Abstract
Ankle sprains are one of the most prevalent athletic injuries. Prior work has investigated lateral ankle sprains, but research on generally more severe medial sprains is lacking. This case report performs a kinematic analysis using novel motion analysis methods on a non-contact medial ankle sprain. Peak eversion (50°) occurred 0.2 seconds following ground contact, maximum velocity of 426°/s, while peak dorsiflexion (64°) occurred with a greater maximum velocity (573°/s). The combination of dorsiflexion at ground contact and rapid eversion is associated with a non-contact eversion sprain. This study provides a quantitative analysis of the eversion ankle sprain injury mechanism.
Keywords: Athletic injury, Biomechanics, Ankle injury, Kinematics
Introduction
A recent consensus statement from the International Ankle Consortium1 highlights the need for preventative programs to reduce the prevalence of ankle sprains. Ankle injuries are commonly seen in both athletic2 and general3 populations. American Football players are at high risk, with 72% reporting a foot or ankle injury during their athletic career.4 These injuries are not insignificant, as over half the incidences reported in a ten-year period in National Football League athletes caused a time loss from play greater than one week.5
In order to develop effective preventative strategies, the injury mechanism must be understood.6 To date, prior work investigating ankle sprain injury mechanisms has focused on inversion sprains, but eversion sprains should also be considered due to their prevalence in sporting situations. In a study on US military cadets, 65% of medial ankle sprains occurred in sporting situations.7 Eversion ankle sprains are associated with comorbidities,8 requiring longer treatment and recovery times than lateral ankle sprains.9 An understanding of the injury mechanism of the more severe eversion sprain is necessary for effective rehabilitation and prevention protocols.
Injury mechanisms have been well described by clinicians,10,11 but recent research has focused on objectively quantifying how injury occurs12, 13, 14, 15; unbiased injury mechanisms are necessary for successful injury prevention work. However, investigating injury mechanisms quantitatively is challenging. Traditional motion analysis techniques can be used when accidental incidents occur in a laboratory setting, although these events are rare. At the ankle, there are currently three documented cases of an accidental lateral ankle sprain injury analyzed using three-dimensional motion analysis.16, 17, 18
The problem of obtaining exact injury biomechanics has been approached in many ways. Often, retrospective analyses that identify pathologies in the musculoskeletal system19 are used, but it is impossible to tell whether the observed pathological symptoms are caused by the injury or were the reason for its occurrence. Other investigative approaches include a simulation of the event within the laboratory setting in healthy participants,20 and using cadaver limbs21 or computer simulations to replicate the injurious motion.
A markerless motion analysis technique was suggested as an alternative approach to investigate injury mechanisms.22 The researchers developed a model-based image matching (MBIM) technique using uncalibrated video images to reconstruct the motion of a subject in three dimensions, applying the method to anterior cruciate ligament injury investigations. The MBIM method was adapted to investigate ankle sprain injuries by Fong and colleagues.16 As the majority of injuries occur outside of a laboratory setting, MBIM allows for investigations of many injuries occurring in their natural settings.
The velocity of ankle inversion is a key mechanism of lateral ankle sprains with high inversion velocities, up to 1752°/s, being reported.14, 15, 16, 17, 18 Eversion is a component of ankle pronation and is commonly seen in running.23 During running, healthy ankle eversion velocities have been reported between 115°/s24 to 207°/s25; we chose an eversion velocity of 250°/s as an injurious threshold for the current case study.
This study will use MBIM to identify potential injury mechanisms for a single ankle eversion sprain case that occurred in an American Football athlete. We hypothesize that an eversion velocity greater than the injury threshold of 250°/s might be observed.
Methods
A search for appropriate video footage (used for analysis under fair use agreement) of ankle eversion injuries that met key criteria was conducted on the official National Football League (NFL) website, using keywords such as ‘ankle sprain’, ‘ankle injury’ and ‘lower leg injury’. Key criteria included multiple views of the injury, with at least one view occurring in real time, clear and visible boundary lines that are ideally perpendicular to each other (such as field markings), adequate resolution for visual identification of knee orientation, the relative size ratio of the foot and shank to overall video, and no more than one consecutive frames where the injured limb is obscured. For an eversion injury event to be considered, the unwanted motion had to cause excessive eversion during landing or cutting, the athlete had to be unable to continue play following injury, and post-match reports must have described the injury as an ankle sprain.
