters are preferentially produced within the placenta and thus most abundantly present in the circulation during pregnancy [13–15], and both clusters are subject to genomic imprinting, as c14mc miRNAs are expressed exclusively from the maternal allele while c19mc miRNAs are solely expressed from the paternal allele [6]. Moreover, miRNAs from c14mc and c19mc may also act as coherent functional groups through shared and/or overlapping target motifs. Bioinformatics resources (Qiagen Ingenuity Pathway analysis and Targestscan.org) indicate that several members of c14mc target genes involved in estrogen receptor signaling and several members of the c19mc cluster target genes regulating the biosynthesis of steroid hormones including estrogen, progesterone, and cortisol [29, 30]. As such, coordinated expression of c14mc and c19mc miRNAs may serve to refine expression of genes within selective canonical pathways involved in pregnancy. Further studies will be required to determine if and how these biomarkers act as groups to influence known pathways of PTB or other adverse pregnancy outcomes.
The findings from this study demonstrate that a different methodology of analyzing miRNAs may prove to be very beneficial in understanding the pathway(s) leading to PTB and associated infant outcomes. This methodology indicates that the clusters of miRNAs (particularly c14mc and c19mc) may function in groups physiologically, and therefore the disparate results from other studies [5] may be explained by differences in the methodology by grouping miRNAs by expression rather than cluster. The strength of the reported study is that it was a case-controlled sample that only had spontaneous PTB and did not have mixed outcomes, such as early delivery due to preeclampsia. It also had a controlled sample as to ethnicity, all being Mexican Americans, without medical complications putting them at high risk. Another strength of the work is that the miRNAs were obtained from plasma samples.
Future work in patient populations with different ethnicities and sociocultural backgrounds will be important for assessing the generalizability of the present findings. In addition, a longitudinal study is needed to help understand differences in how the clusters of miRNA work over time in the pregnancy, both for term and PTBs. A larger sample would also be of benefit to confirm the results reported here and further explore how miRNA clusters are related to PTB risk factors such as history of PTB.
The study of circulating miRNAs as biomarkers for PTB is relatively nascent. Thus far, studies on miRNA and PTB widely vary in terms of experimental design, tissue source, method of quantification and interpretation of findings. As a result, the collective findings are inconsistent across studies [7]. Thus, we emphasize the need for further investigations to clarify relationships between circulating miRNAs and adverse pregnancy outcomes.
Supporting information
(A) Correlation matrix of individual miRNAs from c14mc, c19mc, and miR-17/92 clusters grouped ordered according to expression (highest to lowest -∆CT) rather than cluster or genomic location. Rows for correlations for select individual miRNAs from the c14mc and c19mc cluster are highlighted in yellow. (B) Correlations between individual miRNAs (ranked by -∆CT) and birth outcomes: length of gestation, birth weight, and infant head circumference. Displayed correlation matrix was analyzed using the whole sample of 42 patients who delivered spontaneous either term (n = 21) or preterm (n = 21). Positive and negative Pearson’s r coefficients are represented by blue and red dots, respectively.
(TIFF)
(XLSX)
(XLSX)
Acknowledgments
We would like to thank Alexander Tseng, Rutu Patel, and Dr. Amanda Mahnke for their thoughtful comments on this manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by an NIH grant (R01NR0107891) awarded to R.J. Ruiz. Microgen Labs LLC provided funding in the form of salaries for author [RS] but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific role of this author is articulated in the ‘author contributions’ section.
