Abstract
Background:
Perimenopausal insomnia (PI) is one of the most common complaints in women. Acupuncture is used to treat PI increasingly considering its less side effect. The subject of this study is to explore the effectiveness and safety of acupuncture for PI.
Methods:
All the randomized controlled trials(RCT) literatures of acupuncture for PI will be searched in the databases of MEDLINE, Cochrane Library, Web of Science, EMBASE, Springer, WHO International Clinical Trials Registry Platform (ICTRP), China National Knowledge Infrastructure (CNKI), Wan fang, Chinese Biomedical Literature Database (CBM), Chinese Scientific Journal Database (VIP), and other available resources using the subject terms of "acupuncture” and “perimenopausal insomnia” and their synonyms. The languages are limited as English and Chinese. Non-RCT literatures will be screened and relative information will be extracted. Sleep quality values is considered as the primary outcome. Secondary outcomes include biochemical indicators, such as hormone levels, side effects caused by acupuncture, total scores on the insomnia severity index and traditional Chinese medicine symptom changes.
Results:
This systematic review study will provide an evidence of acupuncture for PI.
Conclusion:
The study will give an explicit evidence to evaluate the effectiveness and side effects of acupuncture for PI.
PROSPERO registration number:
CRD42018092917.
Keywords: acupuncture, perimenopausal insomnia, protocol, systematic review
1. Introduction
1.1. Description of the condition
Perimenopause is deemed to a specific surrounding period of the final years of reproductive life, and it starts from the first menstrual irregularity and concludes after 1 year of amenorrhea.[1] Insomnia is a common syndrome in perimenopausal women. According to reports, the prevalence of sleep disorders in perimenopausal women is in connection with culture and ethnicity.[2] The prevalence is high in China, with 51% to 55%.[3,4] It is 40% in Caucasian,[5] 31% to 42% in America,[6] while 28% in Japanese and 15.9% in Korean.[7] Insomnia dose not only have an impact on mental health but also the morbidity and mortality of cardiometabolic and neurocognitive, and it increases health care expense.[6,8,9] Meanwhile, perimenopausal insomnia (PI) is often in a tangle with other coexistent medical conditions such as depression, hot flashes, fatigue, decreased/increased appetite or weight loss/gain, nocturia,[1,10,11] which may amplify harm in relation to common insomnia. The pathological mechanism is not explicit, and study shows lower estradiol and higher luteinizing hormone levels are significantly correlated with PI.[12,13] Also menopausal hormone replacement therapy is widespread used for PI.
In order to obtain high quality of life of menopausal women, adding to menopausal care programmes is necessary during reducing sleep condition.[14] Women suffering from PI also would like to remit their sleep difficulties through comprehensive counseling under the assessment of their body constitution rather than simply prescribing drugs for sleep difficulties.[15] So, it is better that interventions could relieve more symptoms not only insomnia.
1.2. Description of the intervention
Various interventions are shown positive effect to improve sleep disorder in menopause. Basing on a literature evaluation of 76 articles,[16] it suggested hormone therapy, isoflavones, escitalopram, gabapentin, eszopiclone, valerian, exercise, and hypnosis to treated insomnia in menopause, and zolpidem, citalopram, quiteiapine XL, mirtazapine followed by long-acting melatonin, ramelteon, Phyto-Female Complex, Pycnogenol, yoga, and massage also could be considered. Eszopiclone could improve insomnia and other symptoms like depressive and anxious, hot flashes in perimenopausal and postmenopausal women.[17] Escitalopram could reduce insomnia symptoms and improved subjective sleep quality in menopausal women with hot flashes.[18]
Besides, more and more patients are employing the nonpharmacological alternative therapies and traditional Chinese medicine (TCM), such as acupuncture,[19] Qigong,[20] and Guasha,[21] which have been used nearly 3000 years in China. Research shows acupuncture could decrease the Pittsburgh Sleep Quality Index (PSQI) and change the insomnia severity index (ISI), and polysomnography (PSG) exam show the sleep efficiency and total sleep time are improved significantly after acupuncture treatment.[19]
Acupuncture is a therapy that uses a sterile needle to penetrate a specific acupoint in body to treat specifc disease. There are 361 acupoints belonged to 14 main meridians. The acupuncture prescription is consisted of more than one acupoint that is selected based on the complicated TCM theory. The significant advantages of acupuncture are less side effect and significant effect.
