Abstract
Introduction
Individuals with subjective cognitive decline (SCD) are at increased risk of Alzheimer's disease and could benefit from a prevention strategy targeting lifestyle factors. Making a program available through the Internet gives a widespread reach at low cost, but suboptimal adherence is a major threat to effectiveness. As a first step in developing an online lifestyle program (OLP), we aimed to identify factors that are barriers and/or facilitators for the use of an OLP in individuals with SCD in three European countries.
Methods
As part of the Euro-SCD project, SCD subjects were recruited at memory clinics in the Netherlands, Germany, and Spain. We combined quantitative and qualitative methods, using a mixed methods approach. We conducted an online 18-item survey on the preferences of SCD patients for an OLP (N = 238). In addition, we held semi-structured interviews (N = 22) to gain in-depth understanding of factors acting as a facilitator and/or barrier for intended use of an OLP. Audio recordings were transcribed verbatim. Content analysis was performed.
Results
One hundred seventy-six individuals completed the survey (response rate 74%). Almost all participants regularly use the Internet (97%). Participants reported trustworthiness (93%), user-friendliness (91%), and up-to-date information (88%) as main facilitators, whereas having contact with other users (26%), needing an account (21%), and assignments (16%) were reported as barriers. Barriers differed slightly between countries, but facilitators were largely similar. In-depth interviews revealed that both program characteristics (e.g., trustworthiness, user-friendliness, and personalization) and personal factors (e.g., expectancy to receive negative feedback) are likely to influence the intended use of an OLP.
Discussion
Involving users provided in-depth understanding of factors associated with the intended use of an OLP for brain health. Both program characteristics and personal factors are likely to influence the use of an OLP. Based on this input from the end-users, we will develop an OLP for individuals with SCD.
Keywords: Prevention, Alzheimer's disease, Dementia, Subjective cognitive decline, Online lifestyle program, E-health, Brain health, Cognition, User participation, Co-creation, Mixed methods
Highlights
-
•
Almost all participants believe that healthy lifestyle contributes to brain health.
-
•
Almost all participants use the Internet daily, on all types of devices.
-
•
Barriers or facilitators can be program characteristics as well as personal factors.
-
•
Trustworthiness, user-friendliness, and personalization are important facilitators.
-
•
One online lifestyle program for different European countries seems feasible.
1. Background
The number of people with Alzheimer's disease (AD) will dramatically increase in the coming 30 years [1]. Unfortunately, there is no successful therapeutic intervention for AD yet [2]. However, there is a large window for preventive strategies because brain changes related to AD start decades before the clinical onset of the disease [3]. Former studies have suggested that roughly 30% of the incidence of dementia is attributable to a combination of modifiable risk factors [4], [5], [6]. This emphasizes the potential for lifestyle intervention as a strategy to reduce the incidence of AD or delay its onset.
The Internet is a suitable medium to make interventions available for a large audience at a low cost [7]. Online strategies have been found to be effective in changing lifestyle behavior [8], [9]. Recently, a number of preventative strategies against cognitive decline were developed including online components (e.g., [10], [11]). However, online interventions have difficulty achieving good adherence rates [12], [13], [14]. A recent analysis of adherence to the FINGER study and MAPT trials showed low simultaneous adherence to all components with lowest adherence being related to more intensive and unsupervised parts of the intervention [15]. It is unknown whether cultural difference between countries might play a role in differences in adherence. Many interventions could benefit from a more participant-centered design. In case of low adherence, it is possible that end-users were insufficiently engaged in the process of development. Involving users throughout development in a process of co-creation has a positive effect on user satisfaction and fitting user preferences [16], [17], [18], [19], [20], [21], [22]. The investigation of preferences, barriers, and facilitators that influence the use of a lifestyle intervention is more common in other clinical research fields (e.g., [23], [24]). However, only a few projects specifically investigated these factors at the beginning of the development process (e.g., [6]). Preferences of individuals with cognitive complaints for a lifestyle intervention for brain health have not yet been investigated.
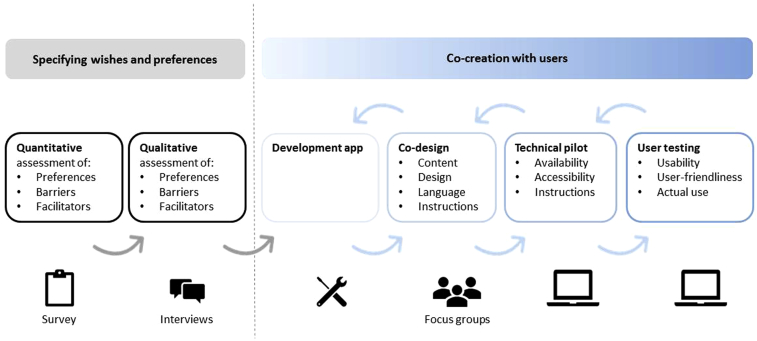
In this study, we focus on individuals who report cognitive decline, while their scores on cognitive tests are normal. Former studies have shown that these individuals with so called “subjective cognitive decline” (SCD) are at increased risk of dementia [23], [24], [25], [26]. Furthermore, individuals with SCD are likely to be highly interested in brain health. With the ultimate aim to develop an online lifestyle program (OLP) tailored for individuals with SCD (Fig. 1: project overview), we performed a mixed methods study to identify factors that would act as barrier or facilitator in the usage of an OLP among SCD subjects in three European countries. We specifically aimed to identify factors important to self-guided programs.
