Short abstract
Objective
We herein present a case involving a prevertebral abscess complicated by a spinal epidural abscess (SEA) secondary to intradiscal oxygen–ozone chemonucleolysis for treatment of a cervical disc herniation.
Methods
A 67-year-old woman with a history of intradiscal oxygen–ozone chemonucleolysis developed numbness and weakness in her right upper and bilateral lower extremities followed by urinary retention. Her symptoms did not respond to intravenous antibiotics alone. Magnetic resonance imaging of the cervical region revealed an extensive SEA anterior to the spinal cord, spinal cord myelopathy due to anterior compression by the lesion, and a prevertebral abscess extending from C2 to T1. She underwent surgical drainage and irrigation.
Results
The patient was successfully treated with surgical drainage and systemic antibiotic therapy without kyphosis. Streptococcus intermedius was detected within the abscess. All clinical symptoms except for the sensory deficit in the left leg were relieved.
Conclusions
The safety of intradiscal oxygen–ozone therapy requires further assessment. High-dose intravenous antibiotics should be initiated empirically at the earliest possible stage of prevertebral and epidural abscesses. Surgical drainage may be a rational treatment choice for patients with a prevertebral abscess complicated by an SEA and spinal cord myelopathy.
Keywords: Oxygen–ozone, cervical disc herniation, prevertebral abscess, spinal epidural abscess, intravenous antibiotics, surgical drainage
Introduction
Prevertebral abscesses are rare but potentially life-threatening. Infections of the prevertebral space always result from infective spondylodiscitis or penetrating injuries to the posterior pharyngeal wall.1 Intradiscal injection of oxygen–ozone (O2-O3) gas can be used to treat disc herniation. The main mechanism of action is dehydration by reduction of proteoglycans and a subsequent decrease in the hernia volume.2,3 Percutaneous techniques can minimize the invasive nature of surgery and decrease complications such as postsurgical infection. However, the safety profile of O2-O3 chemonucleolysis remains controversial. We herein present a case of an acute prevertebral abscess secondary to intradiscal O2-O3 chemonucleolysis for treatment of a cervical disc herniation in a patient who subsequently recovered well without cervical instability or progressive kyphosis. This case is being reported to alert clinicians to the potential complications associated with O2-O3 therapy and the need for caution when considering this treatment.
Case report
The present study was approved by the ethics committee of Tianjin Medical University General Hospital. Written informed consent was obtained from the patient.
A 67-year-old woman developed pain and numbness in her left hand and was diagnosed with cervical disc herniation. She received a percutaneous intradiscal injection of an O2-O3 gas mixture at C5 to C6 in another hospital 2 weeks before admission (Figure 1(a)). Her symptoms were partially relieved after the treatment. However, 3 days later she developed fever and chills. Her body temperature ranged from 37°C to 39°C. Her white blood cell count was 27.79 × 109/L with predominant neutrophilia (87.3%). She was diagnosed with an upper respiratory tract infection and received intravenous levofloxacin for 1 week in another clinic. Her fever and chills vanished. However, she subsequently presented to our hospital with a 4-day history of numbness and weakness in her right upper and bilateral lower extremities as well as urinary retention.
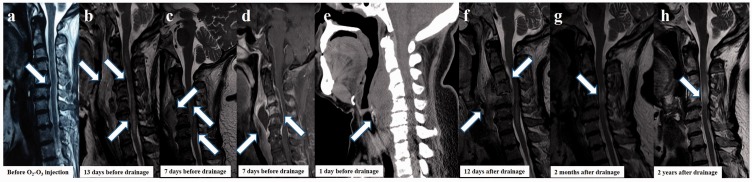
Figure 1.
