Abstract
OBJECTIVE:
To evaluate the efficacy and safety of acupuncture therapy for children with cerebral palsy.
DATA SOURCES:
We conducted electronic searches of PUBMED (1950/2017), EMBASE (1974/2017), ScienceDirect (1986/2017), Academic Source Premier (1887/2017), the Cochrane Library (Issue 4, April 2017), Science Citation Index Expanded (1900/2017), China National Knowledge Infrastructure (1915/2017), China Biological Medicine (1990/2017-04), WanFang (1980/2017), VIP (1989/2017), and Chinese Science Citation Database (1989/2017).
DATA SELECTION:
We included randomized controlled trials that aimed to compare the effect of acupuncture plus rehabilitation training versus rehabilitation training alone. Data about functional motor abilities, daily activity/social participation, effective rate, intellectual development, and adverse effects were included. We used Revman 5.2 software for statistical analysis.
OUTCOME MEASURES:
The primary outcomes included functional motor abilities, daily activity, and effective rate. The secondary outcomes included intellectual development and adverse effects.
RESULTS:
Twenty-one studies with a total of 1718 participants met the inclusion criteria. The effect size of gross motor function (SMD = 0.64, 95% CI: 0.52 to 0.76, P < 0.00001; I2 = 0%, P = 0.69; in 13 studies with 1144 patients) and the total effective rate (RR = 1.28, 95% CI: 1.20 to 1.37, P < 0.00001; I2 = 18%, P = 0.27; in 12 studies with 1106 patients) suggested that acupuncture plus rehabilitation produced a significant improvement in gross motor function and a high total effective rate. The pooled fine motor function (SMD = 3.48, 95% CI: 2.62 to 4.34, P < 0.00001; I2 = 64%, P = 0.10; in 2 studies with 193 patients), modified Ashworth scale scores (SMD = –0.31, 95% CI: –0.52 to –0.11, P = 0.003; I2 = 74%, P = 0.004; in 5 studies with 363 patients) and activities of daily living (SMD = 1.45, 95% CI: 1.20 to 1.71, P < 0.00001; I2 = 78%, P = 0.004; in 4 studies with 313 patients) also indicated improvements in children with cerebral palsy. Publication bias was not observed. Only mild adverse events related to acupuncture were reported.
CONCLUSION:
Acupuncture plus rehabilitation training improved gross motor function, reduced muscle spasms, and enhanced daily life activities in children with cerebral palsy. However, this conclusion should be interpreted with caution due to the small number of randomized controlled trials available and the small sample sizes. More high-quality and large-scale studies are needed.
Keywords: nerve regeneration, acupuncture, rehabilitation, children, efficacy, safety, cerebral palsy, meta-analysis, randomized controlled trials, neural regeneration
Introduction
Cerebral palsy refers to a group of motor conditions that affect movement and coordination. Cerebral palsy is a life-long condition attributed to a non-progressive disturbance that occurs in the developing fetal or infant brain. The disorder can occur at any time during pregnancy, delivery, or the first 3 to 5 years of age (Morris, 2002). Cerebral palsy results from brain malformation that arises early in life and subsequently interferes with normal motor development (Verma et al., 2012). Cerebral palsy may be accompanied by disturbances in sensation, cognition, communication, perception, and behavior, as well as seizure disorder (Bax et al., 2005). Some risk factors associated with the incidence of cerebral palsy include low birth weight, premature birth, multiple births, asphyxia (lack of oxygen), infection, and cerebral bleeding (Odding et al., 2006; Pountney, 2013; Lou et al., 2016). Other possible causes include severe neonatal illness, non-accidental injury, vehicle accidents, meningitis, encephalitis, near drowning, and cardiopulmonary arrest (Hull and Johnston, 1999). Cerebral palsy may be formally diagnosed and classified following a complete history and neurological examination. Severity is variable depending on the affected limbs and the degree of movement impairment. Spastic cerebral palsy is characterized by a combination of tight, stiff, and weak muscles, making control of movement difficult. It is the most common type of cerebral palsy, accounting for 70% of affected children (Hull and Johnston, 1999; Pountney, 2013). It can be further subcategorized into diplegia, characterized primarily by involvement of the lower limbs; quadriplegia, in which all four limbs are affected; and hemiplegia, in which the limbs on one side of the body are affected. Dyskinetic, ataxic, and hypotonic cerebral palsy are known as extrapyramidal forms of cerebral palsy and account for the remaining 30% of cases (Hull and Johnston, 1999). Dyskinetic cerebral palsy is characterized by impaired ability to control movement. It can be subcategorized into a) dystonia (athetosis), which involves sustained muscle contractions associated with twisting or repetitive movements; b) rigidity, which refers to increased tone and co-contraction; c) chorea, which is characterized by jerky, irregular, and rapid involuntary movement; d) ataxia, which is characterized by abnormal balance and coordination; and e) hypotonia, which refers to a decrease in muscle tone (Rosenbaum et al., 2007; Pakula et al., 2009). Many children also have mixed-type cerebral palsy, which can be both spastic and non-spastic (Hull and Johnston, 1999). The incidence of cerebral palsy is approximately 2–2.6 per 1000 live births, making it the most common physical disability in childhood (Stanley and Watson, 1992; Hagberg et al., 1996; Pharoah and Cooke, 1996; Colver et al., 2000; Graham, 2001, 2002; Duncan et al., 2004). This rate has remained stable for the last 60 years despite technological advances in medical interventions (Blair and Watson, 2006). A study conducted in six Chinese provinces revealed that the prevalence of children with cerebral palsy (aged from 1 to 6 years) was approximately 1.92/1000 from May 1997 to December 1998 (Li et al., 2001). Because there is no cure, children with cerebral palsy and their families seek multiple forms of therapy, particularly those that have the potential to improve the way in which the children function or feel (Liptak, 2005). Various therapies have been found to improve activities of daily living (ADL). These include physical therapy and occupational therapy, as well as speech and language therapy (Pennington et al., 2004; Steultjens et al., 2004). Surgical approaches for treatment of spastic cerebral palsy also exist, these include orthopedic surgery (Lin and Li, 2000) and selective posterior rhizotomy (cutting of a spinal nerve root) (Wang et al., 2000). Acupuncture-centered rehabilitation as part of a unified treatment plan including conventional therapies has been proposed as an appropriate strategy for overcoming disability associated with cerebral palsy. This remains the main method practiced in both top-grade hospitals and national research institutes in China (Liao et al., 2017). Acupuncture therapy, which is a relatively simple, inexpensive, and safe treatment compared with other conventional interventions, has been found to improve motor activity, sensation, speech, and other neurological functions in children with cerebral palsy (Zhang et al., 2005). Acupuncture incorporates many specific techniques. Classical acupuncture involves the insertion of needles into specific locations in the skin. The target sites have been empirically defined over thousands of years. Auricular acupuncture involves the insertion of tiny seeds into predetermined points on the outer ear. In children, the target sites are associated with various pediatric diseases (Graff and McDonald, 2016). Chinese scalp acupuncture is another microsystem technique in which the acupuncture needle is inserted into various areas of the scalp. Specific manipulations of the needle are conducted to regulate and strengthen various functional activities of the brain and body. Tongue acupuncture is also commonly used as a treatment for cerebral palsy. One study reported that the physiological effect of tongue acupuncture might result from the modification of neural signaling in the motor/somatosensory cortex, resulting in improved motor function (Sun et al., 2004). Preliminary reports have suggested that acupuncture can increase the supply of blood and oxygen to blood vessels, and that acupuncture may repair, activate, and regenerate injured neurons in the brain (Wang and Wu, 2005). Modern neuroimaging methods (magnetic resonance imaging) confirmed the activation of subcortical and cortical centers after acupuncture (Wu et al., 2008) and confirmed the ability of acupuncture to increase cerebral blood flow and cerebral oxygen supply in children with cerebral palsy. The above studies provide clinical support for acupuncture treatment in individuals with cerebral palsy. However, further investigation is necessary. Benefits attributed to acupuncture have included warmer extremities (Svedberg et al., 2001), a decrease in painful spasms (Sanner and Sundequist, 1981; Svedberg et al., 2003), improved use of arms (Huang, 2005) or legs, more restful sleep, increased mood, improved bowel function (Duncan et al., 2004), and heightened bone density. Several systematic reviews have shown acupuncture to be clinically effective in children with cerebral palsy (Yang et al., 2015), while others have reported conflicting viewpoints (Mu et al., 2012). Therefore, an evidence-based assessment of the efficacy and safety of acupuncture in children with cerebral palsy is still needed. Here, we systematically reviewed all available randomized controlled trials (RCTs) of acupuncture in children with cerebral palsy.
