SUMMARY
Among the ameloblastomas, the desmoplastic variation is rare. The desmoplastic ameloblastoma (DA) is characterized by specific clinical, imaging, and histological features. The here presented retrospective analysis investigated the clinicoradiographic features of an overall of 115 DA-cases, having been reported in literature from 1984 to 2008. DA showed a nearly equal male to female ratio (55/59) with a prevalence within the forth and fifth decades. Sixty-two lesions occurred in the mandible and fifty-one lesions in the maxilla. Clinically, a painless swelling with buccal extension was the most common presentation being found in 48 cases. Radiologically, the lesion often presented multilocular (49.3%; 36/73), mixed radiolucent/radiopaque (55.6%; 50/90) and with ill-defined borders (64.0%; 48/75). Whereas enucleation provided a recurrence rate of 21.1%, resection reduced this rate remarkably to 3.1%. The average period until recurrence was 36.9 months. Histologically, scattered epithelial nests and extensively desmoplasia were prominent features of DA. In conclusion, these retrospective results confirm the statement that DA is a variation among ameloblastomas. DA present clinicoradiographic and histologic distinct features, when compared with “conventional ameloblastomas”.
Keywords: Desmoplastic ameloblastoma, Mandible, Maxilla, Histology, Radiology, Treatment
Introduction
Ameloblastomas, although locally invasive, are considered to be benign neoplasms deprived from odontogenic epithelium. The term “ameloblastoma” includes several clinicoradiographic and histological different types. DA is rare, accounting for approximately 4% to 13% of ameloblastomas.1–3 It was first described by Eversole et al.4 in 1984 as a new type of ameloblastoma which affected different mandibular areas, presenting a unique histopathological pattern and clinicoradiographic findings. This variation has been included in the World Health Organization’s histopathological classification.
Histologically, it is characterized with extensive stromal collagenisation or desmoplasia with small nests and strands of odontogenic epithelium (Fig. 1).5 Additionally “hybrid” lesions showing some microscopic features of the desmoplastic variant together with typical areas of follicular or plexiform ameloblastoma have been described.1 Most diagnoses are made related to the histological specimen after the DA was already removed.
Figure 1.
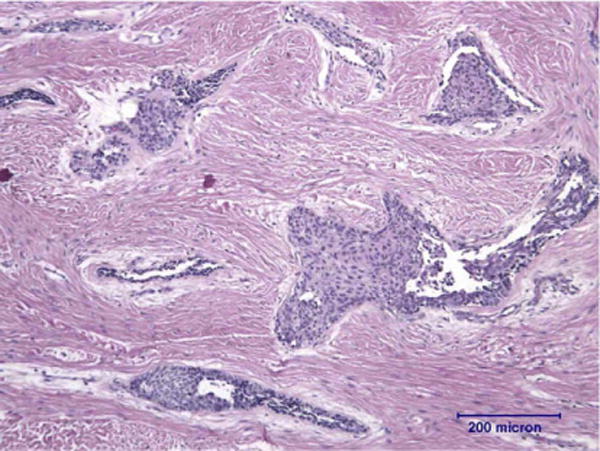
Histological specimen of a desmoplastic ameloblastoma presenting with irregularly shaped epithelial island, surrounded by narrow zones of loose-structured connective tissue embedded in desmoplastic stroma. (HE Hematoxylin and eosin stain, original magnification ×10.)
Radiologically, the DA frequently presented as diffuse, mixed radiolucent – radiopaque lesion, apting to be misdiagnosed as fibro-osseous lesion.6 Both surgeons and radiologists may be aware of clinicoradiographic features of the “common” ameloblastomas, however, may ignore this variation. The purpose of this article was to review the DA within the English literature in order to provide diagnostic tools for this rare variation of ameloblastomas.
A research on MEDLINE for adequately documented cases of DAs was performed in the English literature. Criteria for inclusion in the here presented study were a confirmed histopathological diagnosis of DAs with a detailed clinicoradiographic description. Thus, a total of 115 cases from 35 published papers1–4,6–36 have been analyzed and the clinicoradiographic data were summarized in Table 1. The 115 cases of DA including 12 cases of so-called “hybrid lesion of ameloblastoma where areas of intraosseous ameloblastoma coexist with areas of DA. The data was analyzed by SPSS 11.5 software program. The X2 test was used for the CROSSTABS procedure and exact test was used when needed. In all analyses, the significance level was set at a level of P ≤ 0.05.
Table 1.
Summary of data on reported cases of desmoplastic ameloblastoma.