Magnetic resonance imaging (MRI) and computed tomography findings. (a) Cervical sagittal T2-weighted MRI performed in another hospital before intradiscal oxygen–ozone (O2-O3) injection shows disc herniation at C5 to C6 (white arrow). (b) Cervical MRI performed before admission reveals an increased soft tissue density along the entire extent of the prevertebral region of the neck with hyperintensity in the spinal cord from C2 to C7 (white arrows). (c, d) Enhanced cervical MRI reveals an extensive spinal epidural abscess extending from C2 to C6 anterior to the spinal cord. Additionally, spinal cord myelopathy is present from C3 to C6 due to anterior compression by the lesion, and a prevertebral abscess with hypointense content and homogeneous enhancement of the wall and septa is present. There is no evidence of an air–fluid level, vertebral erosion, or foreign body (white arrows). (e) Cervical computed tomography shows a prevertebral abscess from C2 from T1 (white arrow). (f) Repeat cervical MRI after drainage shows a significant decrease in the hyperintensity and size of the cervical prevertebral and epidural spaces (white arrows). (g, h) MRI shows hyperintensity in the spinal cord at C4 to C5 after the 2-month and 1-year follow-ups (white arrow).
The patient was afebrile with a normal pulse, blood pressure, and respiratory rate. Clinical examination revealed weakness in the right upper limb (Medical Research Council [MRC] grade 2/5) and bilateral lower limbs (MRC grade 3–4/5) and normal reflexes with sensory deficit below T6 on the left side. Babinski’s sign was positive. There was no evidence of any neck swelling. She had no history of tuberculosis or diabetes.
Laboratory testing revealed a normal white blood cell count and an elevated erythrocyte sedimentation rate and C-reactive protein concentration. The patient’s fasting and postprandial blood glucose levels were both normal. Lumbar puncture results showed an elevated white cell count (60 × 106/L) with predominant lymphocythemia and elevated protein (2.34 g/L), but decreased glucose and chloride concentrations. Blood and cerebrospinal fluid cultures were negative. Cervical magnetic resonance imaging (MRI) revealed an increased soft tissue density along the entire extent of the prevertebral region of the neck with hyperintensity in the spinal cord from C2 to C7 (Figure 1(b)).
The patient was started on intravenous ceftriaxone; however, her symptoms were not relieved. One week later, enhanced cervical MRI revealed an extensive spinal epidural abscess (SEA) extending from C2 to C6 anterior to the spinal cord, spinal cord myelopathy from C3 to C6, and a prevertebral abscess with hypointense contents and homogeneous enhancement of the wall and septa (Figure 1(c), (d)). The patient was switched from intravenous ceftriaxone to intravenous vancomycin. Two days later, she developed neck pain and dysphagia. Cervical computed tomography showed a prevertebral abscess from C2 from T1 (Figure 1(e)). She underwent surgical drainage under general anesthesia with endotracheal intubation. A 6-cm transverse incision was made at the level of the thyroid cartilage, and 60 mL of frank pus was drained from the abscess. A negative-pressure drain was inserted into the space and secured in place for constant postoperative drainage of the abscess and irrigation of the space with antiseptic solution. The pus was sent for Gram staining, aerobic bacterial culture and sensitivity, and acid-fast bacilli (AFB) staining and culture. Gram staining and culture revealed growth of Streptococcus intermedius sensitive to cefotaxime and vancomycin. Acid-fast bacilli staining and culture were negative. Cervical MRI carried out 12 days later showed a significant decrease in the hyperintensity and size of the cervical prevertebral and epidural spaces (Figure 1(f)). The patient was discharged after 16 days of intravenous antibiotic therapy and was advised to undergo 4 weeks of treatment with an oral antibiotic. At the 2-month follow-up, physical examination revealed no weakness but hypoesthesia in the right leg. MRI showed hyperintensity in the spinal cord from C4 to C5 (Figure 1(g)). Both the sensory and MRI abnormalities persisted after 1 year (Figure 1(h)).
