Abstract
Study Design:
Questionnaire.
Objectives:
Iatrogenic dural tear is a complication of spinal surgery with significant morbidity and cost to the health care system. The optimal management is unclear, and therefore we aimed to survey current practices among Canadian practitioners.
Methods:
A questionnaire was administered to members of the Canadian Neurological Surgical Society designed to explore methods of closure of iatrogenic durotomy.
Results:
Spinal surgeons were surveyed anonymously with a 55% response rate (n = 91). For pinhole-sized tears, there is no agreement in the methods of closure, with a trend toward sealant fixation (36.7%). Medium- and large-sized tears are predominantly closed with sutures and sealant (67% and 80%, respectively). Anterior tears are managed without primary closure (40.2%), or using sealant alone (48%). Posterior tears are treated with a combination of sutures and sealant (73.8%). Nerve root tears are treated with either sealant alone (50%), or sutures and sealant (37.8%). Tisseal is the preferred sealant (79.7%) over alternatives. With the exception of pin-hole sized tears (39.5%) most respondents recommended bed rest for at least 24 hours in the setting of medium (73.2%) and large (89.1%) dural tears.
Conclusions:
This study elucidates the areas of uncertainty with regard to iatrogenic dural tear management. There is disagreement regarding management of anterior and nerve root tears, pinhole-sized tears in any location of the spine, and whether patients should be admitted to hospital or should be on bed rest following a pinhole-sized dural tear. There is a need for a robust comparative research study of dural repair strategies.
Keywords: dural tear, durotomy, spinal surgery, lumbar surgery
Introduction
Iatrogenic durotomy is a complication of spinal surgery which may reach as high as seventeen percent.1–5 The risk factors for this complication include revision surgery, decompression for spinal stenosis, increasing age, ossified ligamentum flavum or posterior longitudinal ligament, and higher body mass index.1–2,6 The reported incidence is overall lower in younger populations with highest rates seen in those with revision surgery,1 whereas in older cohorts the incidence is relatively higher with the most important risk factors being age, revision surgery, ossification of ligaments, and the type of procedure (ie, multilevel decompression).2
A leak of cerebrospinal fluid (CSF) may complicate the postoperative period with headaches, nausea, vomiting, back pain, abducens nerve palsy, fistula formation, pseudomeningocoele, surgical site infections, meningitis, and in rare circumstances, chronic subdural hematomas.1,5,7–10 This may lead to a significant burden on health care systems, with an estimated 4000-dollar cost per dural tear in the United States.11
Dural tears range in size from pinpoint holes to lesions measuring centimeters in length12 and controversy exists as to the best method of primary repair. Sutures remain the gold standard1; however, fascia or fat patch, different brands of fibrin glue, and alternative sealants are described in the literature.13–15 Some authors recommend primary repair with sutures along with biologic augmentation using fibrin analogues,1 which is shown to reduce risk of persistent CSF leak.16,17 Lumbar drains placed proximal to the durotomy may reduce hydrostatic pressure on the leak allowing it to heal with varying success.18 Postoperative bed rest is thought to reduce hydrostatic pressure,6 thereby reducing CSF leaks; although, the efficacy of this intervention is not clearly demonstrated.19 Intuitively, one would expect Trendelenburg bed position to reduce this pressure and improve the risk of CSF leaks; while anecdotally described,14 there is no research to support this intervention. The duration of recommended bed rest also remains controversial.12,14,20 While it offers a theoretical benefit, bed rest may potentially add the risk of medical comorbidities such as deep vein thrombosis and pneumonia21 and adds significant costs to health care systems.11
With the multitude of controversies in the management of dural tears, the present study aims to establish the current practice patterns among spinal surgeons in Canada. A questionnaire is used to assess the management of dural tears in relation to position and size of the tear. In addition, this study assesses Canadian preferences for sealant augmentation and recommendations for postoperative bed rest and hospital admission requirements.
Methods
A 10-question survey was developed by 2 of the authors (K.R. and M.A.) with input from members of the Division of Neurosurgery at McMaster University. The survey was administered anonymously online via www.surveymonkey.com to all practicing members of the Canadian Neurological Surgical Society (CNSS). Results were extracted to SPSS (2015) statistical software package for analyses using chi-square tests with Bonferroni correction.