Data and Methods
Search strategies
Electronic search
We searched six English databases (PUBMED, EMBASE, ScienceDirect, Academic Source Premier, the Cochrane Library, and Science Citation Index Expanded) and five Chinese databases (China National Knowledge Infrastructure, China Biological Medicine, WanFang, VIP, and Chinese Science Citation Database) for articles with any publication status from inception to April 26, 2017. We used the following English terms: “cerebral palsy” OR “brain paralysis” OR “cerebral paralysis” OR “spastic cerebral palsy” OR “athetoid cerebral palsy” OR “ataxic cerebral palsy” OR “mixed cerebral palsy” OR “spastic diplegia” OR “little disease” OR “congenital cerebral palsy” OR “dystonic-rigid cerebral palsy” OR “monoplegic infantile cerebral palsy” OR “quadriplegic infantile cerebral palsy” AND “acupuncture” OR “acupuncture therapy” OR “acupuncture treatment” OR “electroacupuncture” OR “electro-acupuncture” OR “acupuncture, ear” OR “ear acupuncture” OR “auriculotherapy” OR “scalp acupuncture” AND “randomized controlled trial” OR “controlled clinical trial” OR “randomized” OR “clinical trial” OR “randomly” OR “RCT” OR “trial”. The Chinese search terms (China National Knowledge Infrastructure) were: (TI = Naotan + Xiaoernaotan + Naoxingtanhuan + Ertongnaotan + Xiaoernaoxingtanhuan + Jingluanxingnaotan) AND (TI = Zhenjiu + Zhenjiufa + Zhenjiufangfa + Zhenjiuzhiliao + Zhenjiuliaofa + Zhencifa + Zhencizhiliao + Zhenciliaofa + Dianzhen + Dianzhenjiu + Touzhen + Toupizhen + Touzhenliaofa + Tizhen + Erzhen + Erzhenliaofa + Erzhenzhiliao + Dianerzhen) AND (AB = Suijiduizhaolinchuangshiyan + Suijishuangmangduizhaoshiyan + Suijiduizhaoshiyansheji + Suijishuangmangshuangmoniduizhaoshiyan + Suijiduizhaoyanjiu + Suijiduizhao + Suijiduizhaolinchuangyanjiu + Suijiduizhaozhiliao + Suijishuangmangduizhao + Duizhaolinchuangshiyan + Duizhaoshiyan).
Manual search
We manually searched the reference lists of the identified studies and reviews for additional references (from inception to April 2016). Authors of papers on the efficacy of acupuncture in cerebral palsy patients were contacted by email or telephone to request any additional published or unpublished studies relevant to our review. We asked the authors of abstracts of potentially eligible studies for full written reports.
Inclusion and exclusion criteria
Two of the authors (LXL, JH) independently checked the titles and abstracts of the trials identified by the search for inclusion in our review based on the selection criteria outlined above. The full text of an article was retrieved if there was any doubt as to whether the article should be excluded. In cases of disagreement between the two review authors, author (MMZ) reviewed the information to decide whether the trial should be included. If articles were written by the same authors or the same researchers were identified, we retained the latest or the most informative study.
Study types
We included both published and unpublished RCTs. Acupuncture was compared with a placebo (sham acupuncture), no treatment, modern rehabilitation, and western medicine. Baseline data were used to compare the two groups in terms of age, duration, and type of cerebral palsy as reported by the eligible studies. We included studies regardless of blinding, language, or publication status. We excluded studies that used quasi-randomization techniques where allocation of patients was conducted via alternation, case record numbers, date of birth, or day of the week, and excluded controlled trials that used any other non-randomized allocation methods. RCTs that did not clearly describe the generation of the random allocation sequence were excluded.
Participant characteristics
Inclusion criteria: Trials that included children 6 months to 14 years of age of either gender with cerebral palsy of any type (spastic cerebral palsy, athetoid cerebral palsy, ataxic cerebral palsy, and mixed cerebral palsy with non-progressive cerebral disease/defect). Ideally, cerebral palsy was diagnosed based on symptoms, physical signs, and case histories (Lin and Li, 2000; Lin, 2005).
Exclusion criteria: Trials that included children with cerebral palsy who had severe skin infections; heart, lung, liver, or kidney disease; or central paralysis due to viral encephalitis or tuberculo-encephalitis.
Intervention types
Studies evaluating the following forms of acupuncture therapy were included regardless of the number of treatments or the length of the treatment period: acupressure, laser acupuncture, and electroacupuncture based on meridians or channel theory related to acupoints (acupuncture points or any specific sites of needle insertion related to acupuncture). We included studies that examined traditional acupuncture using classical meridian points and contemporary acupuncture using non-meridian or trigger points regardless of the method of stimulation (hand, needle, laser, or electrical stimulation), although we excluded studies concerning acupoint injection and catgut embedding. Acupuncture could be given alone or in addition to conventional treatment. The control interventions included placebo or sham acupuncture, no treatment, or conventional treatment. Placebo acupuncture refers to the use of needles that are placed on the skin surface (at the correct acupoints) but do not penetrate the skin (Furlan et al., 2005). Sham acupuncture refers to the use of needles positioned close but not inside the acupoints (Furlan et al., 2005) or subliminal skin electrostimulation via electrodes attached to the skin (Johansson et al., 2001). Conventional treatment included modern rehabilitation, such as physical therapy, occupational therapy, speech and language therapy, and western medicine. We assessed studies that made the following treatment comparisons: (1) acupuncture alone compared with placebo or sham acupuncture, (2) acupuncture plus conventional treatment compared with placebo or sham acupuncture plus conventional treatment, and (3) acupuncture plus conventional treatment compared with conventional treatment alone. Studies that compared only different forms (different manipulation methods or different acupoints) of acupuncture were excluded.
Quality assessment of studies
We assessed risk of bias as described in the updated Cochrane Reviewers’ Handbook version 5.0 (Higgins and Green, 2008), which included the following criteria:
-
(1)
Sequence generation: Was the allocation sequence adequately generated?
