Abstract
Purpose
As cancer centres move forward with earlier discharge of stable survivors of early-stage breast cancer (bca) to primary care follow-up, it is important to address known knowledge and practice gaps among primary care providers (pcps). In the present qualitative descriptive study, we examined the practice context that influences implementation of existing clinical practice guidelines for providing such care. The purpose was to determine the challenges, strengths, and opportunities related to implementing comprehensive evidence-based bca survivorship care guidelines by pcps in southeastern Ontario.
Methods
Semi-structured interviews were conducted with 19 pcps: 10 physicians and 9 nurse practitioners.
Results
Thematic analysis revealed 6 themes within the broad categories of knowledge, attitudes, and resources. Participants highlighted 3 major challenges related to providing bca survivorship care: inconsistent educational preparation, provider anxieties, and primary care burden. They also described 3 major strengths or opportunities to facilitate implementation of survivorship care guidelines: tools and technology, empowering survivors, and optimizing nursing roles.
Conclusions
We identified several important challenges to implementation of comprehensive evidence-based survivorship care for bca survivors, as well as several strengths and opportunities that could be built upon to address those challenges. Findings from our research could inform targeted knowledge translation interventions to provide support and education for pcps and bca survivors.
Keywords: Breast cancer, evidence-based guidelines, clinical practice guidelines, survivorship care, primary care, qualitative research, knowledge translation
BACKGROUND
Canadian cancer centres, including those in Ontario, are discharging stable survivors of early-stage breast cancer (bca) earlier to primary care follow-up1. The U.S. Institute of Medicine report, From Cancer Patient to Cancer Survivor: Lost in Transition, outlined these four essential components of survivorship care: prevention, surveillance, intervention, and coordination2. Although research suggests that primary care providers (pcps) routinely implement American Society of Clinical Oncology–recommended surveillance tests3, bca survivors report that many health care needs are not being met4. Our research team synthesized existing clinical practice guidelines (cpgs) for bca survivorship care that are relevant to primary care5. We also identified self-reported gaps in pcp knowledge and implementation of other components of survivorship care that require further study6.
The present study was conducted within a broader knowledge translation program of research that aims to improve outcomes for bca survivors. In Ontario, where the population of nurse practitioners (nps) conducting primary health care is growing and many pcps are practicing in team-based models such as family health teams, the strategies that would be the most effective to promote evidence-based survivorship care remain unclear. The behaviours of health care providers are influenced by their knowledge and attitudes, as well as by external barriers and facilitators such as patient factors, guideline factors, and environmental factors7. Thus, enhancing translation of evidence-based guidelines to primary care requires an understanding of the practice context. The purpose of the present study was to determine challenges and opportunities related to implementing evidence-based bca survivorship care by pcps.
METHODS
The Consolidated Criteria for Reporting Qualitative Research guided reporting of the study methods and results8. A more detailed description is found in the primary author’s dissertation9.
Study Design
A qualitative descriptive method was used to explore the perceptions by pcps of the challenges, strengths, and opportunities related to providing effective evidence-based bca survivorship care, and to inform recommendations for knowledge translation strategies. The goal of qualitative descriptive studies is to provide comprehensive summaries of events or descriptions of phenomena. Thus, qualitative description is pragmatic and applicable to answering questions of relevance to health professionals and policymakers10.
Setting and Participants
Participants were recruited from the South East Local Health Integration Network in Ontario, which serves an estimated population of 500,451. The estimated 2017 incidence of female bca in the region is 155.4 per 100,000 women, which is higher than the provincial estimate of 146.4 per 100,000 women11. Locally, the first cohort of early-discharge bca survivors (n = 144) were discharged from the regional cancer centre between January 2015 and July 2016 (Luctkar-Flude M, Langley H, Tyerman J. Exploring the perspectives of early-discharge breast cancer survivors following the transition to primary care follow-up. Presented at the 2016 cano/acio Annual Conference; Calgary, AB; 20–23 October 2016).
A combination of purposive and snowball sampling resulted in the recruitment of 19 pcps, who were contacted by e-mail or telephone after they had indicated interest on a related survey distributed to primary care physicians (mds) and nps across the region6. All survey participants were invited to participate in an interview, and all who agreed were interviewed. After 14–15 interviews had been completed, data saturation was felt to have been obtained because of recurrence of themes and lack of new findings. The study received ethics approval, and informed consent was obtained from all study participants.