| No. | % | |
|---|---|---|
| Patient age (yr) | 114 | |
| Mean, 41.9 | ||
| Range, 17–83 | ||
| Gender (n=114) | ||
| Female | 59 | 51.8 |
| Male | 55 | 48.2 |
| Tumor size (cm) (n = 72) | ||
| ⩾3.0 | 36 | 50.0 |
| <3.0 | 36 | 50.0 |
| Tumor location (n = 113) | ||
| Maxilla | 51 | 45.1 |
| Mandible | 62 | 54.9 |
| Tumor borders (n = 75) | ||
| Poorly defined | 48 | 64.0 |
| Well defined | 27 | 36.0 |
| Tumor locularity (n = 73) | ||
| Multilocular | 36 | 49.3 |
| Unilocular | 19 | 26.0 |
| No loculation | 18 | 24.7 |
| Tumor radiographic appearance (n = 90) | ||
| Mixed radiolucent/radiopaque | 50 | 55.6 |
| Radiolucent | 40 | 44.4 |
Clinical features
Age and gender distribution
Apart from 1 case without mentioned of age, the age and gender distributions of 114 cases DAs were listed in Fig. 2A. The age at time of primary presentation ranged from 17 to 83 years with a mean age of 41.9 years (males: 44.6 years, females: 39.0 years) and a median age of 42.0 years. The age prevalence was in the 3th to 5th decades. Whereas there were two peaks among females, in the 3rd and in the 4th decades, the males presented only a single peak in the 5th decade. Among the 114 DA patients, there were 59 (51.8%) females and 55 (48.2%) males. However, there is no statistically significant gender distribution as in other types of ameloblastomas. In the fifth decade the incidence rate is a significantly higher in males than females (p < 0.05). Although no difference between genders has been reported14 in the onset of this disease, people in the 4th and 5th decade are most commonly affected.
Figure 2.
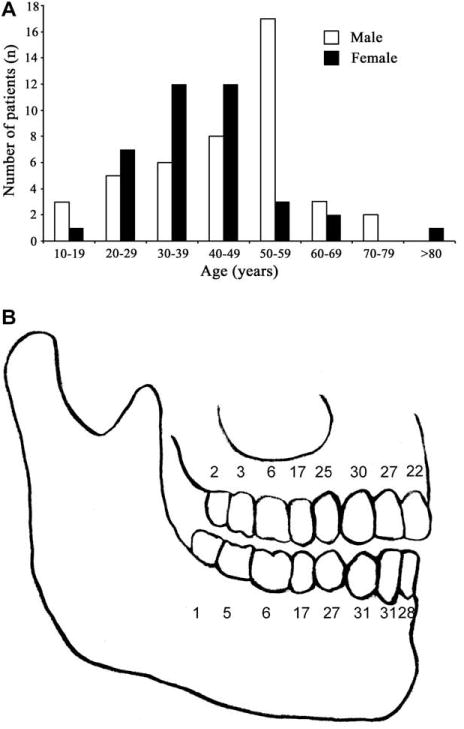
Age and gender distribution of 114 desmoplastic ameloblastomas (A). Distribution of tooth involvement among 61 desmoplastic ameloblastomas (B).
Race
The incidence of DA among ameloblastomas ranges from 0.9% to 12.1% in different races.1,26,31,35,37 Concerning the race, 69 out of 115 cases DAs with detailed description, of which 25(36.2%) were Japanese, 15(21.7%) were Chinese and 10(14.5%) were Indian. Data from different geographical regions seem to suggest a biogeographical pattern in that the relative frequency of DA is slightly higher in Asian population. However, more systematic studies on DA are needed to verify such suggestions.
Size
Regarding the tumor size of 3.0 cm in diameter, 32 cases (44.4%) of the DAs were larger, 36 cases (50.0%) smaller and only 4 cases (5.6%) equal to 3.0 cm at the initial presentation. In a review of 3677 ameloblastomas, Reichart et al.38 reported that the average tumor size at the initial presentation was 4.3 cm (median, 3.0 cm). Therefore it may be assumed that DA may be smaller than the “normal” type of ameloblastomas. There were neither statistical significance between the tumor size and localization, nor the recurrence (p > 0.05).
Location
Anatomical localization was described in 113 cases. 62 cases occurred in mandible and 51 cases in the maxilla. Detailed tooth location was reported in 61 cases, being shown in Fig. 2B. The anterior regions until the first premolar were frequently involved. In the maxilla, 42(82.4%) lesions were in the anterior region and 34(54.8%) in the mandible. The maxillary sinus was involved in nine and the ramus in two cases. Whereas most lesions were one-sided, a total of 18 crossed the midline.
Presentation
The clinical presentation of 56 cases DAs was summarized. Forty-eight (85.7%) patients presented with a painless swelling or a bone expansion,2–4,6–9,11–18,21,24–28,30–32,34,36 which was the most conspicuous clinical manifestation of the affected area. Six patients presented with a tender swelling.10,20,23,31,33 In case of maxillary sinus involvement, nasal27 and pharyngeal obstruction4 occurred, however with a very small probability (1.8%).
Among these 56 cases, 16 (69.6%) patients showed a buccal (Fig. 3), one (4.35%) a palatal/lingual and six (26.1%) both a buccal and a palatal/lingual expansion. Only 36 out 114 reports of DAs provided information about tooth resorption and 27 cases provided information about tooth displacement. In nine cases (25.0%) tooth resorption was reported. In 24(88.9%) out of 27 cases tooth displacement was observed (Fig. 4).
Figure 3.

Clinical aspect of a desmoplastic ameloblastoma presenting with slow-growing mass with buccal/labial expansion.
Figure 4.

Radiological features of desmoplastic ameloblastoma. The lesion presents with a “honeycomb appearance” with tooth displacement (A).Radiograph revealing a unilocular radiolucency (arrow) with tooth displacement in the mandible (B). Computed tomography present with an ill-defined mixed density (arrow) of buccal expansion (C).
