Abstract
Background
Despite remarkable progress in the reduction of under-five mortality, childhood diarrhea is still the leading cause of mortality and morbidity in this highly susceptible and vulnerable population. In Ethiopia, study findings regarding prevalence and determinants of diarrhea amongst under-five children have been inconsistent. Therefore, this systematic review and meta-analysis estimates the pooled prevalence of diarrhea and its determinants among under-five children in Ethiopia.
Methods
International databases, including PubMed, Web of Science, EMBASE, CINAHL, Google Scholar, Science Direct, and the Cochrane Library, were systematically searched. All identified observational studies reporting the prevalence and determinants of diarrhea among under-five children in Ethiopia were included. Two authors independently extracted all necessary data using a standardized data extraction format. STATA Version 13 statistical software was used. The Cochrane Q test statistics and I2 test were used to assess the heterogeneity of the studies. A random effects model was computed to estimate the pooled prevalence of diarrhea. Moreover, the associations between determinant factors and childhood diarrhea were examined using the random effect model.
Results
After reviewing of 535 studies, 31studies fulfilled the inclusion criteria and were included in the meta-analysis. The findings from the 31 studies revealed that the pooled prevalence of diarrhea among under-five children in Ethiopia was 22% (95%CI: 19, 25%). Subgroup analysis of this study revealed that the highest prevalence was observed in Afar region (27%), followed by Somali and Dire Dawa regions (26%), then Addis Abeba (24%). Lack of maternal education (OR: 2.5, 95% CI: 1.3, 2.1), lack of availability of latrine (OR: 2.0, 95%CI: 1.3, 3.2), urban residence (OR: 1.9, 95%CI: 1.2, 3.0), and maternal hand washing (OR: 2.2, 95%CI: 2.0, 2.6) were significantly associated with childhood diarrhea.
Conclusion
In this study, diarrhea among under-five children in Ethiopia was significantly high. Lack of maternal education, lack of availability of latrine, urban residence, and lack of maternal hand washing were significantly associated with childhood diarrhea.
Introduction
Childhood diarrhea is defined as the passage of three or more loose or watery stools per 24 hours or an increase in stool frequency or liquidity that is considered abnormal by the mother [1, 2]. Despite remarkable progress in the reduction of under-five mortality, childhood diarrheal disease is still a leading cause of mortality and morbidity [3, 4]. Globally, diarrheal disease contributed to 15% of all under-five deaths (approximately 2.5 million deaths each year), making diarrheal disease the second leading cause of death in the youngest members of society [5, 6]. Developing countries or economically disadvantaged regions carried the highest burden of under-five mortality, with nearly four fifths of all under-five mortality occurring in Sub-Saharan Africa and south Asia [7, 8]. According to World Health Organization (WHO) (2016), the under-five mortality rate in low-income countries was 73.1 deaths per 1000 live births, nearly 14 times the average rate in high-income countries (i.e., 5.3 deaths per 1000 live births) [9].
In Ethiopia, diarrheal diseases are major contributors to under-five mortality. According to the 2016 Ethiopia Demographic and Health Survey report,12% of under-five children had a diarrheal episode in the 2 weeks before the survey [10]. More than half of under-five child deaths are attributable to diseases that are easily preventable and treatable through simple, cost effective, and affordable interventions. Strengthening health systems to provide such interventions to all children will potentially save many young lives [7]. In 2015, the United Nation adopted the Sustainable Development Goals (SDGs) to reduce child mortality and to promote well-being for all children. The SDG goal #3 Target 3.2 aims to end preventable deaths of newborns and under-five children by 2030 [7]. Likewise, the Ethiopian government also implemented various strategies, such as the Health Extension Program, to prevent and control infectious diseases like diarrhea [11].
Despite interventions and innovations by a range of stakeholders, under-five mortality related to diarrhea remains a major concern, especially in developing countries like Ethiopia. In Ethiopia, several studies were conducted to estimate the prevalence as well as to identify modifiable factors of under-five diarrheal diseases [11–32]. However, the prevalence reflected in these small and fragmented studies varied widely and remained inconclusive. Besides prevalence, identifying modifiable risk factors is a critical step in identifying potential interventions. The lack of a nationwide study that determines the prevalence and determinants of diarrhea among under-five children is a significant gap. Therefore, this systematic review and meta-analysis aimed to determine the pooled prevalence and determinants of diarrhea among under-five years of children using available studies in Ethiopia. The findings from this systematic review will highlight the prevalence and determinants of childhood diarrhea with implications to improve health workers’ interventions, to ensure cost-effectiveness, and to accelerate the reduction of childhood diarrhea in Ethiopia.
Methods
Study design and setting
A systematic review and meta-analysis was conducted to estimate the prevalence and determinants of diarrhea among under-five children in Ethiopia. Ethiopia is located in the horn of Africa. It is bounded by Eritrea to the north, Djibouti and Somalia to the east, Sudan and South Sudan to the west, and Kenya to the south. Currently, the Ethiopian population is estimated to be 106,059,710 with 20.2% living in urban areas [33, 34].
Search strategies
We prepared and presented this meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [35] (S1 Table). To find potentially relevant articles, a comprehensive search with no date limits was performed in the following databases: PubMed/MEDLINE, Web of Science, EMBASE, CINAHL, Google Scholar, Science Direct and Cochrane Library (Table 1). All searches were limited to articles written in English given that such language restriction does not alter the outcome of the systematic reviews and meta-analyses[36]. Gray literature of observational studies was searched through the review of reference lists and input of content experts. In addition, to find unpublished papers relevant to this systematic review and meta-analysis, some research centers, including the Addis Ababa Digital Library were searched. Studies identified by our search strategy were retrieved and managed using Endnote X7 (Thomson Reuters, Philadelphia, PA, USA) software. The search of the literature was conducted between the 1st of October to the 1st of November,2017. All papers published until the 1st of November, 2017 were considered. The search used the following keywords “prevalence”, “diarrhea”, “diarrheoa”, “under-five”, “children”, “determinants”, “associated factors” and “Ethiopia”. The search terms were used separately and in combination using Boolean operators like “OR” or “AND”.
Table 1. Example of searches for the MEDLINE/ PubMed and Google Scholar databases to assess the prevalence and determinants of diarrhea among under-five children in Ethiopia.
| Databases | Searching terms | Number of studies |
|---|---|---|
| Google scholar | "prevalence" and "determinants" or "associated factors " and "children" or "under-five" and "diarrhea" or "diarrhoea" and "Ethiopia"-Adults | 124 |
| MEDLINE/ PubMed | ("epidemiology"[Subheading] OR "epidemiology"[All Fields] OR "prevalence"[All Fields] OR "prevalence"[MeSH Terms]) AND ("diarrhoea"[All Fields] OR "diarrhea"[MeSH Terms] OR "diarrhea"[All Fields]) AND under-five[All Fields] AND ("child"[MeSH Terms] OR "child"[All Fields] OR "children"[All Fields]) AND ("ethiopia"[MeSH Terms] OR "ethiopia"[All Fields]) | 43 |
| From other databases | 368 | |
| Total retrieved articles | 535 | |
| Final full text relevant to our review | 31 |
Eligibility criteria
Inclusion criteria
Study area: Only studies conducted in Ethiopia
Population: Only studies involving under-five year children
Publication condition: Both published and unpublished articles were included
Study design: All observational study designs (i.e., cross-sectional, case-control and cohort) reporting the prevalence of diarrhea in under-five children were eligible for this review.
Language: Only articles reported in English language were considered
Exclusion criteria
Articles, which were not fully accessible, after at least two-email contact with the primary authors, were excluded. Exclusion of these articles is because of the inability to assess the quality of articles in the absence of full text.
Measurement of outcome variables
This study has two main outcomes. Childhood diarrheal disease, as the primary outcome variable of this study, is defined as having three or more loose or watery stools in a 24 hour period [37, 38]. The prevalence of childhood diarrhea was estimated as the total number of diarrhea cases divided by the total number of under-five children participating in the study multiplied by 100. The second outcome of this study was to identify the determinants of diarrhea among under-five children. For the second outcome, we determined the association between under-five diarrhea and determinants in the form of the log odds ratio. For major determinants, the odds ratio was calculated based on binary outcomes from the primary studies. The determinants included in this review were: residence (urban versus rural), educational status of caregiver (unable to read and write versus able to read and write), hand washing practices of caregiver (yes versus no), and availability of any type of latrine (yes versus no).
