Abstract
The purpose of this study was to evaluate the clinical and radiological outcomes of 2 piezosurgical split techniques performed in conjunction with the sinus lift.
The present retrospective study included 20 patients with edentulism of the posterior maxilla who had undergone the sinus lift and alveolar ridge split treatment separately or the sinus lift combined with the monoblock alveolar ridge split. Differences between these 2 techniques were analyzed.
All the surrounding areas successfully produced an adequate bone volume for the insertion of implants. A clinical evaluation showed a mean vertical augmentation of 3.6 ± 0.4 mm in Group A and 3.2 ± 0.7 mm in Group B. With regards to the lateral augmentation, the clinical evaluation gives a mean gain of 5.2 ± 0.3 mm in Group A and 4.9 ± 0.5 mm in Group B. The mean vertical and horizontal bone augmentation recorded for both types of surgical procedures were comparable.
The proposed surgical procedures enabled the tridimensional volume of the alveolar ridge to be recreated. This resulted in the creation of a natural contour of hard and soft tissues which enabled a functional and aesthetic rehabilitation of the edentulous posterior maxilla to be obtained.
Keywords: implantology, oral rehabilitation, oral surgery
1. Introduction
Missing teeth can be replaced successfully via implant procedures providing that a sufficient bone volume and a favorable architecture of the alveolar ridge are present. Given these conditions, long term prognosis can be guaranteed.[1,2] A systematic review by Lang et al[3] revealed a survival rate of 96.5% after 5 years for single tooth replacement, 95.4% for implant–implant fixed bridgework and 90.1% for implant–tooth reconstruction. Nevertheless the difference between survival and success rate should be outlined because survival was defined as implant and fixed prosthesis present in the mouth while success was defined as being free from biological and/or technical complications.[4] Implant placement in the ideal prosthetic position, can be compromised by bone resorption due to the presence of an increased inter-arch distance or an unfavorable horizontal and sagittal intermaxillary relationship.[4–6] Resorbed ridges may need to undergo regeneration treatment prior to or in conjunction with implant placement in order to increase the amount of hard and soft tissues.[6,7] This enables us to reduce the crown/implant ratio, place axial implants and achieve a good occlusion and a quality aesthetic appearance.[8] The alveolar ridge split is a predictable and reliable procedure characterized by its low invasiveness. This procedure only allows us to obtain a significant bone augmentation only on the horizontal plane. For this reason we have introduced 2 types of piezosurgical split techniques which achieves both horizontal and vertical bone gain. These techniques are based on specific osteotomies of the vestibular cortex and the use of a mandibular ramus graft as an interpositional graft. In this study, the piezosurgical split techniques were used in conjunction with a maxillary sinus elevation to further increase the vertical augmentation. The maxillary bone, in edentulous superior premolars and molars, undergoes atrophy and sinus pneumatization which decreases the amount of bone in horizontal and vertical dimensions, making it insufficient for implant placement. Maxillary sinus elevation via a lateral approach is a reliable surgical technique for implant placement. It offers a positive long-term prognosis and survival rate comparable with that of implants placed in nongrafted maxillae, and in particular, rough surface implants.[5] Maxillary sinus elevation via a lateral approach is classed as a technique-sensitive procedure due to the high risk of Schneiderian membrane perforation.[10,11] The perforation of the Schneiderian membrane is the most common surgical complication and occurs in 7% to 10% to 35% of maxillary sinus elevation procedures.[5,11] In 1988, however the introduction of piezosurgery in oral surgery has made procedures such as sinus lift and alveolar ridge split both easier and safer.[12] In the presence of a Cawood and Howell's class V, 2 types of alveolar ridge split techniques were performed in conjunction with a maxillary sinus elevation via a lateral approach. The aim is to recreate the tridimensional volume of the alveolar ridge and restore the correct intermaxillary relationship.
