Abstract
Diagnosis-related groups (DRGs) have been receiving increasing attention in health service research in China. In the present study, we used the 2014 Beijing-Diagnosis Related Groups (BJ-DRGs) to evaluate the inpatient service performance of the clinical subspecialty “major operation of the digestive system” of a cancer specialist hospital.
The research hospital is one of 16 public municipal hospitals overseen by the Beijing Health Bureau (“16 hospitals”). Discharge data collected between 2008 and 2015 were drawn from the front pages of the medical records of these hospitals. After the data were reported to the Beijing Public Health Information Centre, as well as being grouped using the BJ-DRGs. We evaluated the service performance of this subspecialty in terms of capacity, efficiency, and service quality, based on the BJ-DRGs risk adjustment tool.
From 2008 to 2015, the total weight of the subspecialty in the research hospital increased annually. In 2015, the cases in this hospital accounted for 50.27% of the total in 16 hospitals. The time consumption index was 0.91, whereas the charge consumption index was 1.24, which was 24% higher than the average in16 hospitals. The mortality rates of the middle–low risk groups (GB15 and GB25) in the research hospital and the 16 hospitals were zero, while the mortality rates for the middle–high risk groups (GB11 and GB23) in the research hospital were significantly lower than those in 16 hospitals.
The service capacity of the subspecialty steadily increased in the research hospital. However, the hospital must offer more attention to complex digestive disease cases (GB11/GB23) and strictly control hospitalization expenses, while maintaining the advantages of service efficiency and quality.
Keywords: clinical subspecialty, diagnosis-related groups (DRGs), medical service performance evaluation
1. Introduction
The performance assessment of medical services offers a basis for rational decision-making and service improvement, making these an important part of medical services research.[1–3] When assessing the service performance of different healthcare providers from different hospitals, the conventional method relies on measuring the number of discharged cases and operations, average length of stay (ALOS), bed rotation rate, etc. However, since this method does not consider the effects of the disease or disease difficulty, it cannot provide an objective assessment result. In order to assess the service capacity of different medical service providers, “case-mixing” is used to classify cases with similar clinical processes or resource consumption, allowing cases in the same group to be directly compared. Cases in different groups, by contrast, can be compared after adjustment, according to weight.[4] A diagnosis-related group (DRG) is a type of case-mix system that included the classification of hospital discharge cases, according to clinical process consistency and homogeneous resource consumption. In fact, this is one of the most popular health services management tools.[3,5,6] This was first developed by Fetter et al at Yale University in 1967,[7] was used in the United States of America since 1982, and implemented in Europe and in fast-developing countries in Asia and Sub-Saharan Africa.[3] Since then, the DRG system has become widely used in multiple areas, including healthcare reimbursement, health expense budgeting, cost control, health service performance assessment, quality assurance, and planning.[3,8–11]
DRGs are based on case-mixes of diagnoses and operations.[3,5,12] It considers a comprehensive range of clinical conditions, such as disease diagnosis, complications and comorbidity, surgery and treatment operations, and the patients individual characteristics of (e.g., age and gender). Accordingly, cases with a similar clinical course and resource consumption are assigned to the same DRGs.[3,5] Adjacent DRGs (ADRGs) refer to groups of cases with the same main diagnosis or treatment operation. According to the DRG grouping process, clinical experts primarily rely on the main diagnosis or operation, and rarely consider individual characteristics, complications, and comorbidities related to the major disease category (MDC), when designating ADRGs. As such, ADRGs reflect certain subspecialties of a medical discipline.[13,14]
In China, improving medical service quality in hospitals has become one of the main goals of governmental health administrative departments.[15] Consequently, DRGs have been receiving increasing attention in recent health service research. Service performance can be evaluated at many levels, such as the case, disease, case-mix, physician, department, and hospital. In the present study, we analyzed this at the level of ADRGs; that is, the clinical subspecialty.[13,16,17]
The research hospital is a cancer special hospital in Beijing, which is one of the Ministry of Education's Key Laboratories of Carcinogenesis and Translational Research. It is also one of the 16 public municipal hospitals overseen by the Beijing Health Bureau (“16 hospitals”). Compared to this research hospital, all hospitals are general hospitals. Every year, numerous cancer patients receive treatment at this research hospital. In 2015, the number of surgical cases of digestive system diseases was 3371, of which 78.91% belonged to ADRGs called “major operation of the digestive system.” Therefore, analyzing the medical service performance of this subspecialty using a DRG risk adjustment tool and evaluating its strengths and weaknesses in terms of service capacity, efficiency, and quality would be of great importance in helping the hospital carry out the fine-tune management of this specialty, and further improving its offered medical services.[18] To the best of our knowledge, it is important to note that no research has been conducted on the performance assessment of the medical services of specific ADRGs. Hence, our study will provide methodological support for researchers in the future.
