Short abstract
Objective
The agranulocytosis-associated perianal infection (PI) rate ranges from 60% to 100% among patients with hematopoietic malignancies. In this study, we assessed the efficacy of a quality control circle (QCC) to minimize the PI rate.
Methods
Among 274 patients with severe immunodeficiency (agranulocytosis of ≥2 weeks) in our bone marrow transplantation center, the PI rate was 17.20%. A QCC was established following the 10 steps of the plan-do-check-act (PDCA) model; this was scientifically supported by culturing the bacterial colony from patients’ perianal skin to determine the sanitization effect and interval time. Because a warm aqueous solution of potassium permanganate is recommended for sanitization, the bacterial colony culture was also used to determine the proper drug concentration, water temperature, and soaking time. All procedures were standardized. Patients, hospital staff, and medical students were enrolled into the QCC team based on the patient–hospital–student (PHS) win–win concept.
Results
After establishment of the PDCA model, the PI rate among 253 patients decreased from 17.20% to 5.93% and remained at 5.25% during the following year. The medical expenses and length of hospital stay consequently decreased.
Conclusion
The QCC and PHS win–win concept can reduce the PI rate and promote medical quality.
Keywords: Quality control, perianal infection, bone marrow transplantation, quality control circle, hematological malignancies, agranulocytosis, patient–hospital–student win–win
Introduction
Approximately 60% to 100% of patients develop infectious complications following high-dose chemotherapy and hematopoietic stem cell transplantation (HSCT), and the mortality rate of such complications ranges from 11% to 57%.1 The main etiologic factor is agranulocytosis (<0.5 × 109/L) with a duration of ≥2 weeks, which can detrimentally aggravate the patient’s clinical condition and lead to an increased risk of infection, particularly perianal infection (2.0%–32.0%) and oral infection (14.7%).2,3
Perianal infections are often accompanied by severe pain, swelling, constipation, perianal abscess formation, fistula infection, and similar conditions. A perianal abscess is defined as the presence of an erythematous firm or fluctuant tender mass located around the anus. An anal fistula is defined as an opening in the skin near the anus that leads into a blind pouch or that may connect the rectal canal through a tunnel.4 In patients with neutropenia, however, the clinical signs and symptoms of perianal infection are often camouflaged.5,6 A reduction in the perianal infection rate could reduce the local and systemic infection rate, treatment expenditure, and mortality rate.
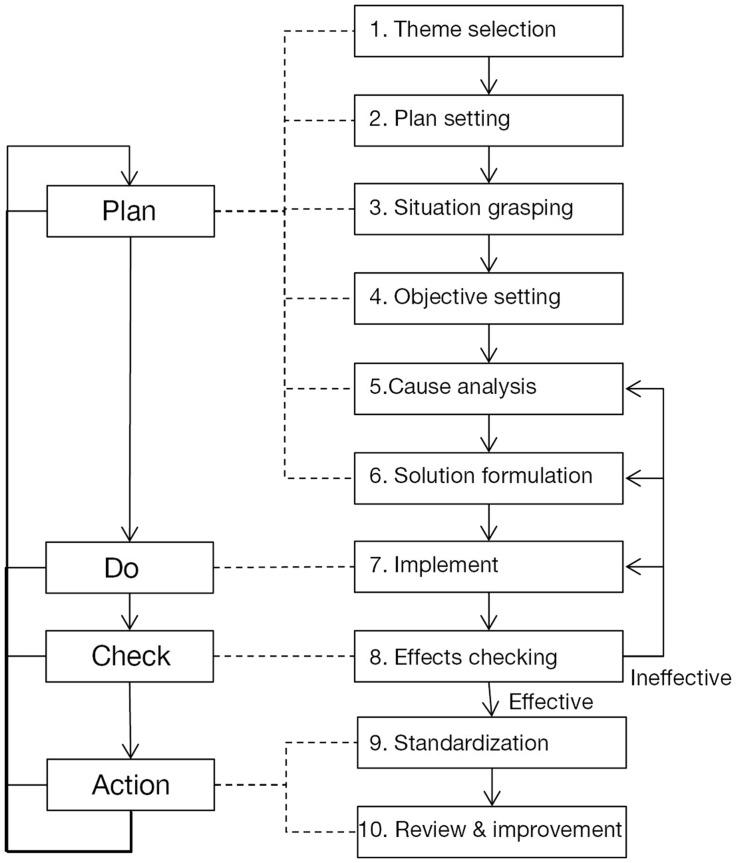
The theoretical basis of the quality control circle (QCC) is the Deming cycle, also known as the plan-do-check-act (PDCA) model, which involves 10 steps (Figure 1). By the end of 2016, more than 40,000 QCC activities had been carried out in the China mainland.7 In the present study, a QCC was established to reduce the perianal infection rate in patients with agranulocytosis at an HSCT center. A patient–hospital–student (PHS) win–win concept was integrated into this QCC. This study was performed to assess the efficacy of this QCC with respect to minimization of the perianal infection rate.