Fig. 1.
Project overview. This figure shows the developmental steps of an online lifestyle program for brain health within the EuroSCD project. First, wishes and preferences were investigated using a mixed methods approach, which is described in the present study. This phase included a survey study and interviews. Second, in co-creation with the users, an iterative process of development and evaluation will be conducted, with the ultimate aim to develop an online lifestyle program fitting the preferences of individuals with subjective cognitive decline. Abbreviation: SCD, subjective cognitive decline.
2. Methods
2.1. Design
This study is part of the European Euro-SCD study (JPND_PS_FP-689-019), of which one aim is to develop an Internet-based tailored lifestyle modification strategy for individuals with SCD (Fig. 1: project overview). The Euro-SCD working group is a collaboration among the VU University medical center, Alzheimer Center in Amsterdam (the Netherlands [27]), Hospital Clinic Barcelona (Spain), and the Center for Memory Disorders, University Hospital Cologne (Germany).
We used a mixed methods design [28], facilitating the integration of quantitative and qualitative findings. First, we distributed a survey among individuals with SCD focusing on Internet usage and the preferences for an OLP, in all three countries. In parallel, semi-structured interviews were conducted in the Netherlands and Germany to gain in-depth understanding of factors associated with the intended use of an OLP. Interviews provide additional information on factors of importance that were not included in the survey but also in-depth understanding of factors that were included in the survey.
The study protocol was approved by the Medical Ethical Committee of the VU University Medical Center Amsterdam, the Medical Ethical Committee of the Hospital Clinic Barcelona, and the Medical Ethical Committee of the University of Cologne. All interviewed participants provided written informed consent.
2.2. Participants
We included participants with SCD. All participants had cognitive complaints for which they visited the memory clinic. Participants underwent clinical workup, including clinical evaluation, neuropsychological assessment, and magnetic resonance imaging scan. When all clinical investigations were normal, patients were labeled as having SCD (i.e., clinical criteria for mild cognitive impairment, dementia, or any psychiatric disorder not fulfilled).
2.3. Recruitment
2.3.1. Survey
For the survey, we invited 238 SCD subjects from three European memory clinics (Barcelona N = 26, Amsterdam N = 176, and Cologne N = 36). Participants were recruited during their annual research visit, by individual telephone call of the interviewer or by a newsletter.
2.3.2. Interviews
The semi-structured interviews were conducted in Amsterdam and Cologne. In Amsterdam, the interviews were announced in a digital newsletter, and subjects were invited to contact the researcher (L.M.P.W.). In Cologne, SCD subjects were approached individually by telephone (A.-K.S.).
2.4. Survey
The survey (available on request) contained questions regarding the Internet usage and preferences for an OLP. We developed the survey in collaboration with the international Euro-SCD working group and members of a scientific patient panel (Amsterdam). We distributed the online survey via an anonymous link (via www.Qualtrics.com) or on paper when requested. Based on automatic time recording, participants approximately needed 15 minutes to fill out the digital version of the survey. The survey consisted of the following domains (number of items): Internet use (seven), sources of health information (seven), use of an OLP for brain health (two), lifestyle topics of interest (one; seven sub items), and possible barriers and facilitators for the use of an OLP (one; 10 sub items) and demographics (six). Based on the Dutch Personal Data Protection Act [29], some demographics were categorized (e.g., age ranges). The survey was adaptive; if the participant for instance reported not using Internet, follow-up questions about Internet use were skipped.
To report topics of interest concerning lifestyle, participants indicated whether they would be interested in topics out of a list of six topics. To report barriers and facilitators, participants indicated for 10 factors whether they expected it to stimulate or hinder them to use an OLP. The importance of trustworthiness was indicated using a VAS scale (Visual Analogue Scale; 0 to 100).
2.5. Semi-structured interviews
We conducted semi-structured interviews to gain in-depth understanding of factors associated with the intended use of an OLP. Of the 22 participants, 14 were Dutch and eight, German (mean age 67 ± 9.2 years; female: 10 [45%]). The education level varied from average (beyond high school) to high (university). The topic list included the following: sources of health information, use of Internet, experience with lifestyle adaptation, OLP for brain health, and barriers and facilitators for the use of an OLP (see Supplementary Material). All topics were discussed in the interviews; the order varied depending on the input of the participant. The semi-structured interviews took approximately 1 to 1.5 hours. The Dutch interviewer (L.M.P.W.) attended the German interviews (A.-K.S.) to ensure a similar interview procedure. Conducting and analyzing the interviews occurred through an iterative process, such that data of past interviews were allowed to influence upcoming interviews. This process allows the researcher to get deeper into the data and see patterns emerge, while continuing data collection. Data were collected until data saturation was reached, meaning that no more new themes emerged from the interview data, and the researchers saw strong repetition [30]. Interviews were audiotaped, and summaries of the interviews were sent to the participants to check for a correct interpretation of the interview (member check) [31]. All 22 participants responded to the member check, of which seven provided minor corrections or additional information. Dutch interviews were transcribed verbatim whereas the German interviews were summarized, including quotes. We used the Dutch transcripts and Dutch summaries of the German interviews for data analysis.