2. Materials and methods
2.1. Data sources
The research data were drawn from the discharge data on the front pages of medical records (FPMRs) of acute inpatients in hospitals from 2008 to 2015. These data were obtained only after they had been reported to the Beijing Public Health Information Centre, and were grouped according to the 2014 edition of the Beijing-DRGs (BJ-DRGs). The ADRGs considered “major operation of digestive system diseases,” which included 4 DRGs: GB11, which includes major operations of the esophagus, stomach, and duodenum that are associated with significant complications or comorbidity; GB15, which includes major operations of the esophagus, stomach, and duodenum that are not associated with complications or comorbidity; GB23, which includes major operations of the small intestine, large intestine, and rectum that are associated with complications and comorbidity; GB25, which includes major operations of the small intestine, large intestine, and rectum that are not associated with complications or comorbidity. For each DRG, the following data were collected for the research hospital and all 16 hospitals (i.e., overall data) in 2015: weight, number of cases, ALOS, average cost, and mortality.
2.2. Analysis
In recent study, the BJ-DRGs were used as a risk adjustment tool to evaluate the performance of inpatient medical services in the ADRG of the research hospital in terms of capacity, efficiency, and service quality.[5,6]
2.3. Capacity index
The indexes for capacity include the total weight of DRG groups and the case-mix index (CMI). The weight of a DRG is calculated using the number of cases, costs, and constituents of that DRG in a given region through statistical methods, in which the weight represents the treatment complexity and consumption of medical resources of a given DRG.[18] A weight of 1 indicates that the DRG disease group has an average treatment complexity within a given period in the region. The total weight refers to the total output of inpatient medical services after risk adjustment for a given DRG, which allows for a more accurate reflection of the medical services output of a unit compared to the “number of discharged cases.”[19,20] The larger the weight, the greater the output of inpatient medical services became. The weight value is usually used to determine the difference in treatment costs between different case types. The more complex the disease, the higher the treatment cost. The CMI represents the weight per case, and is calculated by dividing the total weight value by the total number of cases. The CMI reflects the overall technical difficulty of discharged cases in an assessment unit. Higher CMI values indicate a greater difficulty in treating a discharged case in that unit.[21,22]
2.4. Efficiency index
The efficiency assessment of inpatient medical services includes 2 indicators: the time consumption index and charge consumption index. These are calculated by standardizing medical expenses and length of hospital stay to facilitate comparison between diseases. The time and charge consumption indexes increase with the length of hospital stay or expenses, respectively. An index of 1 indicates that the consumption of resources for treatment of the same disease in the assessment unit is equivalent to that of the average in the Beijing region. Therefore, the lower the value, the lower the average hospital cost and length of hospital stay for the same disease.[4–6,18,23]
2.5. Quality index
The service quality indexes include the raw mortality and mortality of the middle–low risk group and middle–high risk group. When DRGs were used for the performance assessment of medical institutions, generally, “inpatient mortality of low-risk group cases” was employed as an index of service quality.[7–9,22,24] However, since there are no low-risk mortality cases in the subspecialty of the research hospital and the “16 hospitals” in 2015, the above mortality indexes were used. These indexes were compared and analyzed in the research hospital and the 16 hospitals.