Data extraction
Data from included articles were extracted using a standardized data extraction format, adapted from the Joanna Briggs Institute (JBI), by two authors (AA and CT) independently extracting all necessary data. Any disagreements during the data extraction were resolved through discussion and consensus (i.e., a Delphi process). The primary author of the original research was contacted for additional information or to clarify method details as needed. For the first outcome (prevalence), the data extraction format included primary author, publication year, region(s) of the country where the study was conducted, study area, sample size, response rate and prevalence with 95%CI. For the second outcome (determinants), data were extracted in a format of two by two tables, and then the log odds ratio for each factor was calculated based on the findings of the original studies.
Risk of bias
Two authors (AA and CT) independently assessed the risk of bias for each original study using the tool. To assess the risk of bias, we used the Hoy 2012 addressing internal and external validity tool using 10 criteria [39]. The tool mainly included (1) representation of the population, (2) sampling frame, (3) methods of participants’ selection, (4) non-response bias, (5) data collection directly from subjects, (6) acceptability of case definition, (7) reliability and validity of study tools, (8) mode of data collection, (9) length of prevalence period, and (10) appropriateness of numerator and denominator. Each item was classified as either low or high risk of bias. Not clear was classified as high risk of bias. Finally, the overall score of risk of bias was then categorized according to the number of high risk of bias per study: low (≤ 2), moderate (3–4), and high (≥ 5) (S2 Table).
Data processing and analysis
Data were extracted in Microsoft Excel format, followed by analysis using STATA Version 13 statistical software. The standard error for each original study was calculated using the binomial distribution formula. Heterogeneity among reported prevalence was assessed by computing p-values of Cochrane Q-test and I2statics [40]. As the test statistic showed there is significant heterogeneity among the studies (I2 = 96.31%, p <0.001) as a result a random effects meta-analysis model was used to estimate the DerSimonian and Laird’s pooled effect. In the current meta-analysis, arcsine-transformed proportions were used. The pooled proportion was estimated by using the back-transform of the weighted mean of the transformed proportions, using arcsine variance weights for the fixed-effects model and DerSimonian-Laird weights for the random-effects model [41]. To minimize the random variations between the point estimates of the primary study subgroup, analysis was done based on study settings (i.e., region(s) where the study occurred). In addition, to identify the possible source of heterogeneity, univariate meta-regression was undertaken by considering year of publication, quality score, region of the country where the study was conducted and sample size, however, none of these were found to be statistically significant. Egger’s and Begg’s tests at 5% significant level were not significant for publication bias [42]. Point prevalence, as well as 95% confidence intervals, was presented in the forest plot format. In this plot, the size of each box indicated the weight of the study, while each crossed line refers to 95% confidence interval. For the second outcome, a log odds ratio was used to determine the association between determinant factors and diarrhea among under-five children in the included evidence set.
Results
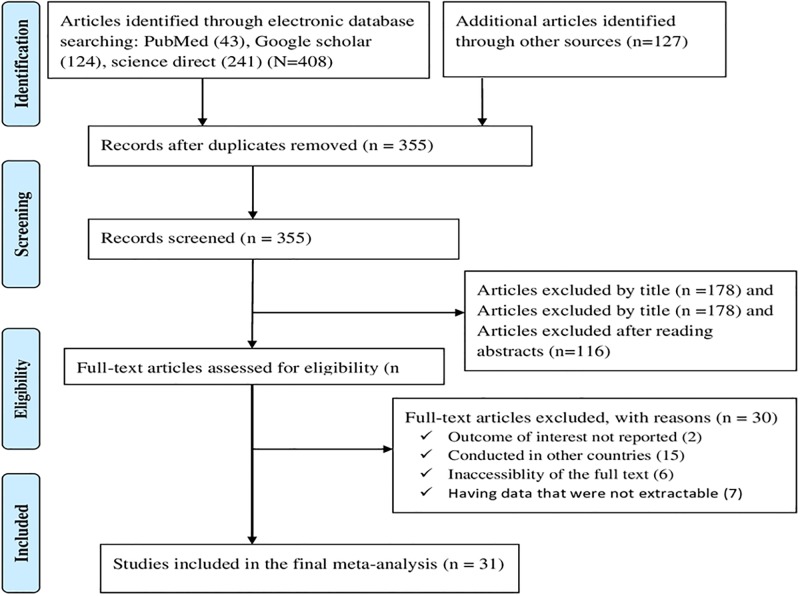
Initially, 535 articles were retrieved reporting prevalence and determinants of diarrhea among under-five children using the range of databases previously described. Of these initial articles, 180 articles were excluded due to duplication. From the remaining 355 articles, 294 articles were excluded after review of their titles and abstracts confirmed non-relevance to this review. Therefore, 61 full text articles were accessed, and assessed for eligibility based on the pre-set criteria, which resulted in further exclusion of 30 articles primarily due to the study locations [30, 43–70] (S3 Table). Ultimately, 31 studies met the eligibility criteria and were included in the final meta-analysis (see Fig 1).
Fig 1. Flow chart of study selection for systematic review and meta-analysis of the prevalence and determinants of diarrhea among under-five children in Ethiopia.
Description of included studies
As described in Table 1, the 31included studies were cross-sectional study design, and published between 2003 to 2017. In the current meta-analysis, 22,744 study participants were involved to determine the pooled prevalence of diarrhea among under-five children. Regarding sample size, the sample size of the studies ranged from 278 to1, 807. The lowest prevalence (8%) of under-five diarrhea was reported in studies conducted in Wolitta Soddo Town, Southern Nations, Nationalities, and Peoples Region (SNNPR) [32] and Mecha District, Amhara region [28]whereas the highest prevalence (37%) was reported in a study conducted in a rural Dire Dawa [18]. In the present meta-analysis, six Ethiopian regions and two administrative towns were represented. Ten of the studies were from Amhara [19, 24, 25, 28, 31, 71–75], five from SNNPR [20, 26, 32, 76, 77], five from Oromia [17, 18, 21, 22, 78], three from Afar [13, 79, 80], three from Addis Ababa [12, 15, 29], two from Tigray [14, 81], two from Somali [23, 82] and one from Dire Dawa [18]. No studies were reported from Benishangul Gumiz, Harari, and Gagmbela regions. Regarding to response rate, almost all studies had a good response rate (>85%), which may, in part be attributable to the use of interviewer-administered questionnaires to collect the data (Table 2).
Table 2. Descriptive summary of 31 studies included in the meta-analysis of the prevalence and determinants of diarrhea among under-five children in Ethiopia 2017.
