Abstract
Intraoral local anesthesia injection is often perceived as a painful and anxiety-causing dental procedure. Vibration stimulus is one of the nonpharmacologic methods used to reduce unwanted sensations of local anesthesia injection. This clinical study evaluated the effectiveness of a recently introduced vibratory stimulation device in intraoral local anesthesia administration. Thirty-two subjects underwent 2 maxillary local anesthesia injections in 2 different sessions: 1 with conventional techniques and 1 with the aid of a vibratory stimulation device (DentalVibe). The pain levels were evaluated with a visual analog scale and the Wong-Baker FACES Pain Rating Scale. The subjects were asked to choose the preferred method for future injections. The data were evaluated statistically. There were no significant differences between the 2 injection methods with regard to either pain evaluation method. The preference of the subjects regarding future injection technique was evenly distributed between the groups. The vibratory stimulation device used in this study did not provide any reduction in pain level associated with maxillary infiltration local anesthesia administration.
Key Words: Vibratory stimulation, Local anesthesia, Pain, Anxiety
A significant number of patients still perceive administration of local anesthesia as a painful and anxiety-causing dental procedure. Several methods have been described to reduce pain and anxiety caused by local anesthesia administration. These include buffering the local anesthetic, warming the local anesthetic, applying topical anesthesia before injection, reducing injection speed, and using fine needles with electric delivery devices.1 Vibration stimulus is one of the nonpharmacologic methods used to reduce unwanted sensations of local anesthesia injection. It is based on gate control theory, which was proposed by Melzack and Wall in 1965.2 This theory implies that nonpainful input closes the “gates” to painful input, which prevents pain sensation from traveling to the central nervous system. Although the theory has been updated because of advances in neuroscience, the basic concept is still applicable.
Although this scientific theory was established in 1965, a device using vibration inhibition of injection pain was designed by George C. McCann in 1939. It was granted a US patent in 1941.3 Other devices have been designed to be used in conjunction with local anesthesia injection.4,5 The common feature of these devices is the delivery of vibration stimulus to the target area to reduce the pain of injection. Numerous types of these devices have been in the market since those years to be used both for intraoral anesthetic administration and intramuscular drug injection through skin. Despite the long history of this method, the number of the studies concerning the effectiveness of these devices for intraoral use is limited. In this prospective, crossover, clinical study, we aimed to evaluate the feasibility and effectiveness of DentalVibe (Boca Raton, Fla), a vibration device that can also retract and illuminate the target injection area, in intraoral local anesthesia administration. It is a wireless, rechargeable, handheld device that delivers pulsed percussive, tapping vibration to the surrounding mucosa at the injection site (Figure 1).
Figure 1.

Vibratory stimulation device used in the study (DentalVibe, Boca Raton, Fla).
METHODS
Thirty-two volunteers, who were undergraduate dental students at Rangsit University, Faculty of Dental Medicine, were recruited for the study. All participants were in American Society of Anesthesiologists physical status 1 or 2. Participants who had an allergy to any ingredient in the local anesthetic solution used in the study or who had an active infection in the area of injection were excluded. The purpose and method of the study were clearly explained to the participants, and an informed consent form was signed. The study was approved by the Rangsit University Ethical Review Committee (approval document code RSEC-49/2558). The study was conducted in full accordance with the World Medical Association Declaration of Helsinki.
The procedures were performed in the Oral Surgery Clinics at the Faculty of Dental Medicine, Rangsit University. Each participant underwent local anesthesia administration by infiltration technique at the apical region of the right maxillary incisors. Each participant was randomly assigned to 1 of the following injection techniques to be used at the first appointment by randomization: (a) conventional local anesthesia infiltration technique (conventional injection group) or (b) conventional local anesthesia infiltration along with the use of DentalVibe. To distribute randomly the technique used at first injection, the participant drew a paper from the bag on which the name of the technique was written. There were an equal number of conventional injections and DentalVibe-assisted injections at the first appointment. Two weeks after the first injection, the same participant was administrated local anesthesia at the same area as the first injection. Thus, all subjects served as their own control in the study.
