Abstract
Background
Cancer-patient navigators who are oncology nurses support and connect patients to resources throughout the cancer care trajectory, including end of life. Although qualitative and cohort studies of navigated patients have been reported, no population-based studies were found. The present population-based study compared demographic, disease, and outcome characteristics for decedents who had been diagnosed with cancer by whether they did or did not see a navigator.
Methods
This retrospective study used patient-based administrative data in Nova Scotia (cancer registry, death certificates, navigation visits) to generate descriptive statistics. The study population included all adults diagnosed with cancer who died during 2011–2014 of a cancer or non-cancer cause of death.
Results
Of the 7694 study decedents, 74.9% had died of cancer. Of those individuals, 40% had seen a navigator at some point in their disease trajectory. The comparable percentage for those who did not die of cancer was 11.9%. Decedents at the oldest ages had the lowest navigation rates. Navigation rates, time from diagnosis to death, and time from last navigation visit to death varied by disease site.
Conclusions
This population-based study of cancer-patient navigation enrolees compared with non-enrolees is the first of its kind. Most findings were consistent with expectations. However, we do not know whether the rates of navigation are consistent with the navigation needs of the population diagnosed with cancer. Because more people are living longer with cancer and because the population is aging, ongoing surveillance of who requires and who is using navigation services is warranted.
Keywords: Patient navigation, navigators, nurses, Nova Scotia, care access, end of life, demographics
INTRODUCTION
Patient navigation was introduced by Freeman and Rodriguez in New York in 1990 when Freeman noticed that poverty was associated with diminished access to health care, leading to worse cancer outcomes. Freeman and Rodriguez’s goal was to eliminate barriers to care for patients with a low socioeconomic status from the time of suspicion of cancer to diagnosis1. In time, the scope of navigation expanded to include the entire cancer trajectory from “prevention, detection, diagnosis, treatment, and survivorship to the end of life”1. Cancer patients find it challenging to navigate through complex health care systems and are often lost at transitions2. Many lack information and access to support systems, resulting in frustration and powerlessness3.
Most of the research into cancer-patient navigation (hereinafter called simply navigation) over past decades has focused on screening and diagnosis4,5, role clarity, improvement in quality of life, delivery of health and social services, and management of health needs6,7. Few studies have focused on the last phase of life5,8. A number of qualitative7 and intervention or disease cohort studies, including randomized trials8, have been carried out, but we found no population-based studies that identify the individuals who are and are not using navigation. Furthermore, the need for navigation might be changing, given the accelerating discovery of innovative cancer treatments, the fact that more people are living longer with cancer9, the current focus on narrowing the gap between oncology and primary care10,11, the aging of the population, and greater interest in advance care planning and a palliative approach to care12–14. Population-based surveillance of people with life-limiting conditions can provide evidence that will help in critically appraising established navigation programs.
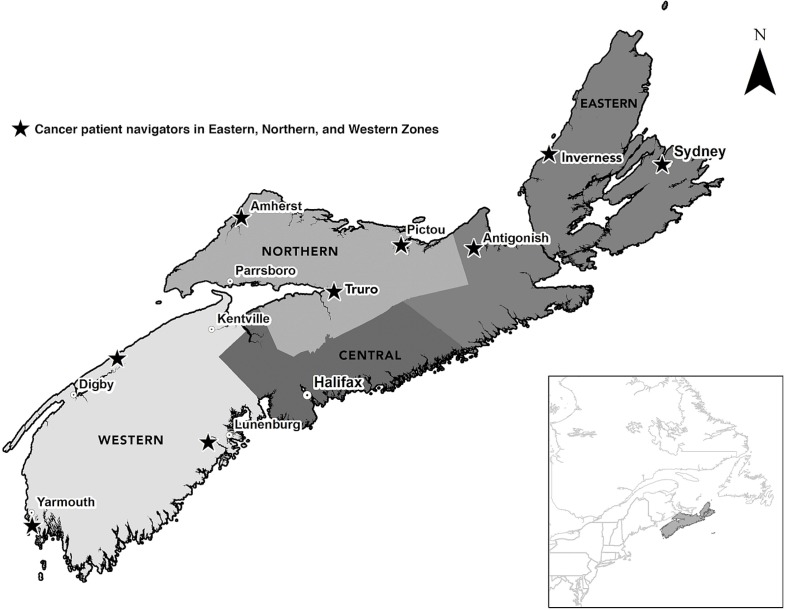
In Nova Scotia, cancer-patient navigation was implemented in the Western and Northern zones (Figure 1) between 2002 and 2009, and in all of the Eastern Zone by 2011. Nine community-based oncology-trained nurses provide support to patients and link them to cancer care and other professional services and volunteers, thus promoting coordination of, and access to, quality care. The resources are meant to meet physical, information, psychological, social, emotional, and practical patient needs at any time during their cancer journey from the diagnostic period to end of life15. They encompass three domains: patient education, psychosocial and practical support, and coordination of care. Navigation for adults was not available in the Central Zone for all cancer sites. For children and youth 0–18 years of age, family care coordinators at the children’s hospital provided some navigation functions and referrals to navigators.
FIGURE 1.
Nova Scotia zones and cancer-patient navigation.
Although few studies of navigation in relation to palliative and end-of-life care have been reported5,8, the population-based study design for investigating care for people at the end of life has been well established in Nova Scotia and elsewhere16–23. Nova Scotia is therefore an ideal setting to investigate use of navigation by people with cancer who are in their last phase of life.