Radiographic features
The radiological information available for each reviewed case was not uniform. Radiographically, 48(64.0%) out of 75 cases with detailed border description presented poorly defined borders, whereas well defined borders were detected in 27 (36.0%). The lesions appeared mixed radiolucent / radiopaque in 50(55.6%) out of 90 case, and radiolucent in 40(44.4%) cases. According to locularity, 36(49.3%) out of 73 cases with detailed description presented multilocular (Fig. 4A), 19(26.0%) cases were unilocular (Fig. 4B) and 18 (24.7%) cases were not loculated. Computed tomography was performed in 20 cases usually detecting ill-defined, mixed radioluceny–radiopacity with buccal expansion (Fig. 4C).2,3,6–9,11–19,25,26,28,29,39
Histopathology
Histologically, scattered epithelial nests and extensively desmoplasia were prominent features of DA (Fig. 1).40 Most tumors contain cords of odontogenic epithelium, but these tumors tend to lack the more typical follicular pattern. Typical ameloblastic columnar cells may be scant, and peripheral pallisading may be absent. In the focal area, the islands have a swirled hypercellular appearance. Osteoplasia may also be present. The surrounding stroma accompanied the cells islands are characterized for significant collagen proliferation. However, in some juxtaepithelial area, loose myxoid changes can be found.
Management
Treatment methods were mentioned in 83 out of 115 cases. Most cases of DA were treated by resection (77.1%) and some cases were treated by enucleation and/or curettage 19 (22.9%). Only 69 DA provided an available postoperative follow-up period between 2 months and 20 years. Eleven patients suffered from recurrence (15.9%) with an average recurrence period of 36.9 months.1,12,22,26,29,31,39 Among these patients, one underwent revision and showing thereafter no sign of recurrence after 6 years. Among these 11 patients, two suffered from recurrence after resection and four after enucleation, the treatment methods of other five cases were not mentioned. The remaining five remained unknown. The recurrence rate through the treatment of enucleation was significantly higher than that of resection (p < 0.01).
Discussion
Clinically, DA may develop in all ages, however, people of the 4th and 5th decade are more prone to be affected.14,17 No gender predilection of DA has been reported. Usually the DA variation is smaller in size than other types of ameloblastoma. DA occurs in the anterior or premolar regions of the jaws and there is not any difference in prevalence between the maxilla and mandible.
This represents a contrast with classic ameloblastomas, which are usually found in the posterior mandibular regions presenting a mandible to maxilla ratio of 5:1.38 The main symptom at first clinical examination of DA is a painless swelling, with frequently buccal expansion. Tooth displacement were frequently been seen.32
Radiologically, there is not any agreement among DA reviews as to whether it deals with a radiolucent or mixed radiolucent– radiopaque lesion.14,32 In a review, only 1 of the 15 cases of DA had a radiolucent appearance.32 Whether this is due to limited data or a specific patient population is uncertain. However, in the here presented retrospective analysis, the content of the lesion was mixed radiolucent/radiopaque in 55.6% cases. Radiographically, other types of ameloblastomas are classically described as a unilocular or multilocular radiolucences with well-defined borders,41 whereas DAs are usually described as poorly defined in most cases. In the series by Reichart et al.38, 51.1% of the tumors were described as unilocular, whereas 48.9% were described as multilocular or multicystic. When applying this criterion to the here presented study, 24.7% did not show any locularity, 26.0% were unilocular, and 49.3% were multilocular. On examination of the radiographic borders of 75 reported cases of desmoplastic ameloblastomas in the here presented study, poorly defined borders were reported in 48 cases (64.0%) and well defined borders were seen in only 27 cases (36.0%). The DA usually appears in the anterior and premolar regions as a mixed radiolucent and radiopaque lesion sometimes mimicking a benign fibro-osseous lesion.1 Approximately half of the reported lesions showed diffuse radiological borders32 and mimicking fibro-osseous lesions or malignant tumors. The lamina dura also was involved.34 The radiographic appearance may indicate that this tumor is more aggressive than other variants of ameloblastoma. According to Philipsen et al.,33 radiographically ill-defined borders suggest an infiltrative process with propensity to recur. Thus the pronounced stromal reaction characteristic of DAs can be viewed as a defensive response of the host to the “aggressive” tumor. This, along with the fact that recurrences of DAs have been documented by more than one author, suggests potentially aggressive biologic behavior.29,31,39 The ill-defined borders of DAs reflect the desirability for a relatively radical approach to treatment.
Concerning the biological behavior of DA, it is mentioned in the WHO classification of odontogenic tumors that DA, like unicystic ameloblastoma and peripheral ameloblastomas, possibly have a lower recurrence rate than other ameloblastomas.5 In contrast to that statement of the WHO, reviewing the literature provided the information that DA showed a similar recurrence rate (15.9%) with the other types of ameloblastomas. Keszler et al.29 even reported a higher recurrence rate (21.4%) than the other type (10.1%) of ameloblastoma. The reason for this may be somewhat hypothetical: First, radiographically, DAs are apt to be mismatched with fibro-osseous lesions. The accurate diagnosis of a DA is hard to achieve before the operation; Second, DA frequently present with ill-defined border making it difficult to investigate the exact interface of the lesion with normal bone; third, the more common location in the maxilla may produce an early invasion of adjacent structures. In view of the paucity of DA case series and the only limited understanding of its biologic behavior and prognosis, the proper treatment strategies for DA are not entirely defined so far. Whether the recurrence is due to the nature of the tumor or due to the incomplete surgery remains speculative. Prospective studies with regular and long term follow-up are needed to provide the necessary information before any conclusions in this aspect can be drawn. According to the average relapse time in 11 patients, which was 36.9 months, the follow-up period should be more than three years.