All data were sorted and analyzed using SPSS 21.0 (SPSS, Inc., Chicago, IL). This study involved neither the human body nor animal experiments or the use of private data.
3. Results
3.1. Inpatient care performance capacity of the subspecialty in the research hospital between the year 2008 and 2015
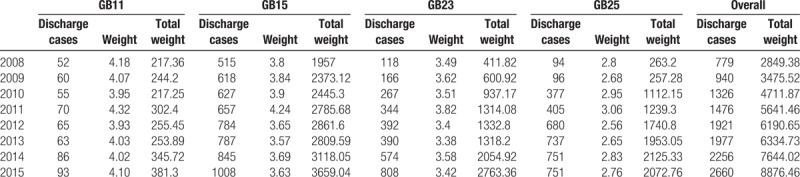
From the year 2008 to 2015, the total weight of the subspecialty in the research hospital increased annually. The overall weight in 2015 was 3.12 times of that in 2008. Furthermore, the total weight of each of the 4 DRGs significantly increased, suggesting that the inpatient care capacity of the subspecialty improved steadily over the study period (Table 1).
Table 1.
Inpatient care performance capacity of the subspecialty in the research hospital from 2008 to 2015.
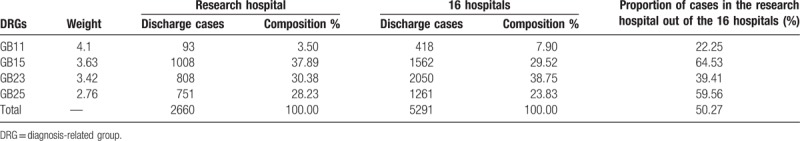
3.2. DRG performance results in the research hospital in 2015
The number of cases for the subspecialty of “major operation of digestive system diseases” in the research hospital in 2015 accounted for 50.27% of all cases in this subspecialty in the 16 hospitals. Regarding the composition of ADRGs, the proportions of the GB15 and GB25 groups in the research hospital were higher than was that of all 16 hospitals. However, the proportions of the GB11 and GB23 groups were lower than was that of the 16 hospitals (Table 2).
Table 2.
Case composition of the subspecialty in the research hospital and 16 hospitals in 2015.
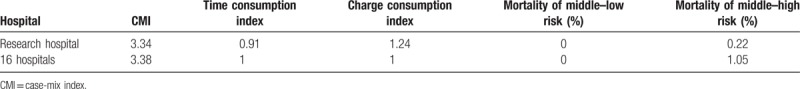
Except for the GB11 group, the ALOS in the 3 remaining groups was lower in the research hospital than in the 16 hospitals, while the average cost in all 4 DRGs was higher. In 2015, the mortality rate was zero in both GB15 and GB25 groups in all hospitals. However, the mortality in the GB11 and GB23 groups was lower in the research hospital than in the 16 hospitals (Table 3).
Table 3.
Comparison of ALOS, average cost, and raw mortality of the 4 DRGs in the research hospital and 16 hospitals in 2015.

The CMI of the subspecialty in the research hospital was slightly lower than was that in the 16 hospitals. It was mainly due to the case structure of the GB11 and GB23 groups, which had higher weights, and lower in the research hospital than in the 16 hospitals (Table 4). The time consumption index of the hospital was lower than was that of the 16 hospitals. However, the charge consumption was 24% higher than the average of the 16 hospitals. The mortality rate in the middle–low risk groups (GB15 and GB25) was zero in all hospitals. However, for the middle–high risk groups (GB11 and GB23), it was significantly lower in the research hospital than in the 16 hospitals.
Table 4.
Comparison of capacity, efficiency, and service quality indexes of the subspecialty in the research hospital and 16 hospitals in 2015.
