Abstract
The purpose of this article was to determine if pediatric dental treatment under general anesthesia utilizing orotracheal intubation takes longer than using nasotracheal intubation techniques. Twenty-six American Society of Anesthesiologists Physical Status Classification I and II pediatric dental patients, ages 2–8 years treated under general anesthesia, were assigned to 1 of 2 groups: (a) nasotracheal intubation (control, n = 13), (b) orotracheal intubation (experimental, n = 13). Times for intubation, radiographic imaging, and dental procedures, as well as total case time were quantified. Data were collected on airway difficulty, numbers of providers needed for intubation, intubation attempts, and intubation trauma. There was a significant difference in mean intubation time (oral = 2.1 minutes versus nasal = 6.3 minutes; p < .01). There was no difference in mean radiograph time (oral = 4.2 minutes versus nasal = 3.4 minutes; p = .144), and overall radiograph image quality was not affected. There was no difference in dental procedure time (p = .603) or total case time (p = .695). Additional providers were needed for intubation and more attempts were required for nasotracheal intubation versus orotracheal intubation (6 additional providers/22 attempts vs 0 additional providers/15 attempts, p < .01 and p < .05, respectively). Nine of 13 nasotracheal intubations were rated as traumatic (69%) versus 0 of 13 for orotracheal intubations (0%) (p < .01). In 7/9 orotracheal intubation cases (78%), the tube was not moved during treatment (p < .01). Orotracheal intubation does not increase case time, does not interfere with radiographic imaging, and is less traumatic for the patient when performed by physician anesthesiologists, emergency and pediatric medicine physician residents, certified registered nurse anesthetists, and student nurse anesthetists, all with variable nasotracheal intubation experience.
Key Words: Oral intubation dental, Pediatric general anesthesia
There are occasions in which children are not able to tolerate dental treatment in the conventional dental office setting. For these patients, advanced techniques, such as general anesthesia, are necessary to provide quality care in a safe and humane manner. Hospital protocols require that surgical and anesthesia consents be obtained before any procedure. During the anesthesia consent process, nasotracheal intubation is discussed, but consent for a specific intubation technique is not obtained. Assuming there are no medical contraindications, the anesthesia provider may defer to the dental provider to choose the preferred method of intubation technique (oral vs nasal). It is the authors' opinion that most pediatric dentists prefer nasotracheal intubation for airway management, because it does not interfere with treatment, it decreases the likelihood of tube displacement from head movement during treatment, no interruption in treatment is necessary to move the tube from side-to side, and evaluation of the dental occlusion can easily be completed. However, there are additional risks associated with nasotracheal intubation, including increased risk of epistaxis, adenoid dislodgement, eustachian tube obstruction, maxillary sinusitis, and bacteremia.1–3
It is also our belief that there is a perception among pediatric dentists that dental procedures and intraoral radiography are easier and faster with nasotracheal intubation compared to orotracheal intubation. There is no supporting literature to validate these perceptions. The purpose of this pilot study is to quantify the time different portions of dental treatment require under general anesthesia utilizing 2 intubation techniques (oral vs nasal).
METHODS
The Mercy Health St. Vincent Medical Center and Mercy Health Children's Hospital institutional review board (Toledo, OH) reviewed and approved this pilot study on March 4, 2015 (P-0115101). Pediatric patients from the University of Toledo Medical Center Dental Service requiring treatment under general anesthesia at Mercy Health Children's Hospital in Toledo, Ohio, or Mercy Health Arrowhead Surgical Center in Maumee, Ohio, constituted a convenience sample for this pilot study. The parent or legal guardian of subjects meeting the inclusion criteria (all American Society of Anesthesiologists [ASA] Physical Status Classification I and II ages 2–12) were offered the opportunity to participate in the study. Written informed consent was obtained by the author (MPN, Diplomate American Board of Pediatric Dentistry) before the initiation of treatment.
Potential research subjects were screened for inclusion during the preoperative evaluation at the time of treatment consent. All subjects consenting to participate were assigned a de-identified case number that corresponded with a randomization schedule that indicated how each subject was to be assigned, either nasotracheal intubation group (control) or orotracheal intubation group (experimental). All dental treatment was completed by 1 provider. Twenty-six ASA I and II pediatric dental patients, ages 2–8 years, scheduled for dental treatment in the operating room were enrolled and randomly assigned to either nasotracheal intubation group (control) or orotracheal intubation group (experimental).