A single non-contact eversion ankle sprain case study was selected for analysis. The 23 year old quarterback landed on his right leg awkwardly on a rollout run in the third quarter of a 2013 pre-season game. He returned to practice two days later but continued to play on restricted timings for the first half of the 2013-14 season. Due to limited access to medical history, neither medical images nor orthopedic reports were available, but athlete height and weight were obtained from the NFL athlete profile (1.91 m and 100 kg respectively).
The obtained video footage comprised of three camera views, with a frame rate of 30 Hz and a resolution of 1280 × 720 pixels. For each view, the footage was trimmed, deinterlaced and transformed into uncompressed AVI image sequences using Adobe Premiere Pro (CC 2015, Adobe Systems Inc., USA). Using Adobe AfterEffects (CC 2015, Adobe Systems Inc., USA), the uncompressed AVI image sequences for each view were synchronized.
To synchronize multiple views of the injurious event, ten seconds of broadcast footage displaying the clock was extracted and key time-points, such as ground contact and toe-off, were used to synchronize between slow-motion views and the ‘normal speed’. The number of frames within this time period was used as the timescale for kinematics. The synchronized image sequences were then rendered into 1 Hz videos, showing each camera view simultaneously, and imported into Poser 4 and Poser Pro Pack (Curious Labs Inc., USA) for matching.
The Poser software includes pre-built humanoid models, the capacity for background video import, split camera views and camera models with multiple translational and rotational degrees of freedom in addition to focal length adjustments. These functions allow for accurate replication of the video set-up, allowing translation, rotation and zoom of each camera to be matched frame by frame.
A virtual environment of the American Football field was reconstructed using the dimensions outlined in the NFL rule book,26 with one meter equal to 0.41 Poser units, or a 410% scale. For each injury view, the reconstructed field was manually aligned with the recorded field by adjusting the camera orientation, position and focal length. Once focal length was identified in the first frame, it remained constant throughout matching.
A male skeleton model (Zygote Media Group Inc., USA) was matched to a still image of the injured athlete to identify body proportions – specifically the shank and the foot. Segment dimensions were adjusted iteratively during matching in order to identify the appropriate scaling parameters. The model used comprised of four segments (pelvis, thigh, shank and foot) with three degrees of freedom at the ankle joint, and two degrees of freedom at the knee and the hip (flexion/extension and ab/adduction for both joints). The default skeleton model ankle joint center was adjusted as previously reported27 to lie at the midpoint between the malleoli.
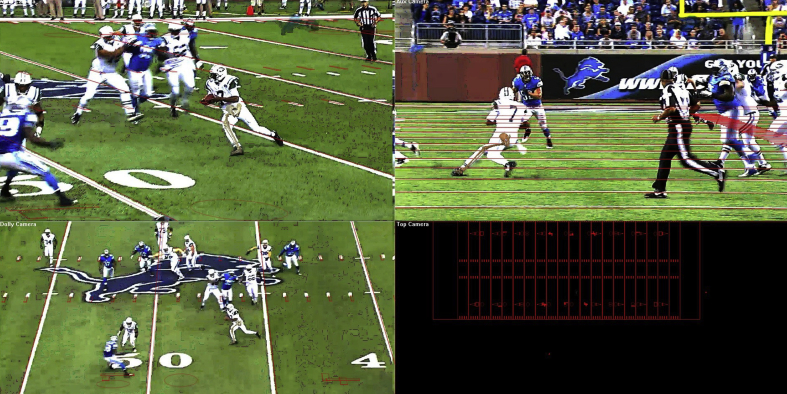
The skeleton model was matched to the synchronized video footage of the athlete, starting at the pelvis and continued distally in each frame. Once matched, the skeleton was replaced with a ‘nude man’ model to determine longitudinal rotation for each segment using surface anatomy. Tibial rotation was assumed to be fully distributed at the ankle. An example matched frame sequence is illustrated in Fig. 1.
Fig. 1.