-
(2)
Allocation concealment: Was allocation adequately concealed?
-
(3)
Blinding of participants, personal and outcome assessors: Was knowledge of allocated interventions adequately prevented during the study?
-
(4)
Incomplete outcome data: Were incomplete outcome data adequately addressed?
-
(5)
Selective outcome reporting: Were reports of the study free of suggestion of selective outcome reporting?
-
(6)
Other potential threats to validity: Was the study apparently free of other problems that could put it at a risk of bias?
In all cases, an answer of “Yes” indicated a low risk of bias, an answer of “No” indicated a high risk of bias, and an answer of “Unclear” indicated an uncertain risk of bias. The judgment criteria were as follows: A) “good” quality corresponded to four or more items indicating a low risk of bias (labeled “Yes”), B) “moderate” quality corresponded to two or three items indicating a low risk of bias, and C) “poor” quality corresponded to only one or no items indicating a low risk of bias or one or more items indicating a high risk of bias (labeled “No”). Quality assessment was performed by two independent review authors (LXL, JH), and any disagreement was reported and resolved by a third author (MMZ).
Outcome measures
Primary outcomes
-
Functional motor abilities (1) Gross motor function (GMF): For assessment of the key function of ambulation (lower extremities) with a Gross Motor Function Measure, the Gross Motor Function Classification System described by Bax et al. (2005)) or other assessment criteria, including the Functional Independence Measure, Berg balance scale, and Holden Walking Functional Classification, were reported in the original studies.
(2) Fine motor function: For assessment of upper extremity function, the Bimanual Fine Motor Function and Manual Ability Classification System described by Bax et al. (2005) or other assessment criteria were reported in the original studies.
(3) Overall motor function: To assess both lower and upper extremities together, we assessed the authors’ reported methods. These included comparisons using a modified Ashworth scale (MAS) and effective rates for overall motor function, which can be categorized into three grades according to the clinical symptoms and signs of cerebral palsy: 1) markedly effective, indicating a normal state in terms of functional motor ability and muscle recovery; 2) effective, indicating improvement in functional motor ability; and 3) no effect, indicating that symptoms were unchanged after treatment according to the assessment criteria reported in the original study.
-
Daily activity/social participation
This outcome could be measured by the ADL scale or another scale reported in the original studies.
Effective rate
Secondary outcomes
Intellectual development (Gessell measurement for child development).
Adverse effects including dizziness, difficulty tolerating electrostimulation, infection, punctured lung, cardiac tamponade, and spinal cord injury, which were presumed to be caused by acupuncture or electrostimulation.
Statistical analysis
Two review authors (LXL and JH) independently extracted information on the patients, methods, interventions, outcomes, and results of the studies using a data extraction form developed for this purpose. Disagreements were resolved by the author (MMZ) or through discussion. For dichotomous outcomes, we extracted the number of participants who experienced the event and the total number of participants in each arm of the trial. For continuous outcomes, we extracted the mean change and standard deviation in each arm of the trial, along with the total number of participants in each group.
Measures of treatment effect
We calculated risk ratios (RRs) with 95% confidence intervals (CIs) for the effective percentages and efficacy rates, and standardized mean differences (SMDs) with 95% CIs for the scores obtained using different impairment scales.
Unit of analysis issues
We only included RCTs in which the participants were individually randomized in the clinical trials.
Dealing with missing data
We did not include trials in which the authors reported conducting an intention-to-treat analysis.
Assessment of heterogeneity
Investigation of heterogeneity: We assessed clinical heterogeneity by examining differences in the distribution of important participant and intervention factors between studies (age, gender, specific diagnosis/diagnostic subtypes, duration of disorder, associated diseases, and treatment type) and assessed methodological heterogeneity according to factors including randomization, concealment, blinding, losses to follow-up, and co-interventions. We assessed statistical heterogeneity by examining I2 (Higgins and Thompson, 2002), a statistic that describes the approximate proportion of variation in a point estimate that is due to heterogeneity rather than sampling error. In addition, we used the chi-square test of homogeneity to determine the strength of the evidence indicating true heterogeneity.
Assessment of reporting bias
We assessed possible publication bias by visually assessing the symmetry of the funnel plots.
Data synthesis
The RRs with 95% CIs were used for binary outcomes as appropriate. SMDs with 95% CIs were used for continuous outcomes. If different measures (scales) for the same outcome were used in different studies, the mean difference (MD) was used across trials. All analyses included all participants in the treatment groups to which they were allocated.
Subgroup analysis and investigation of heterogeneity
We did not conduct a subgroup analysis because the information regarding the patients and the interventions was difficult to divide into subgroups.
Sensitivity analysis
We conducted a sensitivity analysis to investigate whether the findings of the present meta-analysis were robust. Specifically, we selected different models and omitted individual studies.
Results
Search results
Initial electronic and manual searches identified 735 references published up until April 26, 2017. After reviewing the titles and abstracts, 637 studies were excluded because they were duplicates, were laboratory or animal studies, or had a study objective that was not relevant to this review. A total of 98 full-text references were retrieved for further, more careful assessment. Ultimately, 21 studies (Jia, 2003; Sun et al., 2004; Ji et al., 2008; Li et al., 2009; Zhou et al., 2010; Wang et al., 2011; Deng and Xiong, 2012; Duncan et al., 2012; Zhang and Hu, 2012; Zhao and Yan, 2012; Liu et al., 2013; Zhang and Du, 2013; Zhu and Yuan, 2013; Li et al., 2014; Liang, 2014; Zhang et al., 2014; Dabbous et al., 2016; Du et al., 2016; Shi et al., 2016; Yang and Hou, 2016; Zhao et al., 2017) with a total of 1718 participants were included in this review, as shown in the search flowchart (Figure 1).
Figure 1.
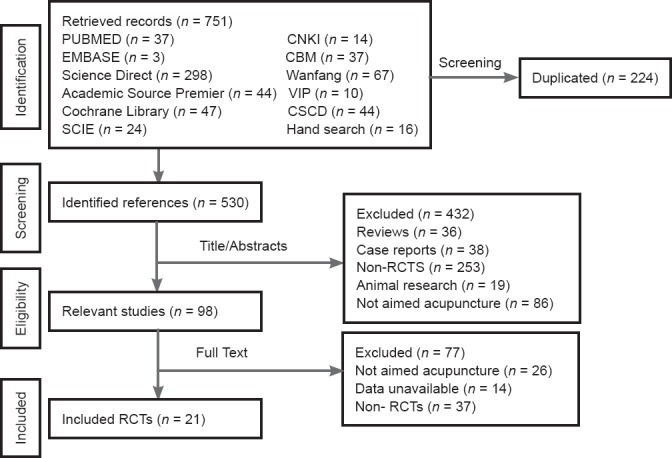
Flow chart of study search protocol.
CNKI: China National Knowledge Infrastructure; CBM: China Biological Medicine; CSCD: Chinese Science Citation Database; SCIE: Science Citation Index Expanded; RCTs: randomized controlled trials.
