Abstract
Purpose
The prevalence and burden of asthma is increasing worldwide. In this study, we analyzed 3 different Korean national health survey datasets to determine the general features of adult asthma in Korea and to obtain basic information that would support future strategies for better management of adult asthma.
Methods
The surveys used in this study included the Korea National Health and Nutrition Examination Survey (KNHANES), Korea Community Health Survey (KCHS) and National Health Insurance Service-National Sample Cohort (NHIS-NSC). We investigated annual asthma prevalence, evaluating the rate and risk factors of asthma exacerbation by age and sex, and clinical data of 1,832 patients with asthma who were registered in the Cohort for Reality and Evolution of Adult Asthma in Korea (COREA) were analyzed to elucidate risk factors for asthma exacerbation. We also analyzed another asthma cohort and added it as replication data.
Results
In the KNHANES database, annual asthma prevalence rates varied from 1.2% to 3.1%. In the KCHS database, overall prevalence increased, with significant regional differences (1.6%–2.1%). The NHIS-NSC indicated a gradual increase in annual asthma prevalence from 4.5% to 6.2%. Interestingly, all 3 surveys indicated the highest prevalence of asthma among elderly women. In addition, elderly women with asthma had a significantly higher risk of asthma exacerbation (odds ratio [OR], 1.87; 95% confidence interval [CI], 1.19–2.93; P=0.006). Approximately 11% of patients were classified as having severe asthma. An asthma cohort analysis identified female sex, low baseline pulmonary function, longer treatment duration, high variability in pulmonary function and significant changes in Asthma Control Test scores as risk factors for asthma exacerbation.
Conclusions
The prevalence of asthma in Korea is consistently high among elderly and female populations. These results should lay the foundation for strategies for effective asthma prevention and management; elderly female patients with asthma should receive particular attention.
Keywords: Prevalence, incidence, asthma
INTRODUCTION
As the prevalence of asthma has increased gradually to its current peak, its associated burden has also increased significantly.1,2 In 2015, asthma was among the most prevalent chronic respiratory diseases, affecting an estimated 358 million people.3 The prevalence of asthma in Asian countries including Korea has been reported to range from 0.7% to 11.9%.4 The clinical features of asthma are well known to vary by age, sex, environment and ethnic background, and each subtype of asthma exhibits different severities and prognoses.5,6,7,8 For example, after the onset of puberty, asthma is observed more frequently in females.5 Although the mechanism is unclear, there is growing interest in female asthma. Therefore, better strategies for asthma management rely on the definition of a certain subtype of asthma based on clinical and epidemiological characteristics.8 Studies involving an analysis of data from large national health surveys or cohorts would be particularly valuable for a comprehensive understanding of asthma features.
In Korea, nationwide datasets such as those generated by the Korea National Health and Nutrition Examination Survey (KNHANES), the Korea Community Health Survey (KCHS) and the National Health Insurance Service-National Sample Cohort (NHIS-NSC) can be used to evaluate disease prevalence. The KNHANES is a nationwide population survey conducted by the Korea Centers for Disease Control and Prevention (KCDC). The KCHS is also a nationwide health survey representing 253 cities, provinces and local health centers. The National Health Insurance (NHI) program covers 97.9% of the total general population, and the NHIS-NSC is a sample cohort of 1 million people randomly selected from the NHI program.
The purpose of this study was to evaluate the status of adult asthma in Korea with the aim of identifying better strategies for asthma management. In the current study, we investigated the prevalence of asthma in the general population according to age and sex over time using national databases. In addition, we evaluated the proportion of each group of patients with asthma according to severity and asthma exacerbation rate. Finally, we attempted to find major risk factors for asthma exacerbation among adult patients with asthma using actual clinical data obtained from the Cohort for Reality and Evolution of Adult Asthma in Korea (COREA), a representative multicenter adult asthma cohort in Korea. To make the results more robust, Soonchunhyang University Asthma Genome Research Center (SCH) was analyzed by the same methods.
MATERIALS AND METHODS
Nationwide databases in Korea and a working definition of asthma
For the general population analysis, 3 databases KNHANES, KCHS and NHIS-NSC, were used. The data did not include any identifiable information about the individual patients. The KNHANES is a nationwide health and nutrition survey that has been maintained since 1998. This survey has collected various data including physical examination findings by physicians, clinical and laboratory tests, information from personal interviews, and related measurements.9 The KNHANES is comprised of 3 types of questionnaires that address health, nutrition and screening. This survey includes some items related to asthma such as questions about asthma diagnoses. To improve the accuracy of asthma diagnoses in this study, asthma was considered only when the study participant provided a positive response to the question: “Have you been diagnosed with asthma by your doctors?” To obtain appropriate estimates, we followed the guidelines for reporting sample weight and stratification as designated by the KCDC. On the basis of the information collected, the prevalence of asthma was analyzed from 1998 to 2013 and by age and sex. We obtained the data regarding age and sex distribution from the Population and Housing Census conducted by Statistics Korea in 2005 and adjusted the data.
The KCHS is another nationwide health survey conducted in 253 cities, provinces and local health centers. This survey also includes asthma-related questions that examine whether the subject experienced wheezing symptoms during the last year, whether they had been diagnosed with asthma by their physicians and received treatment, or whether they had experienced a worsening of their condition over the past year. From the KCHS data, the prevalence of asthma was defined as the experience rate of diagnosed asthma by a physician during the lifetime period of 2008–2013 and was standardized by sex and age. We also compared asthma prevalence among different regions in Korea.
The NHIS-NSC database is a cohort database created in 2002, excluding noncitizens and special purpose employees with an unidentifiable income level. It links an individual's social and economic variables (i.e., qualification data) with their medical history and health screening data. A sample of 1 million people (1,025,340; 2.2% of the total population in 2002) in the NHIS database followed participants for 11 years unless their eligibility was disqualified because of death or emigration. Systematic stratified random sampling with proportional allocation within each stratum was conducted using the individual's total annual medical expenses. Within each stratum, systematic sampling was conducted after sorting population data by the value of annual medical expenses and maintaining a sampling rate of 2.2%. During the follow-up period, the cohort was updated annually by adding a representative sample of newborns using the 2.2% sampling rate.10 The NHIS-NSC database can be longitudinally analyzed for 11 years (2002–2012). We defined eligible asthma patients for this study as those whose medical claims included International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes (J45–J46) for asthma during the identification period of January 1, 2002 through December 31, 2012. In addition, the prescription of 1 or more asthma medications and the performance of designated asthma-related tests were considered an operational definition of asthma (Supplementary Table 1). In other words, asthma was defined as a condition that meets an asthma diagnosis code (J45–J46) at the same time asthma-related tests were performed or medications were prescribed. The prevalence was determined by the number of patients with asthma divided by the total number of patients registered by the NHIS-NSC and was analyzed annually by age and sex. Incidence was defined as the number of patients with a new case of asthma diagnosed in a specific year, with the denominator as the number of patient-years of observation (calculated from the number of patients registered with practices and their length of registration). The incidence was analyzed for all ages, except children under 1 year of age.