The objective of the present study was to answer this question: Of individuals diagnosed with cancer who died in Nova Scotia during 2011–2014, how do adult decedents who were navigation enrolees differ from those who were not?
METHODS
This population-based retrospective descriptive study used administrative data from the person-based cancer registry information system managed by the Cancer Care Program of the Nova Scotia Health Authority. For cancer patients diagnosed since the early 1970s in Nova Scotia, the system contains information that was recorded in the population-based Nova Scotia Cancer Registry, death certificate information, and navigation visits. Approval for the study was received from the Nova Scotia Health Authority Research Ethics Board.
Study Population
The study population consisted of all adults 19 years of age and older who were diagnosed with invasive cancer in Nova Scotia and who died during 2011–2014 in the Western and Northern zones or during 2013–2014 in the Eastern Zone according to Vital Statistics death records. Decedents who died of cancer and of non-cancer causes were included. Death certificate–only cases (that is, people with a date of diagnosis that was also their date of death, n = 257) were excluded, as were the cases of people with a non-melanoma skin cancer diagnosis only (n = 76), because registration of non-melanoma skin cancers is not population-based, and very few people die of those cancers. Because end of life was the study focus, all study decedents were followed back in time from their date of death for a minimum of 1 year.
Variables
The demographic characteristics of the study decedents (age at death, sex, year of death, zone of residence at death), the presence of a cancer cause of death (either a primary or a secondary cause), and hospital as the place of death were obtained from death records. The status of a study decedent as a navigation enrolee was obtained from navigation records. Time from the last navigation visit to death was calculated as the interval between the date of the last navigation visit and the date of death. Time from the last cancer diagnosis to death was calculated as the interval between the date of the last cancer diagnosis and the date of death.
Study decedents could have had more than one invasive cancer diagnosis. Because end of life was the focus of the study, the last (closest to death) diagnosis was used to group the decedents by cancer diagnosis and stage. Cancer diagnoses were grouped using the categories in Canadian Cancer Statistics 2017 9, which uses the International Classification of Diseases for Oncology (3rd edition). For the present study, the focus was on the four most frequent diagnoses (breast, prostate, colorectal, and lung cancer)9; two other diagnoses with high mortality rates (pancreatic and esophageal cancer)9; a complex, high-needs diagnosis (head-and-neck cancer)24; and hematologic cancers for which the time of death is more difficult to predict25. The TNM best-stage group classification of the last invasive diagnosis was used. The Collaborative Stage Data Collection System26 was initiated in 2001 in Nova Scotia for colorectal cancer diagnoses and in 2003 for breast cancer diagnoses. Staging for the other cancer sites was introduced over time and has been available for all cancers since 2010. Whether the decedents had more than 1 invasive cancer diagnosis was obtained from the cancer registry.
Analysis
Microsoft Excel (Microsoft Corporation, Redmond WA, U.S.A.) was used to compute frequency counts and percentages for navigation use by enrolee characteristics, and medians and interquartile ranges (iqrs) for time periods. Those statistics were verified using the SAS statistical software application (SAS Institute, Cary, NC, U.S.A.). To protect the confidentiality of the study subjects, any variable with a count less than 5 is not reported. Chi-square calculations were carried out using the SAS statistical software application.
RESULTS
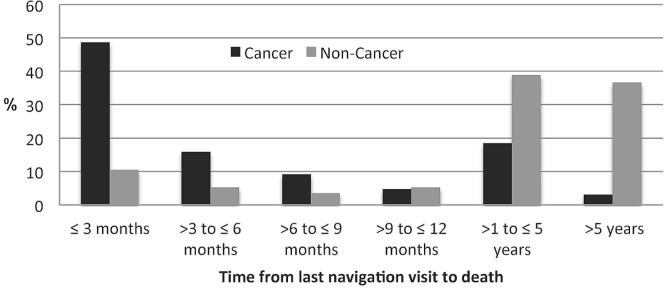
Of the 7694 study decedents, 32.9% were navigation enrolees (Table i) at some point in their cancer trajectory. Compared with those who did not die of cancer, those who died of cancer were more likely to have used navigation (40.0% vs. 11.9%). Most of the decedents died of cancer (5761, 74.9%), but a substantial number did not (1933, 25.1%). Figure 2 shows that those who died and did not die of cancer differed substantially in terms of the interval from their last navigation visit to death.
TABLE I.
Use of patient navigation by decedent category
| Cancer death? | Decedents (n) | Navigated [n (row %)] | |
|---|---|---|---|
|
| |||
| Yes | No | ||
| Yes | 5761 | 2302 (40.0) | 3,459 (60.0) |
| No | 1933 | 230 (11.9) | 1,703 (88.1) |
| TOTAL | 7694 | 2532 (32.9) | 5,162 (67.1) |
FIGURE 2.
Interval from last navigation to death, by cause of death.