Data Collection and Analysis
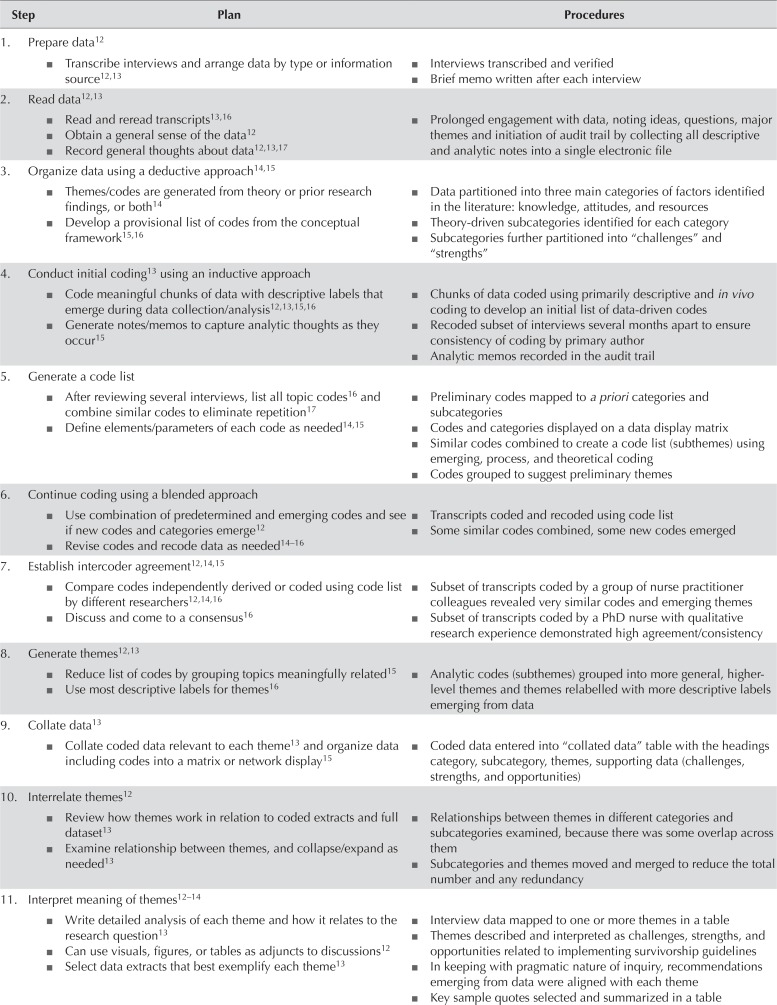
Semi-structured interviews were based on an interview guide developed and informally pilot-tested with 1 np and 1 md. All participants were reminded of the context for the interviews (Table i). Additional prompts and probing questions were improvised at the discretion of the interviewer. Interview recordings were transcribed verbatim by the primary researcher. Interviews were conducted by the primary author (MLF), and the second author (AA) reviewed all aspects of the data analysis. Data analysis was guided by the principles and steps of qualitative data analysis described by Creswell12 and by the phases of thematic analysis described by Braun and Clarke13. Coding procedures used a pragmatic, blended approach that was both deductive and inductive12,14–17, and a variety of activities were undertaken to maintain study rigour—specifically, peer review, member checking, and triangulation18. Table ii provides a detailed description of the analysis plan and procedures.
TABLE I.
Interview guide
| Interview context | |
| These interviews are being conducted within the following context: | |
| 1 | The cancer centre is discharging stable early-stage breast cancer (BCa) survivors back to primary care follow-up earlier than previously—that is, within 1–2 years after diagnosis rather than 5 or more years. |
| 2 | It is recommended that comprehensive survivorship care should include these four domains: (1) prevention of recurrent and new cancers, and late effects; (2) surveillance for recurrent or new cancers, and late effects; (3) interventions for late and long-term effects; and (4) coordination between primary care providers (PCPs) and specialists to ensure that all health care needs are met. |
| 3 | Evidence-based BCa survivorship care refers to implementation of the key guideline recommendations included in the survey of PCPs from which the study sample was recruited; thus, interview participants were now familiar with those recommendations. |
| Interview questions | |
| 1 | Tell me about your experience of providing care to women after primary treatment for BCa. |
| 2 | What is your perception of the care that BCa survivors receive in primary practice? |
| 3 | What are the challenges and barriers related to providing effective care to BCa survivors? Related to practicing in a city/town/rural setting? Related to the nurse practitioner (NP) role? |
| 4 | How has your experience of caring for BCa survivors affected your confidence in caring for this patient population? |
| 5 | Tell me about the education that prepared you for working with BCa survivors. |
| 6 | Tell me about how you access research evidence related to BCa survivorship care. Are there any specific guideline sources that you access? |
| 7 | Are there any barriers or challenges related to implementing the guidelines? Related to the health care system? To the patients themselves? |
| 8 | What are the PCP’s education needs related to caring for BCa survivors? How prepared do you feel to assume responsibility for survivorship care after early discharge from the cancer centre? |
| 9 | What is your choice for an education delivery method that will enhance your ability to provide evidence-based survivorship care? |
| 10 | With respect to the four domains of survivorship care: prevention, surveillance, intervention, and coordination, which domains do you feel comfortable/confident with? Any domains that you feel less comfortable/confident with? |
| 11 | Can you suggest anything else that would facilitate implementation of the key guideline recommendations? |
TABLE II.