Among these defined patients with asthma, an episode of acute exacerbation was defined as an event requiring an asthma-related hospital admission, emergency room visit or the use of prescribed systemic steroids in an outpatient-based treatment setting. We divided these patients by the total number of patients defined as having asthma to calculate the annual asthma exacerbation rate. In addition, all the patients with asthma were divided into 3 groups according to severity levels that were defined according to their medications: mild asthma, low-dose inhaled corticosteroid (ICS); moderate asthma, medium-dose ICS; and severe asthma, high-dose ICS. Each ICS dose was converted to the budesonide-equivalent dose and was then classified as low-, medium- or high-dose ICS according to the annual Global Initiative for Asthma (GINA) guidelines.11 This study was approved by the Ethics Committee of the National Institute of Health (NIH).
Risk factors for asthma exacerbation: analysis of a cohort of adult patients with asthma
For COREA, a total of 1,832 patients with asthma were recruited by allergists or pulmonologists at 23 referral centers in diverse areas of the Republic of Korea.8,12 These patients had experienced dyspnea, cough, sputum production or wheezing for >3 months. All the patients showed positive airway hyperresponsiveness as indicated by a 20% fall in the forced expiration volume in 1 second (FEV1) with a methacholine dose of 16 mg/mL (PC20) during a bronchial provocation test, or positive bronchodilator responsiveness (12% and 200 mL improvement in FEV1 after inhalation of 180 µg of albuterol). At enrollment, the patients' conditions were stable with regular medications. Patients with severe lung damage, bronchiectasis or a history of lung resection were excluded.11 Another independent cohort of patients was registered at the SCH (Bucheon, Korea), and their asthma diagnosis was based on GINA guidelines. All the patients were aged >18 years, and they were regularly followed up and treated with appropriate medications based on the GINA guidelines. Unlike the COREA cohort analysis, longitudinal data for 1 and 3 years were not obtained and analyzed. The design and protocol for this cohort study were approved by the Institutional Review Board of each center (2012-0234). Asthma exacerbation was defined as the presence of 1 or more of the following during the previous year: 1) emergency department visit, 2) unexpected outpatient visit, 3) inpatient or intensive care unit treatment, or 4) use of systemic corticosteroids (>3 consecutive days). According to this definition, we compared the differences between patients who experienced asthma exacerbations and stable patients with asthma without exacerbations, and we considered variables with significant differences to be risk factors.
Statistical analysis
To obtain unbiased estimates of asthma in the general population, we applied the KNHANES sampling weights. We followed the guidelines for reporting sample weight (sampling weights) and stratification designed by the KCDC. This information is also available on the KNHANES website (http://knhanes.cdc.go.kr). In addition, the weights were modified by adjusting for sex and age. Given that samples in the same areas exhibited high correlations, an analysis of prevalence was performed using the generalized linear mixed model method while considering the spatial correlation. We conducted logistic regression and univariate analyses to determine risk factors for asthma exacerbation. Next, we selected statistically significant variables satisfying P<0.05 in the univariate analysis. We then performed a multiple regression with these selected variables to determine the association of asthma exacerbation with each variable. Next, we extracted significant variables that correlated strongly with the deterioration of the patient's asthma and calculated the odds ratios. We further analyzed and compared the risk factors for asthma exacerbation between male and female patients. All the statistical analyses were performed using R software (R Project for Statistical Computing, Vienna, Austria; www.r-project.org). A P value of <0.05 was considered statistically significant.
RESULTS
Prevalence and incidence of asthma in Korea
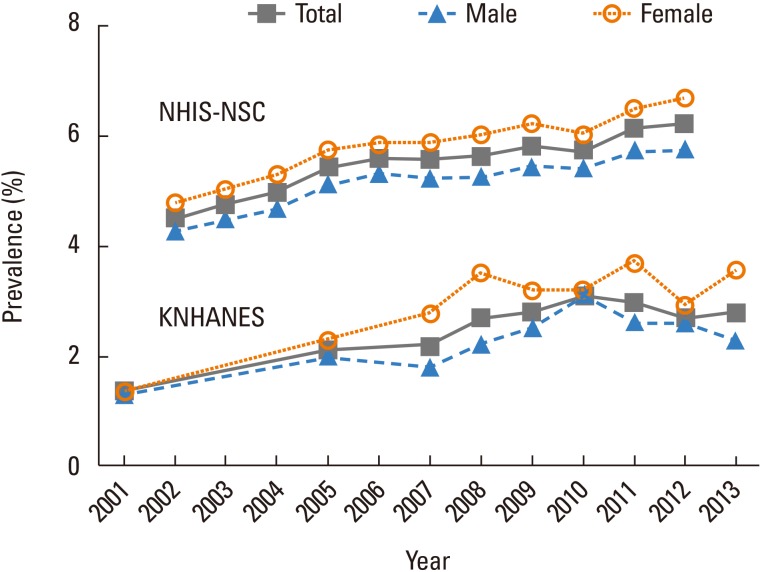
According to the KNHANES database from 1998 to 2013, the annual asthma prevalence among individuals older than 19 years ranged from the lowest rate of 1.2% in 1998 to the highest rate of 3.1% in 2010. The prevalence of asthma was consistently higher among women than among men (Fig. 1 and Supplementary Fig. 1). In particular, the largest sex-based difference in prevalence occurred in 2013, with rates of 2.3% and 3.6% among male and female subjects, respectively (Table 1). An analysis by age revealed a significantly higher prevalence in the elderly group (≥65 years old) than that in the younger group (Table 1 and Supplementary Fig. 1A and B). In particular, the prevalence of asthma among female elderly patients (≥65 years old) in 2013 was 9.7%, or 3-fold higher than that in men (Table 1 and Supplementary Fig. 1C). The KCHS data showed an increasing trend in overall prevalence, and a regional analysis revealed that Chungnam Province had the highest prevalence of 3.0% in 2013. The annual regional trends of asthma prevalence varied, and the prevalence in Jeju Province increased continuously (Table 2). According to the NHIS-NSC database from 2002 to 2012, the prevalence of asthma also increased gradually from 4.5% to 6.2%. Similar to the results of the KNHANES analysis, the prevalence of asthma was significantly higher in women than in men in each year (Table 3 and Supplementary Fig 2A). In addition, the prevalence of asthma was remarkably higher in the elderly group (≥65 years old) than in any other age group of adult patients with asthma (Table 3, Supplementary Fig. 2A and B).