2.6. Data analysis
2.6.1. Survey
We used completed surveys in the analysis. Because the survey was anonymous, we do not have information on nonresponders. Descriptive statistics were used to report participant characteristics. Chi-squared tests were performed to investigate whether Internet usage and barriers and facilitators varied between age groups, sex, and countries. We used IBM SPSS Statistics, version 22 [32]. P values less than .05 were considered significant.
2.6.2. Interviews
Thematic content analysis [33], [34] was performed on the transcripts of the interviews, using MAXQDA software (www.maxqda.com). All Dutch transcripts were independently coded by two researchers (L.M.P.W. and J.H.P.M.). We used open coding, allowing codes to arise from the data and avoiding codes based on prepositions of the researchers [35]. The codes were compared, and in case of discrepancies, coded transcripts were discussed up to consensus. Thematic categories were extracted, and a coding framework was developed. Dutch summaries of German interviews were coded based on the coding system that emerged from the Dutch data, specifically looking for information to complement Dutch data. If additional insights were collected, the coding system was adapted. Otherwise, German data were included into the coding system.
3. Results
3.1. Survey
3.1.1. Participant characteristics
The total response rate for the survey was 176/238 (74%), female: n = 80 (45%). Most of the participants were aged 60 to 70 years (n = 79, 45%) and had education beyond secondary school (n = 129, 73%) (Table 1). The majority of the participants used Internet on a daily basis (n = 134, 78%), and only five participants (3%) did not use Internet at all. Compared with German participants, Dutch participants more often used the Internet (daily: Netherlands: 82%; Germany: 62%, P = .003). While computer, laptop, and smartphone use did not differ between countries, Dutch participants more often used a tablet compared with the other countries (Netherlands: 52%; Germany: 28%, and Spain 33%, P = .009). Frequency of Internet usage did not differ between age or gender groups (Table 1). Most participants reported the Internet as their main source for information on memory and the brain (n = 140, 80%).
Table 1.
Demographics and Internet usage of survey participants
| Characteristics | Participants N = 176 |
|---|---|
| Female, n (%) | 80 (46) |
| Age group, n (%) | |
| <40 y | 1 (1) |
| 40–49 | 6 (3) |
| 50–59 | 31 (18) |
| 60–69 | 79 (45) |
| 70–79 | 54 (31) |
| ≥80 y | 5 (3) |
| Education, n (%) | |
| Primary school not completed | 3 (2) |
| Primary school completed | 4 (2) |
| Secondary school completed | 40 (23) |
| Vocational training, diploma, certificate | 35 (20) |
| University college, university | 94 (53) |
| Internet access at home, n (%) | |
| Yes | 169 (99) |
| Frequency of Internet usage, n (%) | |
| Daily | 134 (78) |
| 4–6 days a week | 12 (7) |
| 1–3 days a week | 20 (12) |
| About once a month | 4 (2) |
| Less than once a month | 1 (1) |
NOTE. Gender, age, education, Internet access at home, and frequency of Internet usage were described based on reporting of participants using multiple choice questions; reported in number and percentage of participants in total.
3.1.2. OLP for brain health
Nearly all participants reported believing that a healthy lifestyle can contribute to brain health (n = 172, 98%). This was consistent across countries and age groups; four female participants reported not to believe this link. In addition, most participants expected that they would use an online program providing advice on lifestyle to maintain brain health (n = 164, 93%). When asked for topics of interest concerning lifestyle, most participants mentioned that they were interested in nutrition (n = 145, 82%), cognitive activity (n = 142, 81%), and physical activity (n = 139, 79%). Topics mentioned less often were sleep and relaxation (n = 117, 67%), positive attitude (n = 80, 46%), and social engagement (n = 73, 41%).
3.1.3. Barriers and facilitators
Trustworthiness, user-friendliness, and up-to-date information were reported as the most important facilitators for the use of an OLP (resp. n = 163, 93%; n = 160, 90%; n = 155, 88%). About half of the participants (n = 90, 52%) reported undertaking steps to establish whether the source of online information is trustworthy. “Having contact with other users”, “account needed to use the program,” and “assignments included in the program” were reported as potential barriers (n = 46, 26%; n = 37, 21%; n = 28, 16%). These results are presented in Table 2.
Table 2.