Conclusions
Clinically, DA usually presents with a painless buccal swelling predominantly located in the anterior of the maxilla and mandible. Radiologically, most DAs present with a multilocular mixed radiolucent/radiopaque lesion with ill-defined borders. Tooth displacement was frequently found and root resorption was discovered in 25% of the reported cases. Resection and enucleation are the main treatment modalities of DAs. The recurrence rate is similar to the “normal” ameloblastomas. The recurrence rate after enucleation is significantly higher than the one after resection.
Acknowledgments
This work is supported by a grant from National Natural Science Foundation of China (No.: 30600712) to Dr. Z.J. Sun.
Appendix
Data on 115 cases of desmoplastic ameloblastoma.
| Author | Age (Y) | Sex1 | Race | Tumor size (cm) | Tumor Location2 | Borders3 | Locularity4 | Radiology5 | Tooth resorption | Tooth displacement | Treatment6 | Follow-up7 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Smullin et al.2 | 44 | F | NA | <3.0 | Max.L3-5 | W | NA | NA | NA | NA | Res | NR1Y |
| Curran and Byerly7 | 56 | M | black | <3.0 | Mand.R4-5 | W | NA | NA | No | NA | Res | NR51M |
| Sivapathasundharam et al.8 | 25 | M | Indian | NA | Max.R3-5 | W | Uni | Mixed | No | Yes | Res | NA |
| 40 | M | Indian | NA | Max.L1-5 | W | Uni | Mixed | No | No | Res | NA | |
| 30 | F | Indian | NA | Max.L1-5 | I | NA | Mixed | No | No | Res | NA | |
| 32 | F | Indian | 3.0 | Max.L1-4 | I | Multi | Mixed | Yes | Yes | Res | NR1Y | |
| a | 40 | M | NA | NA | Max.L1-6 | I | NA | Mixed | No | No | Res | NA |
| a | 31 | F | NA | NA | Mand.L2-R5 | I | Uni | Mixed | No | Yes | Res | NA |
| Shashikanth et al.9 | 32 | F | Indian | <3.0 | Max.L1-4 | I | Multi | Mixed | Yes | Yes | Res | NR1Y |
| Desai et al.10 | 32 | M | Indian | >3.0 | Mand.Ramus | W | Uni | RL | NA | NA | Cure | NR2Y |
| Hirota et al.11 | 17 | F | Japanese | NA | Max.R3-4, sinus | W | Multi | Mixed | NA | Yes | Res | NR7Y |
| Pillai et al.12 | 24 | F | Indian | <3.0 | Max.L3-5, sinus | I | Multi | RL | No | Yes | Cure+BG | R2M |
| Durmus et al.13 | 68 | M | Turkish | <3.0 | Mand.R1-3 | W | Uni | RL | Yes | NA | Cure | NR32M |
| Beckley et al.14 | 31 | M | Hispanic | <3.0 | Mand.L3-4 | I | No Loc | Mixed | No | Yes | Res+BG | NR19M |
| Iida et al.15 | 52 | M | Japanese | NA | Max.L2-5.sinus | I | Multi | Mixed | NA | Yes | Res | NR |
| Manuel et al.16 | 20 | F | NA | <3.0 | Max.L3-4 | W | Uni | Mixed | No | Yes | Res | NR22M |
| Mintz and Velez17 | 52 | M | NA | NA | Max.L1-8, sinus | I | Multi | Mixed | NA | Yes | Res | NR |
| 51 | F | NA | NA | Mand.R3-L5 | I | Multi | Mixed | NA | Yes | Res+BG | NR1Y | |
| Wakoh et al.18a | 35 | F | Japanese | >3.0 | Mand. L3-5 | W | Multi | Mixed | Yes | Yes | Res | NR |
| Philipsen et al.3 | 42 | F | Caucasian | NA | Mand.L4-R4 | I | Uni | Mixed | NA | Yes | Res+BG | NR36M |
| Kishino et al.19 | 41 | M | Japanese | >3.0 | Max.R5-L2 | W | Multi | RL | No | NA | Res | NR17Y |
| 28 | M | Japanese | >3.0 | Max.R1-R4 | I | NA | Mixed | No | NA | Res | NR72M | |