Results
Demographic Information
A total of 165 surveys were administered with 91 respondents. Multiple email reminders were sent to potential participants. All demographic information is presented in Table 1. The majority (76.9%) did not have formal spinal fellowship training. A minority of respondents (13.2%) were in practice for less than 3 years, 38.5% were in practice for 3 to 15 years, and 48.4% of respondents were in practice for more than 15 years. The majority of respondents (94.4%) routinely performed spinal surgery, while the remaining 5.6% did not. Most participants, 80.9% performed open procedures routinely while 19.1% practiced minimally invasive tubular surgery. Residents and fellows were not surveyed. Orthopedic spine surgeons were not surveyed as a list of contact information for this group was not available.
Table 1.
Demographic Information of Respondents.
| Demographic Variable | Percentage of Respondents |
|---|---|
| Formal spinal fellowship training | 23.1 |
| Practicing for less than 3 years | 13.2 |
| Practicing for 3-15 years | 38.5 |
| Practicing for more than 15 years | 48.4 |
| Routinely performed spinal surgery | 94.4 |
| Performed mostly open procedures | 80.9 |
| Performed mostly minimally invasive surgery | 19.1 |
Size of Dural Tear
The preferred method for repair was divided arbitrarily by the size of dural tear, with pinhole tears defined as less than 1 mm, medium-sized tears defined as 1 mm to 1 cm, and large tears greater than 1 cm. For pinhole tears 22.9% did not close the tear, 18.4% used sutures, 36.7% used sealant, and 21.8% used sutures and sealant (P = .04). For medium-sized tears, no respondents selected “no primary repair,” 24.7% selected sutures, 8.2% used a sealant, and 67% use both sutures and sealant (P < .001). For large tears, none of the respondents selected “no repair,” 15.4% used sutures, 3.5% used sealant, and 80% use both sutures and sealant (P < .01). The information is presented graphically in Figure 1.
Figure 1.
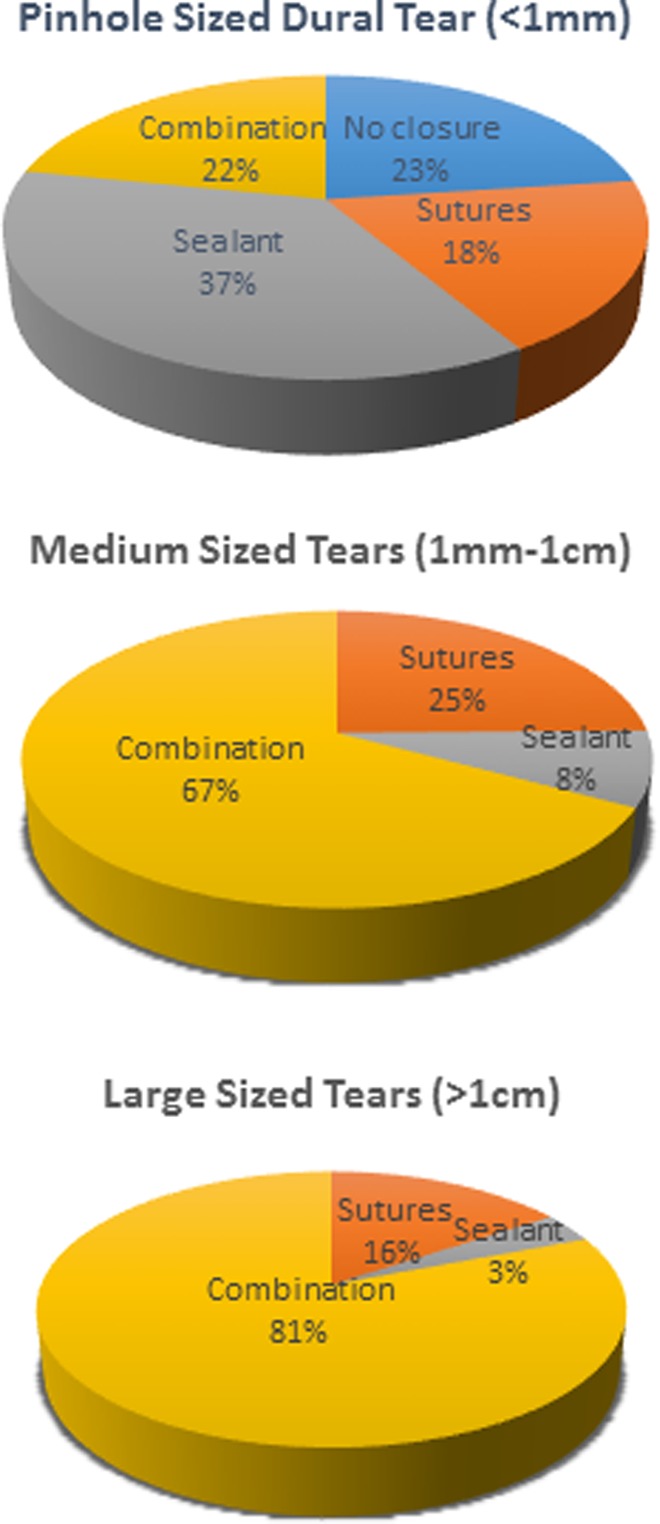
Graphical representation of preferred method of closure for pinhole, medium, and large dural tears.
Location of Dural Tear
Respondents were questioned regarding anterior, posterior, and nerve root tears along with the preferred method of repair. For anterior tears, 40.2% did not attempt closure, 1.2% used sutures, 48.0% used sealant, and 10.3% used both sutures and sealant (P < .001). In post hoc analyses, there are no differences between “no closure” and sealant-only closure, both of which are preferred over other methods (P < .001). For posterior dural tears, 1.1% did not attempt closure, 17.8% used sutures, 7.1% used sealant, and 73.8% used both sutures and sealant (P < .001) with combination therapy preferred over alternative methods. For nerve root tears 10.9% did not close the tear, 4.8% used sutures, 50.0% used sealant, and 37.8% used both sutures and sealant (P < .001). In post hoc analyses, there are no differences between sealant and combination treatment, both of which are preferred over other methods (P < .001). The results are presented graphically in Figure 2.
Figure 2.
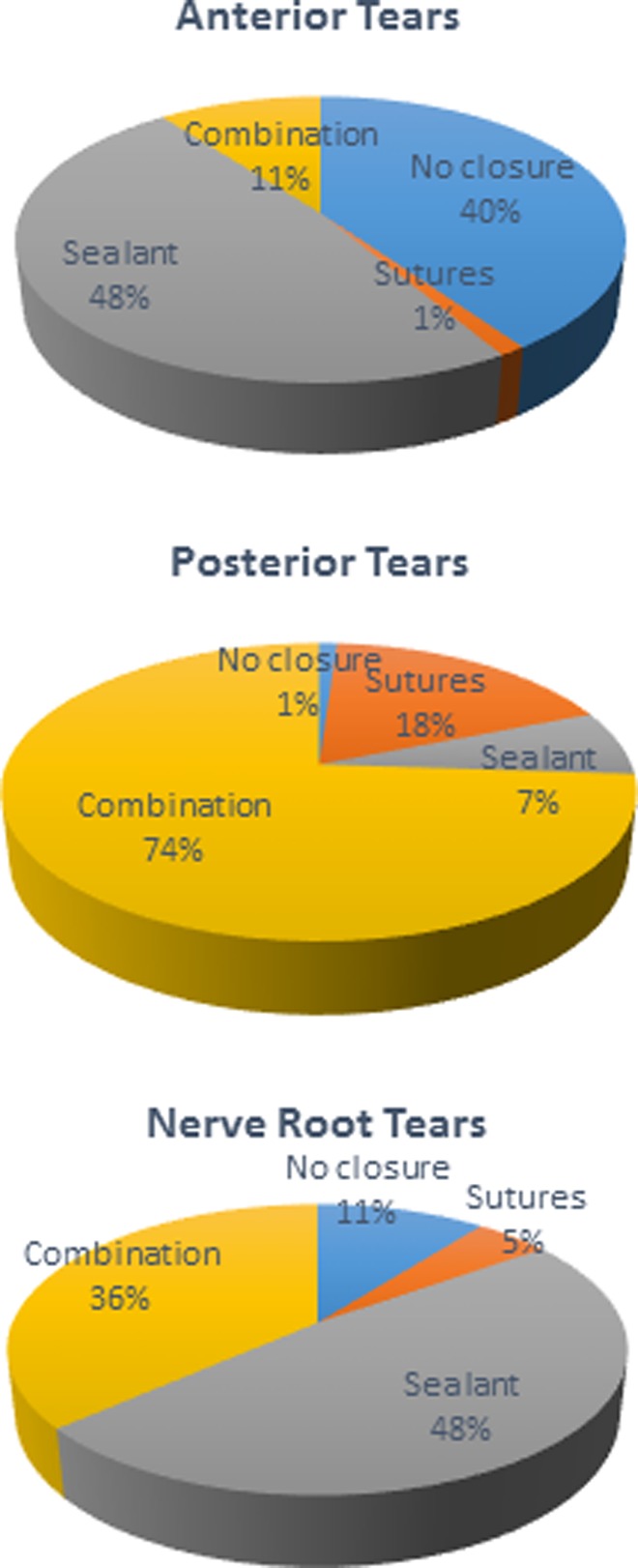
Graphical representation of location of dural tears and preferred method for primary repair.