Reported barriers and facilitators (survey)
| Factors | Facilitator n (%) |
Neutral n (%) |
Barrier n (%) |
|---|---|---|---|
| Trustworthiness | 163 (93) | 13 (7) | 0 |
| User-friendliness | 160 (91) | 16 (9) | 0 |
| Up-to-date information | 155 (88) | 21 (12) | 0 |
| Accessible at no charge | 131 (74) | 43 (24) | 2 (1) |
| Personalized program | 121 (69) | 45 (26) | 10 (6) |
| Receiving reminders of the program | 95 (54) | 68 (39) | 13 (7) |
| Self-monitoring of behaviour | 91 (52) | 62 (35) | 23 (13) |
| Assignments included in the program | 71 (40) | 77 (44) | 28 (16) |
| Account needed to use the program | 43 (24) | 96 (55) | 37 (21) |
| Having contact with other users | 29 (17) | 101 (57) | 46 (26) |
Abbreviation: OLP, online lifestyle program.
NOTE. Participants could indicate whether they expected these factors to facilitate using an OLP to be a barrier for the use of an OLP or to have no impact for the use of an OLP (neutral).
The reported barriers and facilitators were the same between age groups and sex. Comparing countries, there were three barriers that differed. First, “having contact with other users” was reported more often as a barrier by Dutch participants (n = 43, 34%) while participants in Germany and Spain mentioned as a neutral factor (barrier reported respectively n = 2, 6%; n = 1, 6%, both P < .01). Second, German participants reported more often “tracking behavior” as a barrier (n = 12, 38%) compared with Dutch and Spanish participants who mainly reported this as a motivating factor (motivating respectively n = 69, 55%; P = .000; n = 14, 78%, P = .001). Third, most Dutch and German participants report “needing an account” as a neutral factor (respectively n = 70, 56% and n = 21, 66%), while Spanish participants considered this a motivating factor (n = 9, 50%; both P < .05).
3.2. Interviews
3.2.1. Identified themes
Content analysis revealed two main themes: program characteristics and personal factors. From these main themes, we extracted 12 subthemes. The results are ordered by the main and sub themes (Table 3) and illustrated with quotes (Tables 4 and 5).
Table 3.
Description of themes and codes (interviews) derived with content analysis
| Theme | Subtheme | Description |
|---|---|---|
| Program characteristics | Barriers | |
| Specific frequency required | If the program requires visits in a high frequency and of long duration. Also, if you cannot quit the program or stop messages by yourself | |
| Content unsatisfying | When content is not interesting, not up-to-date, too scientific or too simple, and when information parts are too long | |
| Facilitators | ||
| Content | Content on desired topics, explanation of difficult words, and possibility to get deeper into the information in case of interest. Clear distinction between information on the total population, people with memory complaints or people with dementia. Trustworthy information. Up-to-date and innovative information. | |
| Functionalities | Messages from the program to remind you, possibility to use program at own frequency and pace, and possibility to ask questions to expert or help desk. | |
| Personalization | Information and advice are tailored and applicable to user, possibility to track behavior and get insight into this, and track progress based on scores and graphs. | |
| User-friendliness | Structured and clear program layout, easy to search within the information, easy to use, quick to use, available at multiple devices, and well-developed technical aspects | |
| Personal factors | Barriers | |
| Limited digital skills | Having difficulties working with technology, logging in, and reminding passwords | |
| Time constraints | Having too little time to work on the program | |
| Psychological barrier | Having to face the truth about your functioning and behavior, expecting to have a hard time persevering, and getting disappointed | |
| Facilitators | ||
| Total package of information | Information on lifestyle and brain collected (not only nutrition or only cognitive activity), holistic view, and no contradictory information | |
| Confirmation of what you know and do | Reading and learning that what you already do and know is the right thing to do | |
| Motivation for a healthy brains | The intrinsic motivation to work on brain health and the feeling of vulnerability of the brain |
NOTE. This table gives an overview of the themes and subthemes identified in the interview data. Every subtheme is described with summarized examples from the interviews.
Table 4.