| 57 | M | Japanese | <3.0 | Max.R1-R2 | W | NA | RL | No | NA | Res | NR8Y | |
| 58 | F | Japanese | 3.0 | Max.L1-L2 | W | Uni | RL | No | NA | Cure | NR16Y | |
| 17 | M | Japanese | <3.0 | Mand.R6-R7 | W | Uni | RL | No | NA | Cure | NR5Y | |
| 50 | M | Japanese | >3.0 | Mand.L5-R4 | I | NA | Mixed | No | NA | Res | NR6Y | |
| 51 | M | Japanese | >3.0 | Mand.L5-R4 | I | NA | Mixed | No | NA | Res+BG | NR23Y | |
| 47 | M | Japanese | >3.0 | Mand.L4-R2 | I | NA | Mixed | No | NA | Res+BG | NR20Y | |
| 42 | M | Japanese | >3.0 | Mand.L3-R5 | I | NA | Mixed | No | NA | NA | NA | |
| Saran et al.20 | 25 | F | Indian | <3.0 | Max.L2-4 | W | Uni | NA | NA | NA | Res | NR10M |
| Louis et al.21 | 33 | M | Black | <3.0 | Max.L3-4, sinus | I | NA | Mixed | No | Yes | Res+BG | NR18M |
| Takata et al.22 | 53 | M | Japanese | >3.0 | Max.R2-3 | W | No Loc | RL | Yes | NA | Res | NR |
| 33 | F | Japanese | 3.0 | Max.R1-5 | I | Multi | Mixed | No | NA | Cure | NR | |
| 51 | M | Japanese | <3.0 | Max.L3-5 | W | Uni | RL | No | NA | Res | NR | |
| 52 | M | Japanese | >3.0 | Max.L2-5 | I | Multi | Mixed | No | NA | Res | NR | |
| 54 | M | Japanese | >3.0 | Mand.R1-L5 | W | No Loc | Mixed | No | NA | Res | NR | |
| 17 | M | Japanese | <3.0 | Mand.L3-5 | I | Multi | Mixed | No | NA | Cure | 4R | |
| a | 48 | M | Japanese | >3.0 | Mand.R2-6 | I | Multi | Mixed | NA | Yes | Cure | R14M |
| Kawai et al.6 | 56 | M | Japanese | NA | Mand. L4-7 | W | Uni | RL | NA | NA | Res | NA |
| Ludvikoya et al.23 | 50 | M | NA | >3.0 | Mand.R4-8 | I | No Loc | RL | NA | NA | Res | NR |
| 42 | F | NA | <3.0 | Mand.L4-5 | I | No Loc | RL | NA | NA | Res | NR3Y | |
| Sakashita et al.24 | 60 | F | Japanese | >3.0 | Max.L1-4 | I | Multi | RL | NA | NA | Res | NR |
| Lee et al.25 | 83 | F | Asian | <3.0 | Mand.L2-3 | W | Multi | Mixed | NA | Yes | Res | NR |
| Lam et al.26 | 64 | M | Chinese | >3.0 | Max: A, PM, M | I | No Loc | RL | NA | NA | Res | R2Y |
| 18 | M | Chinese | >3.0 | Max: A | I | Multi | RL | NA | NA | Res | NR53M | |
| 68 | F | Chinese | <3.0 | Max:PM | I | Multi | RL | NA | NA | Cure | R74M | |
| 37 | F | Chinese | <3.0 | Mand: A | I | Multi | RL | NA | NA | Res | NR77M | |
| 37 | M | Chinese | <3.0 | Mand: A | I | No loc | RL | NA | NA | Res | NR32M | |
| Fukushima et al.27 | 70 | M | NA | >3.0 | Max: PM, M.sinus | I | No Loc | Mixed | NA | NA | Res | NR18M |
| Thompson et al.28 | 31 | F | Black | >3.0 | Max: L2-6.sinus | I | No Loc | Mixed | Yes | Yes | Res+BG | NR3Y |
| Keszler et al.29(14 cases) | 19-62 (Mean 37.8) in 13; 1NA | 11 F 2 M 1 NA | NA | NA | 2Max; 10Mand; 2NA | 4W | 4 Uni 5 Multi | 9 RL; 3 Mixed | NA | NA | 5 Res9Cure | 3R;11NR |
| Ashman et al.30 | 53 | M | Black | >3.0 | Mand: A, PM | W | No Loc | Mixed | NA | Yes | Res | NR9M |
| Ng and Siar31 | 21 | F | Chinese | <3.0 | Mand;L1-4 | I | NA | RL | NA | NA | Res | NA |
| 25 | M | Chinese | NA | Max, right | NA | NA | Mixed | NA | NA | Res | NA | |
| 25 | M | Malay | NA | Mand.R2-L4 | NA | Multi | RL | NA | NA | Res | NA | |