Type of Sealant
Regarding the preferred type of sealant, most surgeons used Tisseel (Baxter Healthcare Corporation) (79.7%), followed by DuraSeal (Integra Life Sciences) (11.4%), Evicel (Ethicon) (3.3%), and the remainder had no preference (P < .01) (Figure 3).
Figure 3.
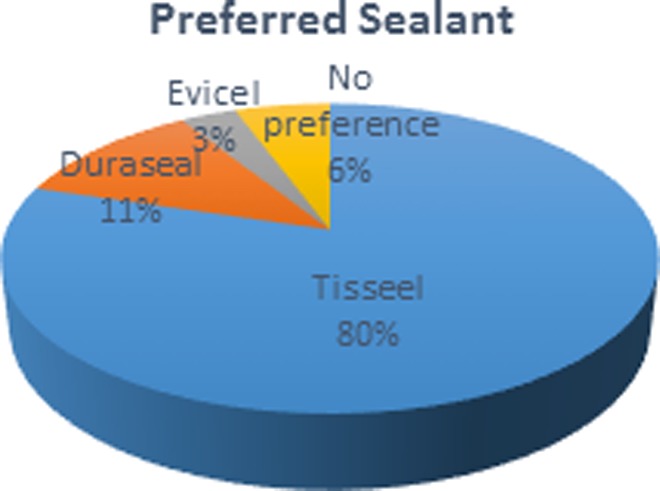
Graphical representation of preferred sealants.
Postoperative Bed Rest for Dural Tears
Postoperative management with bed rest was questioned in relation to the size of the dural tear. For pinhole tears, 55.8% of respondents had no postoperative bed rest orders while 42.8% recommended bed rest (P = .22). For medium-sized dural tears, 23.8% had no specific bed rest orders while 69.1% recommended 24 hours of rest (P < .001). For large dural tears, 16.4% did not recommend postoperative bed rest while 79.7% recommended bed rest (P < .001). All participants recommended between 24 and 48 hours of bed rest.
Postoperative Admission by Presence and Size of Tear
Surgeons were questioned whether admission to a hospital bed is required based on the presence and size of dural tears. In the presence of an unrepaired dural tear, 80% of respondents believed an admission to hospital is warranted (P < .001). In the setting of a repaired dural tear, 70% of respondents admit the patient to hospital (P < .001). For pinhole-sized tears specifically, 39.5% of respondents believed a ward bed was warranted while 60.5% did not (P = .05). Admission to hospital is supported by the majority of respondents when questioned about medium-sized (73.2%) and large-sized (89.1%) tears (P < .001).