Qualitative thematic analysis plan and procedures: a pragmatic blended approach
| Step | Plan | Procedures |
|---|---|---|
| 1. | Prepare data12 | |
|
||
| 2. | Read data12,13 | |
|
||
| 3. | Organize data using a deductive approach14,15 | |
|
||
| 4. | Conduct initial coding13 using an inductive approach | |
|
||
| 5. | Generate a code list | |
|
||
| 6. | Continue coding using a blended approach | |
|
||
| 7. | Establish intercoder agreement12,14,15 | |
|
||
| 8. | Generate themes12,13 | |
|
||
| 9. | Collate data13 | |
|
||
| 10. | Interrelate themes12 | |
|
||
| 11. | Interpret meaning of themes12–14 | |
|
||
| 12. | Peer review or debriefing18 | |
|
|
|
| 13. | Member checking18 | |
|
||
| 14. | Triangulation18 | |
|
|
|
| 15. | Produce report13 | |
|
|
RESULTS
Interviews were conducted with 10 mds and 9 nps (Table iii) similar in age and practice type, with most being women. Compared with the nps, the mds had significantly more primary care experience (mean: 21.8 ± 13.0 years vs. 6.1 ± 4.7 years). Interview duration ranged from 10 minutes to 47 minutes (mean: 24.9 ± 9.5 min).
TABLE III.
Characteristics of the 19 interview participants
| Characteristic | Value |
|---|---|
| Profession (n) | |
| Family physician | 10 |
| Primary health care nurse practitioner | 9 |
| Sex | |
| Women | 15 |
| Men | 4 |
| Age (years) | |
| Mean | 50.2±10.8 |
| Range | 34–75 |
| Primary care experience (years) | |
| Mean | 14.3±12.6 |
| Range | 1–46 |
| Practice location (n) | |
| Large urban (≥100,000) | 6 |
| Small urban (10,000–99,999) | 4 |
| Town (3,000–9,999) | 5 |
| Rural (<3000) | 4 |
| Practice type (n) | |
| Family health team | 11 |
| Family health organization | 5 |
| Community health centre | 1 |
| Nurse-led clinic | 1 |
| Solo physician | 1 |
Preliminary analysis resulted in 38 subthemes mapped to categories of knowledge, attitudes, resources, and other. Final analysis revealed 6 overarching themes (Table iv) representing 3 major barriers and 3 major strengths or opportunities related to implementing bca survivorship care. In keeping with the pragmatic nature of the inquiry, recommendations emerging from data were aligned with each theme.
TABLE IV.
Primary care provider perceptions of providing breast cancer survivorship care
| Themes, by category | Subthemes | Potential knowledge translation strategies |
|---|---|---|
| Perceived challenges | ||
| Inconsistent education preparation | ||
| No formal education |
|
|
| On-the-job learning | ||
| Overwhelming to keep up-to-date | ||
| Diversity of learning needs and preferences | ||
| Provider anxieties | ||
| Fear of patients falling through the cracks |
|
|
| Fear of missing diagnosis | ||
| Fear of legal consequences | ||
| Comfort zone | ||
| Feeling like a beginner | ||
| Primary care burden | ||
| Shifting burden to primary care |
|
|
| Not my responsibility | ||
| Breast cancer survivors bring more to a visit | ||
| Primary care workload | ||
| Administration support workload | ||
| Infrastructure and funding | ||
| Access inequities | ||
| Perceived strengths and opportunities | ||
| Tools and technology | ||
| Keeping track of breast cancer survivors |
|
|
| Electronic health records | ||
| Communication tools | ||
| Protocols and survivorship care plans | ||
| Empowering survivors | ||
| Patient responsibility |
|
|
| Survivor expectations for follow-up | ||
| Positive attitudes and behaviours | ||
| Providing survivorship care plans | ||
| Optimizing nursing roles | ||
| Nurse practitioner role frustration and scope of practice |
|
|
| Nurse navigator role | ||
| Nursing chronic disease management role | ||
| Nurse practitioner role benefits | ||
Inconsistent Educational Preparation
Analysis highlighted the diversity of pcp knowledge and experience, the challenges in keeping up to date with guidelines, and the diversity of learning needs and preferences. All pcps emphasized that they had no formal education about survivorship care and that ongoing education was “hit and miss.” Most described knowledge gaps, lack of experience, challenges related to “knowing the system,” and “learning on the job.”
I’ve learned along the way by just doing; learn as you go, not because of specific education.
— md 10
I think I learned the most about survivorship from patients, really—on the job learning.
— np 4
The pcps described how the volume of information contributed to a feeling of being “overwhelmed” by “keeping up to date” on a variety of primary care topics. Perceived lack of relevance was also seen as a barrier to using cpgs. Some providers, mostly nps with access to university library databases, described comfort in accessing guidelines and conducting literature searches to answer clinical questions. The mds and nps both wanted more information and education about survivorship cpgs.
So many time constraints.... It’s a tough job in primary care because GPs need to know a little about everything.... It’s overwhelming to look for guidelines, there are so many.
— md 7
In terms of accessing guidelines and educational updates, it was clear that one size does not fit all. Providers preferred a wide range of education formats such as webinars, workplace lunch-and-learns, and continuing medical education events. Barriers to attending continuing medical education events included time and costs, particularly for rural practitioners. Many relied on Google searches; others used subscription services such as UpTo-Date (Wolters Kluwer Health, Waltham, MA, U.S.A.), which summarize research evidence. Others relied on colleagues and specialists for clinical information. Overall, a desire was expressed for “short and sweet” guidelines and centralized resources for “one-stop shopping.”