| 27 | F | Chinese | NA | Mand.R2-L4 | NA | NA | Mixed | NA | NA | NA | NA | |
| 29 | F | Kadazan | NA | Mand.R5-L5 | NA | Multi | Mixed | NA | NA | Res | NA | |
| 32 | F | Indian | NA | Max.L2-3 | NA | NA | NA | NA | NA | NA | NA | |
| 33 | M | Malay | 3.0 | Max.R1-L3 | NA | NA | Mixed | NA | NA | NA | NA | |
| 33 | F | Malay | NA | Max.R2-L5 | I | NA | NA | NA | NA | Res | NR1Y | |
| 38 | M | Malay | <3.0 | Max.L2-3 | NA | NA | NA | NA | NA | Res | NA | |
| 40 | F | Chinese | NA | Mand;anterior | NA | Multi | RL | NA | NA | NA | NA | |
| 41 | F | Malay | NA | Max, R3 | NA | NA | NA | NA | NA | Res | NA | |
| 42 | F | Chinese | NA | L, Horiz ramus | NA | NA | NA | NA | NA | NA | NA | |
| 43 | F | Malay | NA | Mand.R3-L3 | NA | NA | NA | NA | NA | NA | NA | |
| 43 | F | Chinese | NA | Mand.R4-L2 | NA | Multi | RL | NA | NA | NA | NA | |
| 44 | F | Indian | <3.0 | Mand.L3 | NA | NA | NA | NA | NA | Res | R4Y | |
| 46 | F | Sikh | NA | Max.Left | NA | NA | Mixed | NA | NA | Res | NR1Y | |
| 60 | M | Chinese | NA | Mand.L2-3 | NA | Multi | RL | NA | NA | NA | NA | |
| Kaffe et al.32 | 41 | M | NA | >3.0 | Max: L2-R7, sinus | I | No Loc | Mixed | NA | NA | Res | NR3Y |
| Philipsen et al.33 | 21 | M | Chinese | >3.0 | Max: L1-R6 | I | Multi | RL | Yes | Yes | Res+BG | NA |
| 53 | M | Chinese | >3.0 | Max: L1-8 | I | Multi | RL | Yes | Yes | Res | NA | |
| a | 55 | M | Chinese | >3.0 | Mand: L3-7 | I | Multi | Mixed | Yes | NA | Res | NA |
| Tanimoto et al.34 | 24 | F | Japanese | >3.0 | Mand: L2-6 | I | NA | Lucent | No | Yes | Res | NR1Y |
| Higuchi et al.35 | 46 | M | NA | >3.0 | Max:A | I | Multi | Mixed | No | Yes | NA | NA |
| 38 | F | NA | >3.0 | Mand:A | W | Multi | Mixed | Yes | Yes | NA | NA | |
| 53 | M | NA | <3.0 | Max:PM.M | W | Uni | Mixed | No | Yes | NA | NA | |
| a | 58 | M | Japanese | >3.0 | Mand:A, PM | NA | Multi | Mixed | NA | NA | Cure | NR |
| a | 70 | M | Japanese | >3.0 | Mand:PM.M | NA | Multi | Mixed | NA | NA | Res | NR |
| Yoshimura and Saito36 | 36 | F | Japanese | >3.0 | Max: A, PM, M, sinus | I | Multi | Mixed | NA | NA | Res | NR9Y |
| Waldron andel-Mofty1 (14 cases) | 21 to 68 (mean, 45.5) | 7M,7F | NA | 13 < 3.0 1 > 3.0 | 2 Mand.A; 3 Mand. PM; 2 Mand.M;6 Maxi.A; 1 Max.PM | 5I;1W | 1 Uni 5 No loc | 4 Mixed 2 RL | NA | NA | NA | 2R1NR 11NA |
| 5 casesa | 25-82 | 2M,3F | NA | NA | 4 Mand: PM, M; 1 Mand | NA | NA | NA | NA | NA | NA | NA |
| Eversole et al.4 | 48 | F | Malaysian | >3.0 | Max: PM, M | I | No Loc | Mixed | NA | NA | Res | NR2Y |
| 50 | F | Caucasian | <3.0 | Mand: A, PM, M | I | Uni | Lucen | NA | NA | NA | NA | |
| 47 | F | Black | NA | Mand: A | I | No Loc | Mixed | NA | Yes | Res+BG | NA |
F: Female, M: Male.
Mand: Mandibular, Max: Maxillary, L: Left, R: Right, A: Anterior, P: Posterior.
I: Ill-defined, W: Well defined.
M: Multilocular, U: Unilocular.
RL: Radiolucency, RO: Radiopaque, Mixed: Mixed radiolucent-radiopaque.
Curr: Curettage; Res: Resection; BG: Bone graft.
NR: No recurrence.
Hybrid lesion of ameloblastoma.