Description of the included studies
Design
All of the included studies were RCTs in which the generation methods of the randomized allocation sequence were clearly reported. Twenty studies reported two parallel treatment arms, while one was designed as a three-arm controlled trial in which the data from the controlled group treated with acupuncture alone were not extracted. One study was conducted in Egypt, and the rest were conducted in China. Five studies (Sun et al., 2004; Duncan et al., 2012; Zhang and Hu, 2012; Liu et al., 2013; Dabbous et al., 2016) were published in English, and the rest were published in Chinese. The research period varied from 9 months to 3 years.
Participants and setting
A total of 1718 participants were included in the 21 studies. All trials randomized participants with cerebral palsy into treatment groups. All participants were Chinese except those in one study (Dabbous et al., 2016), including outpatients and inpatients. All studies included children with various clinical subtypes of cerebral palsy. Three studies (Zhou et al., 2010; Wang et al., 2011; Zhang and Hu, 2012) reported the severity of the disease, and four (Jia, 2003; Zhang and Hu, 2012; Zhang et al., 2014; Zhao et al., 2017) reported the duration of the disease. The participant age ranged from 6 (mean) months to 10.68 ± 3.13 (mean ± standard deviation) years.
Diagnosis
The diagnostic criteria for cerebral palsy differed between the studies. One study (Duncan et al., 2012) used the five Gross Motor Function Classification System severity levels, and two pediatric neurologists diagnosed cerebral palsy. Three studies (Jia, 2003; Sun et al., 2004; Dabbous et al., 2016) did not mention the criteria used. The remaining studies were based on the Chinese national clinical diagnostic criteria and classification criteria.
Interventions
Acupuncture was used in all the included studies as an intervention treatment. One study (Sun et al., 2004) used acupuncture as an intervention versus sham acupuncture, and the other 20 studies used acupuncture combined with modern rehabilitation training as an intervention versus modern rehabilitation training alone. All of the included studies used traditional acupuncture points, and none used the contemporary non-meridian or trigger points. In terms of acupuncture treatment, we observed substantial diversity in the acupuncture protocol among the included studies. Specifically, the acupuncture points, depth and direction of insertion, retention time of needles, and duration of acupuncture sessions varied. The acupuncture rationale, practitioner background, needle type, and responses elicited were also not described. One study (Zhang and Hu, 2012) reported a 12-month follow-up.
Outcomes
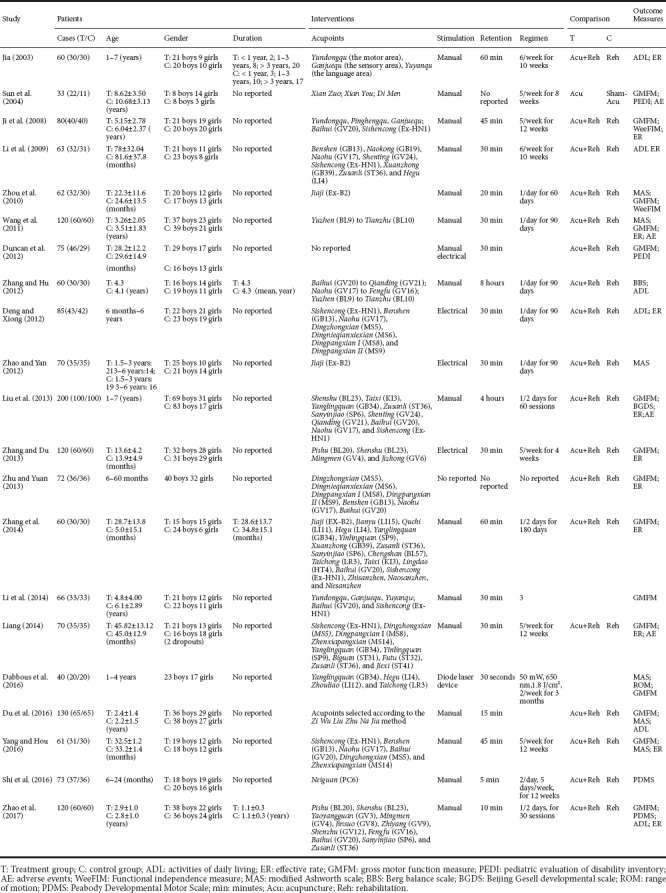
The outcomes of the enrolled studies included the Gross Motor Function Measure (Sun et al., 2004; Ji et al., 2008; Zhou et al., 2010; Wang et al., 2011; Duncan et al., 2012; Liu et al., 2013; Zhang and Du, 2013; Zhu and Yuan, 2013; Li et al., 2014; Liang, 2014; Zhang et al., 2014; Dabbous et al., 2016; Du et al., 2016; Yang and Hou, 2016; Zhao et al., 2017), Functional Independence Measure (Ji et al., 2008; Zhou et al., 2010), Peabody Developmental Motor Scale (Shi et al., 2016; Zhao et al., 2017), Berg balance scale (Zhang and Hu, 2012), MAS (Zhou et al., 2010; Wang et al., 2011; Zhao and Yan, 2012; Dabbous et al., 2016; Du et al., 2016; Yang and Hou, 2016), pediatric evaluation of disability inventory (Sun et al., 2004; Duncan et al., 2012), Beijing Gesell Developmental Scale (Liu et al., 2013), range of motion test (Dabbous et al., 2016), ADL (Jia, 2003; Li et al., 2009; Deng and Xiong, 2012; Zhang and Hu, 2012; Du et al., 2016; Zhao et al., 2017), and rate of efficacy (Jia, 2003; Ji et al., 2008; Li et al., 2009; Wang et al., 2011; Deng and Xiong, 2012; Liu et al., 2013; Zhang and Du, 2013; Zhu and Yuan, 2013; Liang, 2014; Zhang et al., 2014; Yang and Hou, 2016; Zhao et al., 2017). Some of the data from the original literature were not available. A full description of the studies is given in Table 1.
Table 1.
Characteristics of the included studies
Risk of bias in the included studies
Two reviewers (LXL and JH) independently assessed the quality of the methodology of the extracted studies. In accordance with the Cochrane risk-of-bias tool and the previous judgment criteria, the results of the methodological quality assessment of the included studies indicated that most of them were of relatively low quality. Only three studies (Sun et al., 2004; Wang et al., 2011; Duncan et al., 2012) were evaluated as grade A, and the rest of the included studies were evaluated as grade B, indicating that all the included trials were deemed to have a median or high risk of bias. No studies reported that the outcomes were analyzed following intention-to-treat principles. The quality assessment is summarized in the “Risk of bias graph” (Figure 2) and the “Risk of bias summary” (Figure 3).
Figure 2.
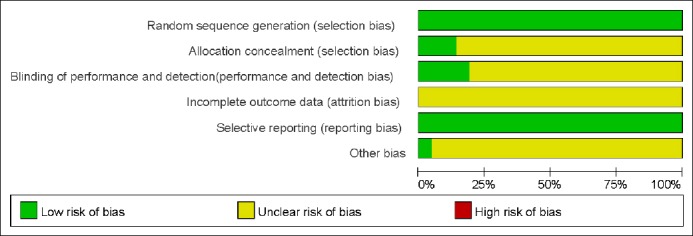
Risk of bias of the included studies.
Figure 3.