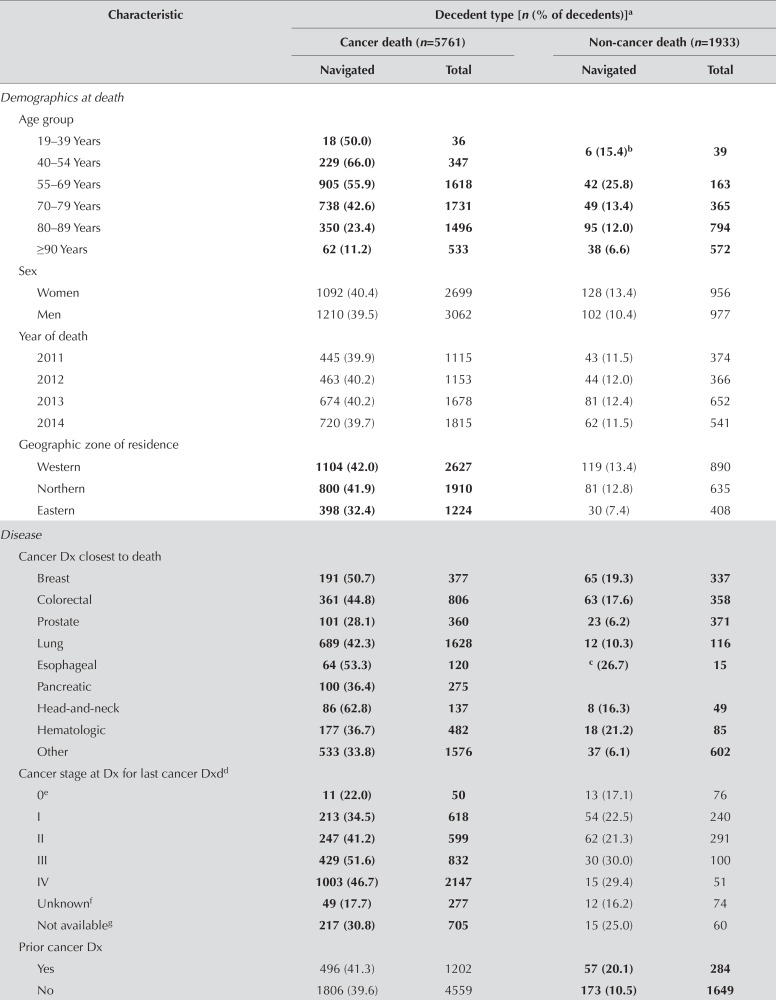
Demographic Characteristics
The use of navigation varied by decedent age whether the individual died of cancer or of non-cancer causes (Table ii). Among the individuals who died of cancer, those 40–54 years of age at death had the highest navigation use (66.0%), and those 90 years of age and older had the lowest use (11.2%). Among the individuals who died of non-cancer causes, those 55–69 years of age at death had the highest navigation rate (25.8%); that rate declined as age increased. Navigation rates did not meaningfully vary by sex or year of death. Navigation rates were lower for residents of the Eastern Zone (where navigation was most recently introduced) than for residents of the Western and Northern zones.
TABLE II.
Demographics, disease, and outcome characteristics by cause of death and navigation
| Characteristic | Decedent type [n (% of decedents)]a | |||
|---|---|---|---|---|
|
| ||||
| Cancer death (n=5761) | Non-cancer death (n=1933) | |||
|
|
|
|||
| Navigated | Total | Navigated | Total | |
| Demographics at death | ||||
| Age group | ||||
| 19–39 Years | 18 (50.0) | 36 | 6 (15.4)b | 39 |
| 40–54 Years | 229 (66.0) | 347 | ||
| 55–69 Years | 905 (55.9) | 1618 | 42 (25.8) | 163 |
| 70–79 Years | 738 (42.6) | 1731 | 49 (13.4) | 365 |
| 80–89 Years | 350 (23.4) | 1496 | 95 (12.0) | 794 |
| ≥90 Years | 62 (11.2) | 533 | 38 (6.6) | 572 |
| Sex | ||||
| Women | 1092 (40.4) | 2699 | 128 (13.4) | 956 |
| Men | 1210 (39.5) | 3062 | 102 (10.4) | 977 |
| Year of death | ||||
| 2011 | 445 (39.9) | 1115 | 43 (11.5) | 374 |
| 2012 | 463 (40.2) | 1153 | 44 (12.0) | 366 |
| 2013 | 674 (40.2) | 1678 | 81 (12.4) | 652 |
| 2014 | 720 (39.7) | 1815 | 62 (11.5) | 541 |
| Geographic zone of residence | ||||
| Western | 1104 (42.0) | 2627 | 119 (13.4) | 890 |
| Northern | 800 (41.9) | 1910 | 81 (12.8) | 635 |
| Eastern | 398 (32.4) | 1224 | 30 (7.4) | 408 |
| Disease | ||||
| Cancer Dx closest to death | ||||
| Breast | 191 (50.7) | 377 | 65 (19.3) | 337 |
| Colorectal | 361 (44.8) | 806 | 63 (17.6) | 358 |
| Prostate | 101 (28.1) | 360 | 23 (6.2) | 371 |
| Lung | 689 (42.3) | 1628 | 12 (10.3) | 116 |
| Esophageal | 64 (53.3) | 120 | c (26.7) | 15 |
| Pancreatic | 100 (36.4) | 275 | ||
| Head-and-neck | 86 (62.8) | 137 | 8 (16.3) | 49 |
| Hematologic | 177 (36.7) | 482 | 18 (21.2) | 85 |
| Other | 533 (33.8) | 1576 | 37 (6.1) | 602 |
| Cancer stage at Dx for last cancer Dxdd | ||||
| 0e | 11 (22.0) | 50 | 13 (17.1) | 76 |
| I | 213 (34.5) | 618 | 54 (22.5) | 240 |
| II | 247 (41.2) | 599 | 62 (21.3) | 291 |
| III | 429 (51.6) | 832 | 30 (30.0) | 100 |
| IV | 1003 (46.7) | 2147 | 15 (29.4) | 51 |
| Unknownf | 49 (17.7) | 277 | 12 (16.2) | 74 |
| Not availableg | 217 (30.8) | 705 | 15 (25.0) | 60 |
| Prior cancer Dx | ||||
| Yes | 496 (41.3) | 1202 | 57 (20.1) | 284 |
| No | 1806 (39.6) | 4559 | 173 (10.5) | 1649 |
| Outcomes | ||||
| Time from last cancer Dx to deathh | ||||
| ≤2 Weeks | 46 (8.5) | 543 | 14 (15.9) | 88 |
| >2 And ≤13 weeks | 360 (31.3) | 1151 | ||
| >13 And ≤26 weeks | 285 (41.8) | 682 | 17 (21.0) | 81 |
| >26 And ≤52 weeks | 422 (51.7) | 817 | ||
| Place of deathi | ||||
| Hospital | 1337 (42.5) | 3149 | 124 (13.4) | 925 |
| Not hospital | 520 (34.7) | 1497 | 63 (9.9) | 634 |
Bold results for a characteristic are statistically significant at p<0.0001.
