Abstract
Rationale:
Immunoglobulin (Ig)G4-related pseudotumors of the liver are very rare diseases that are difficult to distinguish from malignant tumors. They can be usually improved by steroid therapy. Actinomycosis is a chronic, suppurative, granulomatous infection, for which immune suppression is a predisposing factor. It can also mimic malignant tumors.
Patient concerns:
A 67-year-old man presented with mild abdominal discomfort and a 5-kg weight loss for 3 months. Initially, he visited another hospital and was treated with antibiotics under the assumption of a liver abscess. Symptom was not resolved.
Diagnoses:
He diagnosed as having an IgG4-related pseudotumor of the right lobe of the liver after liver biopsy. Despite 2 months of steroid therapy, the liver mass was aggravated and invaded the right lung, as observed on follow-up computed tomography scan.
Interventions:
We performed en bloc resection of the tumor under the assumption that it was a malignant tumor.
Outcomes:
The pathology of the tumor was revealed as actinomycotic colonies and IgG4-positive plasma cells of the liver. He recovered well and was discharged with ursodeoxycholic acid tablet for 14 days. After 3 months, he underwent postoperative follow-up CT and there was no remarkable finding in remnant left hepatic lobe.
Lessons:
Hepatic actinomycosis and IgG4-related pseudotumors of the liver are both difficult to diagnose. As in our patient, combined diseases are more difficult to diagnose and to determine the optimal treatment. Since immunosuppression therapy of autoimmune diseases can cause and aggravate infection, management must be approached carefully. We can learn that various possibilities must be considered before diagnosing and treating a hepatic mass.
Keywords: actinomycosis, hepatic actinomycosis, IgG4-related liver disease
1. Introduction
Since IgG4-related disease was identified initially in 2003, it is well known that disease can be involved in various sites of the body, for example, the pancreas, biliary tree, liver, kidneys, salivary gland, breast, pericardium, skin, lungs, meninges, and pituitary gland.
IgG4-related diseases that involve the liver appear in the form of sclerosing cholangitis or an inflammatory pseudotumor. Histological confirmation and an accurate diagnosis are important to avoid unnecessary treatment, such as surgical resection, in patients with IgG4-related hepatopathy.[1–3]
Actinomycosis, primarily from Actinomyces, is a chronic, suppurative, granulomatous infection.[4–7] It can occur in various anatomical sites such as the face, bone and joint, gastrointestinal tract, urogenital tract, and central nerve system. Among them, hepatic actinomycosis is rare. It accounts for 15% of abdominal actinomycosis and 5% of all actinomycosis. Hepatic actinomycosis is easily misdiagnosed as a malignant tumor because it manifests nonspecific symptoms, and it is similar to a tumor radiologically.
IgG4-related hepatitis and hepatic actinomycosis are not easily distinguished from malignant tumors. Both diseases are rare and require different treatments. We describe a patient in whom IgG4-related hepatitis and liver actinomycosis were diagnosed simultaneously.
2. Case report
A 67-year-old man presented with mild abdominal discomfort and a 5-kg weight loss for 3 months. He was on medication because of diabetes mellitus for 4 years and hypertension for 6 years. Initially, he visited another hospital and was treated with antibiotics (type unknown) under the assumption of a liver abscess. However, as the symptom was not resolved, he was transferred to our hospital's Internal Medicine Department. Radiologic and hematological evaluations were performed to make a differential diagnosis. During the radiologic evaluation, the computed tomography (CT) scan showed an 8.5 × 7.8-cm ill-defined, suspicious, delayed enhancing lobulated mass in the right hepatic lobe. It seemed to be an inflammatory pseudotumor (Fig. 1). On the magnetic resonance imaging, a 9.3 × 8.3-cm ill-defined, suspicious, delayed enhancing lobulated mass was identified (Fig. 2). The positron emission tomography-CT scan on December, 2016 showed a lobulated mass about 6.8 cm with strong fluoro-2-deoxy-D-glucose uptake in segments 6 and 7 of the liver and small hypermetabolic nodes in the portocaval and aortocaval areas at the celiac axis level (Fig. 3). After the liver biopsy, we found that the mass was present with an abscess in the background of parenchymal fibrosis with increased IgG4-positive lymph plasma cells (about 30 IgG4-positive cells per high power field) (December, 2016) Thus, he received steroid therapy for 3 months according to the treatment guideline. When steroid therapy ended, he underwent follow-up CT. The CT scan showed that the liver mass was aggravated and increased in size from 8 × 6 cm to 9 × 7 cm, and it invaded the right lower lung. It had an unusual feature of sarcomatous transformation (Fig. 4). The patient was referred for operation, so we performed en bloc resection (lobectomy of the liver, wedge resection of the right lower lobe, excision of the diaphragmatic tumor, and lymph node dissection) (Fig. 5A and B). The final pathologic report showed dense lymphoplasmacytic infiltration with fibrosis and abscess formation, and actinomycotic colonies in hepatic and lung parenchyma. It also showed many IgG4-positive plasma cells (Fig. 6A and B). He recovered well and was discharged on May, 2017 with ursodeoxycholic acid tablet for 14 days. After 3 months, he underwent postoperative follow-up CT and there was no remarkable finding in remnant left hepatic lobe.