I feel like getting it both ways, e-mail and mail... Something published on some card stock, laminated, with the protocol for follow-up... Something to refer to for the first little while, until we get used to it.
— md 10
Team-based education, short, over lunch.... We’re all learning the same content at the same time.... Even a video we can watch ourselves.
— np 2
Provider Anxieties
Providers were divided in their confidence with providing survivorship care. Many described such care as falling within their “comfort zone,” but they were mainly individuals who had prior experience with cancer survivors. Others expressed anxiety about their lack of expertise and felt that such care would be easier for experts. Many described “feeling like a beginner” or simply said “tell me what to do.”
Maybe physician anxieties.... There are a lot of things that I think can get dealt with pretty easily by someone who has expertise and is doing this all day long.
— md 4
Not very confident. I don’t know where to start. To be honest, I’d have to go online and search for cancer surveillance guidelines.
—np 9
Providers were divided in their attitudes. Many felt that survivorship care was not their responsibility and described a fear of patients “falling through the cracks” if follow-up care were missed and a fear of legal consequences if a cancer recurrence were to be missed. Others suggested that pcps were ideally positioned to assume such care because of their ongoing relationships with patients.
My fear is having people fall through the cracks.... We need to clearly know what medically–legally we’ll be held responsible for ... to ensure they don’t get lost in our 1700 patient mix.
— md 5
Primary Care Burden
Many participants, particularly mds with large caseloads, were concerned about the workload effect of survivorship care being “downloaded.” They were concerned about the increased burden on administrative staff if additional infrastructure or funding was not provided. Technologies such as electronic medical records (emrs) require time and personnel to manage them. Unreliability of technology in rural settings and a need to update or migrate to new systems were also described.
We’ve got emrs, but without some structure, things may not get done. Someone has to go into the program deliberately, run lists, set up appointments, call people.
— md 3
Although many providers regarded bca survivors as similar to non-cancer patients, others perceived that they “bring more to a visit” in terms of their “cancer mindset” and higher levels of anxiety and uncertainty, and that they require more time, more frequent visits, and more reassurance.
Usually, these patients have more complaints, and they’re hard to manage. It takes a bit longer. It’s not easy things, either, where there’s a quick fix. It often involves counselling and support.
— md 10
The primary care burden was further challenged by inconsistent access to specialists and resources. Most mds described oncologists as approachable; however, nps reported challenges accessing the same specialists. Providers reported lack of access or prolonged wait times for supportive resources such as diagnostic imaging, lymphedema specialists, cancer psychiatrists, and community support groups. Time, costs, transportation, and illiteracy were cited as barriers for rural patients accessing resources; however, home visits and volunteer drivers were available in most settings to support care delivery.
I certainly wouldn’t hesitate to call an oncologist to get advice.... They’re happy to answer family doctor’s questions.... I know I’ve got somebody at my back if I don’t know what’s going on.
— md 2
We don’t have all the resources needed.... There is no specialist or physiotherapy to treat lymphedema.... There’s only one cancer psychiatrist, [and] so patients are waiting for care they need—care I can’t give or don’t have time to give.
— md 7
Tools and Technology
Participants described how technology could support the tracking of survivors and could facilitate implementation of cpgs. Guidelines could be built into emrs with fillable templates that cue practitioners to provide and document care.
We can build templates in our emr which correspond to guidelines ... and fill in the blanks specific to each patient.... I just have to type over them.
— md 10
Although many providers were satisfied with communication from the cancer centre, many described feeling “out of the loop” once a referral was made, and they expressed a desire for “post-therapy protocols,” “patient-specific survivorship care plans,” and tools to enhance communication and embed cpgs into routine practice.
A care plan or outline of specific screening and interventions for each patient would be helpful.... Something simple and easy to follow ... specific to my patient.
— md 7
Pediatric oncology is very different... We had better post-therapy protocols.... In the adult world, there seems to be more variability depending on the practitioner organizing it.
— np 8
Empowering Survivors
Providers saw survivors on a continuum from those lacking responsibility or “not very good advocates” to those who were well-informed and engaged in their own care. Providers believed that patients expected them to be “up to date” and to play an intermediary role with oncology. Some providers reported that patients preferred to be seen in primary care for follow-up; others believed that patients lacked confidence in their pcps when it came to cancer. Many providers were interested in empowering survivors to share responsibility or to coordinate their own care, and suggested that guidelines or care plans be provided to patients and providers alike.
Some of it has to be cooperation. The patient has to have some responsibility to ensure follow-up happens appropriately ... not to sit back if they don’t hear back from my office in 6 months.
— md 10
Having something like a care plan shared with the patient, like we have for asthma, where the patient’s in charge ... engagement of the client in their own care to give them more of a sense of control.... With cancer, you can feel pretty not in charge.... Empower patients to take this on.
— np 7
Optimizing Nursing Roles
Team practices offer opportunities for collaboration and for access to specialty services and expertise such as pharmacists and dieticians; however, many nps described further opportunities to optimize survivorship care if nps were able to practice to their full scope of practice. They described “role frustration” related to restrictions on prescribing and diagnostics that led to delays in care delivery. Others perceived “role confusion” related to the np scope of practice and “lack of respect” for the np role.