2. Material and methods
A total of 24 patients, who presented an edentulous posterior maxilla and an inadequate bone volume for receiving oral implants, were referred to the Oral and Maxillofacial Department at the Gemelli Hospital between January 1 2014 and December 1 2016. Then 20 patients with edentulous superior premolars and/or molars were selected. To be eligible for this study, patients had to be at least 18 years old. In order to be included, patients needed to have a clinical and radiographical diagnosis of a maxillary sinus pneumatisation and a Cawood and Howell's class V with residual bone height ≤ 4 mm and bone width ≤4 mm. Participants were also required to have good oral hygiene prior to treatment and FMPS (full mouth plaque score) and FMBS (full mouth bleeding score); cut off was set at 15%. Patients were excluded if they were suffering uncontrolled systemic conditions or if they presented an American Society of Anesthesiologists’ physical status classification of IV. Patients were also excluded if they were taking medications known to modify bone metabolism, if they were smokers, if they engaged in excessive alcohol consumption or had ever been affected by periodontal disease. Patients were classified as smokers if they were currently smoking, or they were classified as past smokers if they had smoked in the previous 6 months but were not smoking currently, or they were classified as nonsmokers. Reasons for rejection were: controindicated general medical condition, periodontal disease, smoking and excessive alcohol consumption. Because of the retrospective nature of the present study, it was granted an exemption in writing by the institutional review board of the Catholic University of Sacred Heart of Rome. This study follows and complies with the STROBE checklist. We have read the Declaration of Helsinki and followed the guidelines in the present investigation. Each patient gave informed consent in writing. Patients treated with the sinus lift and alveolar ridge split treatment separately represent Group A, patient treated with the sinus lift combined with the monoblock alveolar ridge split represent Group B (Table 1). The 2 groups were homogeneous for sex, age, and bone atrophy. Group A was treated with a piezosurgical sinus lift and an alveolar ridge split which uses the horizontal partial thickness incision connecting the caudal ends of the 2 vertical osteotomies as rotational fulcrum during the greenstick fracture. Group B was treated with a sinus lift in conjunction with an alveolar ridge split which uses one of the 2 vertical osteotomies as rotational fulcrum during the greenstick fracture. All the patients were treated with a general anesthetic in a single surgical session. At least 2 hours prior to surgery, 1 g of amoxicillin was administered to each patient. A week long course of antibiotics was given to each patient postoperatively using 1 g of amoxicillin every 12 hours. Analgesics were prescribed for postoperative pain relief, 50 mg of ketoprofen every 12 hours for 3 to 4 days. A 4 mg single dose of intramuscular injection of dexamethasone was also administered. Patients were also asked to rinse their mouths with chlorhexidine 0.12% twice a day for 2 weeks following the surgery. Every patient underwent radiological examinations prior to the surgery for the preoperative planning to be completed. A cone beam computed tomography (CT) was performed so that the subsinus residual bone height could be evaluated. Two linear measurements were taken with a calibrated periodontal probe during both the first (Time 1, T1) and the second surgery (Time 2, T2). The first measurement (T1) was taken before the alveolar ridge splitting, and the second measurement (T2) was taken when the screws were removed (6 months). Vertical bone defects were measured from their apex (most resorbed point of the ridge on the vertical plane) to a line which connected the vestibular cusps of the teeth adjacent to the site where the volume was to be augmented. The width of the alveolar ridge was measured at the crestal level. The number of bone grafts required for each patient, donor sites and implants placed in each augmented site were recorded. Clinical follow-ups were carried out at 1 week, 1 month, 3 months, and 6 months after surgery. A radiological follow-up was performed 6 months after the operation with a cone beam CT scan (T2). Further follow-ups took place between 6 months and 18 months after surgery. Complications that occurred during the surgery or postoperatively were recorded. In order to assess the subsinus vertical bone augmentation, morphometric analyses were performed on the 2 CT scans of each patient: the one taken before the surgery (T0), and the one taken 6 months after the surgery (T2). The subsinus bone height was measured at 3 points each distant 1 mm from other through the cone beam CT scan. The first measurement was taken at the maximum height of the ridge while the other 2 were taken measuring the height of the ridge at 1 mm from the first point on both sides. From these 3 measurements the mean height was calculated. The tips used were produced by SILFRADENT (Silfradent srl, Sofia, Italy) and made from stainless steel 420 B. The tips were developed for a piezosurgery unit which has the ability to set the power, regulate the vibration function and regulate the percussion action (SURGYBONE SILFRADENT , Silfradent srl, Sofia, Italy).
Table 1.
Demographic variables.
