Recent United Nations General Assembly political resolution on antimicrobial resistance (AMR) articulates serious concerns of the global community, including the political leadership at the highest level on the impact of this burgeoning issue with profound implications not only on human health but more so on economy, food security and overall human development1. The review on AMR projects AMR causing 10 million deaths annually and wiping off a massive cumulative US$ 100 trillion from economy by 2050 as a consequence of inaction to contain AMR2. This report also estimates that mortality due to AMR globally shall exceed those due to cancers and road accidents put together. Moreover, most of these deaths will be in developing countries creating greater impact on health and economy. Data from World Bank reveal that global exports will see a decrease of up to 3.5 per cent, livestock production will diminish by 7.5 per cent and additional healthcare-related costs will be staggering US$ 1 trillion by 20503.
At clinical and public health platforms, patients with infections caused by drug-resistant bacteria are at increased risk of worse clinical outcomes and death and consume more healthcare resources than patients infected with non-resistant strains of the same bacteria4 Outbreaks with resistant strains lead to serious outcomes. The WHO estimates that carbapenem antibiotics which are the last resort treatment for Klebsiella pneumoniae infections do not work in more than half of the people treated for hospital-associated infections due to this organism, fluoroquinolone resistance in Escherichia coli has become widespread and is ineffective in 50 per cent patients in some geographical areas. Ten countries have reported treatment failure in gonorrhoea to third-generation cephalosporins. Methicillin-resistant Staphylococcus aureus (MRSA) are firmly entrenched in healthcare facilities making people infected with MRSA, 64 per cent more likely to die than people with a non-resistant form of the infection4.
AMR is a public health concern in India. Carbapenem-resistant isolates of K. pneumoniae increased from 29 per cent in 2008 to 57 per cent in 2014 and MRSA showed an increase of 18 per cent during this period5. Seventy eight per cent of clinical isolates of Neisseria gonorrhoeae were resistant to ciprofloxacin6. Sixty one per cent of E. coli were extended-spectrum beta-lactamase (ESBL) producers7. Acinetobacter species responsible for hospital-associated infections in a tertiary care hospital in Delhi showed 57-80 per cent resistance to imipenem8.
The health sector has been developing various strategies and plans to combat AMR. Its complexities and various competing national priorities demand a strategic, efficient and cost-effective doable approach that can yield rich dividend in short term. Although almost one hundred countries in the world have drafted their respective national action plans, almost all are finding it difficult to initiate implementation of their national action plans against AMR because of the complexity and internecine nature of the problem. It is neither technically nor financially feasible to have a stand-alone national programme, especially in developing countries. These countries have to thus identify a point of entry for AMR implementation that is doable, practical and feasible. This article discusses about universal health coverage (UHC) initiative as a possible and workable entry point for AMR national action plans as well as an ideal enabling platform since it can support various AMR specific as well as AMR sensitive interventions9.
UHC is the aspiration that all people obtain quality promotive, preventive, curative, rehabilitative and palliative health services without suffering financial hardship paying for them. It occupies a prominent place in the United Nation's Sustainable Development Goals (SDGs)10,11. UHC is dependent on an efficient health system. At the same time, countries with strong health system shall indeed have better outcomes from their UHC activities. Its successful implementation from now onwards shall strengthen health system in the countries which have traditionally suffered from weak health systems providing comprehensive benefits to people.
UHC is recognized as a development promoting endeavour that carries tremendous potential to enhance economic growth by enabling adults to work and earn an income and children obtain an education, thus keeping them away from poverty. It thus neutralizes a major impact of AMR of pushing people into avoidable poverty. World Bank estimates that if left uncontrolled AMR shall push 28 million people into poverty3. Accordingly, AMR containment through UHC can be the key to achieving the World Bank Group's twin goals of ending extreme poverty and increasing equity and shared prosperity12,13. UHC can act as an enabling platform through improved governance, an expanded coverage in activities such as vaccination, preventative care and hygiene measures that reduce disease burden thus bringing about a proportionate reduction of antimicrobial agents and resultant spread of resistance; improved supervision that assures use of standardized protocol leading to rational use of antimicrobials; improving access to affordable antimicrobials and systematic approach to complex problem of AMR. UHC improves access to health services and dramatically reduce out-of-pocket expenditure by the communities especially the poorer segments.