There were 5 primary variables tested in this investigation: anesthesia intubation time, radiograph time, radiographic image quality and quantity, dental procedure time, and total case time. In addition, secondary variables gathered included age, gender, weight, ethnicity, number of teeth restored/extracted, type of teeth restored/extracted, anesthesia provider type, anesthesia provider experience, Mallampati score, intubation difficulty, number of providers needed for intubation, number of intubation attempts, trauma associated with intubation, additional intubation equipment necessary, and side-to-side movement of the orotracheal tube.
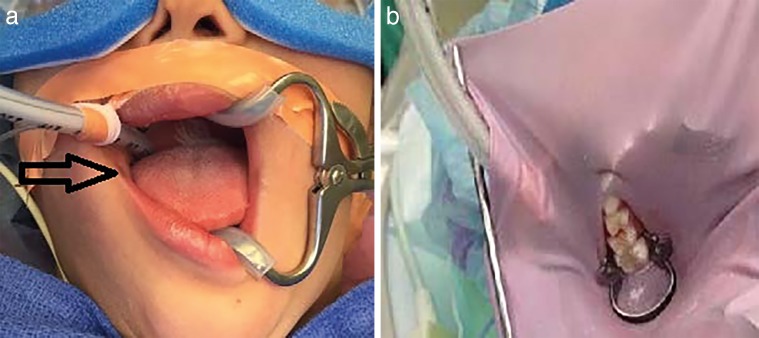
All data were collected by a dentist in an observational role. Chronographs were used to quantify the intubation time, radiograph time, dental procedure time, and total case time (Figure 1). An anesthesia survey was completed by the anesthesia provider at the completion of each case to gather the secondary variables. Dental treatment completed was recorded, and a relative value unit (RVU) scale was utilized to quantify case size and complexity.
Figure 1.
Timeline.
Intubation time was measured in the following manner. For orotracheal intubation, time started when the laryngoscope entered the oral cavity (which is the first airway maneuver after mask induction), and ended when the tube was taped and secured in position. For nasotracheal intubation, the time was started at the initiation of the first airway maneuver after mask induction (this was selected due to anesthesia provider technique variability, such as use of vasoconstrictor spray and/or nasal dilation with nasopharyngeal tubes), and ended when the tube was taped and secured in position. Radiograph time started with the placement of the first film/sensor and ended when the last image was exposed. Radiograph film size, the number of images taken, the number of nondiagnostic images, and the number of retakes based upon poor image quality were recorded. Dental procedure time was started when the operator verbally indicated “exam start,” and ended with the removal of the throat pack. Total case time was measured from the beginning of the intubation time until removal of the throat pack.
No effort was made to interfere with the anesthesia provider's methodology. Anesthesia providers performing the intubations included 3 physician anesthesiologists (average 16 years' experience), 16 certified registered nurse anesthetists (average 18.6 years' experience), 5 student nurse anesthetists, 1 emergency medicine physician resident, and 1 pediatric medicine physician resident. The anesthesia staff at Mercy Health Children's Hospital and Mercy Health Arrowhead Surgical Center perform approximately 15–20 nasotracheal intubations per month for pediatric dentistry and oral surgery cases divided among a large anesthesia staff. Our goal was to quantify our primary research variables in the environment in which we often work.
The intubation technique was relatively consistent for the orotracheal intubation (experimental) group. General anesthesia was induced by way of mask induction. Intravenous access was established. Intravenous medications were administered, primarily lidocaine, fentanyl, and glycopyrrolate. Direct laryngoscopy was performed followed by intubation. Confirmation of intubation was accomplished by the presence of expired carbon dioxide. Correct tube position was assessed by the presence of equal and bilateral chest expansion and auscultation of lung fields. The orotracheal tube was secured in its correct position.
The intubation technique for the nasotracheal intubation (control) group involved more steps and had more variability. General anesthesia was induced by way of mask induction. Intravenous access was established. Intravenous medications were administered, primarily lidocaine, fentanyl, glycopyrrolate, and sometimes a muscle relaxant. Some providers used phenylephrine nasal spray (n = 9) prior to nasotracheal intubation. One provider used a lubricated nasopharyngeal airway following the use of phenylephrine nasal spray prior to nasotracheal intubation. All intubation tubes were conventional cuffed endotracheal tubes used nasally. Some providers used an endotracheal tube smaller than would be calculated for orotracheal intubation; others did not. The tubes were warmed and lubricated prior to introduction into the nasal cavity. Once the tube was gently passed into the nasopharynx, direct laryngoscopy and intubation with McGill forceps was accomplished. Confirmation of intubation was accomplished by the presence of expired carbon dioxide with correct tube position assessed by the presence of equal, bilateral chest expansion and auscultation of lung fields. The nasotracheal tube was secured in its correct position.