Fig. 1. Prevalence of asthma in Korea: KNHANES database and NHIS-NSC from 2001 to 2013. KNHANES, Korea National Health and Nutrition Examination Survey; NHIS-NSC, National Health Insurance Service-National Sample Cohort.
Table 1. Prevalence of asthma from 1998 to 2013: KNHANES database.
| Characteristics | 1998 | 2001 | 2005 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence* (%) | 1.2 | 1.4 | 2.1 | 2.2 | 2.7 | 2.8 | 3.1 | 3.0 | 2.7 | 2.8 |
| Sex | ||||||||||
| Male | 1.0 | 1.3 | 2.0 | 1.8 | 2.2 | 2.5 | 3.1 | 2.6 | 2.6 | 2.3 |
| Female | 1.3 | 1.4 | 2.3 | 2.8 | 3.5 | 3.2 | 3.2 | 3.7 | 2.9 | 3.6 |
| Age (yr) | ||||||||||
| 19–29 | 0.4 | 0.4 | 1.1 | 0.7 | 2.3 | 2.9 | 3.2 | 3.8 | 2.4 | 3.8 |
| 30–39 | 0.4 | 0.4 | 0.7 | 0.5 | 1.5 | 2.3 | 3.1 | 1.8 | 2.4 | 1.4 |
| 40–49 | 0.6 | 0.7 | 1.2 | 2.0 | 1.7 | 1.7 | 1.5 | 1.6 | 2.5 | 1.3 |
| 50–59 | 1.4 | 1.6 | 2.6 | 3.5 | 2.8 | 2.3 | 2.9 | 2.6 | 2.4 | 2.0 |
| 60–69 | 3.4 | 3.4 | 4.8 | 4.9 | 4.3 | 4.6 | 3.8 | 5.5 | 3.1 | 5.2 |
| ≥ 70 | 4.3 | 6.2 | 8.3 | 7.0 | 8.9 | 5.5 | 6.7 | 6.6 | 5.5 | 7.7 |
| Elderly (≥ 65) | 4.2 | 5.5 | 7.1 | 7.1 | 7.4 | 5.2 | 5.6 | 6.4 | 4.4 | 7.0 |
| Male | 5.2 | 6.2 | 7.4 | 6.2 | 5.1 | 5.0 | 5.1 | 4.8 | 3.9 | 3.2 |
| Female | 3.5 | 5.0 | 6.9 | 7.7 | 8.9 | 5.3 | 6.0 | 7.5 | 4.8 | 9.7 |
KNHANES: Korea National Health and Nutrition Examination Survey.
*Standardized for >19 years of age.
Table 2. Prevalence of asthma by region from 2008 to 2013: KCHS database.
| Regions | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Prevalence (%) | 1.7 | 1.8 | 2.0 | 2.1 | 2.1 | 2.1 |
| Seoul | 1.9 | 2.4 | 2.9 | 2.8 | 2.8 | 2.6 |
| Busan | 2.1 | 1.9 | 2.2 | 2.1 | 2.1 | 2.2 |
| Daegu | 1.7 | 1.5 | 1.4 | 2.0 | 2.2 | 1.8 |
| Incheon | 3.6 | 3.2 | 2.8 | 2.8 | 2.5 | 2.3 |
| Gwangju | 2.5 | 1.7 | 1.9 | 3.0 | 2.7 | 2.5 |
| Daejeon | 1.7 | 1.7 | 2.2 | 2.0 | 2.0 | 1.8 |
| Ulsan | 2.3 | 2.4 | 1.4 | 1.9 | 1.9 | 1.8 |
| Gyeonggi | 2.6 | 2.3 | 2.4 | 2.5 | 2.7 | 2.4 |
| Gangwon | 3.3 | 3.0 | 2.1 | 2.4 | 2.5 | 2.2 |
| Chungbuk | 1.5 | 2.0 | 2.1 | 2.2 | 2.9 | 2.5 |
| Chungnam | 2.3 | 2.1 | 2.6 | 2.3 | 3.2 | 3.0 |
| Chonbuk | 2.1 | 1.5 | 1.5 | 2.5 | 2.6 | 2.7 |
| Chonnam | 2.5 | 2.2 | 2.1 | 2.5 | 2.3 | 2.7 |
| Kyungpook | 1.9 | 1.8 | 1.7 | 1.6 | 1.7 | 2.3 |
| Kyungnam | 2.4 | 1.7 | 1.7 | 1.6 | 1.5 | 1.9 |
| Jeju | 1.9 | 1.5 | 2.5 | 2.5 | 2.7 | 2.7 |
KCHS, Korea Community Health Survey.