A WHO and World Bank Group report launched in 201514 showed that 400 million people did not have access to essential health services leading to significant out-of-pocket expenditure. At 62 per cent, India's out-of-pocket expenditure for health is one of the highest in the world15. To overcome this and in alignment with global initiatives, India is embarking on an ambitious target of achieving UHC for all16.
One of the major interventions in overall fight against AMR is improving access of antimicrobial agents to vulnerable populations. Through UHC, this becomes feasible as improving access aligns with the core UHC objective.
All UN Member States have agreed to try to achieve UHC by 2030, as part of the SDGs. Several countries have already initiated UHC reforms. UHC is being recognized even by developing countries as a revolutionary public health aspiration to catalyze development and negate several ill-effects of poor health. Given the pan-global prevalence of resistant pathogens17, UHC comes out to be the ideal platform for extending activities that prevent and contain AMR.
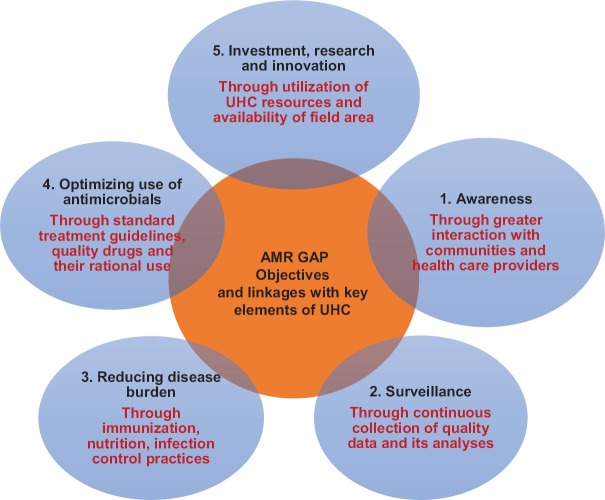
UHC is not just about health financing. It strengthens all components of the health system. The UHC promoted strong health system shall be better equipped to launch effective measures to contain AMR. UHC impacts all key elements of WHO Global Action Plan on AMR (Figure).
Figure.
Linkages between objectives of antimicrobial resistance (AMR) action plan and key elements of Universal Health Coverage (UHC). Objectives of WHO Global Action Plan (GAP) on AMR are shown in bold. UHC key elements influencing specific GAP objectives are shown in red.
Recognizing that sustainability of financing is one of the most important challenges to achieve UHC, World Bank and other partners are financing UHC in several developing countries. At the same time, implementation of AMR stands at risk of getting hampered because of inadequate or erratic availability of resources. Instead of lobbying for significant budgets from dwindling and finite global resources for development purposes, it will be cost-effective for AMR activities to dovetail into UHC. It shall promote access to quality antimicrobials and their rational use.
UHC under its pillar of providing quality health care shall be using standard treatment guidelines and quality antimicrobial agents for common ailments including diarrhoeal diseases and acute respiratory infections (ARI). These will substantially reduce widespread indiscriminate use of antimicrobial agents including those of questionable quality in ARI and diarrhoea18.
UHC aims to expand health services to cover entire population in a geographical area. Apart from curative services, UHC has a focus on preventive services, especially vaccination and disease prevention interventions, which shall contribute to a reduction in disease burden. This shall lower the need for antimicrobials and thus prevent emergence and spread of AMR.
The confidence of community in sustained availability of quality health care through stronger health system under UHC will prevent the storing and self-medication of antimicrobial agents. It may catalyze a behavioural change in the community towards rational use of antimicrobials by them.
On working under the broad umbrella of UHC, AMR activities shall derive management benefits from UHC's inbuilt service delivery, outreach and logistics related components. Apart from efficient utilization of available human resource, data management and infrastructure under UHC, bulk procurement of antimicrobials shall reduce the cost and improve the quality of these agents. A robust UHC approach shall build systems governance and coordination capacities that will be critical for the AMR fight.
UHC has been prominently public-sector approach. Given the growing importance of private sector in several countries, UHC needs to engage and establish workable linkages with private sector for improving efficacy and reach of UHC for AMR containment. As with many other developing countries, India's current public healthcare spending and infrastructure is currently well short of what is required to fulfil its ambition of achieving universal health care19. Ninety three per cent of all health facilities in India belong to private sector; and hence, public-private-partnership (PPP) will have to play a major role20. Several successful PPP models have emerged over the last few years. Rashtriya Swasthya Bima Yojana, launched in 2008, has been successful in enhancing health coverage for poor households in India21. However, for a nation-wide successful implementation of UHC for AMR containment several such PPPs need to be established and nurtured.