| No | Author | Publication Year | Region | Study Area | Sample Size | Response Rate | Prevalence with 95% |
|---|---|---|---|---|---|---|---|
| 1. | Hailemariam Berhe[81] | 2016 | Tigra | Enderta | 278 | 94.2 | 36 (30, 41) |
| 2. | Mohammed et al [20] | 2013 | SNNPR | Arba Minch | 590 | 100 | 31 (27, 34) |
| 3. | Mohammed and Zungu[21] | 2016 | Oromia | Sebeta | 477 | 100 | 10 (7, 13) |
| 4. | Mengistie et al [22] | 2013 | Oromia | Kersa District | 1456 | 97.8 | 16 (14, 18) |
| 5. | Woldu et al [13] | 2016 | Afar | Hadaleala District | 704 | 100 | 26 (23, 30) |
| 6. | Regassa and Lemma [16] | 2016 | Oromia | Adama Rural District | 442 | 100 | 15 (12, 18) |
| 7. | Teklit Angesom[14] | 2015 | Tigray | Laelay-Maychew District | 543 | 100 | 18 (15, 21) |
| 8. | Dessalegn et al [28] | 2011 | Amhara | Mecha District | 768 | 100 | 8 (6, 10) |
| 9. | Gedamu et al [25] | 2017 | Amhara | FartaWereda | 988 | 99 | 17 (15, 19) |
| 10. | Zeleke and Alemu [12] | 2014 | Addis Ababa | Yeka Sub City | 350 | 100 | 33 (29, 39) |
| 11. | Anteneh et al [31] | 2017 | Amhara | Jabithennan District | 775 | 99.2 | 25 (22, 28) |
| 12. | Gedefaw et al [24] | 2015 | Amhara | Bahir Dar | 667 | 99.1 | 22 (19, 25) |
| 13. | Tadesse Yared[15] | 2016 | Addis Ababa | Yeka Sub City Woreda 3 | 399 | 99.7 | 9 (6, 11) |
| 14. | Hashi et al [23] | 2016 | Somalia | Jigjiga District | 1807 | 100 | 27 (25, 29) |
| 15. | Alambo Kedir Addisu[32] | 2015 | SNNPR | Wolitta Soddo Town | 954 | 98.4 | 8 (6, 10) |
| 16. | Regassa et al [17] | 2008 | Oromia | Nekemte Town | 461 | 96.6 | 29 (25, 33) |
| 17. | Demelash Ayele[29] | 2014 | Addis Ababa | Addis Ababa | 348 | 83.3 | 30 (25, 35) |
| 18. | Jamboree et al [26] | 2016 | SNNPR | Gummer Woreda, Guragie | 611 | 96.4 | 15 (12, 18) |
| 19. | Mulugeta Teklu[19] | 2003 | Amhara | Meskanena Mareko Woreda | 987 | 100 | 22 (20, 25.0) |
| 20. | Keneni et al [18] | 2016 | Dire Dawa | Dire Dawa Rural District | 291 | 98.6 | 37 (32, 43) |
| 21. | Gebru et al [77] | 2014 | SNNPR | Sheko Rural District | 792 | 96 | 19 (17, 22) |
| 22. | Awoke [72] | 2013 | Amhara | Bahir Dar Town | 415 | 98.34 | 27 (22, 31) |
| 23. | Tamiso et al [76] | 2014 | SNNPR | rural area of Shebedino | 769 | 98.8 | 20 (17, 23) |
| 24. | Mamo and Hailu [71] | 2014 | Amhara | Debre Birehan Town | 483 | 100 | 32 (28, 36) |
| 25. | Bitew et al [80] | 2017 | Afar | Hadaleala District | 704 | NR | 26 (23, 30) |
| 26. | Gizaw et al [79] | 2017 | Afar | Hadaleala District | 367 | 100 | 31 (27, 36) |
| 27. | Ayele et al [74] | 2014 | Amhara | Enemay District | 634 | 100 | 19 (16, 22) |
| 28. | Mekasha and Tesfahun[78] | 2003 | Oromia | Jimma Town | 605 | NR | 23 (20, 27) |
| 29. | Alelign et al [75] | 2016 | Amhara | Debre Birehan Town | 312 | NR | 12 (9, 16) |
| 30. | Getu et al [73] | 2014 | Amhara | Dejen District | 710 | 96.5 | 24 (21, 27) |
| 31. | Bizuneh et al [82] | 2017 | Somali | Jigjig Town | 492 | 92.8 | 15 (12, 18) |
NR: not reported, SNNPR: Southern Nations, Nationalities, and Peoples Region.
Risk of bias
The risk of bias for each original study was conducted using a risk of bias tool which encompassed ten different items [39]. Among the 31 included studies, our summary assessment revealed that more than three fourth (77.4%) of the included studies had low risk of bias [12–14, 17–19, 22–26, 28, 29, 32, 71, 73–80, 82] whereas, about 16.1% of the included studies had moderate risk of bias [15, 16, 21, 31, 72] the remaining, 6.5% of the studies had high risk of bias [20, 81].
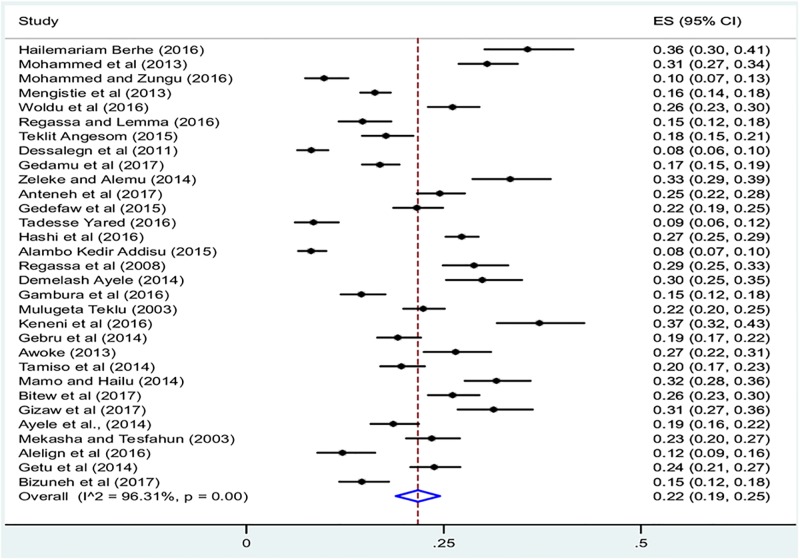
Prevalence of diarrhea among under-five children in Ethiopia
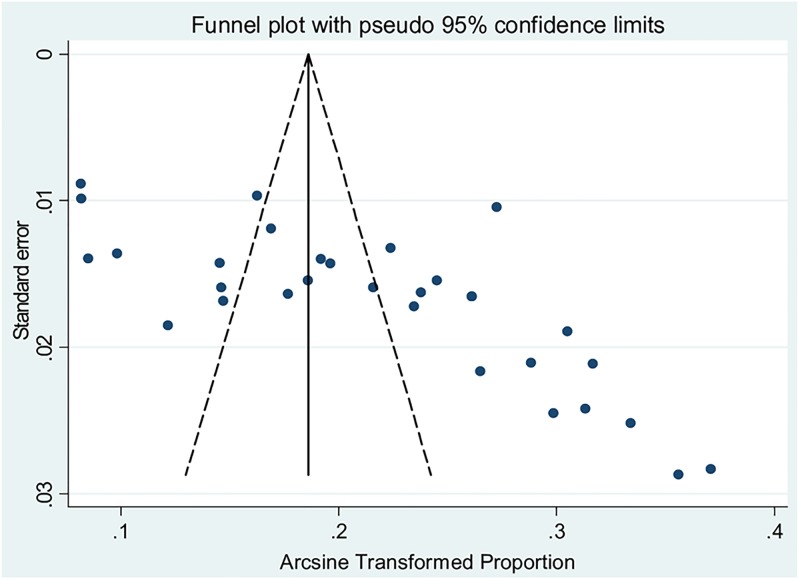
The 31 included studies revealed that a pooled prevalence of under-five diarrhea in Ethiopia was 22% (95%CI: 19, 25) (Fig 2). High heterogeneity was observed across the included studies (I2 = 96.31, p<0.001). Therefore, a random effect meta-analysis model was computed to estimate the pooled prevalence of under-five diarrhea in Ethiopia. From this meta-analysis, the highest prevalence was 37% (95%CI: 32, 43) reported in a study by Keneni et al [18]whereas the lowest prevalence of 8% was reported elsewhere [28, 32]. To identify possible sources of heterogeneity, different factors associated with heterogeneity, such as year of publication, quality score, region of the country where the study conducted and sample size, were investigated by using univariate meta-regression models, although none of these variables were found to be statistically significant (Table 3). Funnel plot asymmetry was used to check the presence of publication bias (Fig 3). The result of funnel plot showed that there was a slight asymmetrical distribution of articles. To confirm this asymmetry, we conducted an objective (Begg’s and Egger’s tests) based tests. The results of Begg’s and Egger’s tests showed that there was no statistical significant publication bias in estimating the prevalence of diarrhea among under-five children [(p = 0.2) and (p = 0.4) respectively].
Fig 2. Forest plot of the pooled prevalence of diarrhea among under-five children in Ethiopia.
Table 3. Related factors with heterogeneity of diarrheal prevalence among under-five children in the current meta-analysis (based on univariate meta-regression).
| Variables | Coefficient | P-value |
|---|---|---|
| Publication year | -0.17 | 0.70 |
| Sample size | -0.004 | 0.30 |
| Quality score | 0.006 | 0.98 |
| Regions | ||
| Addis Ababa | -2.44 | 0.72 |
| Afar | 1.73 | 0.80 |
| Amhara | -5.51 | 0.33 |
| Oromia | -7.53 | 0.23 |
| SNNPR | -7.76 | 0.22 |
| Tigray | 0.22 | 0.97 |
| Somali and Dire Dawa (Constant) | 26.01 | <0.001 |
Fig 3. Funnel plot with 95% confidence limits of the pooled prevalence of diarrhea among under-five children in Ethiopia.