1.3. How the intervention might work?
According to TCM cognition, PI is caused by the deficiency of liver and kidney, and the mind cannot be nourished adequately coupling with the attenuation of reproductive function. To treat PI, the acupoints that have the function of nourishing liver and kidney and calming the heart and tranquilizing the mind are always been selected. The mechanism of acupuncture for PI is not entirely clear. Research shows that acupuncture could regulate neurotransmitters in the brain like immune cytokines, antioxidant defense systems, hormones, and neuroelectrophysiology,[22] and which may be the reason of the improvement of sleep by acupuncture. Besides, acupuncture also could affect the estrogen receptor expression and then to adjust the estrogen level.[23]
1.4. Why it is important to conduct this review?
Although acupuncture is widely used to treat PI, and RCT has proved its effect,[19] it still lack of high quality evidence to convince more physician to adopted this treatment.[16,24] The evidence of system review is the highest level, and could give the effect and effectiveness and safety of one therapy for a disease. So, it is important to conduct this study.
1.5. Objectives
The aim of this systematic study is to evaluate the effectivity and safety of acupuncture on PI, which may provide evidence to clinician and researcher.
2. Methods
2.1. Study registration
PROSPERO systematical review protocol registration number is CRD42018092917. This protocol should be reported basing on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement guidelines.[25]
2.2. Inclusion criteria for study selection
2.2.1. Types of study
In order to estimate the effectiveness and safety of acupuncture on PI, all relevant RCTs will be retrieved and information will be evaluated. This review will include only RCTs about acupuncture on PI. Chinese and English are defined as language restrictions. Others like case reports, animal mechanism studies, non-RCTs, or RCT protocol will be excluded.
2.2.2. Types of participants
There is a restriction on perimenopausal woman. The insomnia may be related to menstrual disorders or unknown causes. The definitions of diagnostic criteria of PI with or without other menopause symptoms will be included.
2.2.3. Types of Intervention
The study focuses on clinical trials of PI with the therapy of acupuncture, and the results will give recommendations to physician. So, different types of acupuncture interventions including manual acupuncture, ear acupuncture, floating needle, electro-acupuncture, etc. will be covered. Both the comparision of acpuncture with other treatment methods and the comparision among different acupuncture methods will be included. Combining therapy which cannot judge the effect of acupuncture will be excluded.
2.2.4. Types of outcome measures
The primary outcome is sleep quality values. Secondary outcomes include biochemical indicators, such as hormone levels, side effects caused by acupuncture, total scores on the insomnia severity index, and traditional Chinese medicine symptom changes.
2.3. Data sources
The English databases incorporating MEDLINE, EBASE, Cochrane Library, Springer, WHO International Clinical Trials Registry Platform (ICTRP), as well as the Chinese databases like CNKI, Wanfang, CBM, and VIP will be searched normatively according to the rule of each database.