Can AMR be measured within UHC?
Together with the World Bank, WHO has developed a framework to track the progress of UHC22. WHO uses indicators in four categories, namely, reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases and service capacity and access (including access to essential medicines). Within the category of infectious diseases, it is proposed to measure TB treatment, HIV antiretroviral treatment, coverage of insecticide-treated bed nets for malaria prevention and adequate sanitation. It is feasible to include at least a few critical indicators from respective National Action Plans into the framework of monitoring and evaluation of UHC.
How to move forward?
AMR integration in UHC should be undertaken optimistically but cautiously. While AMR sensitization of the implementers of UHS is important, primary objectives of UHC must not get diluted. This requires continuous dialogue and discussions at policy and programmatic level between senior managers of UHC and AMR for better understanding and coordination. A step-by-step approach is essential. UHC governance mechanism should have AMR national focal point on its highest decision-making and planning committee. At peripheral level also, a dedicated AMR person should be part of implementing mechanism to ensure efficient coordination, seamless integration and effective response. An approach suggested by Marie-Paul and Evan23 for implementation of UHC can also be utilized for integration of AMR in its framework. This approach calls for sustained funding, fair distribution of resources, motivated health workforce, quality services and efficient referral services in addition to strengthening primary health care and making all services accessible to everyone.
Challenges
UHC is health oriented. AMR is strongly influenced by significant use of antimicrobials in both animal health and agriculture sectors as well as the availability of these agents in various environments especially hospital and industrial effluents. Awareness among communities and local officials may catalyze implementation of a One Health Policy by bringing in other sectors within its ambit thus catalyzing a multisectoral approach and promoting a cascading effect.
Conclusions
AMR is not only a health issue. It has serious development dimensions and impact on poverty. AMR has the potential to augment extreme poverty. The efforts being made by the global community to eliminate extreme poverty (at $1.90/day) by 2030 is at serious risk if the problem of AMR is not tackled aggressively3.
Developing countries desire to contain AMR are facing several technical and management challenges24. Solutions that are workable at local level have to be identified and implemented. Several solutions are inbuilt into UHC and can be fine-tuned to generate AMR sensitive and AMR specific actions without creating a new resource-intensive structures. Implementation of UHC shall vary from country to country and hence the integration of AMR in UHC has to be tailor-made to be context specific. The burgeoning issue of AMR needs to be tackled utilizing available resources and strategies. The battle against AMR25 is long one but needs to be fought collectively and smartly through innovative collaborations, sustainability and efficient use of domestically available resources.
Footnotes
Financial support & sponsorship: None
Conflicts of Interest: None.
References
- 1.Geneva: WHO; 2016. [accessed on August 13, 2017]. World Health Organization. At UN, global leaders commit to act on antimicrobial resistance. Available from: http://www.who.int/mediacentre/news/releases/2016/commitment-antimicrobial-resistance/en/ [Google Scholar]
- 2.The Review on Antimicrobial Resistance. The Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Countries. 2014. [accessed on August 11, 2017]. Available from: https://www.amrreview.org/sites/default/files/160525_Final%20paper_with%20cover.pdf .
- 3.TheWorld Bank. By 2050, Drug-Resistant Infections could Cause Global Economic Damage on Par with 2008 Financial Crisis. 2016. [accessed on August 10, 2017]. Available from: http://www.worldbank.org/en/news/press-release/2016/09/18/by-2050-drug-resistant-infectionscould-cause-global-economic-damage-on-par-with-2008-financial-crisis .
- 4.World Health Organization. Antimicrobial resistance. Geneva: WHO; 2017. [accessed on September 17, 2017]. Available from: http://www.who.int/mediacentre/factsheets/fs194/en/ [Google Scholar]
- 5.Center for Disease Dynamics Economics and Policy. Resistance map. [accessed on June 20, 2016]. Available from: http://www.resistancemap.cddep.org/resmap/c/in/India .