Subgroup analysis
In this meta-analysis, we performed subgroup analysis based on the region of the country where studies were conducted as well as sample size. Accordingly, the highest prevalence was observed in Afar region with a prevalence of 27% (95% CI: 25, 30) followed by Somali and Dire Dawa regions at 26% (95% CI: 15, 37) and then Addis Abeba at 24% (95% CI: 7, 41). With regard to sample size, the prevalence of diarrhea was higher in studies having a sample of size<670, 23% (95% CI: 19, 27) compared to those having a sample size> = 670, 20% (95%CI: 16, 24) (Table 4).
Table 4. Subgroup prevalence of diarrhea among under-five children in Ethiopia, 2017 (n = 31).
| Variables | Characteristics | Included studies | Sample size | Prevalence with (95% CI) |
|---|---|---|---|---|
| By region | Amhara | 10 | 6,714 | 21 (16, 25) |
| Oromia | 5 | 3,441 | 18 (13, 24) | |
| Afar | 3 | 1,775 | 27 (25, 30) | |
| Addis Ababa | 3 | 1,079 | 24 (7, 41) | |
| SNNPR | 5 | 3,716 | 18 (11, 25) | |
| Tigray | 2 | 821 | 22 (19, 25) | |
| Somali and Dire Dawa | 3 | 2,590 | 26 (15, 37) | |
| By sample size | > = 670 | 12 | 10,704 | 20 (16,24) |
| <670 | 19 | 6,722 | 23 (19, 27) | |
| Overall | 31 | 22,744 | 22(19, 25) |
Determinants of under-five diarrhea in Ethiopia
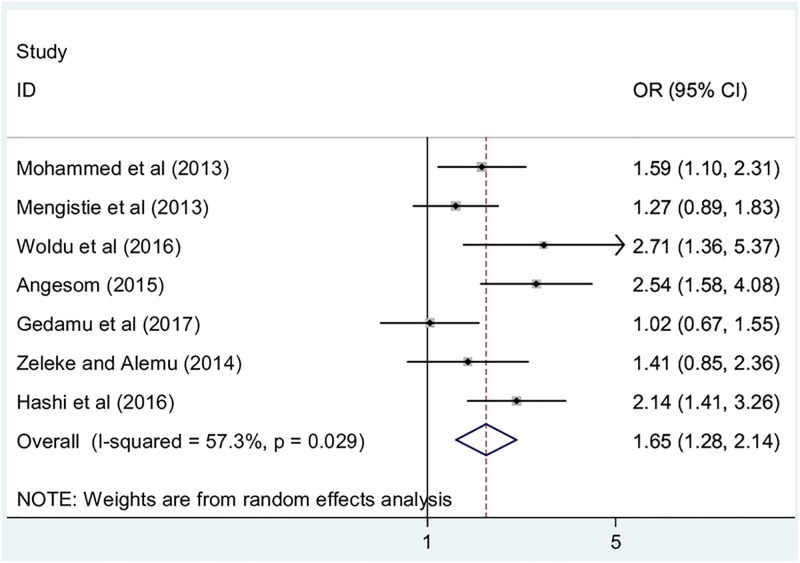
The association between maternal education and childhood diarrhea
In this meta-analysis, we examined association between maternal educational status and childhood diarrhea by using seven studies [12–14, 20, 22, 23, 25]. The findings from these seven studies revealed that the occurrence of childhood diarrhea was significantly associated with mothers’ educational status. Accordingly, the likelihood of diarrhea occurrence was 1.7 times higher among children whose mothers’ were unable to read and write as compared to their literate counterparts (OR: 2.5, 95% CI: 1.3, 2.1). The result of the test statistics indicated that moderate heterogeneity (I2 = 57.3% and p = 0.03) was presented across the included studies. Therefore, a random effect meta-analysis model was employed to determine the association(Fig 4).
Fig 4. The pooled odds ratio of the association between maternal education and childhood diarrhea in Ethiopia.
Association between latrine availability and childhood diarrhea
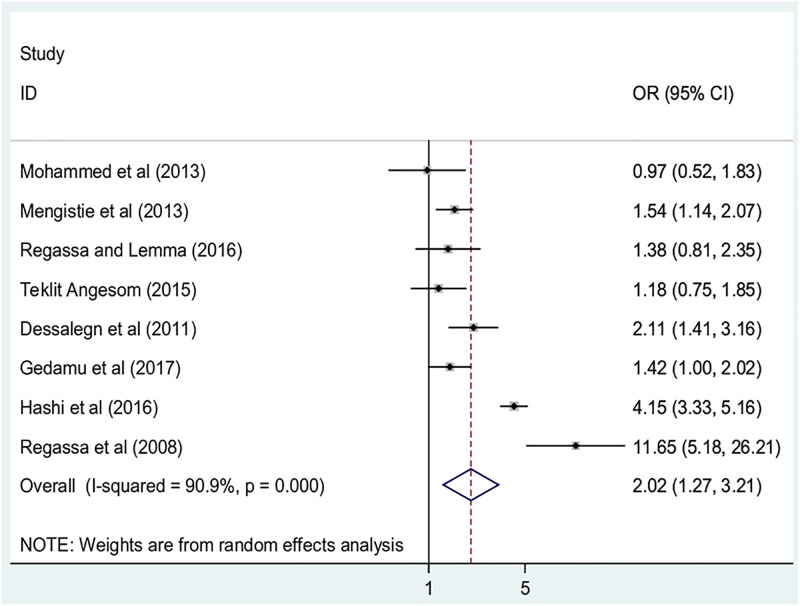
Similarly, the association between the availability of any type of latrine and childhood diarrhea was examined by using eight studies [14, 16, 17, 20, 22, 23, 25, 28]. Four of the included studies reported that the availability of any type of latrine were not significantly associated with childhood diarrhea [14, 16, 20, 25] whereas, four indicated that absence of any type of latrine was positively associated with childhood diarrhea [17, 22, 23, 28]. The result of this meta-analysis revealed that the absence of any type of latrine was positively associated with childhood diarrhea. From this result, children living in households without latrine facilities were found to be 2.0 times more likely to develop diarrhea than children living in households with such facilities (OR: 2.0, 95%; CI: 1.3, 3.2) (Fig 5). The included studies exhibited high heterogeneity (I2 = 90.9% and p< 0.001), hence random effect meta-analysis was computed.
Fig 5. The pooled odds ratio of the association between latrine availability and childhood diarrhea in Ethiopia.
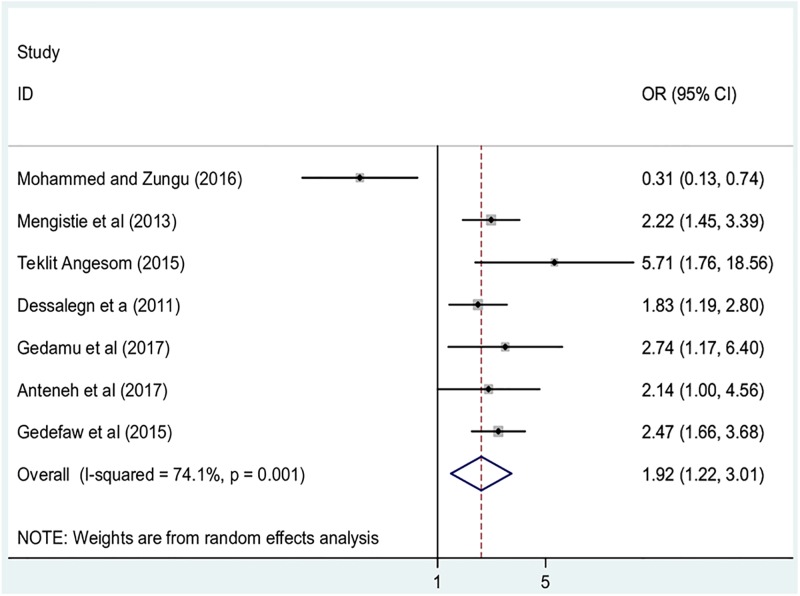
Association between residence and childhood diarrhea
To examine the association between residence and childhood diarrhea, studies that examined the association between respondents’ residences and under-five diarrhea were included [14, 21, 22, 24, 25, 28, 31]. According to Mohammed and Zungu [21], children from households of rural households were less likely to have diarrhea than their urban counterparts. Conversely, five studies disclosed that children from rural households were more likely to have diarrhea as compared to children from urban households [14, 22, 24, 25, 28]. One study [31]found residence was not significantly associated with childhood diarrhea. The pooled result of this meta-analysis indicated that children from rural households were 1.9 times more likely to have diarrhea as compared to their urban counterparts (OR: 1.9, 95%CI: 1.2, 3.0) (Fig 6). In this meta-analysis, included studies were characterized by high heterogeneity (I2 = 74.1%; p = 00.1), we computed a random effect meta-analysis.