Quotes illustrating program characteristics and subthemes (interviews)
| Program characteristics: Subtheme and quote |
|---|
| Barriers |
| Specific frequency required |
| P1: Well too much is more times a day. There should be an option to choose: not every day. Because I do look a lot [at digital devices], but if you don't, then it should be possible to look once a week and not miss out on anything. |
| Content unsatisfying |
| P12: I would stop using it [the OLP] when I would see that it is not up-to-date and relevant. If I would see things in all other media and not in this thing. I would think ‘You guys are sleeping’. |
| Facilitators |
| Content |
| P1: I would prefer small items. That is how I use twitter at the moment. And if you think, well that is interesting, that you have the choice to get more information. |
| P9: I think for content is it fine to get faced with the facts at some point. Be confronted with things that you would not think of yourself. |
| P14: Well at first it should be provided by people of calibre. Those that are familiar with the content. That is really important to me. |
| Content–trustworthiness |
| P6: I value it [trustworthiness] a lot and I am certain that what I read is true, often. Especially when you come across scientific sites or if you read other things about it and you keep getting the confirmation. At some point, for me at a some moment is it true, that's how it is, easy. |
| P5: I think that is great [more possibilities with upcoming technology] And the social media is fantastic. But I do think, well there is quite a proliferation with millions of opinions and visions. And it is quite hard to find your way in these. |
| Functionalities |
| P2: If there would be a new item every day, then you look at the site every day. But if it would be once a week, then I would prefer a reminder [of new content]. |
| Personalization |
| P4: [on implementing advices in daily life] I think you should show the things in a positive way, like, it can be really nice to do. If you do not think that extra glass of alcohol, you will be much brighter. Or, let's go, take your bag and go to town for some shopping. |
| P9: What I am thinking about is (…) a personal page for the user, where you can indicate things and where you can track progress based on core numbers. |
| User-friendliness |
| P3: There should be a page with answers to questions. If you cannot figure it out on your own, you can get in contact with the person that knows about it. (…) A guideline for using the program, yes. |
| P12: and from a technical view, it should work in a convenient way. (…) It should be well readable on a tablet or phone. |
Abbreviations: OLP, online lifestyle program; P, participants and number.
NOTE. This table gives insight into the subthemes, by providing specific quotes of participants.
Table 5.
Quotes illustrating personal factors and subthemes (interviews)
| Personal factors: Subtheme and quote |
|---|
| Barriers |
| Limited digital skills |
| P11: I make so many mistakes [with digital forms], I cannot get it done. I tried to fill out some online forms a few times already and what not, and it never ends well. And then I get, well, shoot, I never succeed. |
| Time constraints |
| P6: I had a brain trainer app on my phone once. We also had too little time for that. |
| P13: A barrier would be that I am too busy, then I won't have time to open the program. |
| Psychological barrier |
| P7: It would be a barrier to have to know the truth [about your memory] … that you're not doing well enough. |
| P4: Let's hope I persevere and keep using it. This is something I've experienced before. That I do not finish it. And that is somewhat disappointing. |
| Facilitators |
| Total package of information |
| P3: I think it would be nice if all can be integrated, interweaved. To make it a total package of information. Now I am trying to figure it out on my own, with advices of doctors. |
| Confirmation of what you know and do |
| P10: For once, I would like to hear whether I am doing the right things. And perhaps they have additional information on it. |
| P13: I think I already know 80% about this [information on lifestyle and brain health]. I did not adjust my nutrition for Alzheimer's alone. But I came across this information, I thought, that is great. I am already on the right track. I only need make small adjustments and then I will have the Mediterranean diet all worked out form myself. |
| Motivation for a healthy brain |
| P11: I want to keep my brain as healthy as possible, because that is what I am feeling vulnerable about. |
Abbreviation: P, participants and number.
NOTE. This table gives insight into the subthemes, by providing specific quotes of participants.
3.2.2. Program characteristics
Program characteristics that were mentioned as a barrier for the use of an OLP were inflexibility of frequency and duration of the online sessions, and if the content would not be up-to-date and relevant to the participants.
Program characteristics that were mentioned as a facilitator were the content of the program when being trustworthy, up-to-date, and interesting. Participants mentioned that to them, trustworthy information is consistent and reliable information from a source that has proven expertise in the field. Online sources for information on brain health that were mentioned were for example random results of Google searches, websites of patient associations, and websites of health institutes. Although trustworthiness was considered very important, participants reported having trouble determining how trustworthy online information is. Program characteristics that were also mentioned as facilitator were receiving reminders and allowing to keep track of results. In addition, personalized content and advice and a user-friendly program were considered motivating functionalities of a program. In the context of user-friendliness, a clear structure, a guideline, and a program that is easy to use were mentioned. Table 4 presents illustrating quotes.
3.2.3. Personal factors
Personal factors that were mentioned as barriers were not having the time or the digital skills to use the program. In addition, participants mentioned psychological barriers, such as the expectancy to get disappointed by results on cognitive results or current lifestyle, or the expectancy to not persevere with the program and get disappointed by oneself. Personal factors that were mentioned as facilitators were having all information about the brain and lifestyle in one place, confirmation of what you already do and know about lifestyle and the brain, and the motivation for a healthy brain. Table 5 presents illustrating quotes.
4. Discussion
We aimed to identify factors that are barriers and/or facilitators for the use of an OLP in individuals with SCD. The data and information presented in this article are of high value to other researchers, developers, and clinicians, as we describe often underrated parts of development of a digital innovation. We found that both program characteristics and personal factors are deemed relevant by end-users for the use of an OLP. Program characteristics that might be a barrier included inflexibility in the use and the content of the program. Program characteristics that were mentioned as facilitators were trustworthiness, user-friendliness, and facilities of the program (e.g., reminders). Personal factors that might be a barrier were limited time, limited digital skills, and psychological barriers. Personal factors reported to facilitate the use were the wish for a total package of information, confirmation of what you do and know, and the motivation for a healthy brain.