3.3. Analysis of DRG indicators of the subspecialty among related wards in the research hospital in 2015
The discharged cases of the subspecialty were mainly located in 6 wards (A, B, C, D, G, and H) of the research hospital. The numbers of cases of GB11, GB15, GB23, and GB25 in the above 6 wards accounted for 66.67%, 88.09%, 86.01%, and 96.67% of all cases of each DRG in the research hospital, respectively. Furthermore, the total number of cases in these 4 DRGs accounted for 89.13% of all cases of the subspecialty in the research hospital. Therefore, we mainly analyzed the inpatient care performance for the studied ADRGs in these 6 wards (Table 5).
Table 5.
Composition of DRGs making up the subspecialty in the related wards of the research hospital in 2015.
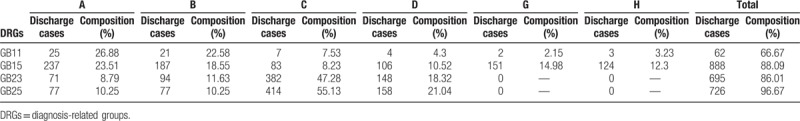
Wards A and B mainly handled gastric cancer cases, and contained 49.46% and 42.06% of cases in the GB11 and GB15 groups, respectively, in the research hospital. Ward C mainly handled cases of colon cancer and rectal cancer, and contained 47.28% and 55.13% of cases in the GB23 and GB25 groups, respectively. Ward D was characterized by minimally invasive surgical treatment for tumors, including patients with gastric cancer, colon cancer, rectal cancer, etc. In 2015, approximately 69.23% of all cases underwent minimally invasive surgery. Wards G and H mainly handled patients with esophageal cancer, including 5.38% and 27.28% of cases in the GB11 and GB15 groups in the research hospital.
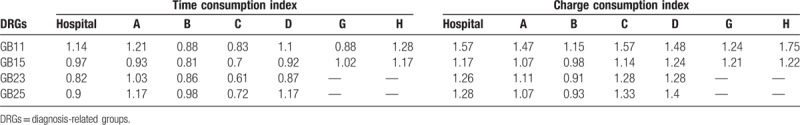
The time consumption index in the GB11 group in the research hospital was 14% higher than the average of the 16 hospitals. However, in the other 3 groups, it was lower than the average. Furthermore, the time consumption index in the GB11 and GB25 groups in wards A and D and the GB15 group in ward H were significantly higher than the average of the 16 hospitals. In wards B, C, and G, the time of the 4 DRGs was well controlled. The costs of all 4 DRGs were higher in the research hospital than the average in the 16 hospitals. Furthermore, except for ward B, the costs related to DRGs in 3 other wards were higher than those in the 16 hospitals combined. These detailed results are shown in Table 6.
Table 6.
Comparison of time consumption and charge consumption index of the subspecialty in related wards of the research hospital in 2015.
4. Discussion
DRG service performance indicators are calculated using BJ-DRGs based on large sample data, thereby producing highly objective results. Thus, when evaluating the clinical specialty of the medical services of hospitals, DRG technology provides not only a useful clinical specialty classification tool for hospital managers, but also a basis for comparing the performance indicators of different service providers in the same specialty using objective data. Therefore, these DRG-based assessments of specialty medical service performance allow hospital managers to objectively understand their specialty's service performance, including their strengths and weaknesses, providing scientific and objective assistance and guidance for improving service quality.[2,25–27]
It is noteworthy to mention that complicated case-mix systems such as DRGs are based on good medical information systems and valid data.[28–30] In other words, the validity of applying DRGs as a tool for risk-adjustment and healthcare management is seriously dependent on the coding quality of the discharge data. Therefore, all countries have considered the importance of implementing DRG systems, in order to establish and maintain accurate and effective medical information systems.[31,32]
In Beijing, by drawing on experiences from abroad, large endeavors have been made to improve the quality of discharge case data before applying DRGs. In fact, these discharge case data have been standardized by the leadership of the Beijing Health Bureau in 2003. This involved numerous changes,[33] and the main changes are listed as follows. First, at the end of 2006, the Beijing Health Bureau carried out a program designed to standardize information in FPMRs and unify the coding of diagnoses and procedures. Furthermore, it published a new data coding system called the ICD-Beijing Clinical Modification (ICD-BJCM), which has a systematic ICD coding maintenance mechanism. Second, regular training and quality control have been performed. The staffs in charge of coding were trained on how to code diagnoses and operations using the new coding system. Not only were they provided with related guidelines and manuals, but also a supervision team that comprised of experts in medical information, ICD coding and hospital management, in order to periodically evaluate the quality of discharge data and oversee the effectuation of the new discharge data coding criterion.