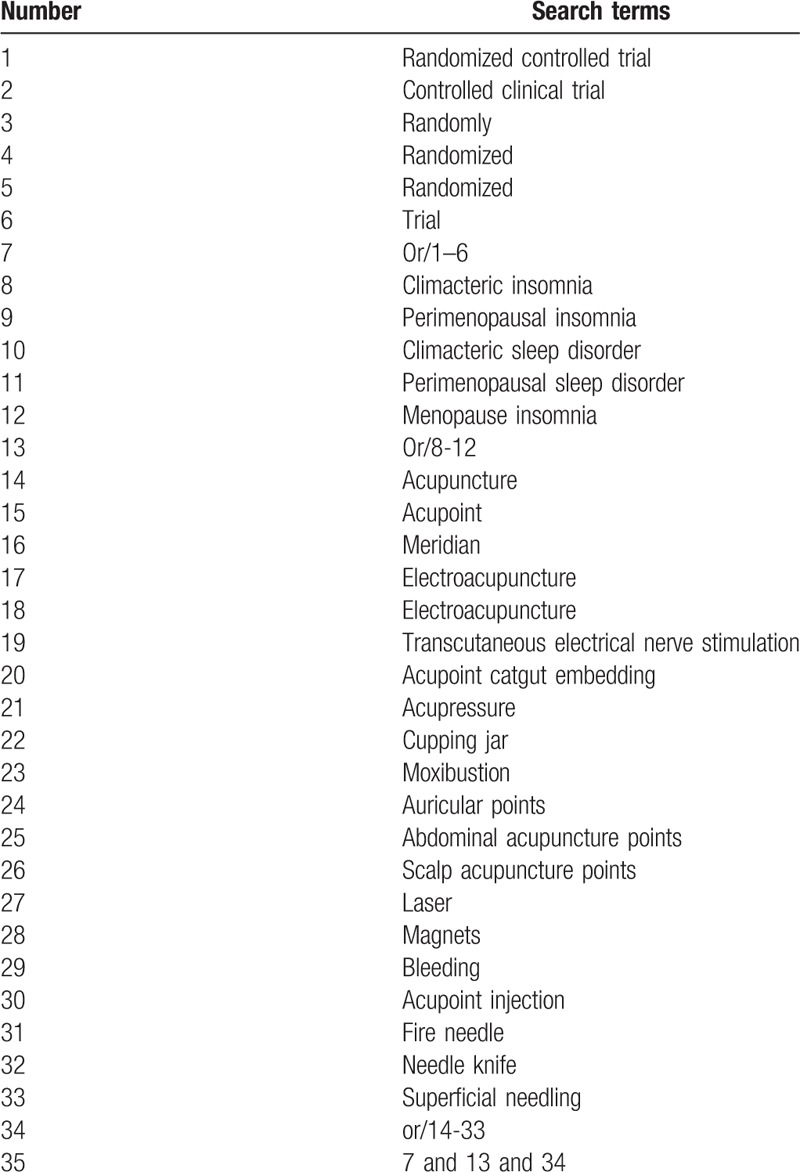
2.4. Search strategy
The following intervention subject term or combination of keyword as acupuncture (e.g., “acupuncture” or “TCM acupuncture” or “ “electroacupuncture” or “fire needling”) will be combined the disease subject term or combination of keyword as PI (e.g., “Climacteric insomnia” or “perimenopausal insomnia” or “Climacteric sleep disorder,” or “perimenopausal sleep disorder” The search strategies for Medline are listed in Table 1.
Table 1.
Medline search strategy.
2.5. Data collection and analysis
2.5.1. Selection of studies
Two researchers (MJ and YHJ) will independently perform as selection, data extraction, and quality assessment. All relevant articles of full text will be filtrated. When different opinions generate between the 2 reviewers and cannot agree on through consultations, the third reviewer (TPG) will make the final decision. The flow process of filtration is shown in a PRISMA flow chart (Fig. 1).
Figure 1.