Count in the 19–39 age group was less than 5, and that group was therefore combined with the 40–54 age group.
Esophageal and pancreatic cancers are combined, because their counts were less than 5.
Because the last cancer diagnosis for 1574 decedents occurred before collaborative staging was introduced, those decedents were omitted.
“Occult” was grouped with stage 0 (in situ), because counts were less than 5.
“Unknown” is a consequence of insufficient information to stage the patient.
“Not available” means that the cancer could not be staged using TNM collaborative staging processes. Many hematologic cancers are included in this category.
For 4332 decedents who received their diagnosis more than 52 weeks before death, we could not guarantee that all had access to navigation at the time of diagnosis, and so they were omitted.
The “hospital death” variable was not available for the 1489 individuals who died in 2011, and therefore those decedents were removed from the analysis.
Dx = diagnosis; Dxd = diagnosed.
Disease Characteristics
Among study decedents who died of cancer, the highest navigation rates were seen for those having a last diagnosis of head-and-neck (62.8%), esophageal (53.3%), breast (50.7%), colorectal (44.8%), and lung (42.3%) cancer. The lowest navigation rate was seen for those with prostate cancer (28.1%). Among study decedents who died of non-cancer causes according to their death certificate, but whose last cancer diagnosis was one of the four most frequent cancer sites, patterns were similar: the highest navigation rates were seen for those having a last diagnosis of breast (19.3%) and colorectal (17.6%) cancer; the navigation rate was intermediate for lung cancer (10.3%) and lowest for prostate cancer (6.2%).
In general, the navigation rate increased with a more advanced-stage cancer at last diagnosis. Having had a prior cancer diagnosis did not make a significant difference for individuals who died of cancer. However, among individuals who died of non-cancer causes, the navigation rate for those with a prior cancer diagnosis was almost twice the rate for those who did not (20.1% vs. 10.5%).
Outcomes
For study decedents whose last cancer diagnosis occurred within their last year of life, navigation rates decreased as the interval from the last cancer diagnosis to death decreased. For both the cancer and the non-cancer decedents, higher navigation rates were associated with dying in hospital.
Time from Last Diagnosis and Last Navigation to Death
Table iii shows that study decedents diagnosed with breast or prostate cancer had the longest interval from diagnosis to death, especially the subgroup who did not die of cancer. In contrast, study decedents diagnosed with esophageal or pancreatic cancer had the shortest survival interval. Those patterns parallel the patterns reported in Canadian Cancer Statistics 20179.
TABLE III.
Interval in weeks from diagnosis and last navigation to death
| Cancer diagnosis closest to death | Interval to death (weeks), by decedent type | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Cancer death (n=5761) | Non-cancer death (n=1933) | |||||||
|
|
|
|||||||
| Since diagnosis | Since last navigation visit | Since diagnosis | Since last navigation visit | |||||
|
|
|
|
|
|||||
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
| Breast | 187 | 105–345 | 25 | 6–80 | 391 | 127–444 | 223 | 104–358 |
| Colorectal | 84 | 30–156 | 22 | 6–76 | 227 | 123–381 | 203 | 104–332 |
| Prostate | 163 | 76–389 | 18 | 5–51 | 313 | 186–431 | 195 | 94–345 |
| Lung | 37 | 14–78 | 10 | 3–30 | 145 | 66–313 | 126 | 20–310 |
| Esophageal | 26 | 20–50 | 14 | 6–34 | 46 | 43–48 | 41 | 40–42 |
| Pancreatic | 26 | 11–46 | 11 | 4–26 | 49 | 32–66 | 29 | 17–40 |
| Head-and-neck | 57 | 32–143 | 11 | 4–38 | 69 | 56–181 | 56 | 34–87 |
| Hematologic | 76 | 25–178 | 18 | 4–75 | 192 | 40–326 | 36 | 15–146 |
| Other | 56 | 22–122 | 14 | 5–39 | 144 | 59–363 | 123 | 4–280 |
IQR = interquartile range.
The longest median intervals from last navigation to death were seen for individuals with breast or colorectal cancer; the shortest median intervals varied depending on whether the decedents died of cancer or non-cancer causes. Among individuals dying of cancer, those with a head-and-neck cancer diagnosis had one of the shortest median intervals from last navigation visit to death (11 weeks; iqr: 4–38 weeks), similar to the intervals for individuals with a diagnosis of lung (10 weeks; iqr: 3–30 weeks), pancreatic (11 weeks; iqr: 4–26 weeks), or esophageal (14 weeks; iqr: 6–34 weeks) cancer.