Table 3. Prevalence of asthma by age from 2002 to 2012: NHIS-NSC database.
| Characteristics | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence (%) | 4.51 | 4.77 | 4.99 | 5.43 | 5.59 | 5.57 | 5.65 | 5.83 | 5.73 | 6.13 | 6.23 |
| Sex | |||||||||||
| Male | 4.27 | 4.49 | 4.69 | 5.12 | 5.32 | 5.25 | 5.27 | 5.44 | 5.41 | 5.73 | 5.75 |
| Female | 4.76 | 5.06 | 5.29 | 5.74 | 5.86 | 5.88 | 6.03 | 6.23 | 6.05 | 6.52 | 6.71 |
| Age (yr) | |||||||||||
| 1–4 | 26.18 | 29.24 | 30.78 | 33.44 | 36.45 | 37.79 | 38.31 | 37.90 | 40.11 | 40.66 | 39.01 |
| 5–9 | 12.20 | 13.04 | 13.95 | 16.57 | 17.84 | 17.75 | 17.33 | 19.85 | 19.85 | 22.06 | 20.17 |
| 10–14 | 4.01 | 3.45 | 4.00 | 4.56 | 4.99 | 4.48 | 4.68 | 6.11 | 5.88 | 6.53 | 5.99 |
| 15–19 | 1.13 | 1.22 | 1.39 | 1.53 | 1.86 | 1.82 | 1.92 | 2.58 | 2.40 | 2.50 | 2.66 |
| 20–24 | 0.95 | 1.02 | 1.21 | 1.35 | 1.42 | 1.51 | 1.47 | 1.68 | 1.74 | 1.84 | 2.08 |
| 25–29 | 1.39 | 1.47 | 1.63 | 1.85 | 1.94 | 1.92 | 1.97 | 2.09 | 2.12 | 2.17 | 2.39 |
| 30–34 | 2.00 | 2.21 | 2.25 | 2.62 | 2.64 | 2.80 | 2.65 | 2.84 | 2.74 | 2.83 | 2.91 |
| 35–39 | 2.08 | 2.18 | 2.37 | 2.67 | 2.70 | 2.90 | 2.89 | 3.01 | 2.92 | 3.09 | 3.35 |
| 40–44 | 2.07 | 2.18 | 2.37 | 2.64 | 2.67 | 2.78 | 2.87 | 2.79 | 2.74 | 2.97 | 3.16 |
| 45–49 | 2.22 | 2.39 | 2.61 | 2.89 | 2.85 | 2.99 | 3.09 | 3.01 | 2.94 | 3.07 | 3.28 |
| 50–54 | 2.74 | 2.95 | 3.14 | 3.33 | 3.32 | 3.45 | 3.70 | 3.53 | 3.33 | 3.55 | 3.82 |
| 55–59 | 3.49 | 3.86 | 4.15 | 4.46 | 4.32 | 4.43 | 4.65 | 4.45 | 4.30 | 4.58 | 4.93 |
| 60–64 | 4.36 | 4.99 | 5.13 | 5.55 | 5.48 | 5.47 | 5.72 | 5.38 | 5.25 | 5.47 | 6.04 |
| 65–69 | 5.19 | 5.98 | 6.19 | 6.59 | 6.68 | 6.73 | 6.99 | 7.10 | 6.85 | 7.25 | 7.62 |
| 70–74 | 6.34 | 7.00 | 7.08 | 7.43 | 7.26 | 7.71 | 8.26 | 8.02 | 7.17 | 8.18 | 8.89 |
| 75–79 | 6.85 | 7.46 | 7.20 | 7.85 | 7.84 | 7.79 | 8.76 | 8.10 | 7.46 | 9.28 | 9.85 |
| ≥ 80 | 4.55 | 4.70 | 5.44 | 5.42 | 5.68 | 6.02 | 6.55 | 6.24 | 5.81 | 6.86 | 8.10 |
| Elderly ( ≥ 65) | 5.88 | 6.58 | 6.70 | 7.10 | 7.11 | 7.22 | 7.77 | 7.58 | 7.06 | 8.06 | 8.70 |
NHIS-NSC, National Health Insurance Service-National Sample Cohort.
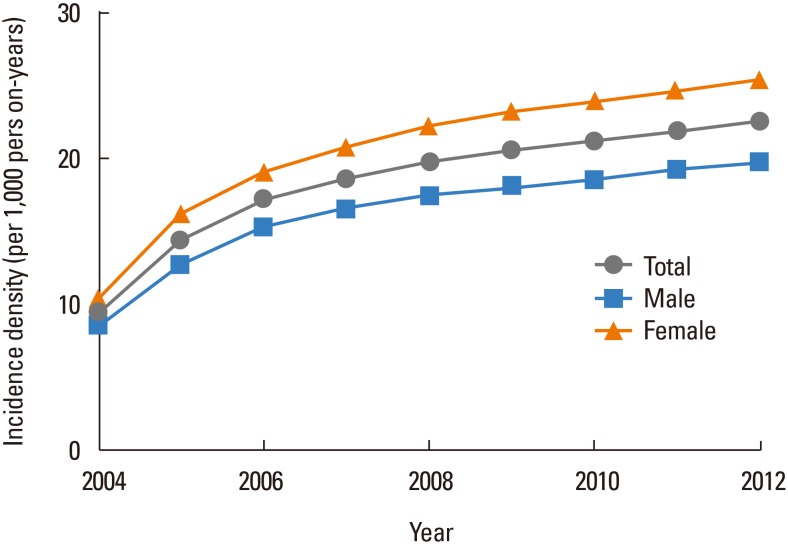
According to the NHIS-NSC database analysis, the overall incidence of asthma per year has exceeded 20 per 1,000 person-years since 2009. Interestingly, the asthma incidence was always higher among women than among men (Table 4 and Fig. 2).
Table 4. Incidence of asthma by sex from 2004 to 2012: NHIS-NSC database.
| Characteristics | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|---|---|---|---|
| Number of people with newly diagnosed asthma | 26,734 | 53,141 | 76,617 | 100,006 | 119,567 | 139,600 | 159,303 | 180,713 | 201,970 |
| Person-year (from 2002) | 2,781,429 | 3,663,136 | 4,446,443 | 5,349,011 | 6,018,190 | 6,755,781 | 7,505,520 | 8,234,300 | 8,942,868 |
| Incidence density (per 1,000 person-years) | 9.612 | 14.507 | 17.231 | 18.696 | 19.868 | 20.664 | 21.225 | 21.946 | 22.584 |
| Sex | |||||||||
| Male | 8.599 | 12.856 | 15.343 | 16.569 | 17.521 | 18.152 | 18.638 | 19.274 | 19.798 |
| Female | 10.677 | 16.181 | 19.149 | 20.861 | 22.272 | 23.242 | 23.887 | 24.702 | 25.465 |
NHIS-NSC, National Health Insurance Service-National Sample Cohort
Fig. 2. Incidence of asthma by sex from 2004 to 2012: NHIS-NSC database. NHIS-NSC, National Health Insurance Service-National Sample Cohort.