2.1. Surgical technique
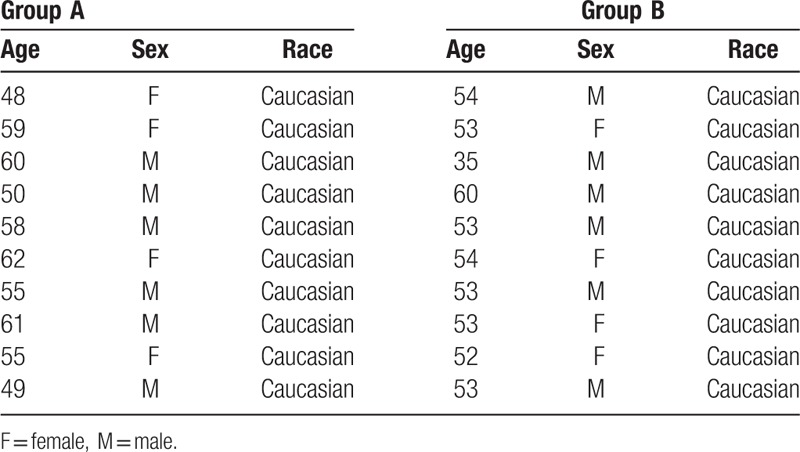
Under a local or general anaesthetic, a papillary sparing crestal incision, which is slightly palatal, is made on the atrophic ridge. This incision is followed by 2 vertical releasing incisions which extend beyond the mucogingival line. Then a muco-periosteal flap is raised, and the alveolar ridge and the lateral wall of the sinus are exposed. The lateral antrostomy is created either by outlining an island of bone, or, by completely removing a bone window on the lateral side of the sinus wall (Fig. 1). Firstly, using a piezoelectric handpiece, the Schneiderian membrane is elevated in order to expose the bone underneath, then hand instruments are used to mobilize and elevate it (Fig. 2). The Schneiderian membrane is detached by starting at the cranial surface and then continuing the incision distally, mesially, and palatally, in that order. Once the elevation is complete, it is possible to begin the alveolar ridge split, starting with the first tip from the first set, and then proceeding progressively with the subsequent tips. In Group A, the first osteotomy is carried out at the center of the occlusal side of the ridge. Then, the vertical osteotomies are performed on the proximal and distal ends of the crestal incision (Fig. 3). In our surgical procedure, the vertical osteotomies are bevelled, starting from the outer surface of the vestibular cortex and leading to the cancellous bone. As a result, the distance between the 2 vertical osteotomies is greater on the outer side than on the inner side of the vestibular cortical plate (Fig. 4). In this group, the height of the osteotomies was determined by the extension of the atrophic ridge. The osteotomy lines should be traced by progressively using the tips and once the osteotomy lines have been outlined, the tips are then used in order to progressively deepen the incision for the osteotomies. The tips should be calibrated so that the desired depth of cut can be achieved accurately. Once the desired depth of the crestal and vertical osteotomies had been achieved, the caudal ends of the vertical osteotomies were connected with a horizontal incision. This last incision is a partial thickness osteotomy. The greenstick fracture was made by using chisels. A cortical bone graft, of an appropriate size and shape, was harvested from the ipsilateral mandibular ramus utilising the aforementioned tips and chisels. Bone chips can be collected from the same donor site. The cortical graft was gently hammered on between the vestibular and lingual cortex, acting as a bone wedge until the desired separation of the 2 cortices was reached. The cortical graft was then stabilized using titanium screws. In order to obtain supracrestal regeneration, the bone graft between the vestibular and palatal cortices can be fixed at a higher level with osteosynthesis screws allowing it to protrude from the occlusal side of the 2 bone plates. In this way, the bone graft acts as a vertical support creating a space for the insertion of particulated autografts mixed with bone xenograft (Geistlich Bio-Oss). In Group B, the vertical osteotomies of the piezosurgical split on the vestibular bone segment of the maxilla reached the bone window on the lateral wall of the sinus, and one of them was a partial thickness osteotomy. Once the mesial and distal vertical osteotomies had reached the window on the lateral wall of the sinus, the greenstick fracture was performed using the partial thickness vertical osteotomy as a rotation fulcrum (Fig. 4). A cortical bone graft, of an appropriate size and shape, was harvested from the ipsilateral mandibular ramus utilising the aforementioned tips and chisels. Bone chips can be collected from the same donor site. The cortical graft was gently hammered on between the vestibular and lingual cortex, acting as a bone wedge until the desired separation of the 2 cortices was reached (Fig. 5). The cortical graft was then stabilized using titanium screws. In order to obtain supracrestal regeneration, the bone graft between the vestibular and palatal cortices can be fixed at a higher level with osteosynthesis screws allowing it to protrude from the occlusal side of the 2 bone plates. In this way, the bone graft acts as a vertical support creating a space for the insertion of particulated autografts mixed with bone xenograft (Geistlich Bio-Oss). The sinus is grafted using autologous bone chips mixed with bone xenograft (Geistlich Bio-Oss) and finally the grafted site is covered with a resorbable collagen membrane (Geistlich Bio-Gide). The mucoperiosteal flap is repositioned and fixed with 4-0 nonresorbable sutures. If the buccal segment were to detach from the jaw, it can be replaced and stabilized by inserting screws through the graft and the vestibular segment. The sutures were removed after 10 days. The surgical site was allowed to heal for 6 months. When healing was complete, the crestal cut was exposed and the screws were removed. Implant beds were prepared in the conventional way, avoiding damage to the crestal bone, and the implants were positioned in accordance with the prosthetic rehabilitation program. The submerged implants were then subsequently exposed, and the patients received fixed implant-supported restorations.
Figure 1.

Group A: Design of the vertical osteotomies.
Figure 2.
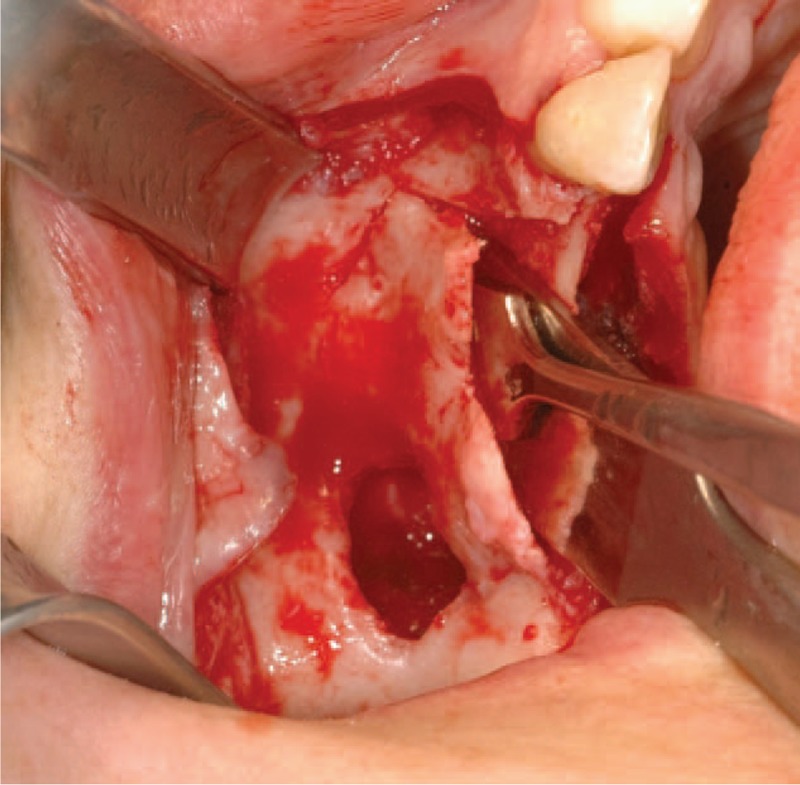
Group B: Greenstick fracture of the vestibular bone segment.