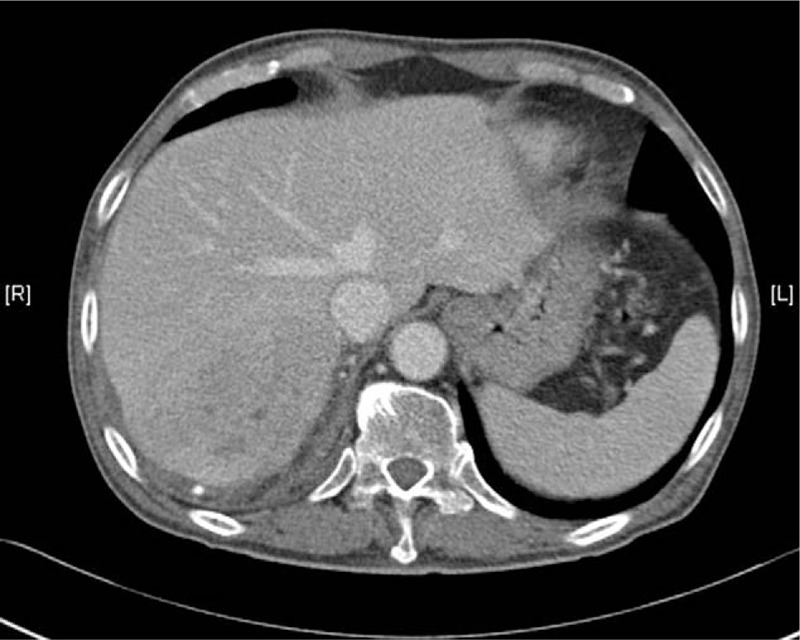
Figure 1.

Computed tomography scan showing an 8.5 × 7.8-cm ill-defined suspicious, delayed enhancing, lobulated mass-like lesion in the right hepatic lobe with hyperemic change of adjacent hepatic parenchyma and segmental portal vein obliteration. The first impression was an inflammatory condition such as an inflammatory pseudotumor.
Figure 2.

Magnetic resonance imaging scan (MRI) showing a 9.3 × 8.3-cm ill-defined suspicious, delayed enhancing, lobulated mass-like lesion in the right hepatic lobe. Lesions show hypo-signal intensities in T1 and hyper-signal intensities in T2. The diagnosis based on MRI scan findings was the same as that based on the computed tomography scan findings. MRI = magnetic resonance imaging.
Figure 3.

Positron emission tomography-computed tomography scan showing a 6.8-cm lobulated mass with strong fluoro-2-deoxy-D-glucose uptake in segments 6 and 7 of the liver.
Figure 4.
Compared to the previous computed tomography scan, the hepatic inflammatory pseudotumor in the posterior segment is aggravated (9 × 7 cm). It has an unusual feature of sarcomatous transformation.
Figure 5.

(A) Photograph showing the status of hilar dissection. (B) After performing right lobectomy of the liver, we repaired the diaphragm with a patch. The photograph shows the diaphragm after repair.
Figure 6.

(A) Liver gross picture, (B) Liver. (C) At a low magnification, sclerosing fibrosis destroying the liver parenchyma is seen (hematoxylin and eosin stain [HE], ×40). (D) At a low magnification, colonies of Actinomyces are seen (HE, ×40). (E) On medium power field, dense lymphoplasmacytic infiltration with fibrosis is shown (HE, × 100). (F) On high power field, dense lymphoplasmacytic infiltration with storiform fibrosis with patchy distribution is revealed (HE, ×200).
