Life expectancy in England and Wales has stalled. At some older ages, it is declining. One of the most widely used measures of the health of the population, life expectancy is calculated from age-specific death rates. Life expectancy at birth in high-income countries has been improving steadily, albeit with some small fluctuations, for decades. If the data are accurate, in the absence of other causative factors – endemic disease, environmental event such as war or natural disaster, or mass migration – stagnation of life expectancy, or worse still, decline, suggests substantial societal problems. This possibility is not, however, supported by the Government, which rejects any suggestion that its policies, in particular austerity and its effects, might have played any causal role in the observed trends.
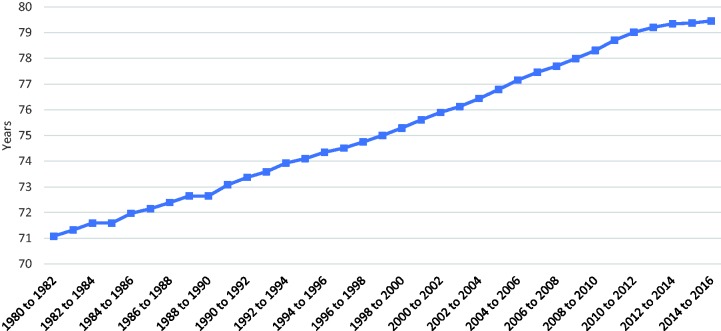
First, it is necessary to describe what has been happening. Data from the Office for National Statistics (Figure 1) show trends in life expectancy at birth from 1980 to 2016 in England and Wales. After 2010, there is a clear slowdown in the rate of improvement. As this has coincided with the imposition of austerity measures by the coalition government elected in that year, this has inevitably raised questions of whether there might be a causal link. In particular, while spending on health and social care continued to grow year-on-year, annual percentage increases were much less than before,1 especially affecting general practice, the main setting for care of most people with chronic diseases. It has experienced a declining share of the NHS budget,2 widespread closures of general practices, unfilled staff vacancies and growing problems of access.3
Figure 1.
Trends in life expectancy at birth, England and Wales, 1980–present (Source: Office for National Statistics).
There is a growing literature suggesting a link between austerity and slowing of improvements in life expectancy at birth, and in some cases actual increases in death rates in older people.4 Some of these have invoked inadequate spending on health and social care.5–11 Yet, others reject this argument, citing alternative explanations such as unknown infectious agents,12 cold weather and influenza.13,14 Others have noted the challenges of interpreting short-term trends and urged caution in inferring causality from an observed association.15,16 In a recent debate on life expectancy and austerity that cited extensively our previous research, Conservative Members of Parliament focused on three main arguments.17 First, as Robert Court MP (Conservative, Witney) said in the debate, ‘life expectancy cannot be expected to increase forever’. Second, slowdowns in the rate of improvement have been seen in some other European countries. Third, the situation is complex and it is not possible to attribute any changes to a single cause. The first point is undoubtedly true but ignores how the United Kingdom has some way to go to reach the level seen in the best performing countries, such as Norway and Sweden, where life expectancy at birth is over a year longer. The second is also true, but other countries have also experienced reductions in social expenditure. Thus, according to OECD data, between 2010 and 2016 it fell, as a percentage of Gross Domestic Product in the United Kingdom from 22.8% to 21.5% and in Germany from 25.9% to 25.3%. In contrast, it increased from 26.3% to 27.1% in Sweden.18 The third point was that the situation is complex and it is difficult to ascertain causality, which we explore here. As Mr Court also said,
‘It is simplistic to look at a straightforward line between necessary control of public spending and an impact on life expectancy. As we have heard, a whole range of factors affect life expectancy and mortality—quality of life, mental health, obesity, housing, air quality—and simply to draw that straightforward causation line is to make things far too simple.’
Jackie Doyle-Price, Under-Secretary of State for Health, argued that ‘We need to be circumspect about drawing too much by way of conclusion’.
It is obvious that the situation is complex and multiple factors are bound to play a role, including both cohort and period effects, some of which have been explored in our previous research in which we examined trends in deaths at different ages and from different causes. Complexity does not prevent factors that have contributed to what is observed being elucidated. It is, however, the issue of causality that we now examine. Correlation does not always imply causation: an association between two events does not mean that one causes the other. So, when and how might we be able to say that one thing causes another? Without a randomised controlled trial, the ‘gold standard’ method in medicine for establishing causality, how can we refute or confirm the association?