DISCUSSION
Navigation was developed and promoted by Freeman and Rodriguez more than 25 years ago to help people affected by cancer who had worse health outcomes as a result of problems accessing needed information and services in a timely way1. However, the present work appears to be the first population-based study of the use of cancer-patient navigation and one of only a few studies12 to describe the use of cancer-patient navigation for those approaching end of life.
Aging and Cancer Survivors with Non-Cancer Causes of Death
Canada’s population is aging, and the need for greater advance care planning and palliative support is widely recognized27. It is therefore worthwhile to begin to examine the role of navigation for those dying of cancer and for cancer survivors who die of a non-cancer cause of death. Because navigation was originally developed for cancer patients, higher rates of navigation for those dying of cancer were not unexpected. However, our study shows that some people approaching death from a non-cancer cause were also navigation enrolees (Figure 2). It is possible that some might have been receiving cancer treatment, but that cancer was not a cause of their death. However, that finding is also consistent with the role of navigation in Nova Scotia, which is designed to be patient-centred. It also aligns with anecdotal reports by navigators that they provide patient-focused information and communication that at times is not cancer-related. Also, some underreporting of cancer as a cause of death is a possibility.
Freeman and Rodriguez advocated a holistic health care navigation approach, and so an assessment of whether non-cancer navigation needs, including advance care planning for palliative support, are being fully met could be timely. Such an assessment could also be important, because, as a result of increasing access to treatments that prolong life, the end-of-life cancer trajectory is beginning to show a pattern that resembles the pattern seen in people dying of organ failure and frailty14. As the population ages and cancer survivors live longer with cancer, non-cancer comorbidities will increasingly have to be considered.
The observation that navigation rates decline for individuals of older age requires examination. Part of the reason could be that as age increases, increases in non-cancer comorbidities might mean that options for aggressive oncology treatment decrease, with a corresponding decrease in the need for cancer-system navigation. However, elderly individuals living with cancer have needs that should be addressed28. Another reason could be that those at end of life are increasingly likely to be nursing home residents. In 2011, of Canadian seniors in their 90s, 43.5% lived in nursing homes or seniors’ residences29. Nursing home residents in Nova Scotia were more likely to die out of hospital, less likely to receive palliative radiation or a medical oncology consultation, and less likely to be registered in a palliative care program30. Nursing home residency was not a variable available for inclusion in our study, and we lack a good understanding of the navigation needs of those residents.
Cancer Diagnoses
The navigation patterns observed by last cancer diagnosis are consistent with multiple known factors. Cancer decedents who had head-and-neck cancer as their last cancer diagnosis had the highest navigation rate (62.8%). The survival time for head-and-neck cancer is quite variable, depending on many factors, including cancer subtype31. Navigation is critically important to patients with head- and-neck cancer, because their treatments are intense, and symptom management is often distributed between a wide range of service providers24. Furthermore, Halifax (which is in the Central Zone) is the major location for delivery and coordination of head-and-neck cancer treatment. A head-and-neck cancer case manager typically links with the 9 community-based navigators to coordinate tertiary care and transitions home for head-and-neck cancer patients living in the three study zones.
The navigation rate for cancer decedents having hematologic cancer was relatively low (36.7%) during the study period. Recently, because hematologic oncology care is centralized, hematologic staff in the Central Zone were given education about cancer-patient navigation in the three study zones. We therefore expect that a future study will show an increased navigation rate.
The short interval from diagnosis and last navigation to death for decedents with esophageal cancer is consistent with the low 5-year survival rate (14%) in that malignancy9. Pancreatic cancer is also very aggressive, with a 5-year survival in the 15%–20% range even when resectable, and just 2% if metastases are present at diagnosis9. Decedents with pancreatic cancer also had a short interval from last navigation to death. However, among individuals dying of cancer, the navigation rate for those with pancreatic cancer was one of the lowest (36.4%), and the rate for those with esophageal cancer was one of the highest (53.3%). We speculate that differences in diagnostic pathways and management practices might explain the lower pancreatic cancer navigation rate. For instance, population-based data demonstrate that a substantial proportion of people with pancreatic cancer in Nova Scotia do not receive a medical oncology consultation32, which might delay—or even preclude—referral to a navigator.
Table iii shows that the three cancers with the longest intervals from diagnosis to death were breast, colorectal, and prostate cancer. However, navigation rates for decedents from those cancers varied, being relatively high (50.7%) for breast cancer decedents, lower (44.8%) for colorectal cancer decedents, and lowest of all (28.1%) for prostate cancer decedents. The navigation rates for the non-cancer decedents in the same groups followed a somewhat similar, but much lower-rate pattern: breast (19.3%), colorectal (17.6%), and prostate (6.2%). Various factors might help to explain those findings. On average, people diagnosed with breast cancer are much younger than those diagnosed with prostate cancer, and our findings also showed that navigation rates decline with increasing age.
In Nova Scotia, urologists are typically the primary specialists caring for men with prostate cancer. They are usually surgeons located across the province. “Watch and wait” rather than active treatment is often advised. That approach contrasts with the approach to treatment for cancers in which medical or radiation oncologists are involved soon after a cancer diagnosis. Also, because urologists outside of the Central Zone care for people with malignant and nonmalignant disease, they have not functioned as part of the formal oncology specialty care program. They might therefore have less information about navigation. In their study of navigation, dela Rama and Pratz33 stated that many centres with navigators designated for specific cancers did not have a navigator for prostate cancer even though navigation could benefit patients. That observation could be especially true in the future, given the increasing options for androgen depletion therapy34.