3. Discussion
We describe the first case of simultaneous IgG4-related hepatopathy and hepatic actinomycosis. IgG4-related disease is a systemic fibroinflammatory condition that affects multiple organs.[8] A histologic examination is essential for diagnosing IgG4-related disease. Diagnostic criterion for IgG4-related hepatopathy is the presence of more than 10 IgG4-positive plasma cells per high power field on liver biopsy or an IgG4:IgG ratio is >40%.[9] Generally, IgG4-related disease can be treated by steroid therapy. The recommended dose of prednisone is 30 to 40 mg daily for 4 weeks before reducing it by 5 mg every 2 weeks. Two-thirds of patients showed radiological or clinical improvement within 4 weeks after steroid therapy. Patients with relapse or slow resolution can be treated with second-line immunosuppressive therapy.[1,8] Surgical resection is only recommended in patients with an uncertain biopsy result, suspicious malignant lesion, combined other pathology, and lack of response to conservative management.
There have been a few reports of the relationship between IgG4-related disease and malignancy. Ahn et al[10] reported that the overall incidence of malignancy in patients with IgG4-related disease was 23 times higher than that in the general population. Wallace et al. reported that the prevalence of malignancy was 2.5 times higher than expected compared to the Surveillance, Epidemiology, and End Results database.[11] Among all reports, 2 studies reported that lymphoma was the most common type of malignancy after or before the diagnosis of IgG4-related disease.[11,12]
Etiologies of hepatic actinomycosis are thought to arise directly or hepatogenically through the portal vein. Previous abdominal operation, diabetes, oral disease, immunosuppression, and the use of an intrauterine device are well-known causes of hepatic actinomycosis. The clinical feature of hepatic actinomycosis is a nonspecific symptom, such as fever, weight loss, and sometimes abdominal pain. A single lesion with slow growing, low-density, mass-like nodular change is the most common feature during a radiologic evaluation. Hepatic actinomycosis mainly involves the right lobe. This clinical feature and radiologic finding mimics a malignant tumor. Pathologically, sulfur granule is a specific finding. It is comprised of small lobulated microcolonies around lymphocytes, plasma cells, epitheloid cells, and histiocytes of an abscess.[13] Cultured and confirmed Actinomyces is the most accurate way to make a diagnosis, but overgrowth of an associated microorganism, an inadequate incubation period, and media make sulfur granule an alternative diagnostic finding. The 16s ribosomal ribonucleic acid gene sequence analysis will become the precise method for making a diagnosis in the near future.[14]
Since many antibiotics are acceptable for treating actinomycosis, a surgical approach is not the first choice of treatment. Generally, the recommended treatment protocol for actinomycosis is about 10 to 20 million units of intravenous penicillin via injection and approximately 6 to 12 months of oral penicillin or amoxicillin.[7,13,15–17] There were 7 cases of published hepatic actinomycosis among Korean patients. Each patient had similar symptoms and was treated with antibiotics (Table 1).[4,5,13,18–21] Our patient received antibiotics at a previous hospital, but we cannot find any record about the kind of antibiotics administered.
Table 1.
Summary of all published papers about patients with hepatic actinomycosis from Korea.

The case of our patient with sarcomatous intrahepatic cholangiocarcinoma was presented at a hepatobiliary multidisciplinary conference. We discussed the possibility of many other diseases. Surgical resection was ultimately recommended because of rapid tumor growth and the invasive morphology. Postoperatively, the pathologist speculated that the actinomycosis of the lungs invaded the liver parenchyma directly with IgG4-related hepatopathy through the diaphragm. This made it difficult to treat and to follow to avoid a misdiagnosis.
In conclusion, IgG4-related hepatopathy and hepatic actinomycosis are difficult to diagnose during the initial evaluation. In our patient, determining proper treatment was more difficult because of the combined diseases. A multifaceted approach, such as from the pathological and microbiological aspects, is needed when determining the treatment method. Various possibilities must be considered before diagnosing and treating IgG4-related hepatopathy.
4. Patient perspective
He did not have any problem when he came to our outpatient clinic after discharge. He relieved symptoms like abdominal pain, discomfort.
Author contributions
Resources: Ji Sub Kim, Dong Ki Lee.
Supervision: Jin Hong Lim.
Writing – original draft: Joo Hyung Lee.
Writing – review & editing: Hyung Sun Kim, Jin Hong Lim.