Clearly, a randomised controlled trial is not possible. It would require two groups of people, equal in all other ways except that one would be assigned, at random, to living through austerity measures. The closest natural experiment involves comparison with other countries in Europe that have made different policy choices. Thus, as noted above, in the Nordic countries, life expectancy continues to rise at a steady rate. However, there are too many differences between these countries and England and Wales to make a fair comparison.
In 1965, Sir Austin Bradford Hill proposed nine ‘viewpoints’ to be considered before invoking causality.19 Drawing on both empirical and rational traditions, the Bradford Hill criteria are: strength of association, consistency, specificity, temporality, biological gradient, plausibility, coherence, experiment and analogy. Here, we apply these in turn to what is known about the recent changes in life expectancy.
Some are easily met. Coherence (‘… interpretation should not seriously conflict with generally known facts of the natural history and biology of the disease’), plausibility (is there a plausible mechanism between cause and effect?) and consistency (‘has it been repeatedly observed by different persons, in different places, circumstances and times?’) can be demonstrated by reference to a now extensive body of research on the impact of financial crises on health, albeit recognising that these associations are complex, including some causes of death (traffic injuries) that do fall.20 The consequences of weakened health systems were apparent in an admittedly extreme example, the collapse of the Soviet Union,21 although the adverse effects of economic hardship can also be seen today in the USA22 and in Greece, which has experienced a marked slowing in the rate of decline from some causes of death and an actual increase in others, such as those amenable to healthcare.23 The converse is seen, with evidence that well-functioning health systems are associated with declining mortality. Temporality, another of Bradford Hill’s criteria,24 is also clear: the imposition of cuts precedes the decline and stalling in life expectancy. The others are less straightforward.
Biological gradient refers to a situation whereby increasing exposure (cuts) leads to worse outcomes (death). This is more difficult to assess, although the scale of pension cuts at the level of local authorities has been linked to differences in early mortality.25 However, other research has found increases in elderly mortality in all areas – poor and affluent.10 This does not exclude the link, but neither does it establish it. Specificity of effect is difficult to establish, but the older population are more dependent on a well-functioning health and social care system, and are the group that have seen the increases in deaths, with corresponding declines in life expectancy at older ages.6 Assessing the strength of the association is more difficult when there is no obvious alternative exposure with which to compare austerity, a problem that is well recognised in the epidemiological literature.26
Concluding his nine viewpoints, Bradford Hill highlights that none of them provide ‘indisputable evidence’, but they help answer the fundamental question: ‘is there any other way of explaining the set of facts before us, is there any other answer equally, or more, likely than cause and effect?’19 To date, no alternative to austerity has been established as the reason for the stalling life expectancy.
Unlike in the physical sciences, establishing causality in epidemiology is complex. Newton’s insights to generate the laws of motion were brilliant, but technically easy to demonstrate. With complex human systems, such as populations, one needs to exclude chance, bias in all its forms and confounding. Thus, few conclusions can ever be definitive. However, as data from across Europe for the year 2016 are released soon, and then for 2017 (12 months after that), it will become increasingly clear whether the UK and other countries that have chosen extreme austerity have become significant outliers – or not.
Health is determined by far more than healthcare. The social determinants of health – the conditions in which we are born, live, work, grown and play27 – all impact the health of the population, and, in turn, are all impacted on by austerity. Yet, each time it has been raised, the Department for Health and Social Care has been dismissive at best. Carrying on as normal without understanding what has caused this decline prevents any measures being taken to halt it. As the evidence builds to suggest a link between cuts and stalling life expectancy, and lacking evidence of an alternative cause, it must be taken seriously and investigated thoroughly.
Declarations
Competing Interests
DD and MM sit on Public Health England's mortality advisory committee.
Funding
None declared.
Ethics approval
Not applicable
Guarantor
LH
Contributorship
LH wrote the initial draft which DD and MM edited and revised.
Acknowledgements
None.
Provenance
Not commissioned; peer-reviewed by Azeem Majeed.
References
- 1.Full Fact Team. Spending on the NHS in England 2017. See https://fullfact.org/health/spending-english-nhs/ (last checked 28 December 2017).