Discussion
Ozone chemonucleolysis for disc herniations has been performed for more than 20 years. Muto et al.2 reported no neurological or infectious complications during follow-up. However, severe infection has been reported in rare cases.3,4 Prevertebral abscesses are extremely uncommon. In developing countries, however, the lack of primary healthcare, antibiotic abuse, and high level of antibiotic-resistant infections have been recognized as prime contributing factors to both deep neck infections and death.5 Deep neck infections, including prevertebral abscesses, are infections within the potential spaces and fascial planes of the head and neck. Most of these infections are of odontogenic origin. However, prevertebral infections usually result from infective spondylodiscitis and penetrating injuries to the posterior pharyngeal wall.1 The patient in the present case had no predisposing risk factors, such as diabetes, malignancy, or human immunodeficiency virus infection. Streptococcus intermedius, a bacterial species native to the mouth, nasopharynx, and esophagus, was isolated from the abscess. Considering the negative blood culture and no evidence of gastrointestinal disease, the most likely route was transesophageal puncture during chemonucleolysis, similar to a previously reported case.3 Andrés-Cano et al.3 and Bo et al.4 each reported a case of a cervical spondylodiscitis with an associated SEA secondary to O2-O3 therapy for cervical disc herniation. Both patients subsequently developed cervical instability with progressive kyphosis after abscess drainage and decompressive laminectomy, which required spinal stabilization with instrumentation. In the present case, we selected surgical drainage to protect the intervertebral disc and maintain the spinal stability. A nasogastric tube was inserted into the space and secured in place for constant postoperative drainage of the abscess and irrigation of the space with antiseptic solution. The patient had been started on intravenous vancomycin before the operation. All of these procedures effectively controlled the infection. Our patient did not develop cervical instability. However, the T2 hyperintensity in the spinal cord on MRI did not resolve. This imaging abnormality indicated the presence of ischemic myelopathy, which caused the residual sensory deficit in her left leg.
The optimal application of conservative versus surgical management of SEAs remains controversial.6,7 In the present case, the SEA complicated with a deep neck infection made treatment more challenging. Broad-spectrum antibiotic therapy is essential at the time of presentation of deep neck abscess, and treatment should subsequently be updated based on culture and sensitivity. Unfortunately, a blood culture was not done before the initiation of antibiotic therapy because the physician did not correlate the patient’s symptoms with the invasive injection. Moreover, inappropriate use of antibiotics before admission changed the clinical presentation of the infections, making the symptoms elusive.
In conclusion, this case indicates that the safety of intradiscal O2-O3 therapy requires further assessment. Even a minimally invasive injection can cause severe complications in rare cases. Surgical drainage should be performed to relieve compression from prevertebral and epidural abscess formation if the patient exhibits a decline in neurologic function or airway obstruction.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by the National Natural Science Foundation of China (grant number: 81571172) and the Tianjin Research Program of Application Foundation and Advanced Technology (grant number: 15JCYBJC49800).
References
- 1.Hedge A, Mohan S, Lim WE. Infections of the deep neck spaces. Singapore Med J 2012; 53: 305–311. [PubMed] [Google Scholar]
- 2.Muto M, Ambrosanio G, Guarnieri G, et al. Low back pain and sciatica: treatment with intradiscal-intraforaminal O2-O3 injection. Our experience Radiol Med 2008; 113: 695–706. [DOI] [PubMed] [Google Scholar]
- 3.Andrés-Cano P, Vela T, Cano C, et al. Cervical spondylodiscitis after oxygen-ozone therapy for treatment of a cervical disc herniation: a case report and review of the literature. HSS J 2016; 12: 278–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bo W, Longyi C, Jian T, et al. A pyogenic discitis at c3-c4 with associated ventral epidural abscess involving c1-c4 after intradiscal oxygen-ozone chemonucleolysis: a case report. Spine (Phila Pa 1976) 2009; 34: E298–E304. [DOI] [PubMed] [Google Scholar]
- 5.Bhandarkar AM, Pillai S, Venkitachalam S, et al. Acute prevertebral abscess secondary to infected pancreatic pseudocyst. BMJ Case Rep 2014; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alton TB, Patel AR, Bransford RJ, et al. Is there a difference in neurologic outcome in medical versus early operative management of cervical epidural abscesses? Spine J 2015; 15: 10–17. [DOI] [PubMed] [Google Scholar]
- 7.Ghobrial GM, Franco D, Theofanis T, et al. Cervical spondylodiscitis: presentation, timing, and surgical management in 59 patients. World Neurosurg 2017; 103: 664–670. [DOI] [PubMed] [Google Scholar]