Figure 3.
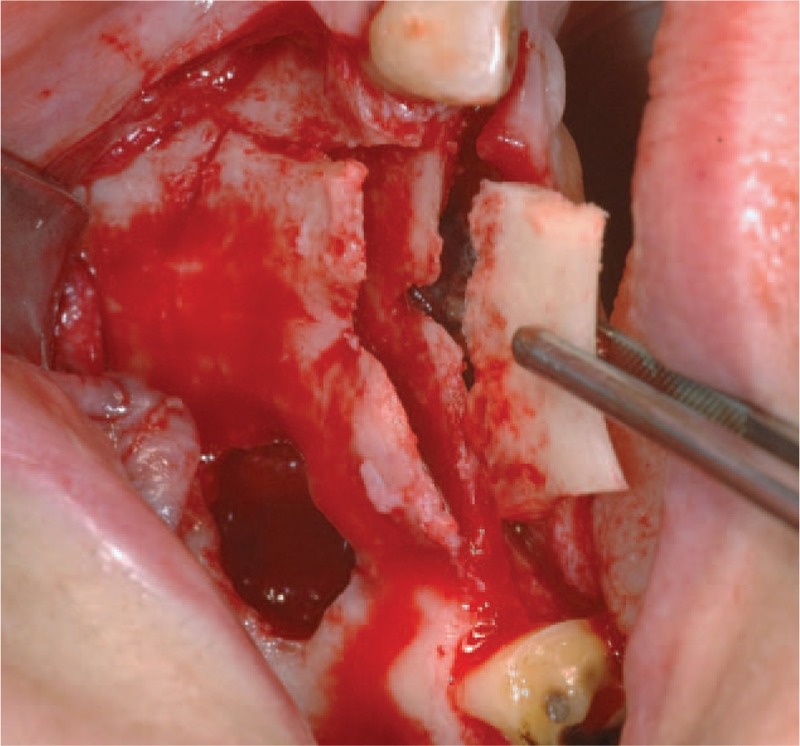
Group B: Cortical graft harvested and placed between the 2 cortices.
Figure 4.
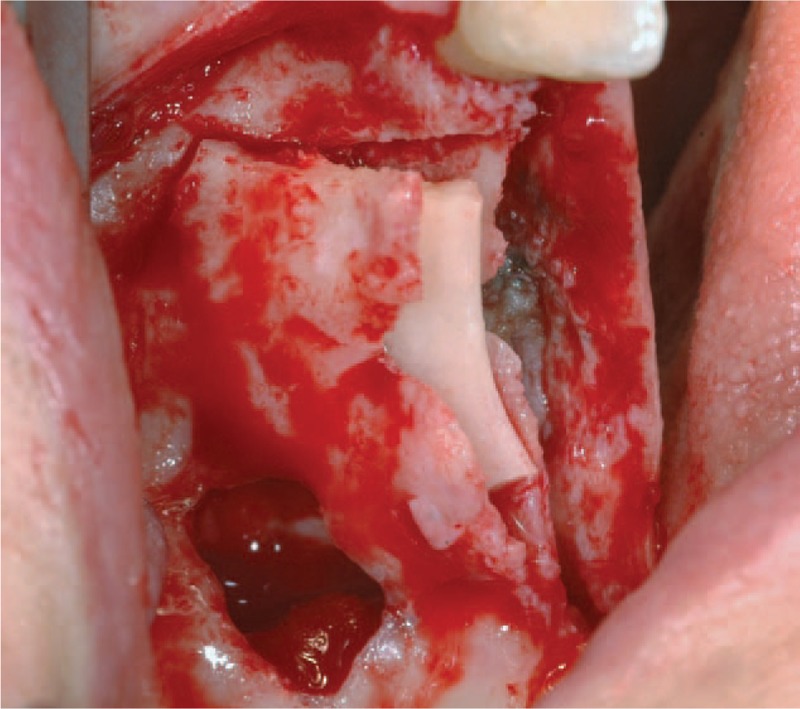
Group B: Bone graft between the vestibular and palatal cortices placed at a higher level to let it protrude from the occlusal aspect of the 2 bone plates.
Figure 5.