Pain management.... We can’t prescribe controlled substances. Another issue is diagnostics.... If we’re worried about a recurrence, we can’t order ct or mri ... getting them done in a timely fashion.
— np 3
Sometimes specialists want to hear from the physician as opposed to the np.... 90% of the time, I’ll get a letter back from the specialist directed to the physician, with no mention of my name. That’s a barrier.... The np is out of the communication equation... It’s part of the role frustration.
— np 9
Much support was expressed for optimizing nurse (rn) roles to include aspects of survivorship care. Many commented positively on the nurse navigator role in bca assessment and suggested expanding it to include survivorship. Others suggested that survivorship care be part of the primary care nurse role, because those providers are already involved in chronic disease management. However, barriers to that change included time, funding, and the comfort level of nurses taking on this additional role.
We’re going to be getting additional nursing support, and that could be a role as part of chronic disease management they could be doing.
— md 3
The breast assessment rn navigator, she’s been great. I don’t know whether it’s reasonable to use her to do survivorship follow-up as well ... or could there be two parts to her role?
— np 8
Some providers questioned the relevance of some guideline recommendations (such as screening for fatigue) or felt that their role in survivorship care was diagnostic follow-up or surveillance for recurrent cancer. Some felt that psychosocial concerns were not well-addressed, whereas others described providing comprehensive care, including prevention. The np role was seen as a facilitator to providing “holistic care” because of a focus on health promotion and longer scheduled visits, affording time for screening and counselling.
Some of these guidelines I don’t do.... Asking about sexual function.... What can be done about it anyway?
— md 8
A breast cancer patient comes to see me, and I’m looking at the entire picture.... Cancer is only one aspect of their health.
— NP 3
DISCUSSION
Our study identified 3 major challenges and 3 major strengths and opportunities, providing insight into the multilevel factors influencing implementation of bca survivorship care. The practices (behaviours) of pcps can be seen to be influenced by internal factors (knowledge and attitudes) and external factors (resources) available at the individual, practice, and system levels. Several findings are consistent with known barriers and facilitators; others added to our knowledge of bca survivorship care in the primary care setting. In keeping with the pragmatic nature of our inquiry, potential knowledge translation strategies were derived from the study participants themselves, as well as from the researcher’s suggestions.
The challenges described by our study participants are well documented in the literature: inconsistent educational preparation, primary care burden, and provider anxieties. Survivorship care has not generally been integrated into health professional curricula2, confirming the need for updating professional school curricula and continuing medical education for pcps. Although many have embraced survivorship care, others find this new role burdensome and express anxiety related to their limited knowledge, education, and experience. In the context of competing demands and relatively small caseloads of cancer survivors, pcps might not have opportunities sufficient to develop expertise and confidence in providing survivorship care. Experience is a key factor promoting comfort: primary care mds who follow more bca survivors in their practice report higher confidence in managing follow-up for those patients19. Fear of missing a cancer recurrence might draw pcps away from care perceived as less urgent, such as prevention activities. That fear is not unreasonable, given that diagnosis in primary care is recognized by the World Health Organization to be an area at high-risk for errors20. Thus, pcps desire support and clear direction from oncologists about expectations for follow-up and potential problems21.
The pcps in our study also reported as barriers a lack of time and funding, and workload burden for themselves and their staff. Overwhelmingly, our participants desired access to reliable, succinct Canadian guidelines housed in one place. They suggested that team-based education could ensure that all team members are aware of cpgs and could facilitate discussion about how teams might implement recommendations. Other studies have highlighted the importance of targeting the whole primary care team with guideline implementation strategies and have demonstrated positive change in attitudes and practices22,23. The pcps in our study, particularly those in rural areas, reported inequities in accessing specialists and supportive care services. The nps in our study were more likely to report challenges in accessing oncologists; the mds felt that access was good. Compared with their colleagues in smaller cities, mds in a larger urban Canadian city reported limited contact with oncologists21. In Canada, access for bca survivors to specialized services, such as lymphedema therapists and rehabilitation, is limited by a need for more certified therapists and lack of funding24,25. Addressing access inequities would facilitate full implementation of guideline recommendations by pcps. As well, knowledge translation interventions could better connect pcps and bca survivors to existing resources.
Strengths and opportunities identified by our study participants could be built upon to address the challenges of providing survivorship care in the primary care setting. Tools and technology were seen as important facilitators to address the primary care burden. Facilitators cited in the literature include integrated emrs, computerized reminders, protocols, and dedicated funding and personnel26. Electronic chart sharing by organizations and having protocols and reminders built into emrs are opportunities to improve care delivery. Recent bca survivorship cpgs for primary care could be incorporated into such protocols5,27. Patient-specific survivorship care plans detailing treatments, follow-up care, and resources were proposed as a communication tool provided by oncologists to keep pcps and patients in the loop and to improve guideline adherence. Survivorship care plans to enhance posttreatment transition care are endorsed by the American Society for Clinical Oncology and the Canadian Partnership Against Cancer28,29. Survivors and pcps have reported high levels of satisfaction with survivorship care plans. However, evidence shows few, if any, measurable patient outcome benefits, whereas time, resources, costs, and incompatibilities are significant barriers30–32.