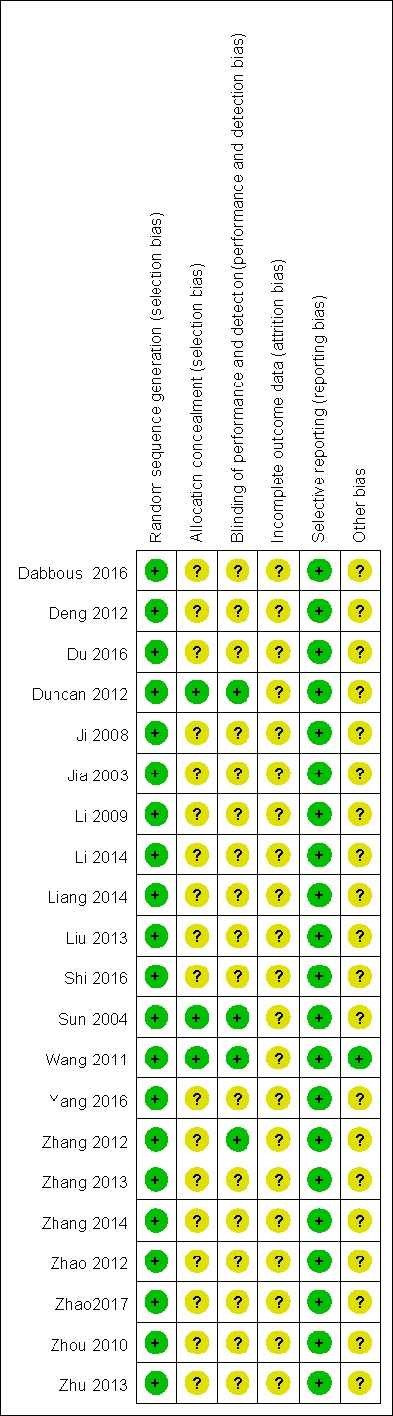
Risk of bias risk of the included studies.
Meta-analysis results
We performed a meta-analysis of GMF, muscular tone, daily activity abilities, and total efficacy. We did not conduct a pooled analysis to assess FMF, intellectual development, or adverse effects, because the data in the original studies were insufficient. Similarly, we did not conduct subgroup analysis because the number of included studies was small and the extracted data in each group was insufficient.
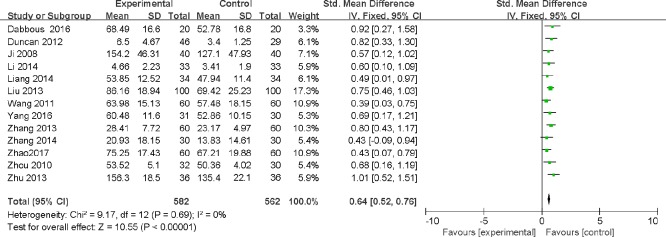
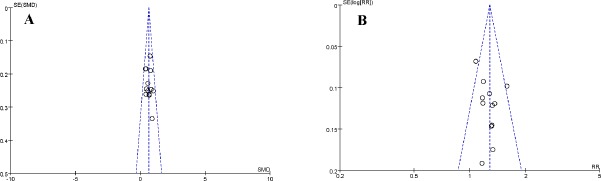
GMF
The pooled analysis of GMF was based on 15 studies that included 1272 children with cerebral palsy. Gross Motor Function Measure data were available in 15 studies (Sun et al., 2004; Ji et al., 2008; Zhou et al., 2010; Wang et al., 2011; Duncan et al., 2012; Liu et al., 2013; Zhang and Du, 2013; Zhu and Yuan, 2013; Li et al., 2014; Liang, 2014; Zhang et al., 2014; Dabbous et al., 2016; Du et al., 2016; Yang and Hou, 2016; Zhao et al., 2017). These data were extracted to perform the meta-analysis. The pooled SMDs and 95% CIs of these 15 studies were estimated with a random effects model (SMD = 0.88, 95% CI: 0.58 to 1.17, n = 15; P < 0.00001), but we observed significant heterogeneity among these studies with respect to GMF (I2 = 84%, P < 0.00001; Table 2). After excluding two studies (Sun et al., 2004; Du et al., 2016) that contributed most strongly to the heterogeneity, as verified visually by a sensitivity analysis, the significant heterogeneity disappeared (I2 = 0%, P = 0.69; Table 2). We then conducted a pooled analysis (13 studies with 1144 patients) with a fixed effects model (SMD = 0.64, 95% CI: 0.52 to 0.76, n = 13, P < 0.00001). The results suggested that the acupuncture intervention yielded improved GMF in children with cerebral palsy, as shown in the forest plot (Figure 4). No evidence of publication bias was found in the funnel plot analysis (Figure 5A). In the meta-analysis of the two excluded studies, the pooled effect sizes (SMD = 2.61, 95% CI: 2.19 to 3.04, n = 2, P < 0.00001; I2 = 0%, P = 0.034; Table 2) also showed a positive improvement in GMF.
Table 2.
Meta-analysis of the included studies for GMF, FMF, MAS, ADL, and ER
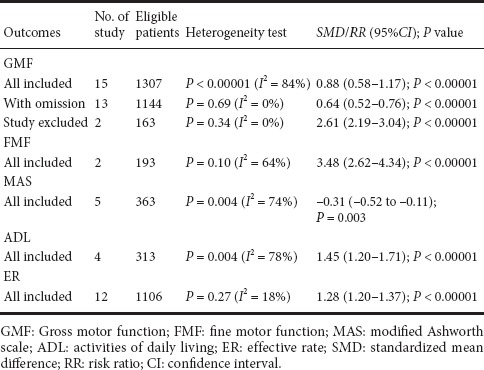
Figure 4.
Forest plot for gross motor function.
Figure 5.
Funnel plot for gross motor function and effective rate.
(A) Funnel plot analysis; (B) pooled analysis.
FMF
The FMF data were extracted from two studies (Shi et al., 2016; Zhao et al., 2017). The pooled effects sizes (SMD = 3.48, 95% CI: 2.62 to 4.34; I2 = 64%, n = 2, P < 0.00001; Table 2) showed that FMF was improved in the treatment group.
MAS ratings
We extracted MAS data, which were available for five studies (Zhou et al., 2010; Zhao and Yan, 2012; Dabbous et al., 2016; Du et al., 2016; Yang and Hou, 2016), to conduct the meta-analysis. The pooled estimated sizes (SMD –0.31, 95% CI: –0.52 to –0.11; I2 = 74%, n = 5, P = 0.003; Table 2) showed that the MAS rating in the trial group was significantly lower than that in the control group.
Four studies (Jia, 2003; Li et al., 2009; Zhang and Hu, 2012; Du et al., 2016) reported ADL results, and the meta-analysis showed that the daily activity abilities of the children in the trial group significantly improved (SMD = 1.45, 95 %CI: 1.20 to 1.71; I2 = 78%, n = 4, P < 0.00001; Table 2).