In contrast, the culture and context of breast cancer is markedly different, and the situation in colorectal cancer is intermediary. When Freeman started navigation, his focus was on breast cancer screening35, and since then, much navigation research has focused on breast cancer36–38. Also, for more than 25 years, breast cancer survivors have been empowered by strong advocacy voices; prostate cancer advocacy is much more recent and muted. Furthermore, the Central Zone has two coordinators for breast health; no parallel exists for colorectal or prostate cancer.
As expected, study decedents with stage iii and iv cancers had the highest navigation rates because of their prognosis and options for care. The low navigation rates for those with an unknown-stage cancer were also expected because those individuals typically lack sufficient diagnostic test results to determine cancer stage. Lack of staging information can be a result of various circumstances. One example is a nursing home resident with dementia whose diagnostic testing would be difficult to perform and would likely not change the decision to use comfort care in the presence of widespread metastases or life-limiting comorbidities such as congestive heart failure, advanced diabetes, compromised renal or liver function, and advancing chronic obstructive pulmonary disease. People with such comorbidities are less likely to be good candidates for surgery or chemotherapy. Those observations raise questions about the role of navigation for people with cancer who reside in nursing homes or who have multi-morbidity.
Another study finding that requires further investigation is the association between a prior cancer diagnosis and variations in the navigation rate by cause of death. A first step in a follow-up study would be to control for confounding, because navigation enrolee status and cause of death both vary by age and cancer diagnosis, especially in the breast and prostate cancer subgroups.
Outcomes
The lower navigation rates for those who die relatively soon after their cancer diagnosis might be an indicator of unmet needs that could have been addressed by expedited navigation. The rate of access to palliative care has been shown to be lower for people who die quickly after a cancer diagnosis23.
The finding that people dying in hospital have a higher navigation rate is not unexpected. In Nova Scotia, navigation staff are hospital-based. An individual’s admittance as an inpatient might facilitate referrals and visits. Also, navigators identify and report problems in the system. When access to community-based care is inadequate, hospitalization rates are higher39. Furthermore, at the time of the present study, Nova Scotia had no community-based hospice beds—only palliative or other beds in hospitals or nursing homes for those whose needs were greater than home care was able to provide.
The results in Table iii are particularly informative, given that the goal of navigation is to ensure timely, up-to-date, and coordinated patient-centred care, and that considerable unmet needs for advance care planning and palliative care at end of life are evident for those dying of advancing life-limiting non-cancer chronic diseases13. For people having one of the cancers associated with the longest survival times who die of non-cancer causes, the median interval from last navigation visit to death is about 4 years (breast cancer, 223 weeks; colorectal cancer, 203 weeks; prostate cancer, 195 weeks); for people having one of the cancers associated with the shorter survival times, the interval is less than 1 year (esophageal cancer, 41 weeks; pancreatic cancer, 29 weeks). Navigation by nurses40 or volunteers41,42 might provide an ideal means to increase advance care planning for people dying of non-cancer conditions, especially those with advancing non-cancer diseases whose navigation rates are less than 20% (Table ii).
Strengths, Limitations, and Recommendations
Nova Scotia led the way in introducing navigation in Canada43,44. It has an electronic database of patient records that goes back to the initiation of navigation in its three zones and a provincial cancer registry containing all invasive cancer cases and deaths of people with cancer that goes back to the early 1970s.
The present study is the first to provide population-based data about navigation use, and it helps fill the gap in studies about the role of navigation for cancer survivors approaching the end of life. However, with no studies for comparison, findings of the present study should not be generalized. On the other hand, our work establishes a method for future population-based navigation studies in other geographic locations.
The number of variables included in the study was limited. For example, only two outcome variables were considered. Those outcomes were selected because, in prior studies, a shorter interval from diagnosis to death16–19,22,23 and in-hospital death18,20,21 were indicators of lower rates of access to out-of-hospital palliative support. Other outcome indicators of the quality of community-based palliative care at end of life are timely enrolment in specialized palliative care16,20,23, no or few days in hospital in the last month of life18,22, and minimal use of the emergency department18–22. Receiving palliative radiation16–20,23 and home care20–22 have also been used as indicators of quality end-of-life care. Access to, and continuity of, primary care, the use of medical oncology and chemotherapy18–20,22, and being a nursing home resident19,23,30 are also relevant. Socioeconomic and distance indicators of inequity should be investigated by linking the postal code of residence at death to census data17,19,22,23,45 because a meta-analysis showed that the benefit from navigation is greatest for the most vulnerable individuals46.
When sufficient data from 2013 onward are available to increase the number of study subjects and the number with a cancer stage recorded, multivariate analyses should be conducted to control for confounding and to identify possible effect modifiers. In addition, outreach oncology clinics have been developed province-wide in recent years, and so the need for navigation could change over time. The present study provides baseline information that will be useful in the design of a next study.
CONCLUSIONS
This first population-based study of cancer-patient navigation compared navigation enrolees with non-enrolees at end of life. Age, cancer diagnosis and stage, death from cancer compared with non-cancer causes, and interval from diagnosis to death were associated with navigation use. However, whether those patterns are consistent with the need for navigation is unknown. Given that more people are living longer with cancer and that the population is aging, surveillance of who benefits from navigation services and who is using those services is warranted.