Footnotes
Conflict of Interest Statement
None declared
References
- 1.Waldron CA, el-Mofty SK. A histopathologic study of 116 ameloblastomas with special reference to the desmoplastic variant. Oral Surg Oral Med Oral Pathol. 1987;63(4):441–51. doi: 10.1016/0030-4220(87)90257-x. [DOI] [PubMed] [Google Scholar]
- 2.Smullin SE, Faquin W, Susarla SM, Kaban LB. Peripheral desmoplastic ameloblastoma: report of a case and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(1):37–40. doi: 10.1016/j.tripleo.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 3.Philipsen HP, Reichart PA, Takata T. Desmoplastic ameloblastoma (including “hybrid” lesion of ameloblastoma). Biological profile based on 100 cases from the literature and own files. Oral Oncol. 2001;37(5):455–60. doi: 10.1016/s1368-8375(00)00111-1. [DOI] [PubMed] [Google Scholar]
- 4.Eversole LR, Leider AS, Strub D. Radiographic characteristics of cystogenic ameloblastoma. Oral Surg Oral Med Oral Pathol. 1984;57(5):572–7. doi: 10.1016/0030-4220(84)90320-7. [DOI] [PubMed] [Google Scholar]
- 5.Gardner DG, Heikinheimo K, Shear M, Philipsen HP, Coleman H. Ameloblastomas. In: Barnes L, Eveson EJ, Reichart P, Sidransky D, editors. World Health Organization classification of tumors: pathology and genetics of head and neck tumors. 3rd. Lyon: IARC Press; 2005. pp. 296–300. [Google Scholar]
- 6.Kawai T, Kishino M, Hiranuma H, Sasai T, Ishida T. A unique case of desmoplastic ameloblastoma of the mandible: report of a case and brief review of the English language literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87(2):258–63. doi: 10.1016/s1079-2104(99)70282-9. [DOI] [PubMed] [Google Scholar]
- 7.Curran AE, Byerly PD. Peripheral desmoplastic ameloblastoma: report of a rare case. J Oral Maxillofac Surg. 2008;66(4):820–5. doi: 10.1016/j.joms.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 8.Sivapathasundharam B, Einstein A, Syed RI. Desmoplastic ameloblastoma in Indians: report of five cases and review of literature. Indian J Dent Res. 2007;18(4):218–21. doi: 10.4103/0970-9290.35836. [DOI] [PubMed] [Google Scholar]
- 9.Shashikanth MC, Neetha MC, Ali IM, Shambulingappa P. Desmoplastic ameloblastoma in the maxilla: a case report and review of literature. Indian J Dent Res. 2007;18(4):214–7. doi: 10.4103/0970-9290.35835. [DOI] [PubMed] [Google Scholar]
- 10.Desai H, Sood R, Shah R, Cawda J, Pandya H. Desmoplastic ameloblastoma: report of a unique case and review of literature. Indian J Dent Res. 2006;17(1):45–9. doi: 10.4103/0970-9290.29892. [DOI] [PubMed] [Google Scholar]
- 11.Hirota M, Aoki S, Kawabe R, Fujita K. Desmoplastic ameloblastoma featuring basal cell ameloblastoma: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99(2):160–4. doi: 10.1016/j.tripleo.2004.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Pillai RS, Ongole R, Ahsan A, Radhakrishnan RA, Pai KM. Recurrent desmoplastic ameloblastoma of the maxilla: a case report. J Can Dent Assoc. 2004;70(2):100–4. [PubMed] [Google Scholar]
- 13.Durmus E, Kalayci A, Ozturk A, Gunhan O. Desmoplastic ameloblastoma in the mandible. J Craniofac Surg. 2003;14(6):873–5. doi: 10.1097/00001665-200311000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Beckley ML, Farhood V, Helfend LK, Alijanian A. Desmoplastic ameloblastoma of the mandible: a case report and review of the literature. J Oral Maxillofac Surg. 2002;60(2):194–8. doi: 10.1053/joms.2002.29822. [DOI] [PubMed] [Google Scholar]
- 15.Iida S, Kogo M, Kishino M, Matsuya T. Desmoplastic ameloblastoma with large cystic change in the maxillary sinus: report of a case. J Oral Maxillofac Surg. 2002;60(10):1195–8. doi: 10.1053/joms.2002.35033. [DOI] [PubMed] [Google Scholar]
- 16.Manuel S, Simon D, Rajendran R, Naik BR. Desmoplastic ameloblastoma: a case report. J Oral Maxillofac Surg. 2002;60(10):1186–8. doi: 10.1053/joms.2002.35030. [DOI] [PubMed] [Google Scholar]
- 17.Mintz S, Velez I. Desmoplastic variant of ameloblastoma: report of two cases and review of the literature. J Am Dent Assoc. 2002;133(8):1072–5. doi: 10.14219/jada.archive.2002.0331. [DOI] [PubMed] [Google Scholar]
- 18.Wakoh M, Harada T, Inoue T. Follicular/desmoplastic hybrid ameloblastoma with radiographic features of concomitant fibro-osseous and solitary cystic lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):774–80. doi: 10.1067/moe.2002.129182. [DOI] [PubMed] [Google Scholar]
- 19.Kishino M, Murakami S, Fukuda Y, Ishida T. Pathology of the desmoplastic ameloblastoma. J Oral Pathol Med. 2001;30(1):35–40. doi: 10.1034/j.1600-0714.2001.300106.x. [DOI] [PubMed] [Google Scholar]