An example of the matching process, with three simultaneous views of the injury, and a birds-eye view in the bottom right corner. The virtual environment is represented by the red lines, and the Zygote skeleton can be seen matched to the athlete's right lower limb.
The overall motion of the skeletal model was assessed and adjusted by two additional researchers to ensure a smooth motion. Individual segment parameters, such as foot segment bend, twist and turn, were evaluated by the same researcher who conducted the initial matching to manually smooth each parameter's angle curve, minimizing the noise in the computed velocities.
The time histories of ankle joint angle from the skeletal model were imported into Matlab (MathWorks Inc., USA), and joint angles were computed using a custom-written script, following the ISB-recommended joint coordinate system.28 Initial foot ground contact, as observed from the multi-view video, was considered the start of the injury, and all kinematics are reported using this event as time zero. Foot orientations are reported relative to the shank segment.
Results
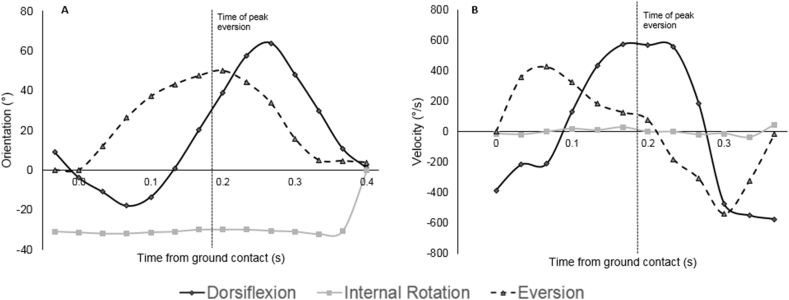
At the point of initial ground contact, time zero, the ankle joint was 11° plantarflexed, 32° externally rotated and 12° everted. At the moment of peak eversion, occurring 0.2 seconds after initial contact, the ankle joint was 39° dorsiflexed, 30° externally rotated and 50° everted. At this time, there was minimal eversion velocity (78°/s) and high dorsiflexion velocity (569°/s), while internal rotation did not change (Fig. 2). The maximum eversion velocity (426°/s) occurred immediately following ground contact. Peak dorsiflexion occurred at 0.27 seconds following ground contact (Fig. 2), later than that of peak eversion, although peak dorsiflexion velocity is observed with peak eversion. Internal rotation remains constant throughout the contact phase.
Fig. 2.
Ankle orientation (A) and velocity (B). Positive values represent dorsiflexion, eversion and internal rotation.
Discussion
Using MBIM on a non-contact eversion ankle sprain case identified an injury mechanism that is a combination of dorsiflexion and eversion, accompanied by high eversion and dorsiflexion velocities that occur just prior to peak eversion. At initial contact, the ankle joint was externally rotated, with slight plantarflexion and a moderate level of eversion. This position is a vulnerable one, characterized by peak eversion occurring rapidly after.
The clinical qualitative eversion sprain injury mechanism is talocrural joint dorsiflexion combined with subtalar joint abduction and eversion.29 In other words, eversion sprains occur through a combination of pronation, abduction and dorsiflexion, and the results from this study support this.
Prior work30 reported injury mechanisms for two eversion ankle sprains in soccer players. The sprains occurred through trampling, with maximum eversion of 25.2° and 20.0°, and associated velocities of 210°/s and 320°/s for each case. The average plantarflexion/dorsiflexion displacement in the current study was 64°, double the 30° reported in the soccer player cases°. The discrepancies between the three cases can be explained due to the nature of the injury, those previously reported30 are contact injuries, while this case study is of a non-contact medial ankle sprain.
Curiously, peak eversion occurred at almost identical timepoints following ground contact - 0.20s and 0.22s for each case reported by Li et al.30 and 0.20s in the present report. This consistent timing reinforces that ankle eversion sprains occur explosively. The rapid time to peak eversion combined with the large range of motion (RoM) we observed implies that medial ligaments are strained first, followed by the talofibular ligaments. The medial ligaments are stronger,31 but rapid changes in orientation strain ligaments to the point of failure.13 The peak eversion velocity reported in this case suggests the ankle joint was acted upon by an excessive torque, leading to rapid changes in kinematics.