Fig 6. The pooled odds ratio of the association between residence and childhood diarrhea in Ethiopia.
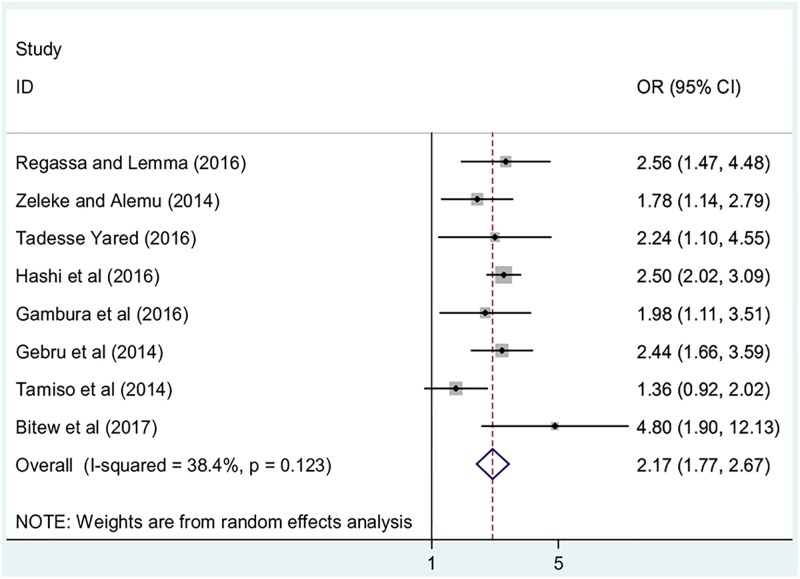
Association between maternal hand washing practices and childhood diarrhea
Finally, in this review, we examined the association between mothers’ hand washing practices and childhood diarrhea. Eight studies that examined the association between childhood diarrhea and mothers hand washing practice were included. Seven studies indicated that mothers’ hand washing practice after toilet visiting was significantly associated childhood diarrhea [12, 15, 16, 23, 26, 80]. These studies reported that mothers who did not practice hand washing after visiting a toilet were positively associated with childhood diarrhea. One study reported that mothers’ hand washing practices were not significantly associated with diarrhea [76]. The overall result of this study revealed that children whose mothers did not practice hand washing after visiting a toilet were 2.3 more likely to develop diarrhea as compared to their counterparts (OR: 2.2, 95%CI: 2.0, 2.6) (Fig 7). Moderate heterogeneity (I2 = 38.4%; p-value = 0.12) was observed among the included studies; hence, a random effect meta-analysis model was employed to estimate the final analysis.
Fig 7. The pooled odds ratio of the association between maternal hand washing practices and childhood diarrhea in Ethiopia.
Discussion
Diarrhea is one of the major causes of morbidity and mortality among under-five children in Ethiopia. Based on the WHO estimates, diarrhea contributes to more than one in every ten (13%) child deaths in Ethiopia [83]. Estimating the pooled prevalence of under-five diarrhea and its contributing factors in Ethiopia may contribute to informing policy makers. To the best our knowledge, this meta-analysis is the first of its kind to estimate the pooled prevalence of diarrhea and its determinants among under-five children in Ethiopia.
The overall prevalence of under-five diarrhea obtained from this study indicated that almost one in five (22%; 95% CI: 19, 25) children under the age of five in Ethiopia experienced diarrhea. The result of this meta-analysis is in line with the 2000 Ethiopian DHS [84, 85] report, which shows the prevalence of diarrhea as 24%. However, this finding is almost two times higher than the 2011 Ethiopian DHS, which suggests 13% of under-five children had diarrhea [86]. In addition, this finding is much higher than 2016 Ethiopian DHS [10]and 2005 [87] reports with reported prevalence of childhood diarrhea of 12% and 18% respectively. Similarly, our finding is two times higher than Ghana’s 2014 DHS (12%) [88], higher than Kenya’s 2014 DHS finding of 15% [89]. The possible explanation for the above variation could be attributed to methodological variation in the assessment of prevalence. The difference in the prevalence of diarrhea between our study and other sub-Saharan countries could be explained by the difference in socio-demographics and sociocultural practices, which has a great impact on child feeding.
The subgroup analysis of this study indicated that the highest prevalence of diarrhea was observed in Afar region, 27% (95% CI: 25, 30) followed by Somali and Dire Dawa regions, 26% (95% CI: 15, 37) whereas the lowest prevalence was observed in Oromia and SNNPR with prevalences of 18% (95%CI: 13, 24) and 18% (95%CI: 11, 25) respectively. This finding of this study is in agreement with the 2011 Ethiopian DHS, which shows Somali region (19.5%) has higher prevalence of diarrhea next to Benishangul-Gumuz (22.7%) and Gambela (22.6%) regions [86]. The possible explanations for this variation might be due to the difference in basic environmental and behavioral characteristics of caregivers. Another possible explanation for this variation could be due to the difference in the socio-demographic, environmental, and behavioral characteristics of households. As the communities living in Somali and Afar regions were nomadic, they go from place to place in search of pasture and water. They have no permanent residential places, hence, lacking access to basic healthcare facilities and sanitation services. The main sources of water for these populations were rivers, streams, and wells that are high risk for contamination. In addition, those populations more commonly practicing open defecation, which leads to the living environment, is polluted with human excreta that are the main source of diarrheal disease, especially for the children who routinely play in the unhygienic environment. Moreover, people suffering from illiteracy and poverty, which, in turn, deteriorates their quality of life. All these phenomena are the direct risk factors for the occurrence of childhood diarrheal disease [90]
The present study was also aimed to identify the determinants of diarrhea among under-five children in Ethiopia. In this study, lack of maternal education, lack of availability of latrine, urban residence, and lack of maternal hand washing were significantly associated with childhood diarrhea. The likelihood of diarrhea occurrence was 1.7 times higher among children whose mothers were unable to read and write as compared to their counterparts. The finding of this study is consistent with studies done in Ghana and Nigeria, which showed that the prevalence of diarrhea was significantly, varieties in related to the caregiver’s educational status. These studies reported that diarrhea was higher among children whose mothers have no formal education [91–93]. This finding may relate to these educated mothers have better knowledge about the rules of hygiene, appropriate child feeding practices, and early signs and symptoms of diarrhea which are the major determinant factors for the occurrence of childhood diarrhea. In addition, education has a great impact in changing behaviors at the household level. Moreover, education may increase the mother’s awareness about methods of transmission and prevention of diarrhea.
Latrine availability was another determinant of under-five diarrhea. Accordingly, children living in households without latrine facilities were 2.0 times more likely to develop diarrhea than children living in households with such facilities. This finding is congruent with a study conducted in Tanzania [94]. Different studies also reported that the absence of latrine facility was strongly associated with the occurrence of diarrheal disease [69, 70, 95]. The accessibility to a latrine in the family unit is an indication of sanitation conditions, which will have an implications to prevent the possibility of transmission of pathogens through fecal contamination [96].
Furthermore, it is indicated that children living in rural areas were more vulnerable to diarrhea than their urban counterparts. Children from rural households were 1.9 times more likely to have diarrhea as compared to their counterparts. This finding is contradictory to a study reported from Iraq [97]; however, similar to a study conducted in Pakistan [98]. This variance could be due to the population living in urban areas having better access to an improved water source, sanitation facility, health care facility and better knowledge about the prevention and control of diarrheal disease in comparison to rural populations. Another possible reason could be that people living in rural areas tend to be poorer than their urban counterparts are, a factor known to have an impact on the level of hygienic practice.