Data analysis was completed using SPSS software and included descriptive statistics, regression analysis, t-test, Mann-Whitney U test, and analysis of variance.
RESULTS
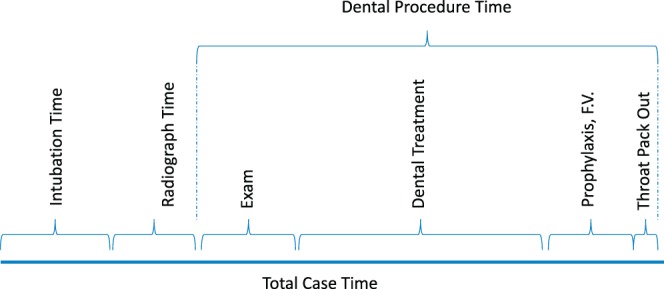
Twenty-six patients were enrolled in this pilot study, 13 in the control (nasotracheal intubation), and 13 in the experimental (orotracheal intubation) groups. The mean intubation time was 2.1 minutes for the orotracheal intubation group (n = 13), and 6.3 minutes for the nasotracheal intubation group (n = 13). T-test and Mann-Whitney U test analysis both revealed significant differences between the groups (p < .01 and p < .01, respectively) (Figure 2).
Figure 2.
Intubation and radiograph time.
The analysis of radiographic time was limited to cases in which 8 radiographs were completed. The film size, number of radiographs taken with the initial series, number of nondiagnostic images exposed, and radiographic technique (conventional versus digital) were documented for each case. The mean radiograph time was not statistically different with t-test analysis at 4.2 minutes for the orotracheal intubation group (n = 8) versus 3.4 minutes for the nasotracheal intubation group (n = 6; p = .144) (Figure 2).
There were no differences in radiographic image quality, and there was no increase in the number of radiographs exposed as a result of intubation technique (radiographic image quality was determined by the need to retake an image).
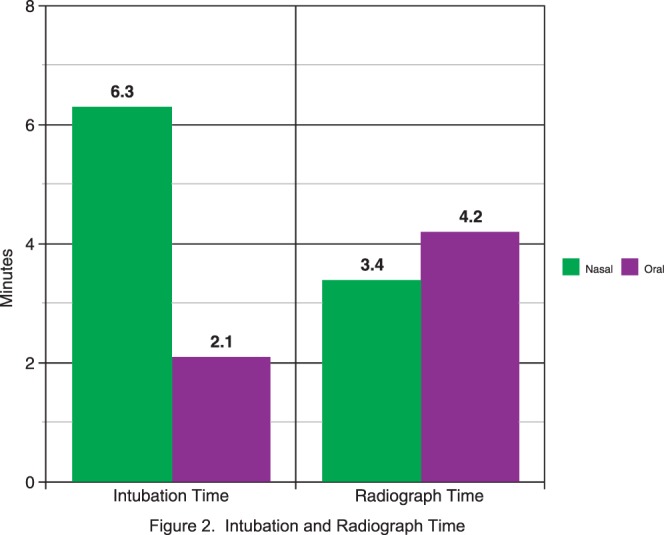
The mean dental procedure time was not significantly different via t-test with 115.9 minutes for the orotracheal intubation group, and 108.5 minutes for the nasotracheal intubation group (p = 0.603; Figure 3). Analysis of dental procedure time using the Mann-Whitney U test analysis did not alter our findings. Analysis of dental procedure time was also completed utilizing RVUs. An RVU was calculated for each case, and cases were placed into 1 of 3 groups based on the RVU and number of teeth treated. In all 3 groups (small, medium, or large), following t-test, there were no significant differences for dental procedure time when completing cases with orotracheal versus nasotracheal intubation.
Figure 3.
Total case and procedure time.
Mean total case time was not significantly different with t-test analysis at 126.6 minutes for the orotracheal intubation cases, and 121.0 minutes for nasotracheal intubation cases (p = 0.695). Analysis of total case time using the Mann-Whitney U test analysis did not alter our findings (Figure 3). Analysis of the total case time was also completed utilizing RVUs. An RVU was calculated for each case, and cases were placed into 1 of 3 groups based on the RVU and number of teeth treated. In all 3 groups (small, medium, or large) following t-test analysis, there were no significant differences for dental procedure time when completing cases with orotracheal versus nasotracheal intubation.