The eversion velocity observed in the current study is higher than that found by Li et al.,30 but the three eversion sprain cases have considerably lower eversion/inversion velocity values than those reported in inversion sprains (Table 1), suggesting different injury mechanisms. In this case, the ankle did not fully roll over its medial edge, instead the shank moved laterally while the foot remained planted, causing the eversion motion to come from tibial displacement rather than a medial shift of pressure. However, there appears to be a similar time-scale of injury between inversion and eversion ankle sprains, thus research on inversion ankle sprain can be used to guide explorations into eversion ankle sprain mechanisms.
Table 1.
A comparison of lateral and medial ankle sprain kinematics from the literature.
| Lateral Ankle Sprains |
Medial Ankle Sprains |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fong et al., 2009 |
Mok et al., 2011 |
Kristianslund et al., 2011 |
Fong et al., 2012 |
Gehring et al., 2013 |
Li et al., 2016 |
This study |
|||||||
| Case 1 | Case 1 | Case 2 | Case 1 | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 1 | Case 1 | Case 2 | Case 1 | |
| Peak inversion (°) | 48 | 142 | 78 | 35 | 94 | 48 | 59 | 67 | 126 | 45 | −25 | −20 | −50 |
| Peak inversion velocity (°/s) | 632 | 1752 | 1397 | 559 | 1488 | 509 | 837 | 724 | 800 | 1290 | −210 | −320 | −426 |
| Time of peak inversion (s) | 0.2 | 0.08 | 0.08 | 0.18 | 0.12 | 0.08 | 0.12 | 0.17 | 0.44 | – | 0.2 | 0.22 | 0.20 |
| Peak plantarflexion (°) | 1 | 52 | 16 | 20 | 30 | 28 | 31 | 37 | −8 | 50 | 15 | 31 | −64 |
| Peak plantarflexion velocity (°/s) | 370 | – | – | – | 1748 | 381 | 561 | 571 | 325 | 1240 | – | – | −573 |
| Time of peak plantarflexion (s) | 0.04 | 0.18 | 0.17 | 0.3 | 0.16 | 0.1 | 0.03 | 0.46 | 0.07 | – | 0.2 | 0.22 | 0.27 |
| Peak internal rotation (°) | 10 | 50 | 45 | 55 | 46 | 26 | 99 | 84 | 75 | 13 | −42 | −49 | −32 |
| Peak internal rotation velocity (°/s) | 271 | – | – | – | 1170 | 412 | 2124 | 1312 | 530 | 580 | – | – | 47 |
| Time of peak internal rotation (s) | 0.2 | 0.15 | 0.12 | 0.16 | 0.26 | 0.06 | 0.12 | 0.26 | 0.41 | – | 0.2 | 0.22 | 0.33 |
Large eversion and dorsiflexion RoM in this case and those reported by Li et al.30 is implicated in the injury mechanism. The injury mechanism for inversion ankle sprains has a larger average plantarflexion RoM than that of eversion sprains (Table 1), although this planar motion appears to be critical to the development of both lateral and medial ankle sprains. This is cogent considering the differences in lateral and medial structures of the ankle anatomy.
The tibialis anterior and posterior, flexor digitorum longus and flexor halluces longus insert on the medial ankle, along with a strong lattice of ligaments, restricting the eversion range of motion. The large RoM over the dorsiflexion and eversion ranges observed is sufficient to injure the deltoid ligament, the posterior talofibular ligament, and, to a lesser extent, the anterior talofibular ligament,32 provided the fibula doesn't restrict the movement. It is this fibular restriction that could explain the lower, but still injurious, frontal plane velocities observed in both the present study and past work,30 when compared with lateral sprain studies.14,15,17,18 The conclusions drawn are somewhat restricted by the televised video frame rate, this will often be no higher than 60 Hz. However, the effective frame rate can be doubled by deinterlacing the footage, reducing the likelihood of missing key events of the injury. Further improvements to the MBIM method involve obtaining subject-specific anthropometric data, where athletes consent to researchers to access their information or are available to take direct measurements. It should also be emphasized that the proposed injury mechanism is only speculated from observations – it cannot be said with certainty whether the reported kinematics are a consequence or cause of the eversion ankle sprain.