Acknowledgments
GP was funded by the Dalhousie Medical Research Foundation Chase Summer Studentship. James Boxall, Geographer, gis Centre, Killam Library, Dalhousie University, prepared the open-access map for Figure 1. We thank the staff of the Cancer Care Program of the Nova Scotia Health Authority for their data and help. Ron Dewar and Devbani Raha assisted with data development and verification for the study. Joanne Turner assisted with data cleaning and resolution. Amanda Jacquard provided information about data entry in the cancer-patient navigation database. Maureen MacIntyre provided oversight and guided us in the data access processes of the Cancer Care Program. The Nova Scotia cancer-patient navigators shared their interpretations after a presentation of the study findings.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Freeman HP, Rodriguez RL. History and principles of patient navigation. Cancer. 2011;117(suppl):3539–42. doi: 10.1002/cncr.26262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Easley J, Miedema B, Carroll JC, O’Brien MA, Manca DP, Grunfeld E. Patients’ experiences with continuity of cancer care in Canada: results from the canimpact study. Can Fam Phys. 2016;62:821–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Fillion L, Cook S, Veillette AM, et al. Professional navigation framework: elaboration and validation in a Canadian context. Oncol Nurs Forum. 2012;39:58–69. doi: 10.1188/12.ONF.E58-E69. [DOI] [PubMed] [Google Scholar]
- 4.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paskett ED, Harrop P, Wells KJ. Patient navigation: an update on the state of the science. CA Cancer J Clin. 2011;61:237–49. doi: 10.3322/caac.20111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cantril C, Haylock PJ. Patient navigation in the oncology care setting. Semin Oncol Nurs. 2013;29:76–90. doi: 10.1016/j.soncn.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Crane-Okada R. Evaluation and outcome measures in patient navigation. Semin Oncol Nurs. 2013;29:128–40. doi: 10.1016/j.soncn.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Krok-Schoen JL, Oliveri JM, Paskett ED. Cancer care delivery and women’s health: the role of the patient navigator. Front Oncol. 2016;6:2. doi: 10.3389/fonc.2016.00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canadian Cancer Society’s Advisory Committee on Cancer Statistics . Canadian Cancer Statistics 2017. Toronto, ON: Canadian Cancer Society; 2017. [Google Scholar]
- 10.Valaitis RK, Carter N, Lam A, Nicholl J, Feather J, Cleghorn L. Implementation and maintenance of patient navigation programs linking primary care with community-based health and social services: a scoping literature review. BMC Health Serv Res. 2017;17:116. doi: 10.1186/s12913-017-2046-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grunfeld E. The two solitudes of primary care and cancer specialist care: is there a bridge? Curr Oncol. 2017;24:69–70. doi: 10.3747/co.24.3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hauser J, Sileo M, Araneta N, et al. Navigation and palliative care. Cancer. 2011;117(suppl):3585–91. doi: 10.1002/cncr.26266. [DOI] [PubMed] [Google Scholar]
- 13.Nova Scotia, Department of Health and Wellness . Integrated Palliative Care Strategy: Planning for Action in Nova Scotia. Halifax, NS: Government of Nova Scotia; 2014. [Google Scholar]
- 14.Hawley P. Integrated Palliative Care [webinar] Halifax, NS: Nova Scotia Health Authority; 2017. [Available at: http://stream2.nshealth.ca/2017-05-10-the-integration-palliative-care; cited 28 August 2017] [Google Scholar]
- 15.Nova Scotia Health Authority, Cancer Care Program . A Cancer Patient Navigator May Help [patient pamphlet] Halifax, NS: Nova Scotia Health Authority; 2018. [Available online at: https://library.nshealth.ca/ld.php?content_id=34315706; cited 23 April 2018] [Google Scholar]
- 16.Johnston GM, Gibbons L, Burge FI, Dewar R, Cummings IE, Levy IG. Identifying potential need for cancer palliation in Nova Scotia. CMAJ. 1998;158:1691–8. [PMC free article] [PubMed] [Google Scholar]
- 17.Johnston GM, Boyd CJ, Joseph P, MacIntyre M. Variation in delivery of palliative radiotherapy to persons dying of cancer in Nova Scotia, 1994 to 1998. J Clin Oncol. 2001;19:3323–32. doi: 10.1200/JCO.2001.19.14.3323. [DOI] [PubMed] [Google Scholar]
- 18.Grunfeld E, Lethbridge L, Dewar R, et al. Towards using administrative databases to measure population-based indicators of quality of end-of-life care: testing the methodology. Palliat Med. 2006;20:769–77. doi: 10.1177/0269216306072553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burge FI, Lawson BJ, Johnston GM, Grunfeld E. A population-based study of age inequalities in access to palliative care among cancer patients. Med Care. 2008;46:1203–11. doi: 10.1097/MLR.0b013e31817d931d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Canadian Cancer Society’s Steering Committee . Canadian Cancer Statistics 2010: Special Topic: End-of-Life Care. Toronto, ON: Canadian Cancer Society; 2010. [Google Scholar]
- 21.Barbera L, Seow H, Sutradhar R, et al. Quality indicators of end-of-life care in patients with cancer: what rate is right? J Oncol Pract. 2015;11:e279–87. doi: 10.1200/JOP.2015.004416. [DOI] [PubMed] [Google Scholar]
- 22.Barbera L, Seow H, Sutradhar R, et al. Quality of end-of-life cancer care in Canada: a retrospective four-province study using administrative health care data. Curr Oncol. 2015;22:341–55. doi: 10.3747/co.22.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao J, Johnston GM, Lavergne MR, McIntyre P. Identifying population groups with low palliative care program enrolment using classification and regression tree analysis. J Palliat Care. 2011;27:98–106. [PMC free article] [PubMed] [Google Scholar]