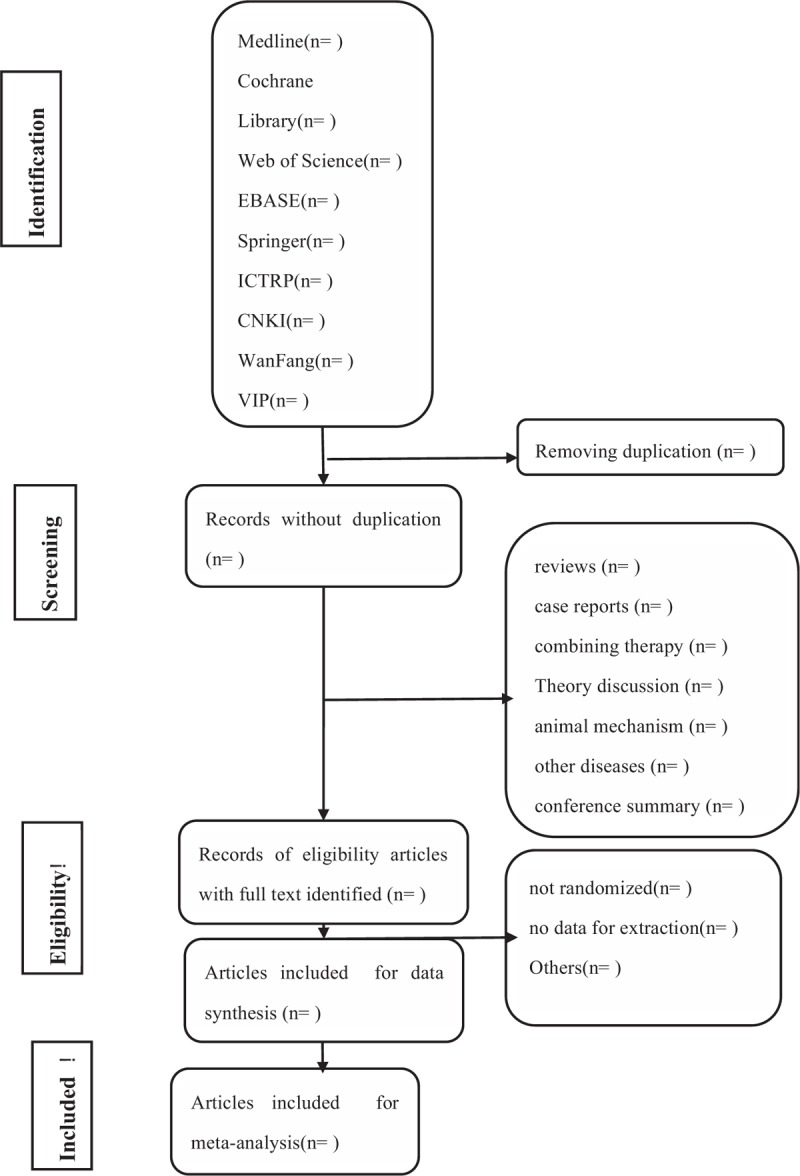
Flow diagram of studies identified.
2.5.2. Data extraction and management
The data such as study design, participant characteristics, interventions both acupuncture, and the control intervention, results will be extracted and recorded in an electronic text. The extraction will be completed independently by 2 reviewers (YHJ and NX) and the information will be recheck crossly. Divergence will be made by the third author (TPG) though discussion.
2.5.3. Assessment of risk of bias and reporting of study quality
To assess the risk of bias, we will adopt the Cochrane risk of bias tool and complete the STRICTA checklist. Meanwhile, the Jadad scale will be employed to estimate the methodological quality.
2.5.4. Measures of treatment effect
Mean differences (MDs) with 95% confidence intervals (95% CIs) will present as the continuous data. Also risk ratio (RR) will be the expression of dichotomous data.
2.5.5. Unit of analysis issues
According to the outcomes, sleep quality values will be pooled to together, and the secondary outcomes including biochemical indicators, total scores on the insomnia severity index, and traditional Chinese medicine symptom changes also be analysed, respectively.
2.5.6. Management of missing data
For missing or incomplete data, we will attempt to contact the original author. Deformity data will be gotten rid of if cannot be supplemented.
2.5.7. Assessment of heterogeneity
χ2 test will be applied to calculate the heterogeneity, and the presentation of heterogeneity degree is depended on the I2 value. According to the results, unimportance of heterogeneity may be explained when the value of I2 is 0% to 40%, and it exists moderate heterogeneity with the I2 is 30% and 60%. Meanwhile, it is presented as substantial heterogeneity if I2 is 0% to 0% and I2 is 75% to 100% means considerable heterogeneity. The fixed-effect model will be used if I2≤50% and I2>50% the random effects model will be chosen.