Discussion
Dural tear is a complication of spinal surgery with rates as high as 17% in the available literature.1–3 There are numerous complications that may result, including headaches, nausea, vomiting, persistent back pain, abducens nerve palsy, CSF fistula formation, pseudomeningocoele development, and increased rates of infection.1,5,7–10 These in turn have significant associated expenses and can be associated with multiple revision surgeries.11 While it is agreed that recognition of the dural tear is critical, the method of primary repair is controversial ranging from no treatment, sutures, sealants, and combinations of these treatments. The present study questioned 91 practicing spinal neurosurgeons in Canada to establish practices based on size and location of dural tears, as well as postoperative management. This is the first Canadian survey on this topic.
While the majority of respondents did not have spinal fellowships, most were in practice for more than 15 years and routinely performed spinal surgeries. The majority of respondents performed open surgery, which may bias the results toward suture or combination suture and sealant fixation. All respondents of this survey were neurosurgeons, and without orthopedic spinal representation in this sample, it is possible that practices vary between specialties, which is a limitation of the current study.
Our results indicate that the greatest area of controversy lies within the management of primary repair of pinhole sized tears. In this study, there is a trend toward the use of sealant alone. With regard to anterior tears, disagreement exists as to whether sealant closure or “no closure” is the best option. Both of these options are preferred over suture fixation or combination therapy of the anterior spine, likely representing the complexity and technical difficulty of closing these leaks. Large anterior tears may be amenable to transdural closure although this is not reflected in our data as few selected suture repair. In the analyses of nerve root tears, there is no preference for sealant compared to combination therapy. While combination therapy is likely preferred, there is added complexity to suturing these leaks as well. Use of magnification (eg, microscope/endoscope) or tubular retractors with laminectomies may influence the nature of nerve root closure; however, this question is beyond the scope of the administered questionnaire.
A significant agreement among respondents were for medium- and large-sized tear repairs, as well as posterior tears, where the majority of participants prefer combination closure with suture and sealant. While the vast majority of surgeons across Canada support an admission to hospital and bed rest in the setting of dural tear, there is less agreement with regard to pinhole-sized tears. The majority of respondents preferred Tisseal over Duraseal, or “other” sealants likely because of practical as well as cost-related factors.
The largest questionnaire to date examining management of iatrogenic durotomy is a European study from 2014.14 Of 175 respondents across Switzerland, Germany, and Austria, 19% only recommended bed rest, and 84% recommended closure. Our data supports comparable figures only for pinhole-sized tears. Of the larger tears, zero respondents supported “no closure” and bed rest indicating a potential difference between the Canadian and European practices. Examining this difference further is difficult as the authors did not separate analyses by the size of durotomy. Of the types of fixation, 69% incorporated a single suture, 26% utilizing a running suture, and the remainder of respondents using combinations of these with fibrin glues, fat or muscle patches, and lumbar drains.14 These responses do not separate preferred management by dural tear size or location so developing future research questions with this information is difficult.
Regardless of size of dural tear and method of repair, one multicenter review suggests that effective repair of cervical durotomy results in no clinical sequelae in 93% of patients while the remainder required some form of revision related to CSF leakage.22 In one series. patients were treated with suture fixation, fibrin glue augmentation, epidural drains, and postoperative bed rest, with successful management in 98.6% of patients.23 Currently, there is no clinical data that teases apart the efficacy of each strategy and their combinations. One study reviewing 69 dural tears comparing the use of suture fixation alone, to muscle/fat patches and combination therapy found no differences in rates of revision surgery, hospitalization time, or clinical outcomes.24 Requirements for revision surgery instead were related to higher body mass indices.24
Protocols for management of dural tears have been proposed25 where repairable dural tears are managed with suture fixation as well as fibrin glues and then checked with a Valsalva maneuver. If the repair required tight suture fixation these authors recommendation placement of a drain without suction and removal at 48 hours. Nontight suture fixation allows for bed rest alone and a stand-up test at 48 hours, which if tolerated can be followed with magnetic resonance imaging at 6 months and if not tolerated should prompt surgical revision. In this algorithm, nonrepairable dural tears should be treated with bed rest alone for 48 hours followed by the stand-up test.25 This algorithm may be criticized as the body of literature supporting each intervention is sparse, and it does not take into consideration size and location of dural tears. While applying this management strategy may result in a low rate of revision surgery, this may not be necessary in all scenarios. As the present study demonstrates, clinical practice varies widely depending on the size and location of durotomy, and in the Canadian health care system, dural drains are not routine practice.