Injection Technique
The injection site of choice was the maxillary right incisor region. The anesthetic solution used for the injections was 2% mepivacaine with 1:100,000 epinephrine (Septodont, Cambride, ON, Canada). The anesthetic was injected with an aspiration-type syringe with a 21-mm, 27-gauge needle. The same oral surgeon made all injections. No topical anesthesia was applied prior the injections.
Conventional Method
The lip was retracted with the DentalVibe turned off. The target area was the muccobuccal fold above the right maxillary incisors. The needle was advanced toward the bone, with bone contact avoided as it may cause discomfort. Once it was confirmed that the needle was not within the blood vessel by means of aspiration, 1.0 mL of anesthetic solution was injected over 1 minute. The needle was removed gently after completion of the injection.
DentalVibe-Assisted Injection
A single-use tip was attached to the handheld device, as instructed by the manufacturer. The lip was retracted with the tip of the device. It was activated for 5 seconds prior to the injection. The device remained on during the injection, and thus vibration stimulus was delivered throughout the injection. The injection was then conducted as by the conventional method, with bone contact avoided and the same amount of anesthetic solution used. The device operated for an additional 5 seconds after the removal of the needle, as it may help diffusion of the solution (Figure 2).
Figure 2.
Photograph showing intraoral local anesthesia injection with the aid of a vibratory stimulation device.
Pain Assessment
The pain perceived by the subject was marked on a visual analog scale (VAS). The VAS used in the study was a horizontal line, 100 mm in length, anchored by no pain and worst possible pain at each end. The subject marked where they perceived the pain of injection. A pain score between 0 and 100 mm was obtained for each injection.
The Wong-Baker FACES Pain Rating Scale was used to measure the pain that was perceived by the patient. This scale is a row of 6 faces ranging from very happy to very unhappy (scores ranging between 0 and 10; 10 indicating the highest pain). The subjects chose the face that illustrates the pain that they experienced during the injections.
After the second injection, the subject was asked which technique she or he would prefer if more injections were to be performed in the future. The preferred method was noted.
Statistical Analysis
The sample size of the study was determined based on the power analysis considering important mean difference in VAS scores as 10 mm, standard deviation 0.5 mm for both groups, significance level .05, and power .80 (a priori: compute N, given alpha, power, ES: GPower 3.1, University of Dusseldorf, Germany) The estimate of the difference in VAS score was obtained from the study by Nanitsos et al.6 Data distribution was assessed using the Kolmogorov-Smirnov test. The data did not show normal distribution for the continuous variables. As the data were not normally distributed, the Wilcoxon signed rank test was used for comparisons.
RESULTS
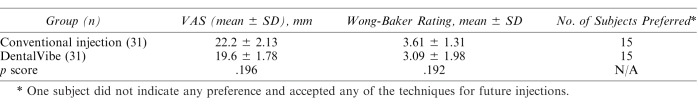
Thirty-one subjects participated in the study. One subject dropped out from the study because of personal reasons. The age of the subjects ranged between 18 and 26 years (mean = 22.2 years) There were 11 men and 20 women. The VAS scores for the conventional injection group ranged between 0 and 62.8 mm (mean = 22.2 ± 2.13 mm), while the scores ranged between 0 and 60.6 mm (mean = 19.6 ± 1.78 mm) for the DentalVibe group. The difference in the VAS scores between the 2 groups was not statistically significant (p = .196).
The mean score of the Wong-Baker FACES Pain Rating Scale was 3.61 ± 1.31 for the conventional injection group, while it was 3.09 ± 1.98 for the DentalVibe group. The difference between the 2 groups was not statistically significant (p = 0.192).
When subjects were asked to indicate their preferred method for future injections, 15 preferred the conventional injection method, 15 preferred injections with the aid of the vibration device, and 1 subject did not indicate any preference (either method accepted). No statistics were applied to this parameter, as the preferred method was equally distributed between the groups. The results of the parameters of the study are presented in the Table.