Figure 1.
Plan-do-check-act circulation and the basic steps of the quality control circle
Methods
Ethics
This study was approved by the ethics committee of Nanfang Hospital. All patients provided written informed consent for inclusion in the study.
QCC team
The PHS win–win QCC team comprised four doctors (two senior, one attending, and one resident), two nurses, one laboratory technician, and one quality control manager of Nanfang Hospital as well as two medical students from Southern Medical University. As guests of the QCC, two patients actively participated in steps 5 to 9.
Plan
Theme selection (step 1)
The 10 members of the QCC team voted to select the theme of the QCC (i.e., the reduction in the perianal infection rate) in terms of urgency, feasibility, economy, and QCC team capacity with the “5-3-1” principle and 80/20 rule.8,9
Plan setting, situation grasping, and objective setting (steps 2–4)
The census of 234 cases of death caused by hematological malignancies during 10 years (2003 June–2013 May) at Nanfang Hospital was analyzed. Before establishment of the QCC, the perianal infection rate of 274 sequential cases at the HSCT center (April 2013–September 2013) was investigated; each patient had an agranulocytosis duration of ≥14 days.
Cause analysis (step 5)
Based on the results of a questionnaire checklist for patients with perianal infection before establishment of the QCC, the cumulative frequency of the following three dominant factors was 80.85% based on Pareto’s principle10–12: 1) lack of knowledge about perianal infection, 2) lack of standard operating procedures (SOP) for skin disinfection, and 3) lack of proper instruments. Based on brainstorming sessions, a fishbone diagram, new follow-up checklists, and a new Pareto’s analysis for the causes of each factor, the “real causes” were identified for improvement.
Solution formulation (step 6)
Ultimately, selection and integration of countermeasures according to the “real causes” were performed. The principle of “5W1H” (Who, What, When, Where, Why, and How) was applied to supplement the countermeasures.
Do (Step 7)
Knowledge publicity and supervision
With the students’ help, training and checklists were given to the medical staff, patients, and family members. Anthropological investigations were applied to the patients to obtain real-time feedback.
SOP of perianal skin disinfection method and implementation
To evaluate the effect of perianal skin disinfection, the quantitative bacterial colony assay results of the perianal area skin were compared before and after the cleaning procedures and used for publicity.
Using the same methodology, the medical students tested the optimal concentration (1:5000/1:5k, 1:10k, 1:20k, 1:40k, 1:80k, 1:160k, 1:200k, and 1:400k), soaking time (5 and 10 min), temperature (4°C, 25°C, 40°C, and 60°C), and pH of potassium permanganate solution for skin disinfection.13
Standardization of perianal disinfection instruments and implementation
We developed a toolkit to ensure professional and simple implementation of the SOP for perianal skin disinfection. For public knowledge, essential factors were recorded and spread by audio and video in the Mandarin, Cantonese, and Teochew dialects.
Check (Step 8)
The perianal infection rate was investigated in the bone marrow transplantation center post-QCC activity (October 2013–May 2014) among 253 sequential cases. The same checklist questionnaire was conducted and compared before and after establishment of the QCC. The economic benefit was calculated with the data provided by the Information, Financial, and Statistics departments. The QCC team capacity was evaluated in eight aspects: problem solving, responsibility, communication and coordination, self-confidence, team unity, enthusiasm, quality control practices, and harmony.
Act (Steps 9 and 10)
The flowchart was standardized for improvement and renewed every 9 months.
Statistical analysis
Statistical analysis was performed either with an unpaired two-sided Student’s t-test or one-way analysis of variance using SPSS software (SPSS 21.0 software; IBM Corp., Armonk, NY, USA).
Results
Plan (Steps 1–6)
Among 234 deaths, 68.40% (160 patients) died of severe infection (98/160 developed a perianal infection within 3 months before death, P < 0.05). Before establishment of the QCC, 47 of 274 patients (17.20%) had developed a perianal infection.
The countermeasures were standardization and implementation of the methods of perianal skin disinfection and standardization of the perianal skin disinfection instruments.