Conclusion
The present study used quantitative analysis to analyze ankle joint kinematics in an ankle eversion sprain case that occurred in an American Football quarterback. The results suggest a case-specific injury mechanism comprising of sudden eversion and dorsiflexion, with constant internal rotation, agreeing with the clinical qualitative pathology. It is hoped this MBIM analysis starts the discussion for further research into the injury mechanism of medial ankle sprain injuries.
Conflicts of interest
The author(s) have no conflicts of interest relevant to this article.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.asmart.2018.02.001.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Gribble P.A., Bleakley C.M., Caulfield B.M. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;0:1–3. doi: 10.1136/bjsports-2016-096188. [DOI] [PubMed] [Google Scholar]
- 2.Fong D.T.-P., Hong Y., Chan L.-K., Yung P.S.-H., Chan K.-M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Waterman B.R. The epidemiology of ankle sprains in the United States. J Bone Jt Surg. 2010;92(13):2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 4.Kaplan L.D., Jost P.W., Honkamp N., Norwig J., West R., Bradley J.P. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop (Belle Mead NJ) 2011;40(1):40–44. [PubMed] [Google Scholar]
- 5.Orchard J., Powell J. Risk of knee and ankle sprains under various weather conditions in American Football. Med Sci Sports Exerc. 2003;35(7):1118–1123. doi: 10.1249/01.MSS.0000074563.61975.9B. [DOI] [PubMed] [Google Scholar]
- 6.Bahr R., Krosshaug T. Understanding injury mechanisms: a key component of preventing injuries in sport. Br J Sports Med. 2005;39(6):324–329. doi: 10.1136/bjsm.2005.018341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waterman B.R., Belmont P.J., Cameron K.L., Svoboda S.J., Alitz C.J., Owens B.D. Risk factors for syndesmotic and medial ankle sprain: role of sex, sport, and level of competition. Am J Sports Med. 2011;39(5):992–998. doi: 10.1177/0363546510391462. [DOI] [PubMed] [Google Scholar]
- 8.Wolfe M.W., Uhl T.L., Mattacola C.G., McCluskey L.C. Management of ankle sprains. Am Fam Physician. 2001;63(1):93–104. [PubMed] [Google Scholar]
- 9.Boytim M.J., Fischer D.A., Neumann L. Syndesmotic sprains. Am J Sports Med. 1991;19(3):294–298. doi: 10.1177/036354659101900315. [DOI] [PubMed] [Google Scholar]
- 10.Harmon K.G. The ankle examination. Prim Care Clin Off Pract. 2004;31(4 SPEC.ISS.):1025–1037. doi: 10.1016/j.pop.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Mullen J.E., O'Malley M.J. Sprains - residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med. 2004;23(1):97–121. doi: 10.1016/S0278-5919(03)00089-9. [DOI] [PubMed] [Google Scholar]
- 12.Chan Y.-Y., Fong D.T.-P., Yung P.S.-H., Fung K.-Y., Chan K.-M. A mechanical supination sprain simulator for studying ankle supination sprain kinematics. 2008;41 doi: 10.1016/j.jbiomech.2008.05.034. [DOI] [PubMed] [Google Scholar]
- 13.Wei F., Fong D.T.-P., Chan K.-M., Haut R.C. Estimation of ligament strains and joint moments in the ankle during a supination sprain injury. Comput Meth Biomech Biomed Eng. 2015;18(3):243–248. doi: 10.1080/10255842.2013.792809. [DOI] [PubMed] [Google Scholar]
- 14.Fong D.T.-P., Ha S.C.-W., Mok K.-M., Chan C.W.-L., Chan K.-M. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: five cases from televised tennis competitions. Am J Sports Med. 2012;40(11):2627–2632. doi: 10.1177/0363546512458259. [DOI] [PubMed] [Google Scholar]
- 15.Mok K.-M., Fong D.T.-P., Krosshaug T. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: 2 cases during the 2008 Beijing olympics. Am J Sports Med. 2011;39(7):1548–1552. doi: 10.1177/0363546511399384. [DOI] [PubMed] [Google Scholar]