Results of Mean Visual Analog Scale (VAS) Scores, Wong-Baker Facial Rating Scales (for the Measurement of Pain), and Distribution of Subjects With Regard to Preferred Method for Future Injections
DISCUSSION
In this clinical, prospective, crossover study, we evaluated the effectiveness of a handheld vibratory stimulation device in reducing pain that was caused by intraoral local anesthesia injection. The device used DentalVibe is a recently introduced device that delivers pulsed, percussive micro-oscillations to the site where an injection is being administered. It was developed to stimulate the mechanoreceptors with vibration during the delivery of dental injections.
The philosophy of the mechanism of the vibratory stimulation device is based on the gate control theory. In 1965, Melzack and Wall2 proposed the gate control theory, which suggests that pain experience can be reduced by activating nerve fibers that conduct nonnoxious stimuli. Stimulation of the larger-diameter nonnociceptive mechanoreceptor fibers (massage, vibrations, rubbing, pressure) causes inhibition of afferent painful information mediated via Aδ and C nociceptive fibers.
Although it was assumed almost 80 years ago that vibration stimulus can alleviate injection pain, there are few studies available in the English language to corroborate this. In previous studies, vibration stimulus has been delivered by means of hand or finger movement or specially designed devices. The devices that were designed to deliver vibration stimulus to the target area for intraoral injections can be categorized into 2 types. The devices in the first category vibrate the syringe itself with a vibrating attachment. One of the devices in this segment has been marketed with the trade name Vibraject (Vibraject, LLC, Trabuco Canyon, Ca). The device is a battery-powered vibrating attachment that snaps on to the body of the standard dental syringe. The results of 2 previous studies that evaluated the effectiveness of Vibraject showed that there was no difference in injection pain level between conventional injection and injection with the VibraJect attachment.7,8
The devices in the second category stimulate the target area separately from the syringe. A relatively new device in this category is DentalVibe, which we used in the present study. Although introduced later than Vibraject, more studies have evaluated the efficacy of DentalVibe when compared with VibraJect. The results of these studies were conflicting. Therefore, we decided to conduct the present study. Nasehi et al9 compared the pain level between the conventional method and DentalVibe-assisted method in 99 patients. A total of 256 injections, which consisted of infraorbital nerve blocks, inferior alveolar nerve blocks, palatal injections, and buccal injections, were conducted. The authors demonstrated significant reduction in pain level with the use of DentalVibe. Elbay et al10 studied the efficiency of DentalVibe in pediatric patients. Sixty children between 6 and 12 years of age were administered maxillary or mandibular infiltration anesthesia either with the conventional method or with the assistance of DentalVibe. The study showed that there was no difference between the 2 techniques. A randomized clinical controlled trial by Ching et al11 compared the pain level in maxillary or mandibular infiltration anesthesia in 36 patients between 10 and 17 years of age. The pain level was evaluated using the Wong-Baker FACES Pain Rating Scale. The study showed that the DentalVibe injection system significantly reduces pain associated with infiltration injection of local anesthesia in an adolescent population. Another recent study by Shilpapriya et al12 studied the effectiveness of DentalVibe on 30 patients between the ages of 6 and 12 years using Frankel's behavior scale. The study showed significant reduction in pain level with the use of DentalVibe.
One of the drawbacks of studies that evaluate pain level with different injection systems, including our study, is that the assessment of pain level cannot be made by objective measurement methods. Usually, subjective methods such as marking on a VAS or choosing the corresponding face image that represents the pain level are used. In the present study, we used VAS measurement and the Wong-Baker FACES Pain Rating Scale for comparison of the pain levels between the groups. In addition, we asked the subjects which method they would prefer for future injections if needed. These methods have been commonly used in previous studies for both pediatric and adult patients.10,11,13,14 Since perception of pain is a multifactorial phenomenon, as clinicians we must accept the patient's description of pain level. Thus, despite the subjective nature of these assessment methods, their current use is accepted as appropriate for pain evaluation.
The present study indicates that the vibratory unit used in this study does not provide any reduction in injection pain when compared with a conventional injection method. All parameters failed to show any difference between the 2 groups. The subjects who disliked the vibration technique usually mentioned that the vibration itself caused discomfort. In addition, the noise that the unit generates also created some unwanted effect during the injection.