References
- 1.Behrman RE, Butler AS. Preterm birth: causes, consequences, and prevention Washington DC: National Academies Press; 2007. [PubMed] [Google Scholar]
- 2.Ashton D. Prematurity-infant mortality: the scourge remains. Ethn Dis 2006; 16(Suppl 3):58–62. [PubMed] [Google Scholar]
- 3.Barker DJ, Eriksson JG, Forsen T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. Int J Epidemiol. 2002; 31(6):1235–9. [DOI] [PubMed] [Google Scholar]
- 4.Romero R, Dey SK, Fisher SJ (2014) Preterm labor: one syndrome, many causes. Science 2014; 345(6198):760–5. doi: 10.1126/science.1251816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elovitz MA, Anton L, Bastek J, Brown AG Can microRNA profiling in maternal blood identify women at risk for preterm birth? Am J Obstet Gynecol 2015; 212(6):782 e781–785. [DOI] [PubMed] [Google Scholar]
- 6.Morales-Prieto DM, Markert UR. MicroRNAs in pregnancy. J Reprod Immunol 2011;88(2):106–111. doi: 10.1016/j.jri.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 7.Morales-Prieto DM, Ospina-Prieto S, Schmidt A, Chaiwangyen W, & Markert UR (2014) Elsevier Trophoblast Research Award Lecture: origin, evolution and future of placenta miRNAs. Placenta 35 Suppl:S39–45. doi: 10.1016/j.placenta.2013.11.017 [DOI] [PubMed] [Google Scholar]
- 8.Zhu XM, Han T, Sargent IL, Yin GW, Yao YQ. Differential expression profile of microRNAs in human placentas from preeclamptic pregnancies vs normal pregnancies. Am J Obstet Gynecol 2009; 661:e1–7. [DOI] [PubMed] [Google Scholar]
- 9.Balaraman S, Schafer JJ, Tseng AM, Wertelecki W, Yevtushok L, Zymak-Zakutnya N, et al. Plasma miRNA profiles in pregnant women predict infant outcomes following prenatal alcohol exposure. PLoS One. 2016; 11(11):e0165081 doi: 10.1371/journal.pone.0165081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams KC, Renthal NE, Condon JC, Gerard RD, & Mendelson CR. MicroRNA-200a serves a key role in the decline of progesterone receptor function leading to term and preterm labor. Proc Natl Acad Sci U S A 2012; 109(19):7529–7534. doi: 10.1073/pnas.1200650109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Altuvia Y, Landgraf P, Lithwick G, Elefant N, Pfeffer S, Aravin A, et al. Clustering and conservation patterns of human microRNAs. 2005; Nucleic Acids Res 33(8):2697–2706. doi: 10.1093/nar/gki567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsochandaridis M, Nasca L, Toga C, Levy-Mozziconacci A. Circulating microRNAs as clinical biomarkers in the predictions of pregnancy complications. Biomed Res Int. 2015; 2015:2949–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morales-Prieto DM, Ospina-Prieto S, Chaiwangyen W, Schoenleben M, Markert UR. Pregnancy-associated miRNA-clusters. J Reprod Immunol. 2013; 97(1):51–61. doi: 10.1016/j.jri.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 14.Miura K, Miura S, Yamasaki K, Higashihima A, Kinoshita A, Yoshiura K, et al. , Identification of pregnancy-associated microRNAs in maternal plasma. Clin Chem. 2010; 56(11):1767–71. doi: 10.1373/clinchem.2010.147660 [DOI] [PubMed] [Google Scholar]
- 15.Kotlabova K, Doucha J, Hromadnikova I. Placental-specific microRNA in maternal circulation—identification of appropriate pregnancy-associated microRNAs with diagnostic potential. J Reprod Immunol. 2011; 89(2):185–191. doi: 10.1016/j.jri.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 16.Hromadnikova I, Kotlabova K, Doucha J, Dlouha K, Krofta L. Absolute and relative quantification of placenta-specific microRNAs in maternal circulation with placental insufficiency-related complications. J Mol Diagn. 2012; 14(2):160–7. doi: 10.1016/j.jmoldx.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 17.Yang S, Li H, Ge Q, Guo L, & Chen F. Deregulated microRNA species in the plasma and placenta of patients with preeclampsia. Mol Med Rep. 2015; 12(1):527–34. doi: 10.3892/mmr.2015.3414 [DOI] [PubMed] [Google Scholar]