In both the survey and the interviews, trustworthiness, user-friendliness, and personalization were mentioned as the main facilitators. In the survey, we only investigated program characteristics. The interviews provided additional information about personal factors of importance, including digital skills, a motivation for a healthy brain, and the expectancy to receive negative feedback or get disappointed by oneself for not persevering. In addition, interviews provided insight into what particular factors, such as trustworthiness, entail according to participants' perspective. While trustworthiness was mentioned as an important facilitating factor for the use of an OLP, the interviews showed that participants have problems determining how trustworthy an online source is. Our study showed that participants have a need for a trustworthy, total package of information, emphasizing the need for trustworthy online information about the prevention of AD. A recent study [36] showed that information about the prevention of AD varies in quality and sometimes includes conflicts of interest. Another study [37] reviewed factors that influence trust and credibility in web-based health information. Our results are in line with these studies because participants also mentioned authority of the owner, advertisement, and layout as factors that influence the perceived trustworthiness. The majority of both the survey and interview participants reported that lifestyle could contribute to brain health and wanted to use an OLP for brain health when available. This is in contrast with results of a recent study, showing that one-third of the people, who did not participate in an Internet-based lifestyle prevention program, thought that an online intervention is not an effective way to improve health [38]. These apparent differences could be due to the discordance between the intended and actual use. Alternatively, the disparate results can be explained by differences in population. Individuals at risk, and perhaps especially individuals with cognitive complaints, might have different intrinsic motivators to participate in preventative strategies compared with healthy individuals or individuals without physical risk factors. In addition, the awareness of a healthy lifestyle for brain health might differ between these groups.
This study has some limitations. First, the survey was primarily distributed via an online link, and a paper version was offered on request. It could be argued that a selection bias was present in our study, including mainly individuals with good digital skills. However, the survey was available on paper on request, and almost all participants reported having access to the Internet at home and using it regularly. In addition, the target population for an OLP are people with sufficient digital literacy and therefore the current participants are representative of the future users. Second, participants were not evenly distributed over three countries, and it is unclear whether this might have induced a bias in our results. However, for this study, it was of interest whether one OLP could fit the preferences of individuals from three different European countries. With the present samples, we were indeed able to reveal subtle differences between the three countries. This is relevant information, as these differences in barriers and facilitators across countries can be taken into account by making certain program facilities optional across countries. For example, participants could choose between not needing an account or receiving personalized feedback. In addition, Spanish participants were involved in the survey study only. Therefore, we have no detailed insights into their potential barriers and facilitators and how this might relate to those of German and Dutch participants. However, our numbers of participants for both the survey and the interview were sufficient for robust analysis, and the survey did not show evidence for cross-cultural differences. We will address the issue of unequal participant distribution by paying attention to differences between countries in future phases of the study. Third, in this study, we focused on SCD individuals who attended a memory clinic. Although this population is selective, they do present the majority of the target population. Future studies targeting population-based samples should be conducted to evaluate the suitability of such programs in samples outside the memory clinic.
The strengths of this study include the following: First, the international character of the study contributing to the generalizability of the results and implementation of the eventual tool in multiple countries. Second, the mixed methods approach, which allowed us to not only compare quantitative data of a larger group but also to perform qualitative in-depth analyses of barriers and facilitators. With this approach, we collected data on Internet usage and in-depth information on the factors that might influence the use of an OLP. Third, several procedures were applied to guarantee quality and validity of our findings. We used standardized procedures as much as possible. For the interviews specifically, we used input of different researchers (investigator triangulation) and member checks to contribute to the credibility of the interview data. Steps were taken to contribute to dependability (data saturation and iterative process), confirmability (e.g., documenting our steps, independent raters), and transferability (presenting quotes of the interviews) of the data [34]. Fourth, our samples were a good representation of the target population, contributing to robustness of the results. The response rate of the survey study was high (74%) compared with usual response rates of online surveys (23%–47%; [39]). In addition, the high number of participants and the emergence of data saturation indicated robustness for qualitative data [40], [41].
In conclusion, in this project focusing on individuals with SCD as a target group for interventions to prevent mild cognitive impairment and AD, we identified barriers and facilitators for the use of an OLP in a process of co-creation. We found that both program characteristics (trustworthiness, user-friendliness, and personalization) and personal factors (time, digital skills, expectancy of feedback, or perseverance) are relevant factors when developing and implementing an OLP for brain health. Participants own devices to access such a program via a computer, smartphone, or tablet. Although some factors differed across countries, similarities prevailed, providing confidence that one OLP fitting the needs of users across different European countries is feasible. As a next step in Euro-SCD, we are currently developing an OLP for brain health, incorporating the recommendations of our end-users. We continue involving end-users throughout the process of development and implementation to develop a tool that fits their wishes, preferences, and needs.
Research in Context.
-
1.
Systematic research: We reviewed the literature using traditional databases, presentations, and conference documents on preventative strategies for cognitive decline, e-health, and mixed methods. Relevant publications are cited.
-
2.