The BJ-DRG system was developed in 2008 to make it easier and more feasible to evaluate medical service performance and provider payment reform. It was the first case-mix system developed for use in China. Through the efforts of the BJ-DRG Project Team and the constant adjustment of packet programs, the BJ-DRG system has shown good adaptability to the data context in Beijing. Under these circumstances, the central government of China encouraged local governments to apply BJ-DRGs in provider payment reform, as well as in medical service performance assessment, at the proper time.[34]
At present, there are 783 DRGs in the 2014 edition of the BJ-DRG grouping scheme, which covers all acute discharges within 60 days. According to the diagnosis of patients at hospitalization and the surgical operations they received during their hospital stay, each discharged case is classified into unique MDCs, as well as DRGs, using the BJ-DRGs system. There are 26 mutually exclusive MDCs in the system. If the discharged case cannot be accurately sorted into any MDC, it is marked as “ungrouped data” at the MDC level, and is not used or analyzed further. If the discharged case could be classified into only one MDC, an attempt is made to further assign it into one of the DRGs that belong to that MDC by drawing on more detailed information related to the discharged case. If a discharge case cannot be assigned to any DRG within the given MDC, it is labeled as “ungrouped data” at the DRG level, and is not used for further analysis. Note that coding errors or evident mistakes in diagnosis or treatment such as a male diagnosed with a female reproductive system disease, or an incorrectly recorded discharge time, can lead to failure in grouping. Studies have shown that the standardization of discharge data improves data quality and consequently enhances the performance of DRGs in Beijing.[35]
4.1. Analysis of the medical service capacity of the subspecialty in the research hospital
Results revealed that from 2008 to 2015, the number of discharges and the total weight of the subspecialty “major operation of digestive system diseases” of the research hospital increased annually, while the service capacity increased steadily. Notably, the number of cases of the subspecialty in the research hospital in 2015 accounted for 50.27% of cases in the 16 hospitals, thereby showing obvious service capacity advantages in the 16 hospitals compared with the research hospital. However, the CMI of the subspecialty in 2015 was 3.34, which was slightly lower than the overall CMI of the 16 hospitals (3.38). This is mainly because the case composition of the subspecialty in the GB11 and GB23 groups, which typically had higher weights, was lower than those in the 16 hospitals. Therefore, it would appear that the subspecialty of the hospital might take on more complex digestive disease cases, including GB11 and GB23, while simultaneously maintaining the advantages of the diagnosis and treatment of major diseases of the digestive system (especially in wards G and H), in order to enhance the technological level of the specialty, and meet the requirements of the health administration departments.
4.2. Efficiency of the medical services of the subspecialty of the research hospital
In present study, the time consumption index of the subspecialty of the research hospital was 0.91 in 2015, which was lower than that of the 16 hospitals. Furthermore, except for the GB11 group, the time consumption of the studied DRGs was lower than the average of the 16 hospitals. It should be noted that the time consumption indexes in the GB11 and GB25 groups in wards A and D and the GB15 group in ward H were significantly higher than in the 16 hospitals. This suggests that it would be valuable to carefully decompose and analyze the number of hospitalized days in these 3 wards, and compare these with similar departments. This would be useful in designing effective measures for reasonably controlling the number of hospitalized days, and further improve service efficiency.