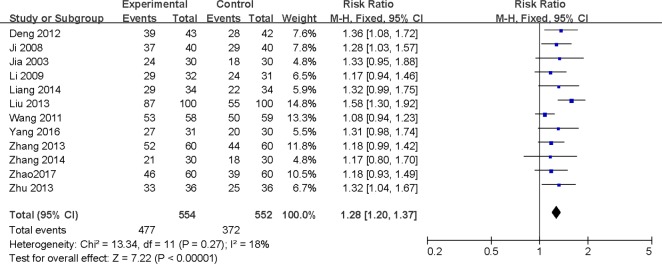
Effective rate
The efficacy data were extracted from 12 studies (Jia, 2003; Ji et al., 2008; Li et al., 2009; Wang et al., 2011; Deng and Xiong, 2012; Liu et al., 2013; Zhang and Du, 2013; Zhu and Yuan, 2013; Liang, 2014; Zhang et al., 2014; Yang and Hou, 2016; Zhao et al., 2017). The pooled RR and 95% CI values of these 12 studies were estimated with a fixed effect model (RR = 1.28, 95% CI: 1.20 to 1.37), and significant heterogeneity was not observed (I2 = 18%, n = 12, P = 0.27; Table 2). The results suggested that the total efficacy rate in the acupuncture group was higher than that of the control group (see forest plot in Figure 6). We found no evidence of publication bias in the pooled analysis (Figure 5B).
Figure 6.
Forest plot for effective rate.
Adverse events
Data concerning adverse events were collected in three studies, and were not mentioned in other studies. One study (Sun et al., 2004) reported that crying and minor pain occurred in the first few sessions due to fear, but most children adapted and became more compliant in later sessions. The other two studies (Duncan et al., 2012; Zhang and Hu, 2012) reported no adverse events related to acupuncture. Above all, none of the included studies suggested that there were any serious adverse events. Although some side effects were reported, including pain, infections, and inappropriate needle placement, which inadvertently caused harm to the patient (Dabbous et al., 2016), most of the existing studies on acupuncture in patients with cerebral palsy and patients with other clinical conditions have supported acupuncture as a safe treatment modality compared with the safety of western medicine.
Discussion
Acupuncture has been and continues to be widely used in China to treat children with cerebral palsy, and several studies claiming to be RCTs have been published. We performed the present systematic review and meta-analysis to assess the efficacy and safety of acupuncture in children with cerebral palsy as a complementary therapy to modern western medicine.
Main results and evidence
Twenty-one studies including 1718 children with cerebral palsy were included in the meta-analysis. The pooled effect size showed positive results for improvements in GMF (SMD = 0.64, 95% CI: 0.52 to 0.76, n = 13), FMF (SMD = 3.48, 95% CI: 2.62 to 4.34, n = 2), MAS (SMD = –0.31, 95% CI: –0.52 to –0.11, n = 5), ADL (SMD = 1.45, 95% CI: 1.20 to 1.71, n = 4), and total effective rate (RR = 1.28, 95% CI: 1.20 to 1.37, n = 12). No serious adverse events related to acupuncture were confirmed. The present meta-analysis supports acupuncture for children with cerebral palsy as a potentially beneficial alternative and complementary therapy in the domain of modern western medicine.
Limitations
Based on the above results, the heterogeneous acupuncture protocol and outcome measures varied across the included studies. Thus, the findings of this review should be interpreted in consideration of several limitations. First, the number of well-designed RCTs was small. Only 21 trials met the inclusion criteria and the outcome measures related to meta-analysis were extracted from a small number of trials (FMF data in two studies, MAS data in five studies, and ADL data in four studies). Thus, we did not analyze heterogeneity and subgroups for FMF, MAS, and ADL. Second, the sample size of the enrolled studies was small. The number of participants ranged from 33 to 200 in the included studies (mean = 82 participants per study). Statistical type I or type II errors can occur even when statistically significant differences are found. Therefore, the conclusions of this study should be interpreted with caution. Third, most of the studies were of poor methodological quality or the protocols were not adequately reported. The standard of reporting of the included studies did not fully comply with the Consolidated Standards of Reporting Trials (CONSORT) statement (Cheuk et al., 2007) or the reporting guidelines of the Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) criteria (MacPherson et al., 2002; Moher et al., 2003). Only one study (Wang et al., 2011) reported the method of sequence generation and allocation concealment. Interestingly this study had a high withdrawal rate (Wang et al., 2011), with 24 participants (20.9%) withdrawing before completing the protocol and 16 participants not completing the evaluations. Hence, the present data might suffer from bias due to study design and selective reporting.
-
1)
There was a significant heterogeneity in the acupuncture treatment protocol between the included studies. For example, the time for needle retention during acupuncture was from no needle retention to 4 hours, and the frequency of acupuncture was from once per day to 2–3 times per week. The duration of acupuncture treatment ranged from 1 to 3 months. This heterogeneity may limit the popularization and application of acupuncture therapy in practice.
-
2)
Most of the studies were conducted by Chinese researchers. Only one study (Dabbous et al., 2016) was conducted by non-Chinese researchers. This may be related to the fact that acupuncture treatment originates from China.
-
3)
All patients enrolled in the study were either inpatients or outpatients. The randomization method was a random number table or random sequence generated by computer software, which ensured that all the studies included were rigorously designed randomized controlled trials.
Implications for practice
This meta-analysis represents updated evidence in support of acupuncture combined with rehabilitation training for the improvement of GMF and total therapeutic efficacy. The data are not sufficient to demonstrate whether acupuncture is effective in improving FMF, reducing muscle spasms, or improving ADL (due to the small number of studies available). Recommendations for practice should be made with caution due to the small number of included RCTs, small sample sizes, and relatively poor methodological quality.
Implications for further research
Further RCTs are required to evaluate the efficacy of acupuncture in the treatment of children with cerebral palsy. Although blinding of acupuncturists is difficult, greater attention should be paid to methodological design, including randomization and blinding of patients, other treatment providers, and outcome assessors, to minimize performance and assessment bias. Future studies will benefit from increased reporting and better study design.
Conclusions
The findings of this meta-analysis of currently available studies indicated that acupuncture combined with rehabilitation training is an effective therapy for improving GMF, FMF, MAS, ADL, and the total rate of treatment efficacy in children with cerebral palsy. Thus, acupuncture may have benefits in both practical and research settings as an alternative and complementary therapy. Although our results should be interpreted with caution due to the limitations of this study, clinicians may consider acupuncture in combination with rehabilitation training for treatment of children with cerebral palsy. Further large-scale, standardized clinical trials are required.
Additional file (3.2KB, pdf) : Open peer review report 1.
Acknowledgments
We thank the Cochrane Developing Countries Network for the English editing and Ema Rogue in the Cochrane movement disorder group for searching for trials. We thank Professor Alan Bensoussan from the University of Western Sydney for giving us valuable suggestions and comments.
Footnotes
Conflicts of interest: The authors declare that there is no conflict of interest related to the publication of this paper.
Financial support: This work was supported financially by the Science and Technology Department of Sichuan Province of China, No. 2016SZ0039, 2016; and a grant from the Sichuan Province Medical Association in China, No. S15063, 2015. The funding bodies played no role in the study design, in the collection, analysis and interpretation of data, in the writing of the paper, and in the decision to submit the paper for publication
Reporting statement: This study follows the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement.
Biostatistics statement: The statistical methods of this study were reviewed by the biostatistician of West China Hospital, Sichuan University, China.
Copyright license agreement: The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open peer reviewer: Jonathan M. Borkum, University of Maine, USA.
Funding: This work was financially supported by the Science and Technology Department of Sichuan Province of China, No. 2016SZ0039, 2016; and a grant from the Sichuan Province Medical Association in China, No. S15063, 2015.