2.5.8. Assessment of reporting biases
Funnel plots will be used to evaluate the reporting biases when more than 10 trials are included. Its symmetry will account for the biases. There are no reporting biases if the funnel plots are symmetrical, and dissymmetry means it exist biases.
2.5.9. Data synthesis
Quantitative analysis will be implemented using RevMan version 5.3 with 95% CI. The mean change in each of the primary and secondary outcomes will be merged. Besides, if the data does not suit to quantitative analysis, the qualitative description will be employed.
2.5.10. Subgroup analysis
Subgroup analysis will be conducted according to the difference of acupuncture forms, participant conditions and controls.
2.5.11. Sensitivity analysis
We will perform a sensitivity analysis according to the heterogeneity and predefined criteria.
3. Discussion
Insomnia is gravely tormenting perimenopausal women and reducing the quality of life. Acupuncture is a nonpharmaceutical therapy that appeals to more and more patient although the action mechanism is not absolutely known, and it almost become a routine treatment replacing the supplement of estrogen in China.[23,26] Insufficient evidence is the restriction of worldwide application. Although the potential low quality of original RCT may influence the reliability of this systematic review, it is still meaningful to carry out this study. This systematic study will merge all the RCT about different kinds of acupuncture stimulation for insomnia in premenopausal women written in Chinese and English, which could provide the efficacy and safety.
Author contributions
Data curation: Tainpin Guo, Yuhao Jin, Na Xu.
Formal analysis: Man Jia.
Investigation: Na Xu.
Methodology: Tainpin Guo, Na Xu.
Resources: Yuhao Jin.
Software: Tainpin Guo, Man Jia, Na Xu.
Supervision: Tainpin Guo, Tianzhong Peng.
Validation: Tianzhong Peng.
Writing – original draft: Tainpin Guo.
Writing – review & editing: Tainpin Guo.
Footnotes
Abbreviations: CNKI = China National Knowledge Infrastructure, ICTRP = International Clinical Trials Registry Platform, MD = mean difference, NIH-CPSI = The National Institutes of Health Chronic Prostatitis Symptom Index, NRS = numerical rating scale, PI = perimenopausal insomnia, PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols, RCT = randomized controlled trial, RR = risk ratio, STRICTA = the Standards for Reporting Interventions in Controlled Trials of Acupuncture, TCM = traditional Chinese medicine, TCM = traditional Chinese medicine, WHO = World Health Organization.
TG and MJ are the first co-authors to this paper.
Ethics and dissemination: There is no requirement of ethical approval and it will be in print or disseminated by electronic copies.
Funding: This paper is funded by Yunnan Provincial Science and Technology Department, Applied Basic Research Joint Special Funds of Yunnan University of Traditional Chinese Medicine (NO.: 2017FF117-011).
The authors have no conflicts of interest to disclose.