Regarding the charge consumption index, the costs for the subspecialty of the research hospital were 24% higher than the average of the 16 hospitals. Except for ward B, the costs for DRGs in the other 5 wards were all higher than the average of the 16 hospitals. As such, the research hospital had a higher cost of treatment for similar diseases compared to other hospitals in the region. This was perhaps because the hospital often used minimally invasive surgery (as opposed to conventional open surgery) to reduce the pain of patients and accelerate their postoperative rehabilitation. In 2015, the overall ratio of minimally invasive surgery in the 4 DRGs in the research hospital was 33.57%, which was as high as 69.32% in ward D. However, minimally invasive surgeries consume more and rather expensive medical materials. Furthermore, since the hospital is a cancer hospital and most cases are cancer patients (accounting for 99.52% of the 4 DRGs in 2015), the costs for preoperative or postoperative examinations or drugs are typically higher than those for common digestive diseases. Therefore, the research hospital must attempt to maintain high-quality medical services, while strictly controlling the costs for carrying out new techniques. This would reduce medical costs for patients, especially those in wards A and B, which had more cases in the GB11 group, wards C and D, which had more cases in the GB23 and GB25 groups, and wards G and H, which had more cases in the GB15 group.
4.3. Medical service quality of the subspecialty in the research hospital
The mortality in the middle–low risk disease groups (GB15 and GB25) for the subspecialty in the research hospital and all 16 hospitals was zero in 2015. Conversely, the mortality in the middle–high risk groups (GB11 and GB23) was significantly lower in the research hospital than in the 16 hospitals. After reviewing these DRG grouping results, we noticed that only one death occurred in each of the GB11 and GB23 groups in 2015 in the research hospital, indicating that this subspecialty had exceedingly safe medical services in the research hospital. Since most cases received in the hospital are cancer patients who often have comorbidity chronic diseases such as hypertension, diabetes, and hyperlipidemia, it may be necessary to continue the strict implementation of preoperative assessment system requirements, a surgical classification system, and other relevant provisions of operative management for large surgical operations, in order to ensure the safety of patients.
5. Conclusions
Analyzing the medical service performance of the subspecialty “major operation of digestive system diseases,” including the evaluation of its advantages and disadvantages in service capacity, time consumption, cost consumption, and service quality, is of great significance for the research hospital to strengthen the construction of key specialties and improve service ability. In the present study, we tracked the medical service capacity development over 8 years at the research hospital, clarifying its difference from the 15 other municipal hospitals in the region in terms of service capacity, time and charge consumption, service quality, and various strengths and weaknesses in the services of the subspecialty. In doing so, hospital managers might find this study useful for drafting plans to improve the function of various subspecialties. Second, our study provides baseline data for the comparison of the same DRGs among the internal wards of the research hospital. Third, we clarified the composition of the 4 studied DRGs in relevant wards in the hospital, as well as the time and cost efficiency of these wards for these DRGs. Again, we expect this information to be useful for hospital managers in their efforts to strengthen the construction of hospital specialties. Taking the GB25 group as an example, discharges were mainly located in wards C and D. Consequently, in the analyses of relevant indicators of this DRG, we might mainly focus on wards C and D, and further take corresponding improvement measures. Overall, the analysis of the medical service performance of subspecialties is of great importance for fine hospital management and specialty construction.
There are several potential limitations in the present study. First, the research hospital is a cancer specialist hospital, while the other 15 hospitals are general hospitals. Therefore, it remains unclear whether the demographic and socioeconomic characteristics of the discharged cases are consistent. Such information may affect the patient's hospitalization expenses. Second, evaluating medical quality merely by using the mortality of the middle–low risk group and middle–high risk group may be insufficient, since various factors affect service quality. In the future, an in-depth analysis of these problems is required.
Acknowledgment
We are particularly grateful to all the people who have given us help on our article.
Author contributions
Conceptualization: Xinqiang Ji, Yun Fang, Jing Liu.
Data curation: Xinqiang Ji, Yun Fang, Jing Liu.
Formal analysis: Xinqiang Ji.
Methodology: Xinqiang Ji, Yun Fang.