(Copyedited by Yu J, Li CH, Qiu Y, Song LP, Zhao M)
References
- Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, Jacobsson B, Damiano D Executive Committee for the Definition of Cerebral Palsy. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005;47:571–576. doi: 10.1017/s001216220500112x. [DOI] [PubMed] [Google Scholar]
- Blair E, Watson L. Epidemiology of cerebral palsy. Semin Fetal Neonatal Med. 2006;11:117–125. doi: 10.1016/j.siny.2005.10.010. [DOI] [PubMed] [Google Scholar]
- Cheuk DK, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database Syst Rev. 2007:CD005472. doi: 10.1002/14651858.CD005472.pub2. [DOI] [PubMed] [Google Scholar]
- Colver AF, Gibson M, Hey EN, Jarvis SN, Mackie PC, Richmond S. Increasing rates of cerebral palsy across the severity spectrum in north east England 1964-1993. The North of England Collaborative Cerebral Palsy Survey. Arch Dis Child Fetal Neonatal Ed. 2000;83:F7–F12. doi: 10.1136/fn.83.1.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabbous OA, Mostafa YM, El Noamany HA, El Shennawy SA, El Bagoury MA. Laser acupuncture as an adjunctive therapy for spastic cerebral palsy in children. Lasers Med Sci. 2016;31:1061–1067. doi: 10.1007/s10103-016-1951-6. [DOI] [PubMed] [Google Scholar]
- Deng LY, Xiong XC. Acupuncture in the rehabilitation therapyfor cerebral palsy children with motor dysfunction. Zhenjiu Linchuang Zazhi. 2012;6:28–30. [Google Scholar]
- Du X, Liang S, Wu ZF, Chen J, Jiang K. Observation on effectiveness of acupuncture treatment of children with spastic cerebral palsy by stimulating acupoints selected according to the day to match the heavenly stems and earthly branches. Zhen Ci Yan Jiu. 2016;41:462–465. [PubMed] [Google Scholar]
- Duncan B, Barton L, Edmonds D, Blashill BM. Parental perceptions of the therapeutic effect from osteopathic manipulation or acupuncture in children with spastic cerebral palsy. Clin Pediatr (Phila) 2004;43:349–353. doi: 10.1177/000992280404300406. [DOI] [PubMed] [Google Scholar]
- Duncan B, Shen K, Zou LP, Han TL, Lu ZL, Zheng H, Walsh M, Venker C, Su Y, Schnyer R, Caspi O. Evaluating intense rehabilitative therapies with and without acupuncture for children with cerebral palsy: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93:808–815. doi: 10.1016/j.apmr.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Furlan AD, van Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 2005:CD001351. doi: 10.1002/14651858.CD001351.pub2. [DOI] [PubMed] [Google Scholar]
- Graff DM, McDonald MJ. Auricular acupuncture for the treatment of pediatric migraines in the emergency department. Pediatr Emerg Care. 2016 doi: 10.1097/PEC.0000000000000789. doi: 10.1097/PEC.0000000000000789. [DOI] [PubMed] [Google Scholar]
- Graham HK. Botulinum toxin type A management of spasticity in the context of orthopaedic surgery for children with spastic cerebral palsy. Eur J Neurol 8 Suppl. 2001;5:30–39. doi: 10.1046/j.1468-1331.2001.00036.x. [DOI] [PubMed] [Google Scholar]
- Graham HK. Painful hip dislocation in cerebral palsy. Lancet. 2002;359:907–908. doi: 10.1016/s0140-6736(02)08015-7. [DOI] [PubMed] [Google Scholar]
- Hagberg B, Hagberg G, Olow I, von Wendt L. The changing panorama of cerebral palsy in Sweden. VII. Prevalence and origin in the birth year period 1987-90. Acta Paediatr. 1996;85:954–960. doi: 10.1111/j.1651-2227.1996.tb14193.x. [DOI] [PubMed] [Google Scholar]
- Higgins J, Green S. Oxford, UK: The Cochrane Collaboration; 2008. Cochrane handbook for systematic reviews of interventions version 5.0.0. [Google Scholar]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- Huang Q. Clinical study on acupuncture for hand dysfunction for children with cerebral palsy. Henan Zhongyi Xueyuan Xuebao. 2005;20:71–72. [Google Scholar]
- Hull D, Johnston DI. Essential Paediatrics. Edinburgh: Churchill Livingstone; 1999. [Google Scholar]
- Ji YH, Sun BD, Zhang J, Zhang R, Ji YH. Therapeutic effect of scalp-acupuncture combined with exercise therapy on spastic cerebral palsy of the child. Zhongguo Zhen Jiu. 2008;28:723–726. [PubMed] [Google Scholar]
- Jia J. Clinical study on treatment of infantile cerebral palsy by scalp acupuncture combined with modern rehabilitation. Zhongguo Zhen Jiu. 2003;9:513–514. [Google Scholar]
- Johansson BB, Haker E, von Arbin M, Britton M, Långström G, Terént A, Ursing D, Asplund K. Swedish Collaboration on Sensory Stimulation After Stroke (2001) Acupuncture and transcutaneous nerve stimulation in stroke rehabilitation: a randomized, controlled trial. Stroke. 32:707–713. doi: 10.1161/01.str.32.3.707. [DOI] [PubMed] [Google Scholar]
- Li HX, Li SW, Cheng LW. Scalp acupuncture combined with rehabilitation treatment to 32 children with spastic cerebral palsy. Xiandai Zhonyiyao. 2009;3:68–69. [Google Scholar]
- Li NL, Zhang Y, Wu WH, Liu JJ, Zeng FY. Effect of acupuncture on motor function of children with spastic cerebral palsy. Zhongguo Kangfu Lilun yu Shijian. 2014;7:679–680. [Google Scholar]
- Li S, Lin Q, Liu J. Prevalence of childhood cerebral palsy in six provinces in China. Zhonghua Yi Xue Za Zhi. 2001;81:1220–1223. [PubMed] [Google Scholar]
- Liang X. Xianyang, China: Shaanxi University of Chinese Medicine; 2014. The clinical study on acupuncture to improve gross motor function of lower limbs in children with spastic cerebral palsy. [Google Scholar]
- Liao HH, Yen HR, Muo CH, Lee YC, Wu MY, Chou LW, Sun MF, Chang TT. Complementary traditional Chinese medicine use in Children with cerebral palsy: a nationwide retrospective cohort study in Taiwan. BMC Complement Altern Med. 2017;17:155. doi: 10.1186/s12906-017-1668-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Q. Definition, diagnosis and classification of children with cerebral palsy. Zhonghua Erke Zazhi. 2005;43:262–264. [Google Scholar]
- Lin Q, Li S. Children with Cerebral Palsy. Beijing: Beijing Medical University Publishing House; 2000. [Google Scholar]
- Liptak GS. Complementary and alternative therapies for cerebral palsy. Ment Retard Dev Disabil Res Rev. 2005;11:156–163. doi: 10.1002/mrdd.20066. [DOI] [PubMed] [Google Scholar]
- Liu ZH, Qi YC, Pan PG, Ma MM, Qian XG, Fu WJ. Clinical observation on treatment of clearing the Governor Vessel and refreshing the mind needling in neural development and remediation of children with cerebral palsy. Chin J Integr Med. 2013;19:505–509. doi: 10.1007/s11655-013-1504-9. [DOI] [PubMed] [Google Scholar]