There are multiple strengths and limitations to this study. The survey was developed by experienced neurosurgeons with an acceptable response rate to adequately elucidate the areas of uncertainty in the management of dural tears. In contrast to previous questionnaires on this topic, this study separates the type of fixation by location and size of durotomy, a critical step in developing future research for this topic. Nonetheless, there are several limitations. This survey has limited sampling, partly because the orthopedic spine surgeons were not involved in the study. Desirable as it is, unfortunately we were unable administer the survey to the orthopedic spine surgeons.
It is also limited to Canadian practice and therefore may not be generalizable to other populations. As with any study involving a survey, the questions rely on memory with no ability of the researchers to validate the accuracy of responses. While the questions reported in this survey help identify areas of uncertainty, we are ultimately unable to determine the best types of closure for various types of dural tears as we do not have individual patient data with follow-up.
Conclusion
This study used a 10-item questionnaire to survey Canadian spinal surgeons regarding the most controversial aspects of dural tear management. The main area of uncertainty identified is the management of pinhole tears. Medium- and large-sized dural tears are predominantly repaired with combinations of sutures and sealants, and respondents agree that generally some period of bed rest is recommended along with admission to hospital. However, As the size of the tear decreases, there is less agreement on the best management, with results trending toward “no repair” or sealant-only fixation for pinhole tears. Postoperative bed rest recommendations are less clear with pinhole-sized tears, as are requirements for admission to hospital. The majority of respondents avoid both for smaller dural tears. Closure of anterior tears and nerve root tears are controversial as well with less agreement between surgeons on the management of these complications. Future research directions in this field include the suitability of various types of closure for various types of leaks, the efficacy of closure, and how it relates to the size of the leak along with the need for bed rest postoperatively. Cost-benefit analyses of various strategies would also be extremely useful given the burden on health care systems, which may be especially important in the case of pinhole-sized tears.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Cammisa FP, Jr, Girardi FP, Sangani PK, Parvataneni HK, Cadag S, Sandhu HS. Incidental durotomy in spine surgery. Spine (Phila Pa 1976). 2000;25:2663–2667. [DOI] [PubMed] [Google Scholar]
- 2. Epstein NE. The frequency and etiology of intraoperative dural tears in 110 predominantly geriatric patients undergoing multilevel laminectomy with noninstrumented fusions. J Spinal Disord Tech. 2007;20:380–386. [DOI] [PubMed] [Google Scholar]
- 3. Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976). 1996;21:626–633. [DOI] [PubMed] [Google Scholar]
- 4. Goodkin R, Laska LL. Unintended “incidental” durotomy during surgery of the lumbar spine: medicolegal implications. Surg Neurol. 1995;43:4–12. [DOI] [PubMed] [Google Scholar]
- 5. Hodges SD, Humphreys SC, Eck JC, Covington LA. Management of incidental durotomy without mandatory bed rest. A retrospective review of 20 cases. Spine (Phila Pa 1976). 1999;24:2062–2064. [DOI] [PubMed] [Google Scholar]
- 6. Kamenova M, Severina L, Mariani L, Schaeren S, Soleman J. Management of incidental dural tear during lumbar spine surgery, to suture or not to suture? World Neurosurg. 2016;87;455–462. [DOI] [PubMed] [Google Scholar]
- 7. Kalevski SK, Peev NA, Haritonov DG. Incidental dural tears in lumbar decompressive surgery: incidence, causes, treatment, results. Asian J Neurosurg. 2010;5:54–59. [PMC free article] [PubMed] [Google Scholar]