Asthma severity and acute asthma exacerbation rate according to the NHIS-NSC database and risk factors for exacerbation in the COREA cohort
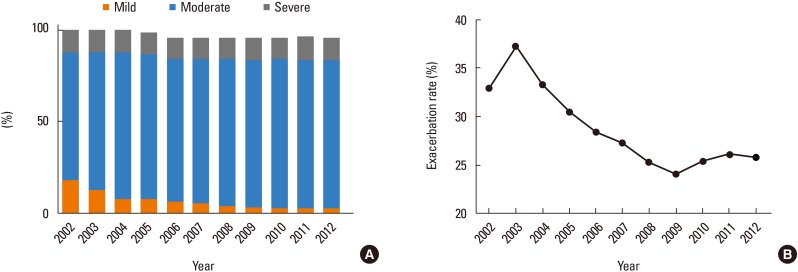
Approximately 80% of the patients had moderate asthma; accordingly, this condition was most prevalent. Approximately 11% of the patients had severe asthma (Supplementary Table 2 and Fig. 3A). The annual asthma exacerbation rates ranged between 25% and 35%, with a decreasing trend over time until 2009, followed by a plateau since 2010 (Supplementary Table 2 and Fig. 3B).
Fig. 3. Asthma severity and exacerbation: NHIS-NSC database. (A) Distribution of asthma severity from 2002 to 2012. (B) Asthma exacerbation rate from 2002 to 2012. NHIS-NSC, National Health Insurance Service-National Sample Cohort.
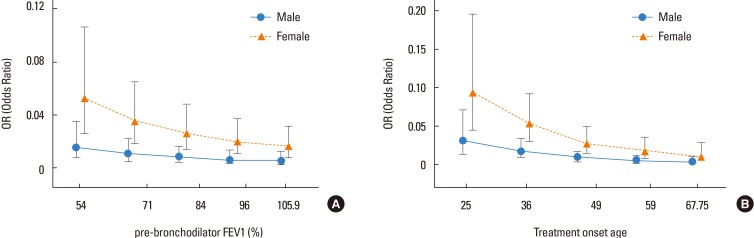
Among COREA's 1,832 patients with asthma, 213 (11.6%) experienced 1 or more exacerbations during the year after enrollment. A univariate analysis identified sex, baseline pulmonary function, treatment duration, and lung function variability or changes in Asthma Control Test (ACT) scores over 1 and 3 years as significant associated factors (Table 5). A multiple regression analysis identified 6 risk factors for acute asthma exacerbation. These factors included sex, baseline pulmonary function (FEV1, FVC, FEV1/FVC), treatment duration, lung function variability over a 1 year period, changes in ACT score over a 1-year period and changes in ACT score over a 3-year period (Table 5). In other words, female sex, a lower pulmonary function at baseline, longer treatment duration, or wide fluctuations in the FEV1 or ACT during the treatment course were identified as risk factors for an acute asthma exacerbation within 1 year. A lower baseline lung function and longer treatment duration were identified as important risk factors for asthma exacerbations, especially in women (Fig. 4A and B). The results of analysis of the SCH cohort were similar to that of COREA. Of the total 2,195 individuals with asthma, 283 (12.9%) experienced exacerbation during the year after enrollment. Lower baseline lung functions (FEV1 and FVC) were also identified as a risk factor. Female sex showed a higher risk of acute exacerbation than male sex, but it was not statistically significant (Supplementary Table 3).
Table 5. Identified risk factors for asthma exacerbation: COREA cohort database.
| Characteristics | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | P value | No. of patients | OR | P value | No. of patients | |
| Age | 1.01 | 0.147 | 1,832 | |||
| Sex (female)* | 1.76 | < 0.001 | 1,832 | 1.87 | 0.006 | 995 |
| BMI | 0.99 | 0.986 | 1,802 | |||
| Pack-years | 0.99 | 0.435 | 1,627 | |||
| Pre-bronchodilator FEV1 (%) | 0.99 | 0.001 | 1,726 | 0.98 | 0.002 | 995 |
| Pre-bronchodilator FVC (%) | 0.99 | 0.016 | 1,726 | |||
| Pre-bronchodilator FEV1/FVC | 0.14 | < 0.001 | 1,727 | 0.111 | 0.039 | 995 |
| Post-bronchodilator FEV1 (%) | 0.99 | 0.012 | 1,023 | |||
| Post-bronchodilator FVC (%) | 0.99 | 0.108 | 986 | |||
| Post-bronchodilator FEV1/FVC | 0.26 | 0.043 | 1,022 | |||
| PC20 | 0.98 | 0.492 | 772 | |||
| Blood eosinophil (%) | 0.97 | 0.135 | 1,524 | |||
| Blood eosinophil (count) | 0.99 | 0.411 | 1,523 | |||
| Sputum eosinophil (%) | 0.99 | 0.399 | 333 | |||
| Sputum neutrophil (%) | 1.00 | 0.950 | 336 | |||
| Blood total IgE (IU/mL) | 0.99 | 0.134 | 786 | |||
| Log (total IgE) | 0.76 | 0.111 | 786 | |||
| CRP (mg/dL) | 0.98 | 0.854 | 794 | |||
| Allergic rhinitis | 0.74 | 0.137 | 1,029 | |||
| Aspirin hypersensitivity | 0.45 | 0.272 | 66 | |||
| Duration of asthma (month) | 1.00 | 0.051 | 1,657 | |||
| Symptom duration (month) | 1.00 | 0.380 | 1,803 | |||
| Duration of treatment (month) | 1.00 | 0.003 | 1,581 | 1.01 | 0.014 | 995 |
| Age at disease onset | 1.00 | 0.807 | 1,657 | |||
| History of asthma exacerbation | 1.83 | 0.001 | 1,809 | 1.46 | 0.055 | 995 |
| Mean of ΔFEV1 over 1 year (%) | 1.07 | < 0.001 | 933 | 1.06 | 0.002 | 796 |
| Mean of ΔFEV1 over 3 years (%) | 1.09 | 0.016 | 470 | 1.04 | 0.289 | 451 |
| Mean of ΔACT over 1 year (score) | 1.31 | < 0.001 | 857 | 1.27 | < 0.001 | 796 |
| Mean of ΔACT over 3 years (score) | 1.55 | < 0.001 | 468 | 1.50 | < 0.001 | 451 |
| Average ICS dose over 1 year (µg/day) | 1.00 | 0.227 | 1,381 | |||
| Average ICS dose over 3 years (µg/day) | 1.00 | 0.284 | 1,447 | |||
COREA, Cohort for Reality and Evolution of Adult Asthma in Korea; OR, odds ratio; BMI, body mass index; FEV1, forced expiration volume in 1 second; FVC, forced vital capacity; PC20, concentration of methacholine that caused a 20% fall in FEV1; IgE, immunoglobulin E; CRP, C-reactive protein; ACT, Asthma Control Test; ICS, inhaled corticosteroid. ΔFEV1: the absolute values for the changes in the FEV1 (which were measured over 3-months intervals). ΔACT: the absolute values for the changes in the ACT (which were measured over 3-months intervals).