Footnotes
Abbreviations: ADRGs = adjacent DRGs, ALOS = average length of stay, BJ-DRGs = Beijing-Diagnosis Related Groups, CMI = case-mix index, DRGs = diagnosis-related groups, FPMRs = front pages of medical records, ICD-BJCM = ICD-Beijing Clinical Modification, MDC = major disease category.
The authors have no conflicts of interest to disclose.
References
- [1].Luigi P, Sabina N, Chiara S, et al. What drives hospital performance? The impact of comparative outcome evaluation of patients admitted for hip fracture in two Italian regions. BMJ Qual Saf 2012;21:127–34. [DOI] [PubMed] [Google Scholar]
- [2].Fung CH, Lim YW, Mattke S, et al. Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med 2008;148:111–23. [DOI] [PubMed] [Google Scholar]
- [3].Roger France FH. Case mix use in 25 countries: a migration success but international comparisons failure. Int J Med Inform 2003;70:215–9. [DOI] [PubMed] [Google Scholar]
- [4].Iezzoni L. Risk Adjustment for Measuring Health Care Outcomes. 3rd ed.Chicago: Health Administration Press; 2003. [Google Scholar]
- [5].Grimaldi PL, Micheletti JA. Diagnosis Related Groups: A Practitioner's Guide. 3rd ed.Chicago: Pluribus Press; 1983. [Google Scholar]
- [6].Jian WY, Hu M, Zhang XM. DRGs-based methodology for medical performance evaluation and case studies. Chin J Hosp Admin (in Chinese) 2013;29:180–5. [Google Scholar]
- [7].Fetter RB, Freeman JL, Averill RF, et al. Case-mix definition by diagnosis related groups. Med Care 1980;18:1–53. [PubMed] [Google Scholar]
- [8].Mihrshahi S, Brand C, Ibrahim JE, et al. Validity of the indicator ’death in low-mortality diagnosis-related groups’ for measuring patient safety and healthcare quality in hospitals. Intern Med J 2010;40:250–7. [DOI] [PubMed] [Google Scholar]
- [9].Barker AL, Brand CA, Evans SM, et al. Death in low-mortality diagnosis-related groups”: frequency, and the impact of patient and hospital characteristics. Med J Aust 2011;195:89–94. [DOI] [PubMed] [Google Scholar]
- [10].Mistichelli J. Diagnosis related groups (DRGs) and the prospective payment system: forecasting social implications. [Accessed January 2, 2017]. Available at: https://repository.library.georgetown.edu/handle/10822/1033789. [Google Scholar]
- [11].International Quality Indicator Project. Acute care indicators. [Accessed January 4, 2017]. Available at: http://www.intemationalqip.com/indicators.aspx. [Google Scholar]
- [12].Kattcy E. Two decades of casemix. Department of Health and Aging. [Accessed January 9, 2017]. Available at: http://www.health.gov.au/internet/MAIN/publishing.nsf/Content. [Google Scholar]
- [13].Jian WY, Lu M, Zhang XM, et al. The grouping process and method of diagnosis related groups, Beijing version (BJ-DRGs). Chin J Hosp Admin (in Chinese) 2011;27:829–31. [Google Scholar]
- [14].Fu TH, Zhang LH, Guo MN, et al. Analysis and comparison of the rationality of grouping scheme of BJ-DRGs. Chin J Hosp Admin (in Chinese) 2013;31:828–30. [Google Scholar]
- [15].The State Council of the PRC. Implementation plan for deepening reform of the medical and health system in China in “thirteenth five-year period”. [Accessed January 2, 2017]. Available at: http://www.gov.cn/zhengce/content/2017–01/09/content_5158053.htm. [Google Scholar]
- [16].Guo MN, Chen F, Zhang LH, et al. Performance evaluation of DRGs-based inpatient medical secondary discipline. Chin J Hosp Admin (in Chinese) 2015;31:852–5. [Google Scholar]
- [17].Guo MN, Liu WR, Qiu YL, et al. Performance evaluation of DRGs-based inpatient medical service in Beijing in 2014: methods and application. Chin J Hosp Admin 2015;31:840–3. [Google Scholar]