- 8. Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res. 2001;389:238–247. [DOI] [PubMed] [Google Scholar]
- 9. Guerin P, El Fegoun AB, Obeid I, et al. Incidental durotomy during spine surgery: incidence, management and complications. A retrospective review. Injury. 2012;43:397–401. [DOI] [PubMed] [Google Scholar]
- 10. Saxler G, Kramer J, Barden B, Kurt A, Pfortner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine (Phila Pa 1976). 2005;30:2298–2302. [DOI] [PubMed] [Google Scholar]
- 11. Puvanesarajah V, Hassanzadeh H. The true cost of a dural tear: medical and economic ramifications of incidental durotomy during lumbar discectomy in elderly Medicare beneficiaries. Spine (Phila Pa 1976). 2017;42:770–776. [DOI] [PubMed] [Google Scholar]
- 12. McMahon P, Dididze M, Levi AD. Incidental durotomy after spinal surgery: a prospective study in an academic institution. J Neurosurg Spine. 2012;17:30–36. [DOI] [PubMed] [Google Scholar]
- 13. Espiritu MT, Rhyne A, Darden BV., 2nd Dural tears in spine surgery. J Am Acad Orthop Surg. 2010;18:537–545. [DOI] [PubMed] [Google Scholar]
- 14. Gautschi OP, Stienen MN, Smoll NR, Corniola MV, Tessitore E, Schaller K. Incidental durotomy in lumbar spine surgery—a three nation survey to evaluate its management. Acta Neurochir (Wien). 2014;156:1813–1820. [DOI] [PubMed] [Google Scholar]
- 15. Miscusi M, Polli FM, Forcato S, et al. The use of surgical sealants in the repair of dural tears during noninstrumented spinal surgery. Eur Spine J. 2014;23:1761–1766. [DOI] [PubMed] [Google Scholar]
- 16. Sawamura Y, Asaoka K, Terasaka S, Tada M, Uchida T. Evaluation of application techniques of fibrin sealant to prevent cerebrospinal fluid leakage: a new device for the application of aerosolized fibrin glue. Neurosurgery. 1999;44:332–337. [DOI] [PubMed] [Google Scholar]
- 17. Jankowitz BT, Atteberry DS, Gerszten PC, et al. Effect of fibrin glue on the prevention of persistent cerebral spinal fluid leakage after incidental durotomy during lumbar spinal surgery. Eur Spine J. 2009;18:1169–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tosun B, Ilbay K, Min Kim MS, Selek O. Management of persistent cerebrospinal fluid leakage following thoraco-lumbar surgery. Asian Spine J. 2012;6;157–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Low JC, von Niederhausern B, Rutherford SA, King AT. Pilot study of perioperative accidental durotomy: does the period of postoperative bed rest reduce the incidence of complication? Br J Neurosurg. 2013;27:800–802. [DOI] [PubMed] [Google Scholar]
- 20. Khan MH, Rihn J, Steele G, et al. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: a review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976). 2006;31:2609–2613. [DOI] [PubMed] [Google Scholar]
- 21. Radcliff KE, Sidhu GD, Kepler CK, et al. Complications of flat bedrest following incidental durotomy. Clin Spine Surg. 2016;29:281–284. [DOI] [PubMed] [Google Scholar]
- 22. O’Neil KR, Fehlings MG, Mroz TE, et al. A multicentre study of the presentation, treatment and outcomes of cervical dural tears. Global Spine J. 2017;7(1 suppl);58S–63S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Masuda S, Fujibayashi S, Otsuki B, Kimura H, Neo M, Matsuda S. The dural repair using the combination of polyglycolic acid mesh and fibrin glue and postoperative management in spine surgery. J Orthop Sci. 2016;21:586–590. [DOI] [PubMed] [Google Scholar]
- 24. Kamenova M, Leu S, Mariani L, Schaeren S, Soleman J. Management of incidental dural tear during lumbar spine surgery. To suture or not to suture. World Neurosurg. 2016;87:455–462. [DOI] [PubMed] [Google Scholar]
- 25. Wolff S, Kheirredine W, Riouallon G. Surgical dural tears: prevalence and updated management protocol based on 1359 lumbar vertebra interventions. Orthoped Traumatol. 2012;98:879–886. [DOI] [PubMed] [Google Scholar]