*The sex defines female as related to male.
Fig. 4. Risk of asthma exacerbation by sex: COREA asthma cohort analysis. (A) According to baseline lung function. (B) According to treatment onset age.
DISCUSSION
The results of this study demonstrate that the prevalence of asthma in Korea continues to increase steadily and is consistently higher in elderly women. Furthermore, elderly women with asthma exhibited a significantly higher risk of asthma exacerbation. On the basis of these results, additional strategies for effective prevention and management of asthma should be established, and elderly female patients with asthma should be given particular attention.
Regarding the improved management of chronic diseases such as asthma, basic information about the disease iuncluding the prevalence, incidence, clinical features, risk factors for development and burden is critically important. Accordingly, analyses of national health surveys could help establish strategies for the prevention and effective management of asthma. However, epidemiologic studies on asthma are difficult, given that asthma is highly heterogeneous and that there is no standardized definition of the disease.1 If these limitations are not properly addressed, the data from some national health surveys may not be completely reliable; therefore, studies based on national datasets are somewhat uncommon in Korea. In the current study, we attempted to analyze and compare the prevalence of asthma in 3 nationally representative samples of the general Korean population: the KNHANES, KCHS and NHIS-NSC databases. Although each database has different characteristics and contains diverse information, the 3 are relatively reliable and can be considered representative of the Korean population. This was the first study to compare these 3 national health datasets.
In this study, the overall prevalence of asthma exhibited a consistent increasing trend, with slight differences among the databases. In the KNHANES database, the prevalence ranged from approximately 1.2% to 3.1%, whereas the ranges were 1.7% to 2.1% and 4.5% to 6.2% in the KCHS and NHIS-NSC databases, respectively. Although both the KNHANES and the KCHS defined asthma as a physician-diagnosed condition, the results differed between these datasets, and the NHIS-NSC database showed the highest prevalence. The difference in asthma prevalence rates between these 3 databases can be attributed to the different criteria used for asthma diagnoses and differences in the populations. In addition, the unique health insurance system in Korea was assumed to contribute to the higher prevalence of asthma in the analysis of NHIS-NSC data, compared with other databases.
It is likely that more “asthma” cases have been entered into the system than there are true cases of asthma due to the inclusion of self-reported cases of asthma. One study on the KNHANES data in 2010 reported an overall asthma prevalence of 4.1%, with rates of 4.7% among males and 3.2% among females.13 In that study, the authors defined asthma as a self-reported condition, which may have led to a higher prevalence compared with the results of our study which defined asthma as a physician-diagnosed condition. Thus, the importance of a consistent working definition of asthma should be emphasized in future studies.
Asthma prevalence differs from country to country. Compared with our results, the asthma prevalence in other Asian countries varies from 1.2% in China to 6.7% in India. In the United States, the asthma prevalence is approximately 7.8%, and similarly to our results, the rate of females with asthma is higher than that of males (9.1%).3,14,15,16,17
The NHIS-NSC database analysis revealed a very high prevalence of childhood asthma (>20%), followed by a sudden decrease in adulthood. We attribute this pattern to the difficulty in diagnosing childhood asthma with the same methods used for adults. Accordingly, patients who are not actually asthmatic might have been included among the childhood asthma cases. Furthermore, childhood asthma could feasibly differ phenotypically from adult-onset asthma in terms of disease sustainability. Compared with childhood asthma, adult-onset asthma is suggested to be more severe, less responsive to treatment and more likely to cause a decline in lung function.18,19 Therefore, it is important to conduct a separate analysis of an adult asthma database in order to identify the clinical course of adult asthma and ultimately establish better strategies and policies for improving asthma management.
In this study, the prevalence and incidence of asthma continued to increase in the Korean population. According to the NHIS-NSC database from 2002 to 2012, the incidence of asthma ranged from 9.6 to 22.6 per 1,000 person-years, and we observed an increasing trend each year. Interestingly, this tendency was more prominent in women. In contrast, some recent studies reported a decreasing prevalence of asthma in other counties as well as Korea.1,20,21 Given that our study only analyzed data collected until 2013, the latest trends in asthma prevalence could be different. In addition, differences in the working definition of asthma could have contributed to differences in the results of these studies.
Despite the conflicting results regarding overall asthma prevalence, all studies reported a consistently high prevalence of asthma among women and elderly individuals.20,22 Many studies have identified a higher prevalence of asthma among post-pubertal females,5,25,26 whereas asthma is more common among males before puberty.5,15,23,24 These sex-based discrepancies in asthma prevalence and outcomes are evident. In 2009, the US National Health Interview Survey also reported asthma prevalence rates of 7.7% and 11.9% among girls and boys younger than 15 years of age, respectively, and asthma prevalence rates of 9.6% and 6.3% among women and men aged 15–34 years, respectively. This difference continued to increase in adults older than 35 years, with rates of 10.1% among women and 5.6% among men.24 A mechanism underlying the higher prevalence of late-onset female asthma has been suggested. Sex hormones affect immune regulation, and the effects of estrogen on eosinophils and mast cells could be linked to the development of asthma in women.22,27 Among postmenopausal women, decreasing estradiol levels might reduce the protective effects of hormones on the development of lung inflammation and thereby increase susceptibility to asthma.22,28 Nevertheless, the precise mechanism underlying the increased susceptibility of elderly women to asthma remains unclear, and further studies are warranted.