- [18].Jian WY, Huang YM, Hu M, et al. Performance evaluation of inpatient service in Beijing: a horizontal comparison with risk adjustment based on Diagnosis Related Groups. BMC Health Serv Res 2009;9:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jian WY, Tang SN, Hu M. Empirical analysis of relationship between scales and outputs of inpatients services of public comprehensive hospitals in Beijing area. Beijing Da Xue Xue Bao (in Chinese) 2011;43:403–7. [PubMed] [Google Scholar]
- [20].Carolin F, Daniel O, Thomas R, et al. Hospital incidence and mortality rates of sepsis-an analysis of hospital episode (DRG) statistics in Germany from 2007 to 2013. Dtsch Arztebl Int 2016;113:159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lichtig LK. Hospital Information System for Case Mix Management. New York: John Wiley & Sons Press; 1986. [Google Scholar]
- [22].Che-Ming Y, William R. Feasibility and validity of international classification of disease based case mix indices. BMC Health Serv Res 2006;6:1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Jian WY, Cui T, Wang H, et al. Using diagnosis relative groups mortality risk classification to assess medical quality. Beijing Da Xue Xue Bao (in Chinese) 2007;39:145–8. [PubMed] [Google Scholar]
- [24].Andrew S, Conrad K, Thomas R, et al. How well do Diagnosis-Related Groups explain variations in cost or lengths of stay among patients and across hospitals? Methods for analyzing routine patient data. Health Econ 2012;21:6–18. [DOI] [PubMed] [Google Scholar]
- [25].Magali P, Caroline D, Lionel DP, et al. Variability of nursing care by APR-DRG and by severity of illness in a sample of nine Belgian hospitals. BMC Nursing 2013;12:26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].McKay NL, Deily M. Comparing high- and low-performing hospital using risk-adjusted excess mortality. Health Care Strateg Manage 2006;24:9–10. [DOI] [PubMed] [Google Scholar]
- [27].Barros PP. Random output and hospital performance. Health Care Manage Sci 2003;11:219–28. [DOI] [PubMed] [Google Scholar]
- [28].Averill RF. Evolution of DRGs and clinical information systems. Soz Praventivmed 1989;34:185–7. [DOI] [PubMed] [Google Scholar]
- [29].Simoes E, Freund JF, Grzeschiuchna CM, et al. Quality of statutory inpatient database before introducing DRGs. Gesundheitswesen 2002;64:521–6. [DOI] [PubMed] [Google Scholar]
- [30].Alexander G, Wilm Q, Reinhard B. Heterogeneity of European DRG systems and potentials for a common EuroDRG system. Int J Health Policy Manag 2015;4:319–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Martins M, Travassos C. Assessing the availability of case-mix information in hospital database systems in Rio de Janeiro. Brazil Int J Qual Health Care 1998;10:125–33. [DOI] [PubMed] [Google Scholar]
- [32].Tzavaras A, Spyropoulos B, Gruen R. Diagnosis Related Groups: approval and suitability for the Greek National Health System. [Accessed January 2, 2017]. Available at: http://medlab.cs.uoi.gr/itab2006/proceedings/eHealth/91.pdf. [Google Scholar]
- [33].Deng XH. The Systematic Research and Application Diagnosis Related Groups, Beijing Version (BJ-DRGs) (in Chinese). Beijing: Beijing Medical University Press; 2015. [Google Scholar]
- [34].National Health and Family Planning Commission of the PRC. Implementation plan for application diagnosis related groups (DRGs) on hospital evaluation. [Accessed January 2, 2017]. Available at: http://www.nhfpc.gov.cn/yzygj/s3586q/201108/c74f1ca5335d48fbb36b877863139ace.shtml. [Google Scholar]
- [35].Jian WY, Lu M, Han W, et al. Introducing diagnosis-related groups: is the information system ready? Int J Health Plann Manag 2016;31:E58–68. [DOI] [PubMed] [Google Scholar]