Lastly, lack of maternal hand washing was significantly associated with childhood diarrhea. Children whose mothers did not practice hand washing after visiting a latrine were 2.3 more likely to develop diarrhea as compared to their counterparts. This finding to those of a study conducted in Nigeria [91]. The rationale for hand washing after going to latrine to reduce the load of microorganisms has been well documented as fecal-oral microorganism transmissions due to post-defecation contamination of hands and fingers is well known [20, 22, 77, 99]. As mothers are the most frequent primary caregivers for their children, it is important to assess the contribution of maternal hand washing practices.
Limitations of the study
This meta-analysis has several limitations. The first limitation of this study was only English articles or reports were considered to conduct this nationally based review. In addition, all of the studies included in this review were cross-sectional in nature; as a result, the outcome variable might be affected by other confounding variables. The majority of the studies included in this review had a relatively small sample size, which could affect the estimated prevalence reported. Almost all research included in this meta-analysis used the WHO tool for diarrheal assessment, its occurrence was determined based on the reports of mothers without the confirmation of physicians. Therefore, this result might be affected social desirability bias. Furthermore, this meta-analysis represented only studies reported from six regions and two administrative town of the country, which may reflect under-representation due to the limited number of studies included.
Conclusion
In this study, diarrheal disease among under-five children in Ethiopia was significantly high. In addition, childhood diarrhea is significantly higher in nomadic population. Lack of maternal education, lack of availability of latrine, urban residence, and lack of maternal hand washing found significantly associated with childhood diarrhea. Therefore, based our findings, we recommend particular emphasis shall be given to the rural communities. Moreover, health educations about personal hygiene as well as, proper disposal of wastes including excreta in integration with the existing national health extension program are recommended.
Supporting information
(DOC)
(XLSX)
(DOCX)
Abbreviations
- CI
Confidence Interval
- DHS
Demographic and Health Survey
- EDHS
Ethiopia Demographic and Health Survey
- OR
Odds ratio
- SDG
Sustainable Development Goals
- SNNPR
Southern Nations, Nationalities, and Peoples Region
- WHO
World Health Organization
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Tsinuel G, Habtamu F, Goitom GY, Assfawossen B, Mekete L, Wogene T et al: Paediatrics and child health lecture note for health science students unpublished source
- 2.Gidudu J, Sack D, Pina M, Hudson M, Kohl K, Bishop P et al. : Diarrhea: case definition and guidelines for collection, analysis, and presentation of immunization safety data. Vaccine 2011, 29(5):1053–1071. doi: 10.1016/j.vaccine.2010.11.065 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization: Children: reducing mortality fact sheet http://www.who.int/mediacentre/factsheets/fs178/en/. 2017.
- 4.Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE et al. : Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet 2015, 385(9966):430–440. [DOI] [PubMed] [Google Scholar]
- 5.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG et al. : Global, regional, and national causes of child mortality in 2008: a systematic analysis. The Lancet 2010, 375(9730):1969–1987. [DOI] [PubMed] [Google Scholar]
- 6.Lomazzi M, Borisch B, Laaser U: The Millennium Development Goals: experiences, achievements and what’s next. Global health action 2014, 7(1):23695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization: Children: reducing mortality fact sheet http://www.who.int/mediacentre/factsheets/fs178/en/. In.; Updated October 2017.
- 8.Boschi-Pinto C, Velebit L, Shibuya K: Estimating child mortality due to diarrhoea in developing countries. Bulletin of the World Health Organization 2008, 86(9):710–717. doi: 10.2471/BLT.07.050054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization: Global Health Observatory (GHO) data under-five mortality http://www.who.int/gho/child_health/mortality/mortality_under_five_text/en/.
- 10.Central Statistical Agency: Ethiopia Demographic and Health Survey https://dhsprogram.com/publications/publication-fr328-dhs-final-reports.cfm. In.; 2016.
- 11.Bilal NK, Herbst CH, Zhao F, Soucat A, Lemiere C: Health extension workers in Ethiopia: improved access and coverage for the rural poor. Yes Africa Can: Success Stiroes from a Dynamic Continent 2011:433–443. [Google Scholar]
- 12.Zeleke AT, Alemu ZA: Determinants of under-five childhood diarrhea in Kotebe Health Center, Yeka Sub City, Addis Ababa, Ethiopia: a case control study. Global Journal of Medical Research 2014. [Google Scholar]
- 13.Woldu W, Bitew BD, Gizaw Z: Socioeconomic factors associated with diarrheal diseases among under-five children of the nomadic population in Northeast Ethiopia. Tropical Medicine and Health 2016, 44(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teklit Angesom ND, Samson Wakuma: Prevalence and associated factors of diarrhea among Under-five children in Laelay-Maychew District, Tigray region, Ethiopia 2015.
- 15.Tadesse Yared: Assessment of prevalence and associated Factors of Diarrheal Diseases among Under-Five Years Children living in Woreda 03 Residence of Yeka sub city, Addis Ababa Ethiopia. ADDIS ABABA UNIVERSITY; 2016. [Google Scholar]
- 16.Regassa W, Lemma S: Assessment of Diarrheal Disease Prevalence and Associated Risk Factors in Children of 6–59 Months Old at Adama District Rural Kebeles, Eastern Ethiopia, January/2015. Ethiopian Journal of Health Sciences 2016, 26(6):581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Regassa G, Birke W, Deboch B, Belachew T: Environmental determinants of diarrhea among under-five children in Nekemte town, western Ethiopia. Ethiopian Journal of Health Sciences 2008, 18(2). [Google Scholar]
- 18.Nagga B, Dejene K, Tadesse A: Prevalence and Associated Factors of Diarrhea Morbidity Among-Under Five Children in Rural Kebeles Of Dire Dawa Administration, Ethiopia. Harmaya University; 2016. [Google Scholar]
- 19.Mulugeta Teklu: Socio-Economic, Environmental, And Behavioural Factors Associated With The Occurrence Of Diarrhoeal Disease Among Under-Five Children. Adis Ababa 2003. [Google Scholar]
- 20.Mohammed S, Tilahun M, Tamiru D: Morbidity and associated factors of diarrheal diseases among under five children in Arba-Minch district, Southern Ethiopia, 2012. Science Journal of Public Health 2013, 1(2):102–106. [Google Scholar]
- 21.Mohammed AI, Zungu L: Environmental health factors associated with diarrhoeal diseases among under-five children in the Sebeta town of Ethiopia. Southern African Journal of Infectious Diseases 2016, 31(4):122–129. [Google Scholar]
- 22.Mengistie B, Berhane Y, Worku A: Prevalence of diarrhea and associated risk factors among children under-five years of age in Eastern Ethiopia: A cross-sectional study. Open Journal of Preventive Medicine 2013, 3(07):446. [Google Scholar]
- 23.Hashi A, Kumie A, Gasana J: Prevalence of Diarrhoea and Associated Factors among Under-Five Children in Jigjiga District, Somali Region, Eastern Ethiopia. Open Journal of Preventive Medicine 2016, 6(10):233–246. [Google Scholar]
- 24.Gedefaw M, Takele M, Aychiluhem M, Tarekegn M: Current status and predictors of diarrhoeal diseases among under-five children in a rapidly growing urban setting: the case of city administration of Bahir Dar, northwest Ethiopia. Open Journal of Epidemiology 2015, 5(02):89. [Google Scholar]
- 25.Gedamu G, Kumie A, Haftu D: Magnitude and Associated Factors of Diarrhea among Under Five Children in Farta Wereda, North West Ethiopia. Quality in Primary Care 2017, 25(4). [Google Scholar]
- 26.Gambura E, Birke W, Terefe G, Yohanes T, Laelago T: Behavioral Factors Associated with Under-Five Diarrhoeal Morbidity in Rural Community of Gummer Woreda, Gurage Zone, Southern Ethiopia: Community Based Cross-Sectional Study. Open Access Library Journal 2016, 3(04):1. [Google Scholar]
- 27.Ephrem Mamo Gebrehiwot, TM B, Alemayehu Worku, Tadele Dana Darebo, Ephrem Lejore Sibamo: Childhood Diarrhea in Central Ethiopia: Determining Factors for Mothers in Seeking Modern Health Treatments Science Journal of Clinical Medicine 2015. [Google Scholar]
- 28.Dessalegn M, Kumie A, Tefera W: Predictors of under-five childhood diarrhea: Mecha District, West Gojam, Ethiopia. Ethiopian Journal of Health Development 2011, 25(3):192–200. [Google Scholar]
- 29.Demelash Ayele TB: Healthfaciltities based cross sectional study on prevalence and associted factors of diarrheal morbidity among under-five childern in armed forces teaching and referral hospital, signal and Gofa health centers Addis Ababa. 2014.