Interpretation: Our findings provide a quantitative perspective on preferences for an online lifestyle program for brain health and qualitative in-depth understanding in the factors influencing the use of such a program.
-
3.
Future directions: the findings are used to develop an online lifestyle program, fitting the preferences of the users. This could contribute to better retention and acceptance of the tool. We will develop an online lifestyle program aimed to improve brain health, specifically for individuals with subjective cognitive decline.
Acknowledgments
Research of the VUmc Alzheimer center is part of the neurodegeneration research program of Amsterdam Neuroscience (www.amsterdamresearch.org). The VUmc Alzheimer Center is supported by Stichting Alzheimer Nederland and Stichting VUmc fonds. The authors thank all participants for their willingness to contribute to this study. The present study was performed within the context of the Euro-SCD project, which has been funded by the EU Joint Programme—Neurodegenerative Disease Research (JPND_PS_FP-689-019; ZonMw grant no. 733051043). W.v.d.F. is recipient of a research grant from Stichting Gieskes Strijbis Fonds (SCIENCe). S.A.M.S. is a recipient of a research grant from Stichting Equilibrio.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.trci.2018.03.003.
Supplementary data
References
- 1.Prince M., Wimo A., Guerchet M., Ali G.C., Wu Y.T., Prina M. Alzheimer's Disease International; London: 2015. World Alzheimer Report 2015: The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends. [Google Scholar]
- 2.Graham W.V., Bonito-Oliva A., Sakmar T.P. Update on Alzheimer's disease therapy and prevention strategies. Annu Rev Med. 2017;68:413–430. doi: 10.1146/annurev-med-042915-103753. [DOI] [PubMed] [Google Scholar]
- 3.Jansen W.J., Ossenkoppele R., Knol D.L., Tijms B.M., Scheltens P., Verhey F.R. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 2015;313:1924–1938. doi: 10.1001/jama.2015.4668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livingston G., Sommerlad A., Orgeta V., Costafreda S.G., Huntley J., Ames D. Dementia prevention, intervention, and care. Lancet. 2017;390:2673–2734. doi: 10.1016/S0140-6736(17)31363-6. [DOI] [PubMed] [Google Scholar]
- 5.Barnes D.E., Yaffe K. The projected effect of risk factor reduction on Alzheimer's disease prevalence. Lancet Neurol. 2011;10:819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Bruijn R.F.A.G., Ikram M.A. Cardiovascluar risk factors and future risk of Alzheimer's disease. BMC Med. 2014;12:130. doi: 10.1186/s12916-014-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Griffiths F., Lindenmeyer A., Powell J., Lowe P., Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. 2006;8:e10. doi: 10.2196/jmir.8.2.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krebs P., Prochaska J.O., Rossi J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51:214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Portnoy D.B., Scott-Sheldon L.A., Johnson B.T., Carey M.P. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988-2007. Prev Med. 2008;47:3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Donnell C.A., Browne S., Pierce M., McConnachie A., Deckers K., van Boxtel M.P. Reducing dementia risk by targeting modifiable risk factors in mid-life: study protocol for the Innovative Midlife Intervention for Dementia Deterrence (In-MINDD) randomised controlled feasibility trial. Pilot Feasibility Stud. 2015;1:40. doi: 10.1186/s40814-015-0035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anstey K.J., Bahar-Fuchs A., Herath P., Rebok G.W., Cherbuin N. A 12 week multidomain intervention versus active control to reduce risk of Alzheimer's disease. Trials. 2013;14:60. doi: 10.1186/1745-6215-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kelders S.M., Van Gemert-Pijnen J.E., Werkman A., Nijland N., Seydel E.R. Effectiveness of a Web-based intervention aimed at healthy dietary and physical activity behavior: a randomized controlled trial about users and usage. J Med Internet Res. 2011;13:e32. doi: 10.2196/jmir.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neve M.J., Collins C.E., Morgan P.J. Dropout, nonusage attrition, and pretreatment predictors of nonusage attrition in a commercial web-based weight loss program. J Med Internet Res. 2010;12:e69. doi: 10.2196/jmir.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christensen H., Griffiths K.M., Farrer L. Adherence in internet interventions for anxiety and depression: Systematic review. J Med Internet Res. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coley N., Ngandu T., Cantet C., Lehtisalo J., Vellas B., Kivipelto M. AAIC; London: 2017. Adherence to Multidomain Interventions for the Prevention of Alzheimer's Disease: Data from the MAPT and FINGER Trials. [Google Scholar]
- 16.Kujala S. User involvement: A review of the benefits and challenges. Behav Inf Technol. 2003;22:1–16. [Google Scholar]