Recognition of the effects of fragmented survivorship care has resulted in efforts to empower cancer survivors and to engage them in self-management, similar to the approach used in other chronic conditions33,34. Chronic disease self-management programs have been associated with improvements in psychological health status, self-efficacy, and selected health behaviors35. Cancer survivors report that many topics concerning the physical and psychosocial effects of cancer and health promotion are not addressed in follow-up36. Thus, tools and interventions that empower survivors to take an active role in their own care might ensure that those issues are addressed37. Physicians in another Canadian study believed that patients should be active partners or leaders in follow-up care, and a number reported incorporating self-management strategies with their patients21. Innovative tools that support self-management include e-health interventions such as Web-based programs or mobile apps38. Work in other chronic disease fields can provide a basis for designing e-health strategies for cancer survivors39,40.
Facilitating nps in practicing to full scope could enhance their ability to provide comprehensive survivorship care in a timely manner. Although provincial legislation allows nps to order diagnostic tests such as computed tomography and to prescribe controlled medications, those provisions will take effect only once relevant regulations are amended and approved by government41. Similarly, allowing primary care rns to practice to full scope could also contribute to comprehensive survivorship care. Although primary care rns were not included in our sample, many of our study participants—mds and nps alike—felt that rns in their practice settings could provide certain aspects of survivorship care such as screening and health promotion. Psychosocial and health behaviour assessment and counselling could be delegated to rns or allied health professionals. Regionally, breast assessment nurse navigators already coordinate pre-treatment assessment, diagnosis, and referral activities for women with bca, and primary care rns are involved in chronic disease management activities for conditions such as diabetes and hypertension. Currently, most Canadian cancer navigation programs concentrate on the diagnostic or treatment phase; however, community nurse navigators could facilitate transition to survivorship, promote self-management, and enhance supportive care42. The “lead physician” model introduced in Manitoba could be appropriate for team-based practices such as family health teams in Ontario, with teams nominating an md, np, rn, or other health professional to become “clinician lead” for survivorship care43. Nurses acting as primary care cancer leaders has been trialled in the United States and the United Kingdom, with positive effects on knowledge and practices44,45.
Because of ongoing and late effects from treatment, cancer can be viewed as a chronic disease. Effective chronic disease management includes prevention of disease progression, complications, and comorbidities, aligning with U.S. Institute of Medicine’s recommendations for cancer survivors. Research has demonstrated that enhanced roles for rns and nps contribute to effective chronic disease management and improved patient outcomes46,47. Thus, it might be effective to delegate aspects of survivorship care to trained primary care rns. A cross-sectional survey of Ontario primary care nurses determined that chronic disease management was not uniform across practices and that there was potential to optimize that role and to improve chronic disease management48. The involvement of primary care rns in cancer survivorship care in Ontario is limited, but involves care coordination, system navigation, emotional support, and facilitation of access to community resources. Expanding the role of primary care rns in cancer survivorship care is proposed as a practical approach to improve survivorship care quality49.
Our sample included rural and urban mds and nps, and experienced and novice practitioners, most situated in team-based practices, thus limiting the generalizability of findings to solo pcps. Individual participants might have had particularly positive or negative feelings toward survivorship care that motivated them to participate. Although the use of a theoretical framework to guide qualitative analysis is appropriate when significant knowledge about a field of study exists, there is a risk that data will be forced into the framework and that new themes will be missed. We were careful to ensure that findings emerged from the data.
CONCLUSIONS
The present study identified important challenges to the implementation of evidence-based care for bca survivors. Primary care providers are striving to deliver comprehensive care to bca survivors in the face of limited educational preparation, few protocols or tools, and strained practice resources. Many of the changes and suggestions aimed at improving survivorship care reflect chronic disease management strategies already in place.
Our study might be the first to include the perceptions of nps, a viewpoint that is important within the Canadian context and wherever else nps provide primary care. Roles for primary care rns in cancer survivorship represent a promising opportunity deserving of further attention. With appropriate education and tools, primary care rns could provide efficient, effective, and comprehensive survivorship care in collaboration with primary care mds and nps.
Addressing barriers to implementation and building on identified strengths and opportunities could ultimately improve the quality of bca survivorship care.
Acknowledgments
We thank everyone who took the time to participate in this study. The primary author was supported in part by a graduate scholarship from the de Souza Institute. The funding source had no involvement in the study design, data collection and interpretation, report writing, or decision to submit the article for publication. Preliminary findings from the study were presented in an abstract during the 8th Annual Meeting of the Cancer and Primary Care Research International Network and the mascc/isoo 2017 annual meeting on Supportive Care in Cancer.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflicts of interest, and we declare that we have none.