- 30.Bogale GG, Gelaye KA, Degefie DT, Gelaw YA: Spatial patterns of childhood diarrhea in Ethiopia: data from Ethiopian demographic and health surveys (2000, 2005, and 2011). BMC Infectious Diseases 2017, 17(1):426 doi: 10.1186/s12879-017-2504-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anteneh ZA, Andargie K, Tarekegn M: Prevalence and determinants of acute diarrhea among children younger than five years old in Jabithennan District, Northwest Ethiopia, 2014. BMC Public Health 2017, 17(1):99 doi: 10.1186/s12889-017-4021-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alambo Kedir Addisu: The Prevalence of Diarrheal Disease in under Five Children and associated Risk Factors in Wolitta Soddo Town, Southern, Ethiopia. ABC Research Alert 2015, 3(2). [Google Scholar]
- 33.WIKIPEDIA Geography of Ethiopia https://en.wikipedia.org/wiki/Geography_of_Ethiopia.
- 34.Ethiopia Population (LIVE) worldometers http://www.worldometers.info/world-population/ethiopia-population/.
- 35.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP et al. : The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology 2009, 62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 36.Moher D, Pham B, Lawson M, Klassen T: The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technology Assessment 2003, 7(41):1–90. [DOI] [PubMed] [Google Scholar]
- 37.UNICEF, WHO D: Why children are still dying and what can be done, The United Nations Children’s Fund https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=UNICEF%2FWHO.+Diarrhoea%3A+why+children+are+still+dying+and+what+can+be+done.+The+United+Nations+Children%E2%80%99s+Fund%2FWorld+Health+Organization%2C+Geneva%2C+2009. World Health Organization report 2009:1–60.
- 38.Black RE, Morris SS, Bryce J: Where and why are 10 million children dying every year? The Lancet 2003, 361(9376):2226–2234. [DOI] [PubMed] [Google Scholar]
- 39.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C et al. : Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. Journal of Clinical Epidemiology 2012, 65(9):934–939. doi: 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 40.Rücker G, Schwarzer G, Carpenter JR, Schumacher M: Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Medical Research Methodology 2008, 8:79 doi: 10.1186/1471-2288-8-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nyaga VN, Arbyn M, Aerts M: Metaprop: a Stata command to perform meta-analysis of binomial data. Archives of Public Health 2014, 72(1):39 doi: 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Borenstein M, Hedges LV, Higgins J, Rothstein HR: A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods 2010, 1(2):97–111. doi: 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 43.Warsame HA, Chomi E, Ngwatu P: Influence of Health System Factors on Morbidity of Diarrheal Disease among Under Five Years Children Living in Internally Displaced Population Camps of Hodan District, Mogadhishu-Somalia. The Journal of Global Health Care Systems 2016, 6(2). [Google Scholar]
- 44.Uwizeye D, Sokoni CH, Kabiru CW: Prevalence and correlates for diarrhoea in the mountainous informal settlements of Huye town, Rwanda. SpringerPlus 2014, 3(1):745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Teklemariam S, Getaneh T, Bekele F: Environmental determinants of diarrheal morbidity in under-five children, Keffa-Sheka zone, south west Ethiopia. Ethiopian Medical Journal 2000, 38(1):27–34. [PubMed] [Google Scholar]
- 46.Tambe AB, Nzefa LD, Nicoline NA: Childhood Diarrhea Determinants in Sub-Saharan Africa: A Cross Sectional Study of Tiko-Cameroon. Challenges 2015, 6(2):229–243. [Google Scholar]
- 47.Siziya S, Muula A, Rudatsikira E: Correlates of diarrhoea among children below the age of 5 years in Sudan. African Health Sciences 2013, 13(2):376–383. doi: 10.4314/ahs.v13i2.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sayed YN, El-Sayed AZM, El-Fattah SAA: Effect of socioeconomic status on infectious diarrhea in Egyptian children.
- 49.Osman F, Abdirisaq H, Abdirahman M, Sayid M: Factors Influencing the Occurrence of Diarrhoea Among Children Under the Age of Five Admitted to Benadir Hospital Mogadishu-Somalia. JAMHURIYA UNIVERSITY:1.
- 50.Olango P, Aboud F: Determinants of mothers’ treatment of diarrhea in rural Ethiopia. Social Science and Medicine 1990, 31(11):1245–1249. [DOI] [PubMed] [Google Scholar]
- 51.Mulatu G, Beyene G, Zeynudin A: Prevalence of Shigella, Salmonella and Campylobacter species and their susceptibility patters among under five children with diarrhea in Hawassa town, south Ethiopia. Ethiop J Health Sci 2014, 24(2):101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mitike G: Prevalence of acute and persistent diarrhoea in north Gondar zone, Ethiopia. East African Medical Journal 2001, 78(8):433–438. [DOI] [PubMed] [Google Scholar]
- 53.Mekasha A, Tesfahun A: Determinants of diarrhoeal diseases: a community based study in urban south western Ethiopia. East African Medical Journal 2003, 80(2):77–82. [DOI] [PubMed] [Google Scholar]
- 54.Kelly P, Khanfir H, David PH, Arata M, Kleinau EF: Environmental and behavioral risk factors for diarrheal diseases in childhood: a survey in two towns in Morocco In: EHP Applied Study. Volume 79, edn.: EHP; 1999. [Google Scholar]
- 55.Karambu S, Matiru V, Kiptoo M, Oundo J: Characterization and factors associated with diarrhoeal diseases caused by enteric bacterial pathogens among children aged five years and below attending Igembe District Hospital, Kenya. Pan African Medical Journal 2013, 16:37 doi: 10.11604/pamj.2013.16.37.2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.ELMI O, DIOSO RP II: Prevalence of Diarrhoeal Diseases Among Children under Five Years in East African Countries from 2012–2017. ASEAN Journal on Science and Technology for Development 2017, 34(1):51–55. [Google Scholar]
- 57.Debajyoti M, Panza A: Demographic Socio-Economic and Environmental Factors Associated with Diarrhoea Morbidity in Children Under-Five in Rural Odisha: A Study of Rayagada District India. Journal of Health Research 2013, 27(6):375–381. [Google Scholar]
- 58.Danquah L, Mensah CM, Agyemang S, Awuah E: Risk factors associated with diarrhea morbidity among children younger than five years in the Atwima Nwabiagya District, Ghana: a cross-sectional study. Sci J Pub Health 2015, 3(3):344–352. [Google Scholar]
- 59.Carvajal-Velez L, Amouzou A, Perin J, Maiga A, Tarekegn H, Akinyemi A et al. : Diarrhea management in children under five in sub-Saharan Africa: does the source of care matter? A Countdown analysis. BMC Public Health 2016, 16:830 doi: 10.1186/s12889-016-3475-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Berhe F, Berhane Y: Under five diarrhea among model household and non model households in Hawassa, South Ethiopia: a comparative cross-sectional community based survey. BMC Public Health 2014, 14(1):187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Azage M, Haile D: Factors affecting healthcare service utilization of mothers who had children with diarrhea in Ethiopia: evidence from a population based national survey. Rural and remote health 2015, 15(3493). [PubMed] [Google Scholar]
- 62.Anteneh A, Kumie A: Assessment of the impact of latrine utilization on diarrhoeal diseases in the rural community of Hulet Ejju Enessie Woreda, East Gojjam Zone, Amhara Region. Ethiopian Journal of Health Development 2010, 24(2). [Google Scholar]
- 63.Mediratta RP, Feleke A, Moulton LH, Yifru S, Sack RB: Risk factors and case management of acute diarrhoea in North Gondar Zone, Ethiopia. J Health Popul Nutr 2010, 28(3):253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Godana W, Mengiste B: Environmental factors associated with acute diarrhea among children under five years of age in derashe district, Southern Ethiopia. Sci J Public Health 2013, 1(3):119–124. [PubMed] [Google Scholar]