- 24.Fillion L, De Serres M, Cook S, Goupil RL, Bairati I, Doll R. Professional patient navigation in head and neck cancer. Semin Oncol Nurs. 2009;25:212–21. doi: 10.1016/j.soncn.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Howell DA, Roman E, Cox H, et al. Destined to die in hospital? Systematic review and meta-analysis of place of death in haematological malignancy. BMC Palliat Care. 2010;9:1–8. doi: 10.1186/1472-684X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Joint Committee on Cancer (ajcc), Collaborative Stage Data Collection System . Home > About [Web page] Chicago, IL: AJCC; 2017. [Available at: https://cancerstaging.org/cstage/about/Pages/default.aspx; cited 12 August 2017] [Google Scholar]
- 27.Canadian Cancer Research Alliance (ccra) Pan-Canadian Framework for Palliative and End-of-Life Care Research. Toronto, ON: CCRA; 2017. [Google Scholar]
- 28.Fitch MI. Focusing on care of older adults with cancer [editorial] Can Oncol Nurs J. 2017;27:208. [PMC free article] [PubMed] [Google Scholar]
- 29.Statistics Canada . Living arrangements of seniors [Web page] Ottawa, ON: Statistics Canada; 2015. [Available at: http://www12.statcan.gc.ca/census-recensement/2011/as-sa/98-312-x/98-312-x2011003_4-eng.cfm; cited 20 July 2017] [Google Scholar]
- 30.O’Brien M, Johnston GM, Gao J, Dewar R. End-of-life care for nursing home residents dying from cancer in Nova Scotia, Canada, 2000–2003. Support Care Cancer. 2007;15:1015–21. doi: 10.1007/s00520-007-0218-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cancer.net . Head and Neck Cancer: Statistics [Web page] Alexandria, VA: American Society of Clinical Oncology; 2017. [Available at: http://www.cancer.net/cancer-types/head-and-neck-cancer/statistics; cited 22 July 2017] [Google Scholar]
- 32.Hurton S, Urquhart R, Kendell C, et al. Variations in medical oncology utilization for pancreatic cancer patients in Nova Scotia. JOP. 2017;18:62–8. [Google Scholar]
- 33.dela Rama F, Pratz C. Navigating treatment of metastatic castration-resistant prostate cancer: nursing perspectives. Clin J Oncol Nurs. 2015;19:723–32. doi: 10.1188/15.CJON.723-732. [DOI] [PubMed] [Google Scholar]
- 34.Dragomir A, Rocha J, Vanhuyse M, et al. Treatment patterns and trends in patients dying of prostate cancer in Quebec: a population-based study. Curr Oncol. 2017;24:240–8. doi: 10.3747/co.24.3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Freeman H. Patient navigation: a community based strategy to reduce cancer disparities. J Urban Health. 2006;83:139–41. doi: 10.1007/s11524-006-9030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mertz BG, Dunn-Henriksen AK, Kroman N, et al. The effects of individually tailored nurse navigation for patients with newly diagnosed breast cancer: a randomized pilot study. Acta Oncol. 2017;56:1682–9. doi: 10.1080/0284186X.2017.1358462. [DOI] [PubMed] [Google Scholar]
- 37.Gunn CM, Parker VA, Bak SM, Ko N, Nelson KP, Battaglia TA. Social network structures of breast cancer patients and the contributing role of patient navigators. Oncologist. 2017;22:918–24. doi: 10.1634/theoncologist.2016-0440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Percac-Lima S, Ashburner J, Bond B, Oo S, Atlas S. Decreasing disparities in breast cancer screening in refugee women using culturally tailored patient navigation. J Gen Intern Med. 2013;28:1463–8. doi: 10.1007/s11606-013-2491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Di Pollina L, Guessous I, Petoud V, et al. Integrated care at home reduces unnecessary hospitalization of community-dwelling frail older adults: a prospective controlled trial. BMC Geriatr. 2017;17:53. doi: 10.1186/s12877-017-0449-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pesut B, Hooper B, Jacobsen M, Nielsen B, Falk M, O’Connor BP. Nurse-led navigation to provide early palliative care in rural areas: a pilot study. BMC Palliat Care. 2017;16:37. doi: 10.1186/s12904-017-0211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pesut B, Duggleby W, Warner G, et al. Volunteer navigation partnerships: piloting a compassionate community approach to early palliative care. BMC Palliat Care. 2017;17:2. doi: 10.1186/s12904-017-0210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dolovich L, Oliver D, Lamarche L, et al. A protocol for a pragmatic randomized controlled trial using the Health Teams Advancing Patient Experience: Strengthening Quality (Health tapestry) platform approach to promote person-focused primary healthcare for older adults. Implement Sci. 2016;11:49. doi: 10.1186/s13012-016-0407-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walkinsaw E. Patient navigators becoming the norm in Canada. CMAJ. 2011;183:E1109–10. doi: 10.1503/cmaj.109-3974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fillion L, Cook S, Veillette AM, et al. Professional navigation: a comparative study of two Canadian models. Can Oncol Nurs J. 2012;22:257–77. doi: 10.5737/1181912x224257266. [DOI] [PubMed] [Google Scholar]
- 45.Lavergne MR, Lethbridge L, Johnston G, Henderson D, d’Intino AF, McIntyre P. Examining palliative care program use and place of death in rural and urban contexts: a Canadian population-based study using linked data. Rural Remote Health. 2015;15:3134. [PubMed] [Google Scholar]
- 46.Freund KM, Battaglia TA, Calhoun E, et al. on behalf of the Writing Group of the Patient Navigation Research Program Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst. 2014;106 doi: 10.1093/jnci/dju115. dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]