One drawback of our study was that we used volunteer dental students as study subjects instead of actual patients. The subjects were from a relatively similar age group and sociocultural background. Actual patients were not used because of the decision of the ethical review committee. The results might have been different if the subjects were recruited from a more diverse patient population. Another drawback of the study is that the subjects were not blind to the technique, as it was obvious which injection the device was turned on. Therefore, they may have been influenced by their perceived anxiety about the pain of the injection. To maximize the similarity of 2 techniques, we used the device in the conventional injection group for lip retraction without turning it on.
CONCLUSION
The DentalVibe vibratory device did not provide any reduction in perceived pain level associated with maxillary anterior infiltration local anesthetic administration.
ACKNOWLEDGMENTS
We would like to express our sincere thanks to Laongthong Vajrabhaya Chommaiporn Nopparathirun, Thunsinee Ronnarongsenee, Papitchaya Vangtal, Papon Pattanasirikun, and Charurin Boonwan for their precious help and support to conduct this study. The authors of the study declare that they do not have a conflict of interest. This study was funded by the Research Institute of Rangsit University (grant RSEC-49/2558).
REFERENCES
- 1. Ogle OE, Mahjoubi G, . Advances in local anesthesia in dentistry. Dent Clin North Am. 2011; 55: 481– 499. [DOI] [PubMed] [Google Scholar]
- 2. Melzack R, Wall PD, . Pain mechanisms: a new theory. Science. 1965; 150: 971– 979. [DOI] [PubMed] [Google Scholar]
- 3. McCann GC, . Mechanical distraction method and device. US Patent 2,258,857. October 14, 1941.
- 4. Branford WG, . Vibratory dental mouthpiece. US Patent 5,030,098. July 9, 1991.
- 5. Kravits H, . Device for reducing the pain of injections of medicines and other biological. US Patent 3,620,209. November 16, 1971.
- 6. Nanitsos E, Vartuli R, Forte A, Dennison PJ, Peck CC, . The effect of vibration on pain during local anaesthesia injections. Aust Dent J. 2009; 54: 94– 100. [DOI] [PubMed] [Google Scholar]
- 7. Roeber B, Wallace DP, Rothe V, Salama F, Allen KD, . Evaluation of the effects of the VibraJect attachment on pain in children receiving local anesthesia. Pediatr Dent. 2011; 33: 46– 50. [PubMed] [Google Scholar]
- 8. Saijo M, Ito E, Ichinohe T, Kaneko Y, . Lack of pain reduction by a vibrating local anesthetic attachment: a pilot study. Anesth Prog. 2005; 52: 62– 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nasehi A, Bhardwaj S, Kamath AT, Gadicherla S, Pentapati KC, . Clinical pain evaluation with intraoral vibration device during local anesthetic injections. J Clin Exp Dent. 2015; 17: e23– e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Elbay ÜS, Elbay M, Yıldırım S, Kaya E, Kaya C, . Evaluation of the injection pain with the use of DentalVibe injection system during supraperiosteal anaesthesia in children: a randomised clinical trial. Int J Paediatr Dent. 2016; 26: 336– 345. [DOI] [PubMed] [Google Scholar]
- 11. Ching D, Finkelman M, Loo CY, . Effect of the DentalVibe injection system on pain during local anesthesia injections in adolescent patients. Pediatr Dent. 2014; 36: 51– 55. [PubMed] [Google Scholar]
- 12. Shilpapriya M, Jayanthi M, Reddy VN, Sakthivel R, Selvaraju G, Vijayakumar P, . Effectiveness of new vibration delivery system on pain associated with injection of local anesthesia in children. J Indian Soc Pedod Prev Dent. 2015; 33: 173– 176. [DOI] [PubMed] [Google Scholar]
- 13. Ga H, Koh HJ, Choi JH, Kim CH, . Intramuscular and nerve root stimulation vs lidocaine injection to trigger points in myofascial pain syndrome. J Rehabil Med. 2007; 39: 374– 378. [DOI] [PubMed] [Google Scholar]
- 14. Kudo M, . Initial injection pressure for dental local anesthesia: effects on pain and anxiety. Anesth Prog. 2005; 52: 95– 101. [DOI] [PMC free article] [PubMed] [Google Scholar]