- 65.Tesfaye F, Enquselassie F, Kebede F, Wendimagegn G: Usage of oral rehydration salt in acute childhood diarrhoea, Adami-Tullu Woreda. Ethiopian Medical Journal 1996, 34(3):163–171. [Google Scholar]
- 66.Eshete WB: A stepwise regression analysis on under-five diarrhoael morbidity prevalence in Nekemte town, western Ethiopia: maternal care giving and hygiene behavioral determinants. 2008. [DOI] [PubMed]
- 67.Ketsela T, Asfaw M, Belachew C: Knowledge and practice of mothers/care-takers towards diarrhoea and its treatment in rural communities in Ethiopia. Ethiopian Medical Journal 1991, 29(4):213–224. [PubMed] [Google Scholar]
- 68.Kakulu RK: Diarrhoea among under-five children and household water treatment and safe storage factors in Mkuranga district, Tanzania. Muhimbili University of Health and Allied Sciences; 2012. [Google Scholar]
- 69.Getaneh T, Assefa A, Tadesse Z: Diarrhoea morbidity in an urban area of southwest Ethiopia. East African Medical Journal 1997, 74(8):491–494. [PubMed] [Google Scholar]
- 70.Mock NB, Sellers TA, Abdoh AA, Franklin RR: Socioeconomic, environmental, demographic and behavioral factors associated with occurrence of diarrhea in young children in the Republic of Congo. Social Science and Medicine 1993, 36(6):807–816. [DOI] [PubMed] [Google Scholar]
- 71.Mamo A, Hailu A: Assessment of prevalence and related factors of diarrheal diseases among under-five year’s children in Debrebirehan Referral Hospital, Debrebirehan Town, North Shoa Zone, Amhara Region, Ethiopia. Open Access Library Journal 2014, 1(01):1. [Google Scholar]
- 72.Awoke W: Prevalence of childhood illness and mothers’/caregivers’ care seeking behavior in Bahir Dar, Ethiopia: A descriptive community based cross sectional study. Open Journal of Preventive Medicine 2013, 3(02):155. [Google Scholar]
- 73.Getu D, Gedefaw M, Abebe N: Childhood Diarrheal Diseases and Associated Factors in the Rural Community of Dejen District, Northwest Ethiopia. American Scientific Research Journal for Engineering, Technology, and Sciences (ASRJETS) 2014, 5(1):1–13. [Google Scholar]
- 74.Ayele A, Awoke W, Tarekegn M: Crossectional survey; Assessment of Diarrheal Disease Prevalence and the Associated Factors among Children under Five in Enemay District, Northwest Ethiopia. Global Journal of Medical Research 2014. [Google Scholar]
- 75.Alelign T A W, Abera A,: A Cross Sectional Study on the Incidence and Risk Factors of Diarrheal Illness among Children Under-five Years of Age in Debre Berhan Town, Ethiopia. Journal of Journal Journal of Health & Medical 2016, 2(2):12. [Google Scholar]
- 76.Tamiso A, Yitayal M, Awoke A: Prevalence and determinants of childhood diarrhoea among graduated households, in rural area of Shebedino district, Southern Ethiopia, 2013. Science 2014, 2(3):243–251. [Google Scholar]
- 77.Gebru T, Taha M, Kassahun W: Risk factors of diarrhoeal disease in under-five children among health extension model and non-model families in Sheko district rural community, Southwest Ethiopia: comparative cross-sectional study. BMC Public Health 2014, 14(1):395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mekasha A, Tesfahun A: Determinants of diarrhoeal diseases: a community based study in urban south western Ethiopia. East African Medical Journal 2003, 80(2):77–82. [DOI] [PubMed] [Google Scholar]
- 79.Gizaw Z, Woldu W, Bitew BD: Child feeding practices and diarrheal disease among children less than two years of age of the nomadic people in Hadaleala District, Afar Region, Northeast Ethiopia. Int Breastfeed J 2017, 12(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bitew BD, Woldu W, Gizaw Z: Childhood diarrheal morbidity and sanitation predictors in a nomadic community. Italian Journal of Pediatrics 2017, 43(1):91 doi: 10.1186/s13052-017-0412-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hailemariam Berhe AM, Gebre Yitayih: Prevalence of diarrhea and associated factors among children under-five years of age in enderta woreda, tigray, northern ethiopia, 2014. International Journal of Therapeutic Applications 2016, 31:32–37. [Google Scholar]
- 82.Bizuneh H, Getnet F, Meressa B, Tegene Y, Worku G: Factors associated with diarrheal morbidity among under-five children in Jigjiga town, Somali Regional State, eastern Ethiopia: a cross-sectional study. BMC Pediatrics 2017, 17(1):182 doi: 10.1186/s12887-017-0934-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Central Statistical Agency [Ethiopiaphic): Demographic and Health Survey Key Indicators https://dhsprogram.com/pubs/pdf/PR81/PR81.pdf. 2016.
- 84.EDHS: Ethiopia Mini Demographic and Health Survey Addis Ababa, Ethiopia. In. http://www.unicef.org/ethiopia/Mini_DHS_2014__Final_Report.pdf; 2014: 57.
- 85.Central Statistical Agency: Ethiopia Demographic and Health Survey https://dhsprogram.com/publications/publication-fr118-dhs-final-reports.cfm. 2000.
- 86.Centeral Statistics: Ethiopia Demographic and Health Survey http://www.unicef.org/ethiopia/ET_2011_EDHS.pd. In.; 20011.
- 87.Centeral Statistics: Ethiopia Demographic and Health Survey, 2005 https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=Ethiopia+Demographic+and+Health+Survey+2000&btnG=. In.: Central Statistical Authority; 2006.
- 88.Ghana Statistical Service Ghana Demographic and Health Survey 2014 https://dhsprogram.com/pubs/pdf/FR307/FR307.pdf. In. Edited by Ghana Statistical Service Accra G; 2015.
- 89.Kenya National Bureau of Statistics: Kenya Demographic and Health Survey 2014 https://dhsprogram.com/pubs/pdf/FR308/FR308.pdf. In.; 2015.
- 90.Ethiopia. Hadaleala District: Finance and economic development office annual report 2014, by Dawud Haji Alisadik and others, Hadaleala: Officer of finance and economic development Afar Region, Ethiopia. 2014.
- 91.Yilgwan CS, Okolo S: Prevalence of diarrhea disease and risk factors in Jos University Teaching Hospital, Nigeria. Annals of African Medicine 2012, 11(4):217 doi: 10.4103/1596-3519.102852 [DOI] [PubMed] [Google Scholar]
- 92.Yilgwan C, Yilgwan G, Abok I: Domestic water sourcing and the risk of diarrhea: a cross-sectional survey of a peri-urban community in Jos, Nigeria. Jos Journal of Medicine 2010, 5(1):34–37. [DOI] [PubMed] [Google Scholar]
- 93.Boadi KO, Kuitunen M: Childhood diarrheal morbidity in the Accra Metropolitan Area, Ghana: socio-economic, environmental and behavioral risk determinants. World Health & Population 2005. [Google Scholar]
- 94.Gascon J, Vargas M, Schellenberg D, Urassa H, Casals C, Kahigwa E et al. : Diarrhea in children under 5 years of age from Ifakara, Tanzania: a case-control study. Journal of Clinical Microbiology 2000, 38(12):4459–4462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.VanDerslice J, Popkin B, Briscoe J: Drinking-water quality, sanitation, and breast-feeding: their interactive effects on infant health. Bulletin of the World Health Organization 1994, 72(4):589 [PMC free article] [PubMed] [Google Scholar]
- 96.Stanly A, Sathiyasekaran B, Palani G: A population based study of acute diarrhoea among children under 5 years in a rural community in South India. Sri Ramachandra J Med 2009, 1(1):1–7. [Google Scholar]
- 97.Siziya S, Muula AS, Rudatsikira E: Diarrhoea and acute respiratory infections prevalence and risk factors among under-five children in Iraq in 2000. Italian Journal of Pediatrics 2009, 35(1):8 doi: 10.1186/1824-7288-35-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Arif A, Arif G: Socio-Economic Determinants of Child Health in Pakistan. Academic Research International 2012, 2(1):398. [Google Scholar]
- 99.Heller L, Colosimo EA, Antunes CMdF: Environmental sanitation conditions and health impact: a case-control study. Revista da Sociedade Brasileira de Medicina Tropical 2003, 36(1):41–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(XLSX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.