- 2.Majeed A. Primary care: a fading jewel in the NHS crown. London J Prim Care 2015; 7: 89–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Majeed A. Shortage of general practitioners in the NHS. BMJ 2017; 358: j3191–j3191. [DOI] [PubMed] [Google Scholar]
- 4.Hiam L, Harrison D, McKee M, Dorling D. Why is life expectancy in England and Wales ‘stalling’? J Epidemiol Community Health 2018; 72: 404–408. [DOI] [PubMed] [Google Scholar]
- 5.Hiam L, Dorling D, Harrison D, McKee M. What caused the spike in mortality in England and Wales in January 2015? J R Soc Med 2017; 110: 131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hiam L, Dorling D, Harrison D, McKee M. Why has mortality in England and Wales been increasing? An iterative demographic analysis. J R Soc Med 2017; 110: 153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watkins J, Wulaningsih W, Da Zhou C, Marshall DC, Sylianteng GDC, Dela Rosa PG, et al. Effects of health and social care spending constraints on mortality in England: a time trend analysis. BMJ Open 2017; 7: e017722–e017722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institue of Health Equity. Marmot indicators briefing 2017. See www.instituteofhealthequity.org/file-manager/MarmotIndicators2017/marmot-indicators-briefing-18-july-2017-updated-.pdf (last checked 27 July 2017).
- 9.Fransham M, Dorling D. Have mortality improvements stalled in England? BMJ 2017; 357: j1946–j1946. [DOI] [PubMed] [Google Scholar]
- 10.Green M, Dorling D, Minton J. The Geography of a rapid rise in elderly mortality in England and Wales, 2014-15. Health Place 2017; 44: 77–85. [DOI] [PubMed] [Google Scholar]
- 11.Green MA, Dorling D, Minton J, Pickett KE. Could the rise in mortality rates since 2015 be explained by changes in the number of delayed discharges of NHS patients? J Epidemiol Community Health 2017; 71: 1068–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones RP. Essays on rising mortality in England and Wales – a MEDLINE search is not infallible. J R Soc Med 2017; 110: 224–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Office for National Statistics. Spike in number of deaths in 2015 driven by increased mortality in over 75s. See www.ons.gov.uk (2016, last checked 10 May 2018).
- 14.Newton J, Baker A, Fitzpatrick J and Ege F. What’s happening with mortality rates in England? Public Health Matters. See gov.uk (2017, last checked 10 May 2018).
- 15.Raleigh V. Why have improvements in mortality slowed down? London: The King's Fund, 2017.
- 16.Science Media Centre. Expert reaction to paper on health and social care spending and excess deaths in England, 2017.
- 17.Hansard. Austerity: life expectancy 2018. See https://hansard.parliament.uk/commons/2018-04-18/debates/6AEE73CE-7C3C-4DC0-A8EB-DA7FE45A34EE/AusterityLifeExpectancy (last checked 2 May 2018).
- 18.OECD. OECD.Stat 2018. See http://stats.oecd.org/ (last checked 2 May 2018).
- 19.Bradford Hill A. The environment and disease: association or causation? Proc R Soc Med 1965; 58: 295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karanikolos M, Mladovsky P, Cylus J, Thomson S, Basu S, Stuckler D, et al. Financial crisis, austerity, and health in Europe. Lancet 2013; 381: 1323–1331. [DOI] [PubMed] [Google Scholar]
- 21.Eberstadt N. The health crisis in the USSR. New York Rev Books 1981; 28: 23–31. [Google Scholar]
- 22.Nosrati E, Ash M, Marmot M, McKee M, King LP. The association between income and life expectancy revisited: deindustrialization, incarceration and the widening health gap. Int J Epidemiol Epub ahead of print 22 November 2017. doi: 10.1093/ije/dyx243. [DOI] [PubMed] [Google Scholar]
- 23.Laliotis I, Ioannidis JPA, Stavropoulou C. Total and cause-specific mortality before and after the onset of the Greek economic crisis: an interrupted time-series analysis. Lancet Public Health 2016; 1: e56–e65. [DOI] [PubMed] [Google Scholar]
- 24.GBD 2015 Healthcare Access and Quality Collaborators. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet 2017; 390: 231–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loopstra R, McKee M, Katikireddi SV, Taylor-Robinson D, Barr B, Stuckler D. Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007–2013. J R Soc Med 2016; 109: 109–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fedak KM, Bernal A, Capshaw ZA, Gross S. Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology. Emerg Themes Epidemiol 2015; 12: 14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marmot M, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives, London: Institute of Health Equity, 2010. [Google Scholar]