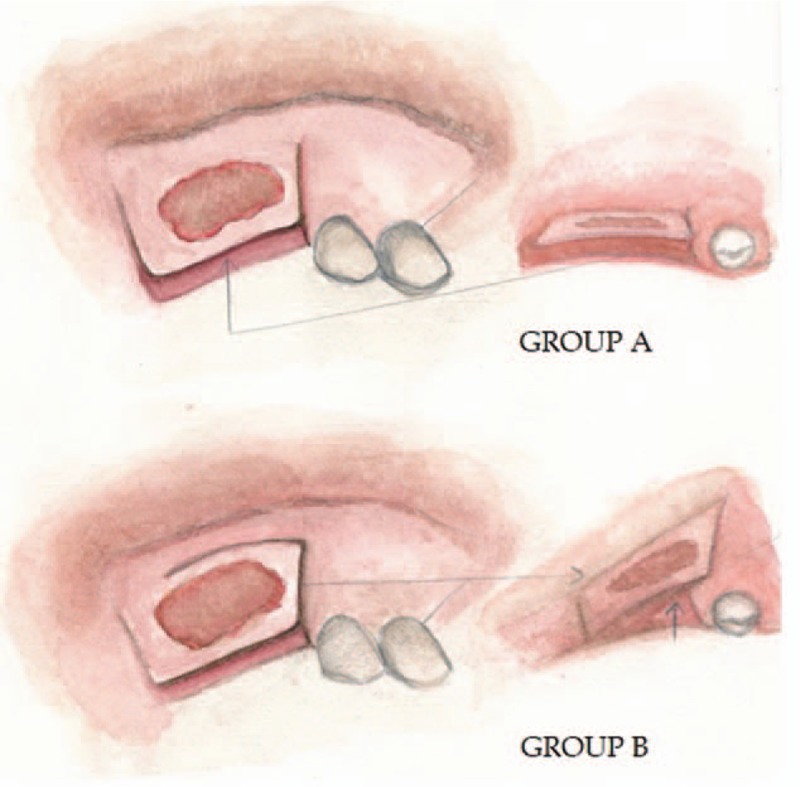
Illustrations of the 2 proposed techniques.
2.2. Statistical methods
A 2 way repeated t-test was performed in order to identify any difference in the clinically measured vertical and horizontal bone augmentation and the radiographically measured subsinus bone augmentation between Group A and Group B. All statistical analyses were carried out using STATA14 for Windows software with a 2-tailed P value of .05 used as a threshold for significance.
3. Results
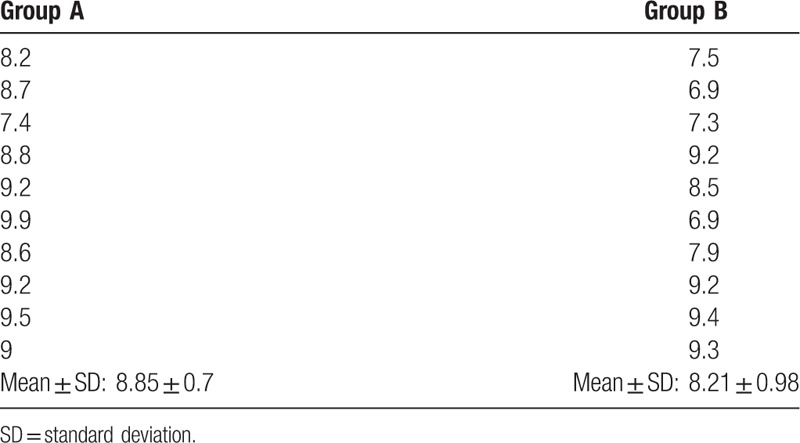
All the patients were partially edentulous. The study sample consisted of twenty patients (eight females and twelve males; mean age ± standard deviation: 53.8 ± 5.9 years, range: 35–62 years). Clinical evaluation was performed at T1 and T2 and radiographic evaluation at T0 and T2. On the whole, all of the defective sites that were treated exhibited excellent bone formation. The same operator took all the measurements at T0, T1, and T2 in accordance with the protocol. A clinical evaluation shows a mean vertical augmentation of 3.6 ± 0.4 mm in Group A and 3.2 ± 0.7 mm in Group B. With respect to the lateral augmentation, the clinical evaluation gives a mean gain of 5.2 ± 0.3 mm in Group A and 4.9 ± 0.5 mm in Group B. No significant differences were observed between the 2 groups in terms of vertical augmentation (P < .15) and horizontal augmentation (P < .29) (Tables 2 and 3]. The radiographic evaluation gives a mean increase in the subsinus bone height of 9 ± 0.7 mm in Group A and a mean increase of 8.2 ± 1 mm in Group B. The difference between Group A and Group B was not significant also in terms of subsinus bone height (P < .12) (Table 4). There were no cases of infection, and no complications were recorded at the donor sites. Within Group A, no patients developed complications at the recipient sites. In Group B, 2 patients developed postoperative complications at the recipient sites. The postoperative complications incurred were 2 cases of premature membrane exposure with soft tissues dehiscence. Both complications were easily resolved without affecting implant placement. Soft tissue healing was uneventful and the pain and swelling incurred was comparable to that usually incurred in dentoalveolar procedures. Each patient required only one donor site and therefore twenty bone grafts were harvested. All the surrounding areas provided an adequate volume of bone and so the implants could be successfully inserted, in accordance to the prosthetic plan. A total of 40 implants were placed. All implants achieved primary stability and were deemed successful according to the Albrektsson criteria.[13] After the osseointegration of the implants, prosthetic loading was successfully reached in all cases.
Table 2.