- 20.Saran RK, Nijhawan R, Vasishta RK, Rattan V. Desmoplastic ameloblastoma: a case report with fine-needle aspiration cytologic findings. Diagn Cytopathol. 2000;23(2):114–7. doi: 10.1002/1097-0339(200008)23:2<114::aid-dc10>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 21.Louis PJ, Fugler RC, August M. Mixed radiolucent/radiopaque lesion of the maxilla. J Oral Maxillofac Surg. 2000;58(1):86–90. doi: 10.1016/s0278-2391(00)80022-1. [DOI] [PubMed] [Google Scholar]
- 22.Takata T, Miyauchi M, Ogawa I, Zhao M, Kudo Y, Sato S, et al. So-called ‘hybrid’ lesion of desmoplastic and conventional ameloblastoma: report of a case and review of the literature. Pathol Int. 1999;49(11):1014–8. doi: 10.1046/j.1440-1827.1999.00972.x. [DOI] [PubMed] [Google Scholar]
- 23.Ludvikoya M, Michal M, Zamecnik M, Houba R, Sedlacek P, Csillagi E, et al. Desmoplastic ameloblastoma. Cesk Patol. 1998;34(3):94–8. [PubMed] [Google Scholar]
- 24.Sakashita H, Miyata M, Okabe K, Kurumaya H. Desmoplastic ameloblastoma in the maxilla: a case report. J Oral Maxillofac Surg. 1998;56(6):783–6. doi: 10.1016/s0278-2391(98)90820-5. [DOI] [PubMed] [Google Scholar]
- 25.Lee CY, Lee J, Hirata K, Tomich CE. Desmoplastic variant of ameloblastoma in an 83-year-ald Asian female: report of a case with literature review. Hawaii Dent J. 1998;29(3):12–4. [PubMed] [Google Scholar]
- 26.Lam KY, Chan AC, Wu PC, Chau KY, Tideman H, Wei W. Desmoplastic variant of ameloblastoma in Chinese patients. Br J Oral Maxillofac Surg. 1998;36(2):129–34. doi: 10.1016/s0266-4356(98)90181-4. [DOI] [PubMed] [Google Scholar]
- 27.Fukushima D, Kobayashi H, Takeda I, Yamane G, Tanaka Y. A case of desmoplastic ameloblastoma of the maxilla. Bull Tokyo Dent Coll. 1997;38(3):223–7. [PubMed] [Google Scholar]
- 28.Thompson IO, van Rensburg LJ, Phillips VM. Desmoplastic ameloblastoma: correlative histopathology, radiology and CT-MR imaging. J Oral Pathol Med. 1996;25(7):405–10. doi: 10.1111/j.1600-0714.1996.tb00287.x. [DOI] [PubMed] [Google Scholar]
- 29.Keszler A, Paparella ML, Dominguez FV. Desmoplastic and non-desmoplastic ameloblastoma: a comparative clinicopathological analysis. Oral Dis. 1996;2(3):228–31. doi: 10.1111/j.1601-0825.1996.tb00229.x. [DOI] [PubMed] [Google Scholar]
- 30.Ashman SG, Corio RL, Eisele DW, Murphy MT. Desmoplastic ameloblastoma. A case report and literature review. Oral Surg Oral Med Oral Pathol. 1993;75(4):479–82. doi: 10.1016/0030-4220(93)90174-3. [DOI] [PubMed] [Google Scholar]
- 31.Ng KH, Siar CH. Desmoplastic variant of ameloblastoma in Malaysians. Br J Oral Maxillofac Surg. 1993;31(5):299–303. doi: 10.1016/0266-4356(93)90064-4. [DOI] [PubMed] [Google Scholar]
- 32.Kaffe I, Buchner A, Taicher S. Radiologic features of desmoplastic variant of ameloblastoma. Oral Surg Oral Med Oral Pathol. 1993;76(4):525–9. doi: 10.1016/0030-4220(93)90023-w. [DOI] [PubMed] [Google Scholar]
- 33.Philipsen HP, Ormiston IW, Reichart PA. The desmo-and osteoplastic ameloblastoma. Histologic variant or clinicopathologic entity? Case reports. Int J Oral Maxillofac Surg. 1992;21(6):352–7. doi: 10.1016/s0901-5027(05)80761-1. [DOI] [PubMed] [Google Scholar]
- 34.Tanimoto K, Takata T, Suei Y, Wada T. A case of desmoplastic variant of a mandibular ameloblastoma. J Oral Maxillofac Surg. 1991;49(1):94–7. doi: 10.1016/0278-2391(91)90277-s. [DOI] [PubMed] [Google Scholar]
- 35.Higuchi Y, Nakamura N, Ohishi M, Tashiro H. Unusual ameloblastoma with extensive stromal desmoplasia. J Craniomaxillofac Surg. 1991;19(7):323–7. doi: 10.1016/s1010-5182(05)80341-5. [DOI] [PubMed] [Google Scholar]
- 36.Yoshimura Y, Saito H. Desmoplastic variant of ameloblastoma: report of a case and review of the literature. J Oral Maxillofac Surg. 1990;48(11):1231–5. doi: 10.1016/0278-2391(90)90546-e. [DOI] [PubMed] [Google Scholar]
- 37.Raubenheimer EJ, van Heerden WF, Noffke CE. Infrequent clinicopathological findings in 108 ameloblastomas. J Oral Pathol Med. 1995;24(5):227–32. doi: 10.1111/j.1600-0714.1995.tb01172.x. [DOI] [PubMed] [Google Scholar]
- 38.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B(2):86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 39.Takata T, Miyauchi M, Ito H, Ogawa I, Kudo Y, Zhao M, et al. Clinical and histopathological analyses of desmoplastic ameloblastoma. Pathol Res Pract. 1999;195(10):669–75. doi: 10.1016/S0344-0338(99)80057-0. [DOI] [PubMed] [Google Scholar]
- 40.Kramer IRH, Pingborg JJ, Shear M. World Health Organization histological classification of tumors. 2nd. Berlin: Springer; 1991. [Google Scholar]
- 41.Mehlisch DR, Dahlin DC, Masson JK. Ameloblastoma: a clinicopathologic report. J Oral Surg. 1972;30(1):9–22. [PubMed] [Google Scholar]