In this study, approximately 11% of all asthma cases were defined as severe asthma requiring high-dose ICS, although this rate might not be accurate. According to the European Respiratory Society/American Thoracic Society guidelines, the estimated prevalence of severe asthma ranges from 5% to 10% of all asthma cases, although the exact prevalence is unknown.29,30 Our study indicated a higher proportion of severe asthma cases in Korea compared with other developed countries. Given the limitations of health survey data, we considered cases requiring the prescription of high-dose ICS to indicate severe asthma; however, more information is needed to precisely diagnose severe asthma.31,32 Nevertheless, it remains clear that Korea faces a substantial burden from severe asthma.
Previous studies clearly indicated higher rates of asthma morbidity and mortality among elderly patients.15,33 In patients with asthma, lung function is also associated with a rapid age-related decline in FEV1.33,34 A study on the prevalence of severe asthma reported rates of 60% or higher among women.35 Although few studies have attempted to determine the cause of more severe asthma among elderly women, some studies have suggested that the various effects of sex hormones such as estrogen and progesterone could lead to the clinical features of asthma.36,37,38 Given the substantial burden of asthma on elderly female patients, the mechanism underlying the development of this subtype of asthma merits further investigation.
In our analysis of a patient cohort, older age and female sex were also identified as risk factors for asthma exacerbation. In addition to the higher prevalence rates among these patient subsets relative to others, this result suggests that elderly female patients with asthma should be separately considered an important subgroup. Furthermore, the results of cluster analyses conducted in several studies also showed that female sex is the critical factor differentiating unique clusters.7,31
This study has some limitations. First, the working definition of asthma used in the analysis was not based on standardized methodology. Therefore, the prevalence rates reported in this study might differ from those reported in other studies. However, when evaluating the databases, we used the criterion of “physician-diagnosed asthma” to maximize the accuracy of our analysis. In the KNHANES and KCHS, physician-diagnosed asthma is generally lifetime prevalence of asthma. Therefore, it might show only asthma history, and its recall bias is also problematic. Secondly, there is a possibility that the actual incidence of asthma is higher than what is reported. The NHIS-NSC cohort is characterized by a gradual increase in the proportion of children and young people because the cohort added newborns annually to the number of individuals lost in order to maintain a sampling rate of 2.2%. The prevalence of pediatric asthma was also significantly higher, and it was estimated that these characteristics influenced incidence as the proportion of children increased. Thirdly, we defined asthma severity only by the prescribed ICS dose. We did not consider the use of other medications. In addition, survey databases did not contain ACT scores, repeated pulmonary function test results, or information on drug adherence; accordingly, it was not possible to distinguish severe refractory asthma from undertreated severe asthma.
In conclusion, the prevalence of asthma in Korea has been increasing in recent decades. Notably, elderly women exhibited the highest prevalence and incidence of asthma, and they also tended to have more severe disease with a higher exacerbation rate. Therefore, we emphasize that the effective management of elderly female patients with asthma is critically important and that further additional studies on this specific patient subset are needed. Specific management strategies for elderly women with asthma might be needed to achieve better disease control and reduce the associated burden.
ACKNOWLEDGMENTS
This research was supported by a fund (2014-ER5605-00) from Research of Korea Centers for Disease Control and Prevention.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIALS
Diagnosis, drug and procedure codes with descriptions
Distribution of asthma severity and rate of exacerbation from 2002 to 2012: NHIS-NSC database
Identified risk factors for asthma exacerbation: SCH asthma cohort database (replication)
Prevalence of asthma in Korea: KNHANES database. (A) Prevalence of adult asthma from 1998 to 2013. (B) Comparison of prevalence according to age for five years, from 2009 to 2013. (C) Comparison of prevalence according to age and sex in 2013.
Prevalence of asthma in Korea: NHIS-NSC database. (A) Prevalence of asthma from 2002 to 2012. (B) Comparison of prevalence according to age from 2010 to 2012.
References
- 1.Sears MR. Trends in the prevalence of asthma. Chest. 2014;145:219–225. doi: 10.1378/chest.13-2059. [DOI] [PubMed] [Google Scholar]
- 2.Uphoff EP, Cabieses B, Wright J, Pickett KE. International prevalence rates of asthma and allergy are associated with income inequality. J Allergy Clin Immunol. 2015;136:189–190.e2. doi: 10.1016/j.jaci.2015.01.037. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song WJ, Kang MG, Chang YS, Cho SH. Epidemiology of adult asthma in Asia: toward a better understanding. Asia Pac Allergy. 2014;4:75–85. doi: 10.5415/apallergy.2014.4.2.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn RM, Lehman E, Chinchilli VM, Martin RJ, Boushey HA, Israel E, et al. Impact of age and sex on response to asthma therapy. Am J Respir Crit Care Med. 2015;192:551–558. doi: 10.1164/rccm.201503-0426OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. 2008;178:218–224. doi: 10.1164/rccm.200711-1754OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim TB, Jang AS, Kwon HS, Park JS, Chang YS, Cho SH, et al. Identification of asthma clusters in two independent Korean adult asthma cohorts. Eur Respir J. 2013;41:1308–1314. doi: 10.1183/09031936.00100811. [DOI] [PubMed] [Google Scholar]
- 9.Kim Y. The Korea National Health and Nutrition Examination Survey (KNHANES): current status and challenges. Epidemiol Health. 2014;36:e2014002. doi: 10.4178/epih/e2014002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46:e15. doi: 10.1093/ije/dyv319. [DOI] [PubMed] [Google Scholar]
- 11.Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet] [place unknown]: Global Initiative for Asthma; 2014. [updated 2015 Aug 12]. [cited 2017 Nov 12]. Available from: http://www.ginasthma.org/ [Google Scholar]