Distribution of horizontal bone augmentation measures (millimeters) after surgery.
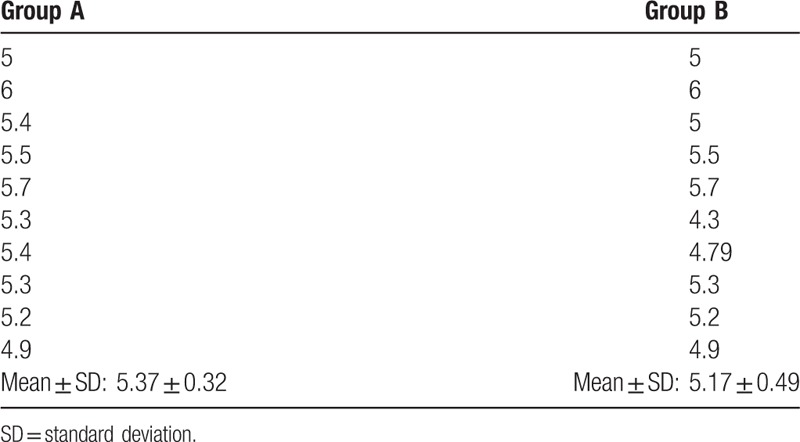
Table 3.
Distribution of vertical bone augmentation measures (millimeters) after surgery.
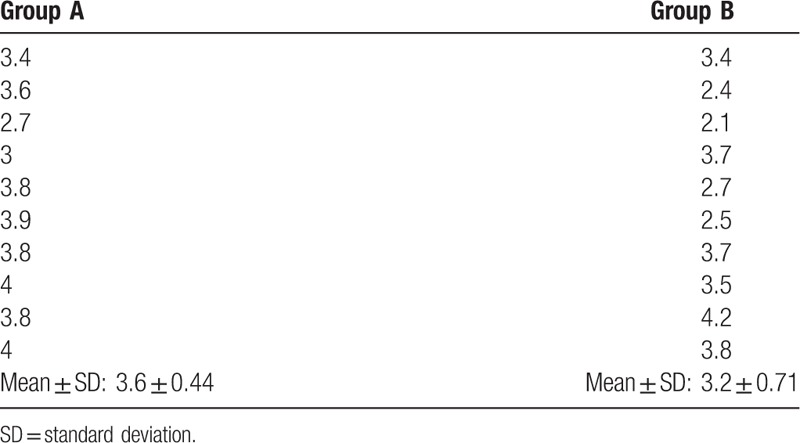
Table 4.
Distribution of subsinus bone augmentation measures (millimeters) after surgery.
4. Discussion
Following the loss of a tooth, the alveolar ridge undergoes bone resorption in the vertical, trasversal, and sagittal plane. Bone resorption in an edentulous or a partially edentulous alveolar ridge is a progressive process. Loss of alveolar bone may also occur prior to tooth extraction due to periodontal disease, a periapical pathology or as a result of damage caused to teeth and bone from a trauma or a tooth extraction procedure.[1,2]
Implant placement in the ideal prosthetic position, can be compromised by bone resorption due to the presence of an increased inter-arch distance or an unfavorable horizontal and sagittal intermaxillary relationship.[4–6] Therefore resorbed ridges may need to undergo regeneration treatment.
Alternative solutions, such as placing short, tilted or zygomatic implants, have been proposed to avoid bone augmentation procedures and to resolve the problem of the atrophic posterior maxilla.
The gold standard in bone regeneration procedures is the autogenous bone graft. There are, however, some drawbacks to the autogenous bone graft. These include donor site morbidity, unpredictable resorption, a limited provision of bone, and the request of an additional surgical site.[6] Thus, in the search for suitable alternatives, substitute bone materials have been introduced, each with specific characteristics and uses. Other factors that influence the clinical outcome of the augmentation procedure are the localization, the extension, and the morphology of the bone defect. The localization and the tridimensional architecture of the bone defect determine the choice of the augmentation procedure. Alveolar ridge defects are classified according to whether the bone deficiency is predominantly horizontal, vertical, or both.[9] Bone defects in the lateral and vertical dimensions of the maxilla can be treated before or at the same time as the implant placement, using the following procedures: Guided bone regeneration (GBR), alveolar ridge split, onlay/inlay bone graft, and maxillary sinus elevation. Regeneration techniques can be categorized according to their main objective in lateral or vertical bone augmentation procedures.[9] A maxillary sinus elevation, via a lateral approach, and an alveolar ridge split are well-accepted treatment options in implant dentistry.
The maxillary sinus elevation, which augments the subsinus bone height, aims to create right vertical conditions for an implant supported, prostethic rehabilitation of the posterior maxilla. This procedure, however, does not recreate a correct inter-arch distance, or correct transversal and sagittal intermaxillary relationships, such as hard and soft tissues contour, which are essential requirements to obtain functional and esthetic success. Among the available bone augmentation procedures, only inlay/onlay bone grafts, GBR and split ridge/ridge expansion techniques represent commonly applied methods for the recreation of correct intermaxillary relationships, adequate bone morphology and bone volume.[5] The existing vertical ridge augmentation procedures are still not wholly reliable. A systematic review reported that, even though there is clinical and histological evidence of their success, there is a low level of predictability and a high rate of complications.[14]
The most common complication after GBR is barrier membrane exposure and its sequelae.[14] Chiapasco et al[15] reported minor complications after onlay bone grafting procedures: transient paresthesia of the area innervated by the inferior alveolar nerve was experienced in 3 out of 8 patients. In a study conducted by Cordaro et al[16] a high percentage of patients experienced a transient paresthesia after bone harvesting from the chin.