- 6.Sethi S, Sharma D, Mehta SD, Singh B, Smriti M, Kumar B, et al. Emergence of ciprofloxacin resistant Neisseria gonorrhoeae in North India. Indian J Med Res. 2006;123:707–10. [PubMed] [Google Scholar]
- 7.Mehta A, Rosenthal VD, Mehta Y, Chakravarthy M, Todi SK, Sen N, et al. Device-associated nosocomial infection rates in intensive care units of seven Indian cities. Findings of the international nosocomial infection control consortium (INICC) J Hosp Infect. 2007;67:168–74. doi: 10.1016/j.jhin.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Taneja N, Samanta P, Mishra A, Sharma M. Emergence of tetracycline resistance in vibrio cholerae O1 biotype el tor serotype Ogawa from North India. Indian J Pathol Microbiol. 2010;53:865–6. doi: 10.4103/0377-4929.72014. [DOI] [PubMed] [Google Scholar]
- 9.Baris E, Irwin A, Thiebaud A, Evans TG. Containing Antimicrobial Resistance is a Smart Investment in Global Public Health and Wealth. AMR Control. 2017. [accessed on August 12, 2017]. Available from: http://www.resistancecontrol.info/2017/containingantimicrobial-resistance-is-a-smart-investment-in-globalpublic-health-and-wealth/
- 10.Sustainable Development Goals. 2016. [accessed on August 13, 2017]. Available from: https://www.sustainabledevelopment.un.org/post2015/transformingourworld,para26 .
- 11.United Nations General Assembly. Adopting Consensus Text, General Assembly Encourages Member States to Plan, Pursue Transition of National Health Care Systems towards Universal Coverage. 2012. [accessed on August 14, 2017]. Available from: https://www.un.org/press/en/2012/ga11326.doc.htm .
- 12.The World Bank. Universal Health Coverage. 2017. [accessed on August 10, 2017]. Available from: http://www.worldbank.org/en/topic/universalhealthcoverage .
- 13.Evans DB, Marten R, Etienne C. Universal health coverage is a development issue. Lancet. 2012;380:864–5. doi: 10.1016/S0140-6736(12)61483-4. [DOI] [PubMed] [Google Scholar]
- 14.Joint WHO/World Bank Group report, June 2015. Geneva: WHO; 2016. World Health Organization. Tracking universal health coverage: First global monitoring report. [Google Scholar]
- 15.World Health Organization. Health system country financing profile India, 2014. WHO global health observatory. Geneva: WHO; 2017. [Google Scholar]
- 16.National Health Portal. Universal health coverage. India: National Health Portal; 2017. [accessed on October 15, 2017]. Available from: https://www.nhp.gov.in/universal-health-coverage_pg . [Google Scholar]
- 17.World Health Organization. Worldwide country situation analysis: Response to antimicrobial resistance, 2015. Geneva: WHO; 2016. [Google Scholar]
- 18.Holloway KA. Promoting the rational use of antibiotics. Reg Health Forum. 2011;15:122–30. [Google Scholar]
- 19.Kalra A. India's universal healthcare rollout to cost $26 billion. Reuters. 2014. [accessed on July 3, 2017]. Available from: https://in.reuters.com/article/uk-india-health/indias-universal-healthcare-rolloutto-cost-26-billion-idINKBN0IJ0VN20141030 .
- 20.Loh LC, Ugarte-Gil C, Darko K. Private sector contributions and their effect on physician emigration in the developing world. Bull World Health Organ. 2013;91:227–33. doi: 10.2471/BLT.12.110791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakraborty D. The Private Sector's Role in Achieving Universal Health Coverage in India. Geneva Network. 2015. [accessed on August 19, 2017]. Available from: https://www.geneva-network.com/wpcontent/uploads/2015/06/private_sector_s_role__briefing.pdf .
- 22.World Health Organization. Universal health coverage data portal. Geneva: WHO; 2016. [Google Scholar]
- 23.Marie-Paul K, Evan DB. Universal health coverage. East Mediterr Health J. 2013;19:305–6. [PubMed] [Google Scholar]
- 24.Bhatia R, Walia K. Combating antimicrobial resistance in India: Technical challenges & opportunities. Indian J Med Res. 2017;146:683–7. doi: 10.4103/ijmr.IJMR_19_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhatia R, Narain JP. The growing challenge of antimicrobial resistance in the South-East Asia region - Are we losing the battle? Indian J Med Res. 2010;132:482–6. doi: 10.4103/0971-5916.73313. [DOI] [PMC free article] [PubMed] [Google Scholar]