REFERENCES
- 1.Grant M, De Rossi S, Sussman J. Supporting models to transition breast cancer survivors to primary care: formative evaluation of a Cancer Care Ontario initiative. J Oncol Pract. 2015;11:e288–95. doi: 10.1200/JOP.2015.003822. [DOI] [PubMed] [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 3.Risendal BC, Sedjo RL, Giuliano AR, et al. Surveillance and beliefs about follow-up care among long-term breast cancer survivors: a comparison of primary care and oncology providers. J Cancer Surviv. 2016;10:96–102. doi: 10.1007/s11764-015-0454-y. [DOI] [PubMed] [Google Scholar]
- 4.Knobf MT. The transition experience to breast cancer survivorship. Semin Oncol Nurs. 2015;31:178–82. doi: 10.1016/j.soncn.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 5.Luctkar-Flude M, Aiken A, McColl MA, Tranmer J. A comprehensive framework and key guideline recommendations for the provision of evidence-based breast cancer survivorship care within the primary care setting. Fam Pract. 2015;32:129–40. doi: 10.1093/fampra/cmu082. [DOI] [PubMed] [Google Scholar]
- 6.Luctkar-Flude M, Aiken A, McColl MA, Tranmer J, Langley H. Are primary care providers implementing evidence-based care for breast cancer survivors? Can Fam Physician. 2015;61:978–84. [PMC free article] [PubMed] [Google Scholar]
- 7.Legare F, Ratte S, Gravel K, Graham ID. Barriers and facilitators to implementing shared-decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns. 2008;73:526–35. doi: 10.1016/j.pec.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 8.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (coreq): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 9.Luctkar-Flude M. Challenges, Strengths and Opportunities Related to Implementing Comprehensive Evidence-Based Guidelines on Breast Cancer Survivorship Care by Primary Care Physicians and Nurse Practitioners in Southeastern Ontario. Kingston, ON: Queen’s University; 2016. [phd dissertation]. [Google Scholar]
- 10.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–40. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 11.Cancer Quality Council of Ontario (cqco) South East LHIN—Cancer System Quality Index (CSQI) 2017. Toronto, ON: CQCO; 2017. [Available online at: http://www.csqi.on.ca/by_lhin/south_east_lhin; cited 19 November 2017] [Google Scholar]
- 12.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage; 2009. [Google Scholar]
- 13.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 14.Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 15.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 16.Tesch R. Qualitative Research: Analysis Types and Software Tools. London, U.K: Routledge Falmer; 1990. [Google Scholar]
- 17.Bryman A. Social Research Methods. 3rd ed. Oxford, U.K: Oxford University Press; 2008. [Google Scholar]
- 18.Lincoln Y, Guba E. Naturalistic Inquiry. New York, NY: Sage; 1985. [Google Scholar]
- 19.Smith SL, Wai ES, Alexander C, Singh-Carlson S. Caring for survivors of breast cancer: perspectives of the primary care physician. Curr Oncol. 2011;18:e218–26. doi: 10.3747/co.v18i5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh H, Schiff GD, Graber ML, Onakpoya I, Thompson MJ. The global burden of diagnostic errors in primary care. BMJ Qual Saf. 2017;26:484–94. doi: 10.1136/bmjqs-2016-005401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Brien MA, Grunfeld E, Sussman J, Porter G, Mobilio MH. Views of family physicians about survivorship care plans to provide breast cancer follow-up: exploration of results from a randomized controlled trial. Curr Oncol. 2015;22:252–9. doi: 10.3747/co.22.2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unverzagt S, Oemler M, Braun K, Klement A. Strategies for guideline implementation in primary care focusing on patients with cardiovascular disease: a systematic review. Fam Pract. 2014;31:247–66. doi: 10.1093/fampra/cmt080. [DOI] [PubMed] [Google Scholar]
- 23.Bekkers MJ, Simpson SA, Dunstan F, et al. Enhancing the quality of antibiotic prescribing in primary care: qualitative evaluation of a blended learning intervention. BMC Fam Pract. 2010;11:34. doi: 10.1186/1471-2296-11-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hodgson P, Towers A, Keast DH, Kennedy A, Pritzker R, Allen J. Lymphedema in Canada: a qualitative study to help develop a clinical, research, and education strategy. Curr Oncol. 2011;18:e260–4. doi: 10.3747/co.v18i5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canestraro A, Nakhle A, Stack M, et al. Oncology rehabilitation provision and practice patterns across Canada. Physiother Can. 2013;65:94–102. doi: 10.3138/ptc.2011-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Addington D, Kyle T, Desai S, Wang JL. Facilitators and barriers to implementing quality measurement in primary mental health care. Can Fam Physician. 2010;56:1322–31. [PMC free article] [PubMed] [Google Scholar]
- 27.Runowiczk CD, Leach CR, Henry NL, et al. American Cancer Society/American Society of Clinical Oncology breast cancer survivorship care guideline. CA Cancer J Clin. 2016;66:43–73. doi: 10.3322/caac.21319. [DOI] [PubMed] [Google Scholar]