Furthermore a form stable membrane is necessary for vertical GBR. On the other hand, when utilizing the existing procedures, lateral bone augmentation has a high level of predictability. Several studies have recently been conducted in this area surrounding the principles of GBR, however, there are still no recommendations with regards to the ideal graft and membrane material.[9] In this study 2 surgical procedures were executed and compared. The results revealed that both of the procedures allow us to place dental implants in an ideal position and direction for prosthetic rehabilitation. In both groups, the maxillary sinus was grafted using particulated autografts mixed with bone xenograft (Geistlich Bio-Oss). In Group A, the alveolar ridge split had some special features, such as the realization of 2 vertical osteotomies with an oblique course. These vertical osteotomies increased the contact area between the 2 bone segments, improving the stability and the engraftment. Another feature is the horizontal osteotomy on the base of the vestibular cortical plate. This acts as a rotational axis during the greenstick fracture of the bone segment. The presence of this feature predetermines the location of the greenstick fracture and, this partial thickness osteotomy, prevents interference with the execution of the greenstick fracture. This facilitates the rotation and helps to avoid fractures in the vestibular cortical plate. In Group B, the alveolar ridge split had vertical osteotomies with an oblique course which stretched to the lateral window of the maxillary sinus. To determine the location of the greenstick fracture, one of these incisions is a partial thickness osteotomy which acts as rotational axis. In both procedures, once the split ridge was complete, a graft of the cortical bone was harvested with the piezosurgical tips, positioned between the 2 cortices and fixed with screws. By surrounding the cortical graft on both sides with cancellous bone, it is possible to create an osteogenic space which promotes engraftment and bone regeneration. It has also been demonstrated that the application of grafts or bone substitutes in the space between the 2 cortical bones, together with a membrane, has resulted in a significant reduction in horizontal bone resorption compared to a one step split technique.[17] In cases where further vertical augmentation is needed, the graft between the 2 cortical bones can be fixed at a higher level in order to allow the graft to protrude from the occlusal surface. Once the bone graft is in position, it creates and maintains a space under the membrane and around its edges which allows bone chips mixed with bone allograft to be inserted. Fixing the bone graft at a higher level makes it possible to use a nonform stable membrane such as a native collagen membrane, which is easier to handle both in the surgical and postoperative phases. According to the principles of GBR, this in turn, promotes further bone regeneration which helps to avoid soft tissue collapse. GBR has proven an effective procedure in both humans and in experimental animals.[4,18–20] The concept of this technique advocates that regeneration of osseous defects is predictably attainable via the application of occlusive membranes. These membranes mechanically exclude nonosteogenic cell populations from the surrounding soft tissues, thereby allowing osteogenic cell populations, originating from the parent bone, to inhabit the osseous wound.[21]
The use of piezosurgery enabled the operator to progressively deepen the osteotomy, obtain linear resected margins of the osteotomies, reduce the risk of uncontrolled bone fracture and preserve the Schneiderian membrane.
In this study, the mean vertical and horizontal augmentation recorded for Group A and Group B were comparable. The ideal conditions for traditional ridge splitting are sites that do not require vertical ridge augmentation.[22] When the splitting technique proposed in this study is used in combination with the maxillary sinus elevation, however, it is possible to treat a transversal bone deficit with vertical resorption, and recreate the correct intermaxillary relationships. The results showed an increase in bone thickness as well as considerable vertical augmentation. After the surgery, the incorporation and remodeling of the bone graft created a natural contour of hard and soft tissues. Both the procedures guarantee good results in terms of bone augmentation, even though a difference in the level of risk of complications was noticed. The results of the investigation show that the technique performed in Group A allows us to reduce the range of variability and this is related to the lower incidence of complications recorded in the postoperative phase. In Group B, a higher risk of premature membrane exposure was recorded and, consequentially, the resulting bone regeneration was compromised. For this reason, preference should be given to the surgical procedure used for Group A as it entails a lower level of risk of postoperative complications and guarantees more predictable outcomes. The reasons are not fully understood but we hypothesize that these results are related to the greater technical difficulty as well as mechanical and microbiological factors. The technique performed in Group B has a greater technical difficulty. As far as mechanical factors are concerned, it is necessary to obtain the stability of the bone graft and the osteotomized bone segment, the stability of the overlying membrane and the passivation of the flap, which may be difficult. Finally linking the sinus lift with the split technique and the bone graft may be significant in terms of bone regeneration after the membrane exposure and the bacterial contamination. In Group A, although the 2 procedures are performed in a single stage approach, they remain unlinked.
5. Conclusion
The proposed piezosurgical procedures allowed us to recreate the tridimensional volume of the alveolar ridge, restore correct intermaxillary relationships and place implants in a prosthetically ideal position. These procedures created a natural contour of hard and soft tissues which resulted in a functional and aesthetically pleasing rehabilitation of the edentulous posterior maxilla.