- 16.Fong D.T.-P., Hong Y., Shima Y., Krosshaug T., Yung P.S.-H., Chan K.-M. Biomechanics of supination ankle sprain: a case report of an accidental injury event in the laboratory. Am J Sports Med. 2009;37(4):822–827. doi: 10.1177/0363546508328102. [DOI] [PubMed] [Google Scholar]
- 17.Kristianslund E., Bahr R., Krosshaug T. Kinematics and kinetics of an accidental lateral ankle sprain. J Biomech. 2011;44(14):2576–2578. doi: 10.1016/j.jbiomech.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Gehring D., Wissler S., Mornieux G., Gollhofer A. How to sprain your ankle - a biomechanical case report of an inversion trauma. J Biomech. 2013;46(1):175–178. doi: 10.1016/j.jbiomech.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 19.Bahr R., Karlsen R., Lian O., Ovrebo R.V. Incidence and mechanisms of acute ankle inversion injuries in volleyball: a retrospective cohort study. Am J Sports Med. 1994;22(5):595–600. doi: 10.1177/036354659402200505. [DOI] [PubMed] [Google Scholar]
- 20.Chu V.W.S., Fong D.T.P., Chan Y.Y., Yung P.S.H., Fung K.Y., Chan K.M. Differentiation of ankle sprain motion and common sporting motion by ankle inversion velocity. J Biomech. 2010;43(10):2035–2038. doi: 10.1016/j.jbiomech.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 21.Konradsen L., Voigt M. Inversion injury biomechanics in functional ankle instability: a cadaver study of simulated gait. Scand J Med Sci Sports. 2002;12:329–336. doi: 10.1034/j.1600-0838.2002.00108.x. [DOI] [PubMed] [Google Scholar]
- 22.Krosshaug T., Bahr R. A model-based image-matching technique for three-dimensional reconstruction of human motion from uncalibrated video sequences. J Biomech. 2005;38:919–929. doi: 10.1016/j.jbiomech.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 23.Engsberg J.R., Andrews J.G. Kinematic analysis of the talocalcaneal/talocrural joint during running support. Med Sci Sports Exerc. 1987;19(3):275–284. http://europepmc.org/abstract/MED/3600242 [PubMed] [Google Scholar]
- 24.Dierks T.A., Davis I.S., Hamill J. The effects of running in an exerted state on lower extremity kinematics and joint timing. J Biomech. 2010;43(15):2993–2998. doi: 10.1016/j.jbiomech.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Snyder K.R., Earl J.E., O'Connor K.M., Ebersole K.T. Resistance training is accompanied by increases in hip strength and changes in lower extremity biomechanics during running. Clin Biomech. 2009;24(1):26–34. doi: 10.1016/j.clinbiomech.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Goodell R. Official playing rules of the National Football League. https://operations.nfl.com/media/2725/2017-playing-rules.pdf. Published 2017. Accessed April 4, 2016.
- 27.Mok K.M., Fong D.T.P., Krosshaug T., Hung A.S.L., Yung P.S.H., Chan K.M. An ankle joint model-based image-matching motion analysis technique. Gait Posture. 2011;34(1):71–75. doi: 10.1016/j.gaitpost.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 28.Wu G., Siegler S., Allard P. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. J Biomech. 2002;35(4):543–548. doi: 10.1016/s0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]
- 29.Ferber R., Hreljac a., Kendall K.D. Suspected mechanisms in the cause of overuse running injuries: a clinical review. Sport Heal A Multidiscip Approach. 2009;1(3):242–246. doi: 10.1177/1941738109334272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li X., Fong D., Chan K.-M. Kinematic analysis of ankle eversion sprain in sports: two cases during the FIFA world cup. J Orthop Transl. 2016;7:135. [Google Scholar]
- 31.Siegler S., Chen J., Schneck C.D. The effect of damage to the lateral collateral ligaments on the mechanical characteristics of the human ankle joint. Eng Med Biol Soc 1988 Proc Annu Int Conf IEEE. 1988;2:622–623. [Google Scholar]
- 32.Colville M.R., Marder R.A., Boyle J.J., Zarins B. Strain measurement in lateral ankle ligaments. Am J Sports Med. 1990;18(2):196–200. doi: 10.1177/036354659001800214. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.