Do (Step 7)
Knowledge publicity
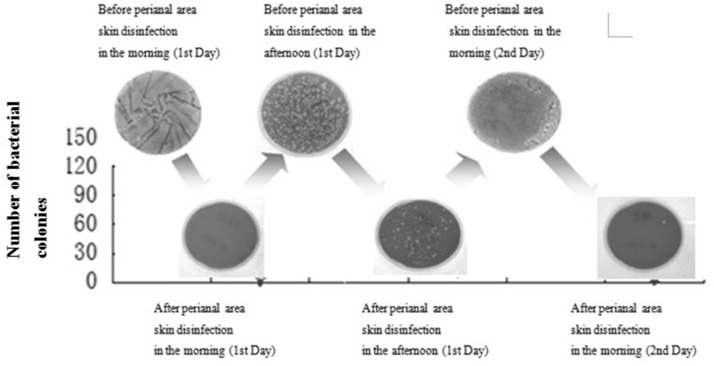
A quantitative bacterial colony assay of the perianal skin before and after cleaning was conducted and used for publicity (Figure 2). This assay was determined to be very efficient.
Figure 2.
Quantitative bacterial colony assay results of perianal skin before and after cleansing
SOP of perianal area skin disinfection
Based on the quantitative bacterial colony assay of the perianal skin, we determined that the cleaning procedure should be performed 3+X times per day (X = number of defecations) and that the anus should be soaked in a warm (40°C) solution of potassium permanganate for 10 minutes at a concentration of 1:100k (a colorimetric chart was developed to ensure achievement of this concentration).
Check (Step 8)
A much lower perianal infection rate was achieved after than that before establishment of the QCC [5.93% of 229 sequential patients (October 2013–April 2014) vs 17.20%, respectively; P < 0.01]. The causes are compared in Table 1. The perianal infection rate was maintained at 5.25% for the next 9 months.
Table 1.
Factors associated with perianal infections in patients with agranulocytosis before and after establishment of the quality control circle
| Before QCC |
After QCC |
|||||
|---|---|---|---|---|---|---|
| Factors to check | Frequency | Percentage | Cumulative percentage | Frequency | Percentage | Cumulative percentage |
| Lack of knowledge about perianal infection | 24 | 51.06% | 51.06% | 1 | 6.67% | 6.67% |
| Lack of SOP of skin disinfection | 9 | 19.15% | 70.21% | 0 | 0.00% | 6.67% |
| Lack of proper instruments | 5 | 10.64% | 80.85% | 0 | 0.00% | 6.67% |
| History of chronic perianal abscess | 2 | 4.26% | 85.11% | 7 | 46.66% | 53.33% |
| Lack of communication between doctors and patients | 1 | 2.12% | 87.23% | 1 | 6.67% | 60.00% |
| No cleansing habits | 1 | 2.13% | 89.36% | 1 | 6.67% | 66.67% |
| History of gastrointestinal disease | 1 | 2.13% | 91.49% | 4 | 26.66% | 93.33% |
| Presence of systemic diseases such as diabetes | 1 | 2.13% | 93.62% | 0 | 0.00% | 93.33% |
| Poor living conditions (food and cleansing) | 1 | 2.13% | 95.74% | 1 | 6.67% | 100.00% |
| Long history of antibiotic prophylaxis | 1 | 2.13% | 97.87% | 0 | 0.00% | 100.00% |
| Lack of antibiotic prophylaxis | 1 | 2.13% | 100.00% | 0 | 0.00% | 100.00% |
QCC, quality control circle; SOP, standard operating procedures
The decrease in the perianal infection rate from 17.20% to 5.93% indicates that 56 cases of infection should be avoided in 1 year, which might save 1,568,000 RMB in antibiotics costs and 784 inpatient days, which can treat 66 new patients in the HSCT center.
After establishment of the QCC, significant improvements were noted in problem solving, responsibility, communication and coordination, self-confidence, team unity, enthusiasm, and quality control practices and harmony.
Action (Steps 9 and 10)
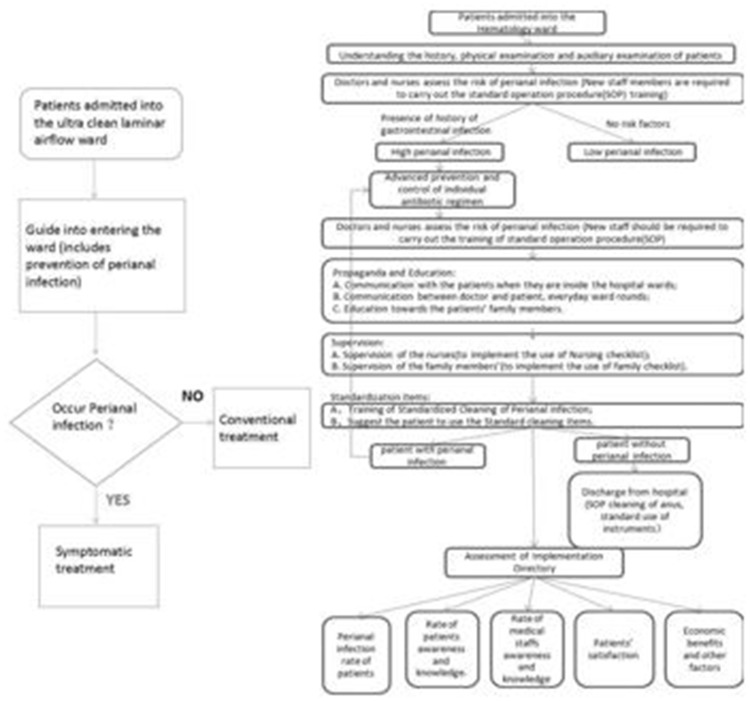
The flowcharts before and after establishment of the QCC are shown in Figure 3.