Of the 13 cases completed with orotracheal intubation, only 1 required a second provider to complete the intubation. In contrast, 6 of 13 cases completed with nasotracheal intubation required a second provider to complete the intubation. This difference was found to be significant (p < .01). Fewer intubation attempts were required for the orotracheal (15 total attempts—in 1 instance, intubation was accomplished on a second attempt by the initial provider, a physician anesthesiologist with 10 years' experience; in another case, intubation was accomplished on the first attempt by an emergency medicine physician resident, and the second attempt was by a certified registered nurse anesthetist with 15 years' experience) versus the nasotracheal (22 total attempts) intubation group; this difference was found to be significant (p < .05) (Table).
Secondary Variables
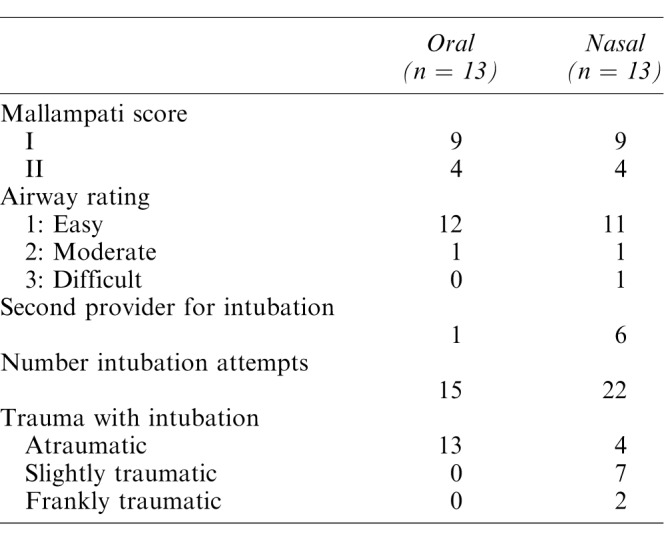
At the completion of the cases, following extubation, the primary anesthesia provider was asked to rate the intubation on a trauma scale. The scale was defined as 1—atraumatic (a bloodless, easy nasal endotracheal intubation), 2—slightly traumatic (presence of blood tinged sputum with suctioning), and 3—frankly traumatic (blood pooling in the oropharynx or nose).2 Orotracheal intubation was rated as significantly less traumatic (p < .01) (Table). Sixty-nine percent of nasotracheal intubations were rated as traumatic (Table), but there were no reports of any negative sequelae the evening of the procedure or at a subsequent follow-up visit.
Our original study protocol did not include tracking data on movement of the orotracheal tube. We assumed we would move the tube from side-to-side, and we did so for some cases, but we found that there were instances where tube movement from side-to-side was not necessary. Once we realized that tube movement from side-to-side may or may not be required, we began documenting whether we moved the tube or not. In 9 orotracheal intubations, data on movement of the orotracheal tube (or lack of movement) were recorded. In 7 of 9 (78%) orotracheal intubation cases, the tube was not moved during the course of treatment.
DISCUSSION
We are well aware that a recommendation to abandon nasotracheal intubation for dental surgery, particularly by anesthesia providers with low nasotracheal intubation case numbers, represents a significant paradigm shift for many dental providers. There were a number of occasions (all nasotracheal intubations) in which there were oxyhemoglobin desaturations during the intubation process, and in some instances, multiple desaturations. On the contrary, as would be expected, the orotracheal intubations were more easily executed even by inexperienced providers (providers with low nasotracheal intubation case numbers, student nurse anesthetists, physician residents). In many training facilities, there is significant anesthesia provider variability, including (physician anesthesiologists, physician and dentist anesthesia residents, certified registered nurse anesthetists, student nurse anesthetists, and nonanesthesia physician and dentist residents), and these types of anesthesia providers (excluding physician and dentist anesthesia residents) were involved in this pilot study. This variability significantly skewed our results. Operator experience in providing dental treatment with an orotracheal tube could have also skewed our results. Prior to this research study, the author (MPN, Diplomate American Board of Pediatric Dentistry) primarily utilized nasotracheal intubation unless there were contraindications to its use, or if anesthesia providers had technical difficulties with the intubation. Since the end of this research project in November of 2015, there has been only 1 instance in which the dental operator (MPN) requested a nasotracheal intubation that was for the treatment of an alveolar bone fracture in the anterior maxilla. After more than 1 year of orotracheal intubations, the dental operator (MPN) has learned how to quickly and efficiently negotiate around an orotracheal tube while providing routine pediatric dental and minor oral surgical procedures, most times without the need to move the tube from 1 side to another.