- 12.Kim TB, Park CS, Bae YJ, Cho YS, Moon HB COREA Study Group. Factors associated with severity and exacerbation of asthma: a baseline analysis of the cohort for reality and evolution of adult asthma in Korea (COREA) Ann Allergy Asthma Immunol. 2009;103:311–317. doi: 10.1016/S1081-1206(10)60530-3. [DOI] [PubMed] [Google Scholar]
- 13.Park HJ, Kim EJ, Yoon D, Lee JK, Chang WS, Lim YM, et al. Prevalence of self-reported allergic diseases and IgE levels: a 2010 KNHANES analysis. Allergy Asthma Immunol Res. 2017;9:329–339. doi: 10.4168/aair.2017.9.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. Current asthma prevalence percents by age, sex, and race/ethnicity, United States. Atlanta (GA): Centers for Disease Control and Prevention; 2015. [updated 2016 Sep 8]. [cited 2017 Nov 12]. Available from: https://www.cdc.gov/asthma/asthmadata.htm. [Google Scholar]
- 15.Asthma Facts. CDC's National Asthma Control Program Grantees [Internet] Atlanta (GA): Centers for Disease Control and Prevention; 2013. [updated 2013 Jul]. [cited 2017 Nov 12]. Available from: https://www.cdc.gov/asthma/ [Google Scholar]
- 16.Bishwajit G, Tang S, Yaya S, Feng Z. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chron Obstruct Pulmon Dis. 2017;12:1093–1099. doi: 10.2147/COPD.S133148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma Q, Yang T. Prevalence and influential factors for asthma among adults in Chinese. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2017;42:1086–1093. doi: 10.11817/j.issn.1672-7347.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 18.de Nijs SB, Venekamp LN, Bel EH. Adult-onset asthma: is it really different. Eur Respir Rev. 2013;22:44–52. doi: 10.1183/09059180.00007112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Westerhof GA, Coumou H, de Nijs SB, Weersink EJ, Bel EH. Clinical predictors of remission and persistence of adult-onset asthma. J Allergy Clin Immunol. 2018;141:104–109.e3. doi: 10.1016/j.jaci.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 20.Kim BK, Kim JY, Kang MK, Yang MS, Park HW, Min KU, et al. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol Int. 2016;65:186–191. doi: 10.1016/j.alit.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 22.Triebner K, Johannessen A, Puggini L, Benediktsdóttir B, Bertelsen RJ, Bifulco E, et al. Menopause as a predictor of new-onset asthma: a longitudinal Northern European population study. J Allergy Clin Immunol. 2016;137:50–57.e6. doi: 10.1016/j.jaci.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 23.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–666. doi: 10.1164/rccm.200611-1717OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newcomb DC, Cephus JY, Boswell MG, Fahrenholz JM, Langley EW, Feldman AS, et al. Estrogen and progesterone decrease let-7f microRNA expression and increase IL-23/IL-23 receptor signaling and IL-17A production in patients with severe asthma. J Allergy Clin Immunol. 2015;136:1025–1034.e11. doi: 10.1016/j.jaci.2015.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kynyk JA, Mastronarde JG, McCallister JW. Asthma, the sex difference. Curr Opin Pulm Med. 2011;17:6–11. doi: 10.1097/MCP.0b013e3283410038. [DOI] [PubMed] [Google Scholar]
- 26.Almqvist C, Worm M, Leynaert B Working Group of GA2LEN WP 2.5 Gender. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63:47–57. doi: 10.1111/j.1398-9995.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- 27.Zierau O, Zenclussen AC, Jensen F. Role of female sex hormones, estradiol and progesterone, in mast cell behavior. Front Immunol. 2012;3:169. doi: 10.3389/fimmu.2012.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009;181:E181–E190. doi: 10.1503/cmaj.080612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mincheva R, Ekerljung L, Bossios A, Lundbäck B, Lötvall J. High prevalence of severe asthma in a large random population study. J Allergy Clin Immunol. doi: 10.1016/j.jaci.2017.07.047. Forthcoming 2017. [DOI] [PubMed] [Google Scholar]
- 30.Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–373. doi: 10.1183/09031936.00202013. [DOI] [PubMed] [Google Scholar]
- 31.Lefaudeux D, De Meulder B, Loza MJ, Peffer N, Rowe A, Baribaud F, et al. U-BIOPRED clinical adult asthma clusters linked to a subset of sputum omics. J Allergy Clin Immunol. 2017;139:1797–1807. doi: 10.1016/j.jaci.2016.08.048. [DOI] [PubMed] [Google Scholar]
- 32.Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, et al. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med. 2005;171:440–445. doi: 10.1164/rccm.200405-623OC. [DOI] [PubMed] [Google Scholar]
- 33.Hanania NA, King MJ, Braman SS, Saltoun C, Wise RA, Enright P, et al. Asthma in the elderly: current understanding and future research needs--a report of a National Institute on Aging (NIA) workshop. J Allergy Clin Immunol. 2011;128:S4–S24. doi: 10.1016/j.jaci.2011.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.James AL, Palmer LJ, Kicic E, Maxwell PS, Lagan SE, Ryan GF, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med. 2005;171:109–114. doi: 10.1164/rccm.200402-230OC. [DOI] [PubMed] [Google Scholar]
- 35.Hekking PP, Wener RR, Amelink M, Zwinderman AH, Bouvy ML, Bel EH. The prevalence of severe refractory asthma. J Allergy Clin Immunol. 2015;135:896–902. doi: 10.1016/j.jaci.2014.08.042. [DOI] [PubMed] [Google Scholar]
- 36.Baptist AP, Hamad A, Patel MR. Special challenges in treatment and self-management of older women with asthma. Ann Allergy Asthma Immunol. 2014;113:125–130. doi: 10.1016/j.anai.2014.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Balzano G, Fuschillo S, Melillo G, Bonini S. Asthma and sex hormones. Allergy. 2001;56:13–20. doi: 10.1034/j.1398-9995.2001.00128.x. [DOI] [PubMed] [Google Scholar]
- 38.Zemp E, Schikowski T, Dratva J, Schindler C, Probst-Hensch N. Asthma and the menopause: a systematic review and meta-analysis. Maturitas. 2012;73:212–217. doi: 10.1016/j.maturitas.2012.08.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnosis, drug and procedure codes with descriptions
Distribution of asthma severity and rate of exacerbation from 2002 to 2012: NHIS-NSC database
Identified risk factors for asthma exacerbation: SCH asthma cohort database (replication)
Prevalence of asthma in Korea: KNHANES database. (A) Prevalence of adult asthma from 1998 to 2013. (B) Comparison of prevalence according to age for five years, from 2009 to 2013. (C) Comparison of prevalence according to age and sex in 2013.
Prevalence of asthma in Korea: NHIS-NSC database. (A) Prevalence of asthma from 2002 to 2012. (B) Comparison of prevalence according to age from 2010 to 2012.