Figure 3.
Flowchart before (left) and after (right) establishment of the quality control circle
Discussion
In the present study, the perianal infection rate of patients with agranulocytosis decreased from 17.20% to 5.93% after establishment of the QCC, indicating that the QCC was very effective and efficient in controlling perianal infection, costs, and acceleration of hospital bed turnover.
Patients and medical students should participate in QCCs. Based on the concept of the “voice of the customer,” patients make special contributions to quality improvement proposals. Using the results of the anthropological investigations and questionnaires of patients administered by medical students, we found that the perception of an absence of bacteria was the key factor in the prevention of implementation of perianal area skin disinfection. Thus, a quantitative bacterial colony assay of the perianal skin before and after cleaning was conducted and used for publicity (Figure 2).
Large hospitals in China are overcrowded and have scarce resources. China contains 2% of the mostly exhausted medical staff worldwide and serves 22% of the world’s population. Thus, China must obtain reinforcement from outside the current medical system for assistance in the time- and energy-consuming, specialized activities performed by the QCC. A classic QCC is a small group of professionals who work in a close, familiar environment. In the present study, the authors developed the SOP with the talent, time, energy, and knowledge of many medical students.
In conclusion, the authors have established a new kind of QCC team using a PHS win–win concept that simultaneously benefits the medical staff, medical students, and patients. This QCC successfully reduced the rate of perianal infection in patients with agranulocytosis.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research has been granted under the Quality Improvement Funding of Nanfang Hospital and College students' innovative entrepreneurial project of Southern Medical University (No.201612121242).
References
- 1.Bertz H, Auner HW, Weissinger F, et al. Antimicrobial therapy of febrile complications after high-dose chemo-/radiotherapy and autologous hematopoietic stem cell transplantation–guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2003; 82(Suppl 2): S167–S174. [DOI] [PubMed] [Google Scholar]
- 2.Solmaz S, Korur A, Gereklioğlu Ç, et al. , Anorectal complications during neutropenic period in patients with hematologic diseases. Mediterr J Hematol Infect Dis 2016; 8: e2016019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bai YL, Li WP, Liu B, et al. Analysis of Infectious Factors in 80 Cases of Acute Leukemia Granulocytosis. Journal of Nursing 2012; 18: 32–33. [Google Scholar]
- 4.Chen CY, Cheng A, Huang SYet al. , Clinical and microbiological characteristics of perianal infections in adult patients with acute leukemia. PLoS One 2013; 8: e60624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huixuan Zheng. The effect of '3S' in promotion of franchising. Chain and franchise. Management engineer. 2008, 7: 34–35 [Google Scholar]
- 6.Perazzoli C, Feitosa MR, Figueiredo-Pontes LL, et al. Management of acute colorectal diseases in febrile neutropenic patients. J Coloproctol 2014; 34: 189–192. [Google Scholar]
- 7.Tingfang Liu. Review of QCC of Chinese hospitals. Journal of Chinese research hospitals 2015; 2: 24–28. [Google Scholar]
- 8.Tingfang Liu, Nan Liu. Operation manual of Chinese hospital quality management[M]. Beijing: People's Medical Publishing House 2012: 36–72. [Google Scholar]
- 9.Minghui Liang. Applied research about the quality control cycle in continuous improvement of medical quality. Chinese hospital management 2012; 32: 37–39. [Google Scholar]
- 10.Chengyuan Liu. Three Xian doctrine of management. Business administration 2008: 76. [Google Scholar]
- 11.Zongjiu Zhang. Chinese hospital review practice [M]. People's Medical Publishing House, 2013.
- 12.Junyang Gao, Tingfang Liu. Existing problems and corresponding countermeasure about validation for the true of Chinese hospital. Chinese hospital 2015; 19: 7–9. [Google Scholar]
- 13.Lifen Lan. Effect of potassium permanganate bath on prevention of perianal infection in leukemia patients. New Medical Information Digest (Continuous Electronic Journal) 2015: 88–89.