- 17.Grol R., Grimshaw J. From best evidence to best practice: effective implementation of change in patients' care. Lancet. 2003;362:1225–1230. doi: 10.1016/S0140-6736(03)14546-1. [DOI] [PubMed] [Google Scholar]
- 18.van Bruinessen I.R., van Weel-Baumgarten E.M., Snippe H.W., Gouw H., Zijlstra J.M., van Dulmen S. Active patient participation in the development of an online intervention. JMIR Res Protoc. 2014;3:e59. doi: 10.2196/resprot.3695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nordin C., Michaelson P., Eriksson M.K., Gard G. It's about me: Patients' experiences of patient participation in the web behavior change program for activity in combination with multimodal pain rehabilitation. J Med Internet Res. 2017;19:e22. doi: 10.2196/jmir.5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross J., Stevenson F., Lau R., Murray E. Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update) Implement Sci. 2016;11:146. doi: 10.1186/s13012-016-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van De Belt T.H., Engelen L.J., Berben S.A., Schoonhoven L. Definition of Health 2.0 and Medicine 2.0: a systematic review. J Med Internet Res. 2010;12:e18. doi: 10.2196/jmir.1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Gemert-Pijnen J.E., Nijland N., van Limburg M., Ossebaard H.C., Kelders S.M., Eysenbach G. A holistic framework to improve the uptake and impact of eHealth technologies. J Med Internet Res. 2011;13:e111. doi: 10.2196/jmir.1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jessen F., Amariglio R.E., van Boxtel M., Breteler M., Ceccaldi M., Chetelat G. A conceptual framework for research on subjective cognitive decline in preclinical Alzheimer's disease. Alzheimers Dement. 2014;10:844–852. doi: 10.1016/j.jalz.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sperling R.A., Aisen P.S., Beckett L.A., Bennett D.A., Craft S., Fagan A.M. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reisberg B., Shulman M.B., Torossian C., Leng L., Zhu W. Outcome over seven years of healthy adults with and without subjective cognitive impairment. Alzheimers Dement. 2010;6:11–24. doi: 10.1016/j.jalz.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell A.J., Beaumont H., Ferguson D., Yadegarfar M., Stubbs B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr Scand. 2014;130:439–451. doi: 10.1111/acps.12336. [DOI] [PubMed] [Google Scholar]
- 27.van der Flier W.M., Pijnenburg Y.A., Prins N., Lemstra A.W., Bouwman F.H., Teunissen C.E. Optimizing patient care and research: the Amsterdam Dementia Cohort. J Alzheimers Dis. 2014;41:313–327. doi: 10.3233/JAD-132306. [DOI] [PubMed] [Google Scholar]
- 28.Castillo-Page L., Bodilly S., Bunton S.A. AM last page: Understanding qualitative and quantitative research paradigms in academic medicine. Acad Med. 2012;87:386. doi: 10.1097/ACM.0b013e318247c660. [DOI] [PubMed] [Google Scholar]
- 29.Dutch Personal Data Protection Act, July 6th, 2000. (Bwb-ID [database]: BWBR0011468 [Dutch]). Available at: http://wetten.overheid.nl/BWBR0011468/2017-07-01.
- 30.Guest G., Bunce A., Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- 31.Krefting L. Rigor in qualitative research: the assessment of trustworthiness. Am J Occup Ther. 1991;45:214–222. doi: 10.5014/ajot.45.3.214. [DOI] [PubMed] [Google Scholar]
- 32.IBM . IBM Corp; New York: 2011. IBM SPSS Statistics for Windows. Version 22.0. [Google Scholar]
- 33.Glaser B., Strauss A. Adline; Chicago: 1967. The Discovery of Grounded Theory: Strategies for Qualitative Research. [Google Scholar]
- 34.Strauss A. Cambridge University Press; Cambridge: 1987. Qualitative Analysis for Social Scientists. [Google Scholar]
- 35.Boyatzis R.E. Sage Publications; Thousand Oaks, CA: 1998. Transforming Qualitative Information: Thematic Analysis and Code Development. [Google Scholar]
- 36.Robillard J.M., Feng T.L. Health advice in a digital world: Quality and content of online information about the prevention of Alzheimer's disease. J Alzheimers Dis. 2017;55:219–229. doi: 10.3233/JAD-160650. [DOI] [PubMed] [Google Scholar]
- 37.Sbaffi L., Rowley J. Trust and credibility in web-based health information: A review and agenda for future research. J Med Internet Res. 2017;19:e218. doi: 10.2196/jmir.7579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Coley N., Guillemont J., van Middelaar T., Barbera M., Rosenberg A., Soininen H. AAIC; London: 2017. Accept–Hatice: A Mixed Methods Study of Facilitators and Barriers to Participation in an Internet-Based Multidomain Trial for the Prevention of Cardiovascular Disease and Cognitive Decline in Older European Adults. [Google Scholar]
- 39.Nulty D.D. The adequacy of response rates to online and paper surveys: what can be done? Assess Eval High Educ. 2008;33:301–314. [Google Scholar]
- 40.Lincoln Y.S., Guba E.G. Sage; Beverly Hills: 1985. Naturalistic Inquiry. [Google Scholar]
- 41.Frambach J.M., van der Vleuten C.P.M., Durning S.J. AM last page: Quality criteria in qualitative and quantitative research. Acad Med. 2013;88:552. doi: 10.1097/ACM.0b013e31828abf7f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.