- Lou YJ, Liu Y, Shan HJ, Cao CH, Jie XS. Effect of acupuncture of “Xingnao Kaiqiao”on the behavior of an immature rat model of cerebral palsy and the underlying mechanism. Zhongguo Zuzhi Gongcheng Yanjiu. 2016;20:7314–7319. [Google Scholar]
- MacPherson H, White A, Cummings M, Jobst KA, Rose K, Niemtzow RC. Standards for Reporting Interventions in Controlled Trials of Acupuncture: the STRICTA recommendations. J Altern Complement Med. 2002;8:85–89. doi: 10.1089/107555302753507212. [DOI] [PubMed] [Google Scholar]
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Clin Oral Investig. 2003;7:2–7. doi: 10.1007/s00784-002-0188-x. [DOI] [PubMed] [Google Scholar]
- Morris S. Ashworth And Tardieu Scales: their clinical relevance for measuring spasticity in adult and paediatric neurological populations. Phys Ther Rev. 2002;7:53–62. [Google Scholar]
- Mu YP, Li N, Guan LJ, Wang CN, Shang SY, Wang Y. Therapies for children with cerebral palsy: A Web of Science-based literature analysis. Neural Regen Res. 2012;7:2632–2639. doi: 10.3969/j.issn.1673-5374.2012.33.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil. 2006;28:183–191. doi: 10.1080/09638280500158422. [DOI] [PubMed] [Google Scholar]
- Pakula AT, Van Naarden Braun K, Yeargin-Allsopp M. Cerebral palsy: classification and epidemiology. Phys Med Rehabil Clin N Am. 2009;20:425–452. doi: 10.1016/j.pmr.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Pennington L, Goldbart J, Marshall J. Speech and language therapy to improve the communication skills of children with cerebral palsy. Cochrane Database Syst Rev. 2004:CD003466. doi: 10.1002/14651858.CD003466.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pharoah PO, Cooke T. Cerebral palsy and multiple births. Arch Dis Child Fetal Neonatal Ed. 1996;75:F174–177. doi: 10.1136/fn.75.3.f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pountney D. Identifying and managing cerebral palsy. Br J of Neurosci Nurs. 2013;6:20–23. [Google Scholar]
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14. [PubMed] [Google Scholar]
- Shi LY, Shang Q, Ma CY. Effective research on treating fine dyskinesia in spastic cerebral palsy children by acupuncture at Neiguan point. Zhongyi Linchuang Yanjiu. 2016;5:24–26. [Google Scholar]
- Stanley FJ, Watson L. Trends in perinatal mortality and cerebral palsy in Western Australia, 1967 to 1985. BMJ. 1992;304:1658–1663. doi: 10.1136/bmj.304.6843.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steultjens EM, Dekker J, Bouter LM, van de Nes JC, Lambregts BL, van den Ende CH. Occupational therapy for children with cerebral palsy: a systematic review. Clin Rehabil. 2004;18:1–14. doi: 10.1191/0269215504cr697oa. [DOI] [PubMed] [Google Scholar]
- Sun JG, Ko CH, Wong V, Sun XR. Randomised control trial of tongue acupuncture versus sham acupuncture in improving functional outcome in cerebral palsy. J Neurol Neurosurg Psychiatry. 2004;75:1054–1057. doi: 10.1136/jnnp.2003.021485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svedberg LE, Nordahl UE, Lundeberg TC. Effects of acupuncture on skin temperature in children with neurological disorders and cold feet: an exploratory study. Complement Ther Med. 2001;9:89–97. doi: 10.1054/ctim.2001.0436. [DOI] [PubMed] [Google Scholar]
- Verma H, Srivastava V, Semwal BC. A review of cerebral palsy and its management. J Sci. 2012;2:54–62. [Google Scholar]
- Wang HL, Wu JW. Lin Xue-Jian's experience on treatment of a part of cerebral diseases with scalp acupuncture. Zhongguo Zhen Jiu. 2005;25:729–732. [PubMed] [Google Scholar]
- Wang Q, Hou T, Zhang C. Treatment of spastic cerebral palsy by selective posterior rhizotomy limited to a small extent. Zhonghua Xianwei Waike Zazhi. 2000;23:260–261. [Google Scholar]
- Wang SQ, Liang WX, Huang GH, Wu PC. Randomized controlled clinical trials for acupuncture treatment of spastic cerebral palsy children by bilateral horizontal puncturing from Yuzhen (BL 9) to Tianzhu (BL 10) Zhen Ci Yan Jiu. 2011;36:215–219. [PubMed] [Google Scholar]
- Wu Y, Jin Z, Li K, Lu ZL, Wong V, Han TL, Zheng H, Caspi O, Liu G, Zeng YW, Zou LP. Effect of acupuncture on the brain in children with spastic cerebral palsy using functional neuroimaging (FMRI) J Child Neurol. 2008;23:1267–1274. doi: 10.1177/0883073808318049. [DOI] [PubMed] [Google Scholar]
- Yang C, Hao Z, Zhang LL, Guo Q. Efficacy and safety of acupuncture in children: an overview of systematic reviews. Pediatr Res. 2015;78:112–119. doi: 10.1038/pr.2015.91. [DOI] [PubMed] [Google Scholar]
- Yang N, Hou XF. Clinical observation on treating 61 cases of spastic cerebral palsy by acupuncture plus physical therapy. Zhongyi Linchuang Yanjiu. 2016;4:20–22. [Google Scholar]
- Zhang HY, Du F. Clinical trials of acupuncture intervention combined with sitting training for cerebral palsy children with parafunctional sitting position. Zhen Ci Yan Jiu. 2013;38:403–406. 410. [PubMed] [Google Scholar]
- Zhang NX, Wang XY, Liu GZ, Li YB, Zhang HY. Randomized controlled clinical trials of individualized treatment of cerebral palsy children by warm-reinforcing needling combined with Bobath rehabilitation training. Zhen Ci Yan Jiu. 2014;39:318–323. [PubMed] [Google Scholar]
- Zhang PY, Hu FF. Influence of cluster needling at scalp acupoints combined with rehabilitation training on balance functions of children with cerebral palsy. World J Acupunct Moxibustion. 2012;22:23–31. [Google Scholar]
- Zhang SH, Liu M, Asplund K, Li L. Acupuncture for acute stroke. Cochrane Database Syst Rev. 2005:CD003317. doi: 10.1002/14651858.CD003317.pub2. [DOI] [PubMed] [Google Scholar]
- Zhao NX, Yan BC. Clinical observation of the electroacupuncture treatment to the hypotonic cerebral palsy on the Ex- B2 points. Jilin Yixue. 2012;5:932–933. [Google Scholar]
- Zhao Y, Liu Z, Jin B. Acupuncture based on nourishing spleen and kidney and dredging the governor vessel for motor function and ADL in children with spastic cerebral palsy. Zhongguo Zhen Jiu. 2017;37:45–48. doi: 10.13703/j.0255-2930.2017.01.010. [DOI] [PubMed] [Google Scholar]
- Zhou J, Liu HY, Deng H. Comparative research and follow-up study on treatment of spastic cerebral palsy with Jiaji (EX-B2) point needling. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2010;30:928–930. [PubMed] [Google Scholar]
- Zhu DJ, Yuan WL. Efficacy of acupuncture treatment to the motor disfunction in children with cerebral palsy. Zhongyiyao Daobao. 2013;5:73–74. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.