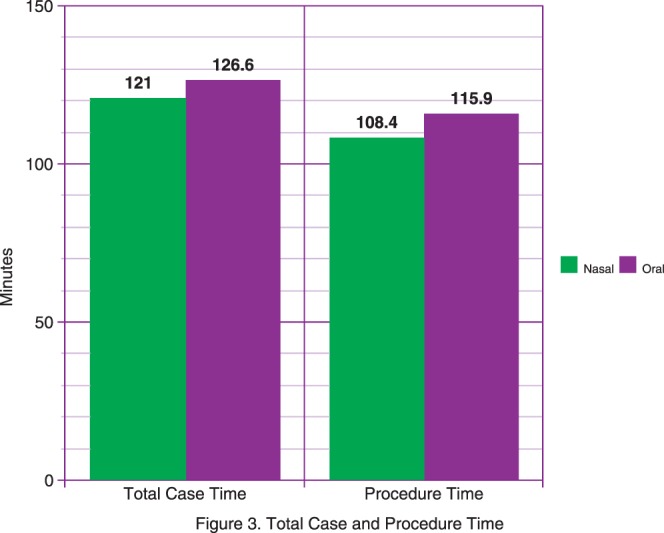
When utilizing orotracheal intubation for pediatric dental services, we typically requested that the tube be positioned on the right side in the commissure of the lip and buccal (lateral) to the maxillary teeth and entering the oropharynx laterally. There is a tendency for anesthesia providers to secure the orotracheal tube with its final position being at the ten o'clock position or higher versus the much preferred nine o'clock position. It is important that the orotracheal tube be secured bilaterally to prevent tube displacement. Because the tube is positioned on the right, it is correct to assume that the most difficult areas to manage are the maxillary right and the maxillary anterior sextants. For the primary and early mixed dentition patients, a winged rubber dam clamp can help position the orotracheal tube out of the operative field. The remaining sextants or quadrants can be treated as you would normally (Figure 4a and b).
Figure 4.
(a) Arrow indicates preferred position. (b) Upper right quadrant isolated.
From an educational standpoint, because nasotracheal intubation is more complex, for those trainees in which anesthesia is not their primary area of study, orotracheal intubation may create more meaningful anesthesia experiences in their training program. For dedicated anesthesia residents, training in nasotracheal intubation is important.
There are patients in which nasotracheal intubation is ill-advised, namely patients with a bleeding disorder, facial dysmorphia, and limited functional residual capacity. As a result, dental providers should become competent at providing high quality dental care in patients intubated with an orotracheal tube.
Weaknesses in the study include the variability in provider experience with nasotracheal intubation, variability in types of provider (physician anesthesiologist vs nurse anesthetist), the addition of anesthesia trainees or providers with variable nasotracheal intubation experience, and the small number of subjects. Additionally, the study did not include highly skilled anesthesia providers at nasotracheal intubation, such as dentist anesthesiologists, for comparison. These data can be used for power analysis in future studies, however.
Based on this study's results, the following conclusions can be made regarding intubation when performed by physician anesthesiologists, nurse anesthetists, and trainees, all with variable nasotracheal intubation experience.
Orotracheal intubation required significantly shorter time than nasotracheal intubation.
Orotracheal intubation required fewer providers and attempts to establish intubation than nasotracheal intubation.
Orotracheal intubation was less traumatic than nasotracheal intubation.
Orotracheal intubation did not significantly increase dental procedure time or total case time.
Orotracheal intubation did not significantly increase radiograph time or affect radiographic image quality.
REFERENCES
- 1. Stoelting RK, Miller RD, . Basics of Anesthesia. 4th ed. New York, NY: Churchill Livingstone; 2000. [Google Scholar]
- 2. Dinner M, Tjew M, Artusio JF, . Bacteremia as a complication of nasotracheal intubation. Anesth Analg. 1987; 66: 460– 462. [DOI] [PubMed] [Google Scholar]
- 3. Stone DJ, Bogdonoff DL, . Airway considerations in the management of patients requiring long- term endotracheal intubation. Anesth Analg. 1992; 74: 276– 287. [DOI] [PubMed] [Google Scholar]