Author contributions
Data curation: Paolo De Angelis.
Investigation: Alessandro Moro, Giulio Gasparini, Giuseppe D’Amato, Pier Carmine Passarelli, Gianmarco Saponaro, Paolo De Angelis.
Methodology: Alessandro Moro, Giulio Gasparini, Gianmarco Saponaro.
Project administration: Sandro Pelo.
Supervision: Alessandro Moro, Sandro Pelo, Gianmarco Saponaro.
Writing – original draft: Paolo De Angelis, Pier Carmine Passarelli.
Writing – review & editing: Pier Carmine Passarelli, Paolo De Angelis.
Footnotes
Abbreviations: CT = computed tomography, FMBS = full mouth bleeding score, FMPS = full mouth plaque score, g = grams, GBR = guided bone regeneration, mg = milligrams, mm = millimeters, T0 = time 0, T1 = time 1, T2 = time 2.
The authors have no conflicts of interest to disclose.
References
- [1].Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 2003;23:313–23. PubMed PMID: 12956475. [PubMed] [Google Scholar]
- [2].Winkler S. Implant site development and alveolar bone resorption patterns. J Oral Implantol 2002;28:226–9. [DOI] [PubMed] [Google Scholar]
- [3].Lang NP, Pjetursson BE, Tan K, et al. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth—implant-supported FPDs. Clin Oral Implants Res 2004;15:643–53. [DOI] [PubMed] [Google Scholar]
- [4].Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10-16-year follow-up of non-submerged dental implants. Clin Oral Implants Res 2010;21:772–7. [DOI] [PubMed] [Google Scholar]
- [5].Chiapasco M, Casentini P, Zaniboni M. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants 2009;24:237–59. [PubMed] [Google Scholar]
- [6].Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants 2009;24:218–36. [PubMed] [Google Scholar]
- [7].Sammartino G, Cerone V, Gasparro R, et al. The platform switching approach to optimize split crest technique. Case Rep Dent 2014;2014:850470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Terheyden H, Cordaro L. Introduction in: Ridge Augmentation Procedures in Implant Patients. ITI Treatment Guide Vol. 7. 2014;Berlin: Quintessence Publishing Co, Ltd, 1-2. [Google Scholar]
- [9].Sanz-Sánchez I, Ortiz-Vigón A, Sanz-Martín I, et al. Effectiveness of lateral bone augmentation on the alveolar crest dimension: a systematic review and meta-analysis. J Dent Res 2015;94(9 suppl):128S–42S. [DOI] [PubMed] [Google Scholar]
- [10].Ardekian L, Oved-Peleg E, Mactei EE, et al. The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. J Oral Maxillofac Surg 2006;64:277–82. [DOI] [PubMed] [Google Scholar]
- [11].Hernández-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus-lift procedures. Clin Oral Implants Res 2008;19:91–8. [DOI] [PubMed] [Google Scholar]
- [12].Magrin GL, Sigua-Rodriguez EA, Goulart DR, et al. Piezosurgery in bone augmentation procedures previous to dental implant surgery: a review of the literature. Open Dent J 2015;9:426–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1986;1:11–25. Review. [PubMed] [Google Scholar]
- [14].Rocchietta I, Fontana F, Simion M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. J Clin Periodontol 2008;35(8 suppl):203–15. [DOI] [PubMed] [Google Scholar]
- [15].Chiapasco M, Zaniboni M, Rimondini L. Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2-4-year prospective study on humans. Clin Oral Implants Res 2007;18:432–40. [DOI] [PubMed] [Google Scholar]
- [16].Cordaro L, Amade’ DS, Cordaro M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin Oral Implants Res 2002;13:103–11. [DOI] [PubMed] [Google Scholar]
- [17].Ella B, Laurentjoye M, Sedarat C, et al. Mandibular ridge expansion using a horizontal bone-splitting technique and synthetic bone substitute: an alternative to bone block grafting? Int J Oral Maxillofac Implants 2014;29:135–40. [DOI] [PubMed] [Google Scholar]
- [18].Lundgren AK, Sennerby L, Lundgren D, et al. Bone augmentation at titanium implants using autologous bone grafts and bioresorbable barrier. Clin Oral Implants Res 1997;8:82–9. [DOI] [PubMed] [Google Scholar]
- [19].Buser D, Dula K, Hirt HP, et al. Lateral ridge augmentation using autografts and barrier membranes: clinical study with 40 partially edentulous patients. J Oral Maxillofac Surg 1996;54:420–32. [DOI] [PubMed] [Google Scholar]
- [20].Cortellini P, Bartolucci E, Clauser C, et al. Localized ridge augmentation using guided tissue regeneration in humans. Clin Oral Implants Res 1993;4:203–9. [Google Scholar]
- [21].Retzepi M, Donos N. Guided bone regeneration: biological principle and therapeutic applications. Clin Oral Implants Res 2010;21:567–76. [DOI] [PubMed] [Google Scholar]
- [22].Mayur S, Khairnar, Darshana Khairnar, et al. Modified ridge splitting and bone expansion osteotomy for placement of dental implant in esthetic zone. Contemp Clin Dent 2014;5:110–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