Footnotes
Abbreviations: CT = computed tomography, Ig = immunoglobulin.
Informed Consent: This study was approved by the Institutional Review Board of Gangnam Severance Hospital, Yonsei University, Seoul, Korea (3-2017-0246). We explained and got an informed consent from patient for publishing case report.
The authors have no conflicts of interest to disclose.
References
- [1].Joshi D, Webster GJ. Biliary and hepatic involvement in IgG4-related disease. Aliment Pharmacol Ther 2014;40:1251–61. [DOI] [PubMed] [Google Scholar]
- [2].Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol 2003;38:982–4. [DOI] [PubMed] [Google Scholar]
- [3].Okazaki K, Uchida K, Koyabu M, et al. Recent advances in the concept and diagnosis of autoimmune pancreatitis and IgG4-related disease. J Gastroenterol 2011;46:277–88. [DOI] [PubMed] [Google Scholar]
- [4].Ha YJ, An JH, Shim JH, et al. A case of primary hepatic actinomycosis: an enigmatic inflammatory lesion of the liver. Clin Mol Hepatol 2015;21:80–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kong EJ. Primary hepatic actinomycosis mimicking hepatic malignancy with metastatic lymph Nodes by F-18 FDG PET/CT. Nucl Med Mol Imaging 2016;50:93–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sharma M, Briski LE, Khatib R. Hepatic actinomycosis: an overview of salient features and outcome of therapy. Scand J Infect Dis 2002;34:386–91. [DOI] [PubMed] [Google Scholar]
- [7].Yang XX, Lin JM, Xu KJ, et al. Hepatic actinomycosis: report of one case and analysis of 32 previously reported cases. World J Gastroenterol 2014;20:16372–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chen JH, Deshpande V. IgG4-related disease and the liver. Gastroenterol Clin North Am 2017;46:195–216. [DOI] [PubMed] [Google Scholar]
- [9].Culver EL, Chapman RW. IgG4-related hepatobiliary disease: an overview. Nat Rev Gastroenterol Hepatol 2016;13:601–12. [DOI] [PubMed] [Google Scholar]
- [10].Ahn SS, Song JJ, Park YB, et al. Malignancies in Korean patients with immunoglobulin G4-related disease. Int J Rheum Dis 2017;20:1028–35. [DOI] [PubMed] [Google Scholar]
- [11].Wallace ZS, Wallace CJ, Lu N, et al. Association of IgG4-related disease with history of malignancy. Arthritis Rheumatol 2016;68:2283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Della-Torre E, Lanzillotta M, Doglioni C. Immunology of IgG4-related disease. Clin Exp Immunol 2015;181:191–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Lee JD, Kim PG, Jo HJ, et al. A case of primary hepatic actinomycosis. J Korean Med Sci 1993;8:385–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hansen JM, Fjeldsoe-Nielsen H, Sulim S, et al. Actinomyces species: a Danish survey on human infections and microbiological characteristics. Open Microbiol J 2009;3:113–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Christodoulou N, Papadakis I, Velegrakis M. Actinomycotic liver abscess. Case report and review of the literature. Chir Ital 2004;56:141–6. [PubMed] [Google Scholar]
- [16].Kocabay G, Cagatay A, Eraksoy H, et al. A case of isolated hepatic actinomycosis causing right pulmonary empyema. Chin Med J (Engl) 2006;119:1133–5. [PubMed] [Google Scholar]
- [17].Lall T, Shehab TM, Valenstein P. Isolated hepatic actinomycosis: a case report. J Med Case Rep 2010;4:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chin SJ, Lee CK, Kim CW, et al. Actinomycosis of liver and greater omentum: a case report. Korean J Pathol 1979;13:303–8. [Google Scholar]
- [19].Jun Uh K, Hyo Jin P, Young Goo S, et al. Case Reports: A case of primary hepatic actinomycosis coinfected with a-streptococcus. Korean J Med 2002;63:596–600. [Google Scholar]
- [20].Ryu JC, Lim CY, Yang ES, et al. A case of primary hepatic actinomycosis. Korean J Gastroenterol 1992;24:388–93. [Google Scholar]
- [21].Sang Jun Park, Chang Goo Lee, Sang Eok Kim, et al. A case of liver abscess associated with duodenal perforation by a toothpick. Clin Endosc 2008;36:390–4. [Google Scholar]