- 28.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–40. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daudt HML, vanMossel C, Dennis DL, Leitz L, Watson HC, Tanliao JJ. Survivorship care plans: a work in progress. Curr Oncol. 2014;21:e466–79. doi: 10.3747/co.21.1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brant JM, Blaseg K, Aders K, Oliver D, Gray E, Dudley WN. Navigating the transition from cancer care to primary care: assistance of a survivorship care plan. Oncol Nurs Forum. 2017;43:710–19. doi: 10.1188/16.ONF.710-719. [DOI] [PubMed] [Google Scholar]
- 31.Boekhout AH, Maunsell E, Pond GR, et al. A survivorship care plan for breast cancer survivors: extended results of a randomized clinical trial. J Cancer Surviv. 2015;9:683–91. doi: 10.1007/s11764-015-0443-1. [DOI] [PubMed] [Google Scholar]
- 32.Mayer DK, Birken SA, Check DK, Chen RC. Summing it up: an integrative review of studies of cancer survivorship care plans (2006–2013) Cancer. 2015;121:978–96. doi: 10.1002/cncr.28884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCorkle R, Ercolano E, Lazenby M, et al. Self-management: enabling and empowering patients living with cancer as a chronic illness. CA Cancer J Clin. 2011;61:50–62. doi: 10.3322/caac.20093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kvale EA, Huang CS, Meneses KM, et al. Patient-centered support in the survivorship care transition: outcomes from patient-owned survivorship care plan intervention. Cancer. 2016;122:3232–42. doi: 10.1002/cncr.30136. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (cdc) Sorting Through the Evidence for the Arthritis Self-Management Program and the Chronic Disease Self-Management Program: Executive Summary of ASMP/CDSMP Meta-Analyses. Atlanta, GA: CDC; 2011. [Available online at: https://www.cdc.gov/arthritis/docs/asmp-executive-summary.pdf; cited 19 November 2017] [Google Scholar]
- 36.Arora NK, Reeve BB, Hays RD, Clauser SB, Oakley-Girvan I. Assessment of quality of cancer-related follow-up care from the cancer survivor’s perspective. J Clin Oncol. 2011;29:1280–9. doi: 10.1200/JCO.2010.32.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Loh SY, Packer T, Chinna K, Quek KF. Effectiveness of a patient self-management programme for breast cancer as a chronic illness: a non-randomised controlled clinical trial. J Cancer Surviv. 2013;7:331–42. doi: 10.1007/s11764-013-0274-x. [DOI] [PubMed] [Google Scholar]
- 38.Ventura F, Ohlen J, Koinberg I. An integrative review of supportive e-health programs in cancer care. Eur J Oncol Nurs. 2013;17:498–507. doi: 10.1016/j.ejon.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 39.Kuijpers W, Groen WG, Aaronson NK, van Harten WH. A systematic review of Web-based interventions for patient empowerment and physical activity in chronic diseases: relevance for cancer survivors. J Med Internet Res. 2013;15:e37. doi: 10.2196/jmir.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Groen WG, Kuijpers W, Oldenburg HSA, Wouters MWJM, Aaronson NK, van Harten WH. Empowerment of cancer survivors through information technology: an integrative review. J Med Internet Res. 2015;17:e270. doi: 10.2196/jmir.4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.College of Nurses of Ontario (cno) Toronto, ON: CNO; 2014. FAQs: Bill 179 [Web page] [Available at: http://www.cno.org/en/what-is-cno/regulation-and-legislation/legislation-governing-nursing/faq-bill-179; cited 19 November 2017] [Google Scholar]
- 42.Fillion L, Cook S, Veillette AM, et al. Professional navigation: a comparative study of two Canadian models. Can Oncol Nurs J. 2012;22:257–77. doi: 10.5737/1181912x224257266. [DOI] [PubMed] [Google Scholar]
- 43.Sisler J, McCormack-Speak P. Bridging the gap between primary care and the cancer system: the upcon Network of CancerCare Manitoba. Can Fam Physician. 2009;55:273–8. [PMC free article] [PubMed] [Google Scholar]
- 44.Elliott TE, Elliott BA, Regal RR, et al. Lake Superior Rural Cancer Care Project, part iii: provider practice. Cancer Pract. 2002;10:75–84. doi: 10.1046/j.1523-5394.2002.102005.x. [DOI] [PubMed] [Google Scholar]
- 45.Leese B, Allgar V, Heywood P, et al. A new role for nurses as primary care cancer lead clinicians in primary care trusts in England. J Nurs Manag. 2006;14:462–71. doi: 10.1111/j.1365-2934.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- 46.Canadian Nurses Association (cna) Effectiveness of Registered Nurses and Nurse Practitioners in Supporting Chronic Disease Self-Management. Ottawa, ON: CNA; 2012. [Available online at: https://www.cna-aiic.ca/~/media/cna/page-content/pdf-en/effectiveness_of_rns_and_nps_in_self-care_managment_e.pdf?la=en; cited 19 November 2017] [Google Scholar]
- 47.Massimi A, DeVito C, Brufola I, et al. Are community-based nurse-led self-management support interventions effective in chronic patients? Results of a systematic review and meta-analysis. PLoS One. 2017;12:e0173617. doi: 10.1371/journal.pone.0173617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lukewich J, Edge DS, VanDenKerkhof E, Tranmer J. Nursing contributions to chronic disease management in primary care. J Nurs Adm. 2014;44:103–10. doi: 10.1097/NNA.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 49.Yuille L. Optimizing Registered Nurse Roles in the Delivery of Cancer Survivorship Care Within Primary Care Settings. Hamilton, ON: McMaster University; 2015. [msc thesis] [DOI] [PubMed] [Google Scholar]