- 18.Seitz H, Royo H, Bortolin ML, Lin SP, Ferguson-Smith AC, Cavaille J. A large imprinted microRNA gene cluster at the mouse Dlk1-Glt2 domain. Genome Res. 2004; 14(9):1741–8. doi: 10.1101/gr.2743304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S, Barad O, et al. , Identification of hundreds of conserved and nonconserved human microRNAs. Nat. Genet. 2005; 37(7):766–70. doi: 10.1038/ng1590 [DOI] [PubMed] [Google Scholar]
- 20.Bortolin-Cavaille ML, Dance M, Weber M, Cavaille J. C19MC microRNAs are processed from introns of large Pol-11, non-protein-coding transcripts. Nucleic Acids Res. 2009; 37(10):3464–73. doi: 10.1093/nar/gkp205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin S, Cheung WK, Chen S, Lu G, Wang Z, Xie D, et al. Computational identification and characterization of primate-specific microRNAs in human genome. 2010; Comput Biol Chem. 34(4):232–41. doi: 10.1016/j.compbiolchem.2010.08.001 [DOI] [PubMed] [Google Scholar]
- 22.Gardiner E, Beveridge NJ, Wu JQ, Carr V, Scott RJ, Tooney PA, et al. , Imprinted DLK1-DIO3 region of 14q32 defines a schizophrenia-associated miRNA signature in peripheral blood mononuclear cells. Mol. Psychiatry 2012; 17(8):827–40. doi: 10.1038/mp.2011.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hromadnikova I, Kotlabova K, Ivankova K, Krofta L. First trimester screening of circulating C19MC microRNAs and the evaluation of their potential to predict the onset of preeclampsia and IUGR. PLoS One. 2017; 12(2):e0171756 doi: 10.1371/journal.pone.0171756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruiz RJ, Dwivedi AK, Mallawaarachichi, Balcazar HG, Stowe RP, Ayers KS, et al. , Psychological, cultural and neuroendocrine profiles of risk for preterm birth. BMC Pregnancy Childbirth 2015; 15:204 doi: 10.1186/s12884-015-0640-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kozomara A, Griggiths-Jones S. MiRBase: integrating microRNA annotation and deep sequencing data. Nucleic Acids Res. 2010; 39:D152–7. doi: 10.1093/nar/gkq1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mogilyansky E, Rigoutsos I. The miR-17/92 cluster: a comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ. 2013; 20(2):1603–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jennrich Robert I. An asymptotic χ^2 test for the equality of two correlation matrices. J Am Stat Assoc. 1970; 65: 904–12. [Google Scholar]
- 28.Hayton JC, Allen DG, Scarpello V. Factor retention decisions in Exploratory factor analysis: a tutorial on parallel analysis. Organ Res Meth. 2004; 7(2):191–205. [Google Scholar]
- 29.miRNA target genes and pathways were identified through the use of IPA (QIAGEN Inc., https://www.qiagenbioinformatics.com/products/ingenuity-pathway-analysis).
- 30.Agarwal V, Bell G, Jin-Wu N, Bartel DP. Predicting effective target sites in mammalian mRNAs. eLife. 2015; 4:e05005. Published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Correlation matrix of individual miRNAs from c14mc, c19mc, and miR-17/92 clusters grouped ordered according to expression (highest to lowest -∆CT) rather than cluster or genomic location. Rows for correlations for select individual miRNAs from the c14mc and c19mc cluster are highlighted in yellow. (B) Correlations between individual miRNAs (ranked by -∆CT) and birth outcomes: length of gestation, birth weight, and infant head circumference. Displayed correlation matrix was analyzed using the whole sample of 42 patients who delivered spontaneous either term (n = 21) or preterm (n = 21). Positive and negative Pearson’s r coefficients are represented by blue and red dots, respectively.
(TIFF)
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.