References
- [1].Santoro N. Perimenopause: from research to practice. J Womens Health (Larchmt) 2016;25:332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Xu Q, Lang CP. Examining the relationship between subjective sleep disturbance and menopause: a systematic review and meta-analysis. Menopause 2014;21:1301–18. [DOI] [PubMed] [Google Scholar]
- [3].Li L, Wu J, Pu D, et al. Factors associated with the age of natural menopause and menopausal symptoms in Chinese women. Maturitas 2012;73:354–60. [DOI] [PubMed] [Google Scholar]
- [4].Zhang JP, Wang YQ, Yan MQ, et al. Menopausal symptoms and sleep quality during menopausal transition and postmenopause. Chin Med J (Engl) 2016;129:771–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].HM K, PAG JB, et al. Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition. Menopause 2003;10:19–28. [DOI] [PubMed] [Google Scholar]
- [6].Ciano C, King TS, Wright RR, et al. Longitudinal study of insomnia symptoms among women during perimenopause. J Obstet Gynecol Neonatal Nurs 2017;46:804–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Shin C, Lee S, Lee T, et al. Prevalence of insomnia and its relationship to menopausal status in middle-aged Korean women. Psychiatry Clin Neurosci 2005;59:395–402. [DOI] [PubMed] [Google Scholar]
- [8].Buysse DJ. Insomnia. JAMA 2013;309:706–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fernandez-Mendoza J, Vgontzas AN. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep 2013;15:418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Smith RL, Flaws JA, Mahoney MM. Factors associated with poor sleep during menopause: results from the Midlife Women's Health Study. Sleep Med 2018;45:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gopal M, Sammel MD, Pien G, et al. Investigating the associations between nocturia and sleep disorders in perimenopausal women. J Urol 2008;180:2063–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Murphy PJ, Campbell SS. Sex hormones, sleep, and core body temperature in older postmenopausal women. Sleep 2007;30:1788–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Joffe H, Petrillo LF, Koukopoulos A, et al. Increased estradiol and improved sleep, but not hot flashes, predict enhanced mood during the menopausal transition. J Clin Endocrinol Metab 2011;96:E1044–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Timur S, Sahin NH. Effects of sleep disturbance on the quality of life of Turkish menopausal women: a population-based study. Maturitas 2009;64:177–81. [DOI] [PubMed] [Google Scholar]
- [15].Hsu HC, Chen NH, Jou HJ, et al. Sleep disturbance experiences among perimenopausal women in Taiwan. J Clin Nurs 2009;18:2116–24. [DOI] [PubMed] [Google Scholar]
- [16].Attarian H, Hachul H, Guttuso T, et al. Treatment of chronic insomnia disorder in menopause: evaluation of literature. Menopause 2015;22:674–84. [DOI] [PubMed] [Google Scholar]
- [17].Joffe H, Petrillo L, Viguera A, et al. Eszopiclone improves insomnia and depressive and anxious symptoms in perimenopausal and postmenopausal women with hot flashes: a randomized, double-blinded, placebo-controlled crossover trial. Am J Obstet Gynecol 2010;202:e171. [DOI] [PubMed] [Google Scholar]
- [18].Ensrud KE, Joffe H, Guthrie KA, et al. Effect of escitalopram on insomnia symptoms and subjective sleep quality in healthy perimenopausal and postmenopausal women with hot flashes: a randomized controlled trial. Menopause 2012;19:848–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Fu C, Zhao N, Liu Z, et al. Acupuncture improves peri-menopausal insomnia: a randomized controlled trial. Sleep 2017;40:1–8. [DOI] [PubMed] [Google Scholar]
- [20].Yeh SC, Chang MY. The effect of Qigong on menopausal symptoms and quality of sleep for perimenopausal women: a preliminary observational study. J Altern Complement Med 2012;18:567–75. [DOI] [PubMed] [Google Scholar]
- [21].Meng F, Duan PB, Zhu J, et al. Effect of Guasha therapy on perimenopausal syndrome: a randomized controlled trial. Menopause 2017;24:299–307. [DOI] [PubMed] [Google Scholar]
- [22].Jianli W, Fan J, Yujie, et al. Review of the mechanism research of acupuncture for insomnia. Shanghai J Acupunct Moxibustion 2016;35:1379–81. [Google Scholar]
- [23].Chen X, Xintong Y, Zhen L, et al. Acupuncture treatment of insomnia in perimenopause. Liaoning J Tradit Chin Med 2014;41:2304–6. [Google Scholar]
- [24].Baumelou A, Liu B, Wang XY, et al. Perspectives in clinical research of acupuncture on menopausal symptoms. Chin J Integr Med 2011;17:893–7. [DOI] [PubMed] [Google Scholar]
- [25].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [26].Jingwen R, Yuzhen Y, Yingshuo Y, et al. Effect of acupuncture on sleeping pattern and qualities in chronic insomnia. Chin J Pathophysiol 2010;26:1616–20. [Google Scholar]


