Abstract
Rationale:
Patients rarely display eye movement dysfunctions as the primary symptom in transient ischemic attack.
Patient concerns:
A 58-year-old patient with a history of hypertension and smoking presented with a 1-month history of paroxysmal exotropia of the left eye and double vision. No obvious abnormality was found in imaging examination and the patient ignored his symptoms. Eleven days later, the symptoms worsened and brain imaging provided an abnormal signal involving the left cerebellar hemisphere and the bilateral occipital lobe.
Diagnoses:
Based on the clinical manifestation and imaging findings, an acute cerebral infarction was diagnosed.
Interventions:
The patient was subjected to antiaggregation therapy.
Outcomes:
One week later, the symptom of paroxysmal exotropia of the left eye was no longer present.
Lessons:
Atypical symptoms of transient ischemic attack are easy to be overlooked. Early diagnosis and timely treatments are keys to reverse the neurological symptoms and can be highly beneficial for patients with this condition.
Keywords: midbrain, paroxysmal exotropia, transient ischemic attack
1. Introduction
Transient ischemic attack (TIA) is a medical emergency that represents a warning of an impending stroke with the probability of 1/3. Acute diagnosis of TIA depends on the presence of a transient neurological deficit caused by ischemic origin fitting a vascular territory, a normal examination, and no neuroimaging evidence of infarction.[1] The symptoms such as loss of muscle power, sensation, or vision are generally represented in cerebral ischemic episodes. However, manifestations of posterior circulation TIA are easily overlooked, and once the cerebral infarction has occurred, it represents a life-threatening emergency. In this report, we present a case of a patient initially presenting with paroxysmal external strabismus of the left eye that eventually developed into brain infarction, demonstrating the importance of recognizing the atypical symptoms of TIA.
2. Case report
A 58-year-old man presented with a 1-month history of paroxysmal exotropia in the left eye and double vision (Fig. 1). The symptoms lasted about 1 min, and the interval with normal performance was 4 or 5 days. Magnetic resonance imaging (MRI) showed no obvious abnormality. However, 11 days later, the episodes lasted more than 10 min and the frequency was increased. In addition, the patient had a headache and was unable to ride a bicycle. The patient had a history of hypertension and smoking. The neurological examination showed deficits of the right visual system and an unstable performance in the left finger-nose test, but revealed no further symptoms. Diffusion weighted imaging revealed a high signal involving the left cerebellar hemisphere and the bilateral occipital lobe (Fig. 2). Neck color Doppler ultrasound revealed low velocity and high resistance in the bilateral vertebral artery. Based on the clinical manifestation and MRI findings, acute cerebral infarction was diagnosed and the patient immediately received antiaggregation therapy. After 1 week, the paroxysmal exotropia of the left eye was no longer present.
Figure 1.

External strabismus of the left eye during the attack.
Figure 2.
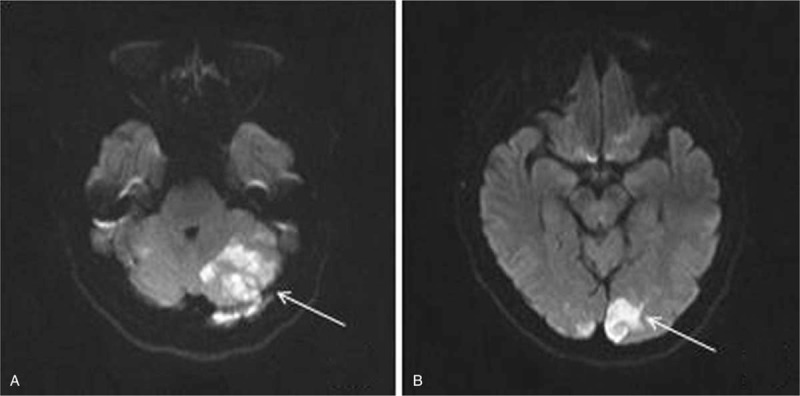
Diffusion weighted imaging showing a high signal involving the left cerebellar hemisphere and the bilateral occipital lobe.
The report was approved by the Research Ethics Board of the First Hospital of Jilin University and the patient approved of the study with an informed consent.
3. Discussion
TIA is a common neurological disease and often develops into cerebral infarction. Diagnosis of TIA is based largely on the patient's symptom recall and clinical judgment. This is particularly challenging for the diagnosis of posterior circulation TIA, which can give rise to diverse clinical manifestations. The most frequent symptoms are dizziness, unilateral limb weakness, dysarthria, headache, nausea or vomiting, gait ataxia, nystagmus, and eye movement dysfunction.[2] These symptoms are usually accompanied by each other during the episodes. Here, we report a case that presented with transient eye movement dysfunction as the only manifestation, which had never been observed before in TIA.
The midbrain has a complex anatomic configuration and is associated with eye movement. The nucleus of the oculomotor nerve is mainly located in the ventral border of the periaqueductal gray of the midbrain, and it comprises several subnuclei which are involved in controlling different ocular functions. Patients with midbrain infarction involving the subnuclei of the oculomotor nerve that presents as isolated medial rectus palsy have been reported before.[3,4] Interestingly, this patient initially presented with paroxysmal exotropia of the left eye as the only symptom, and neurological examination and MRI did not reveal any causes for the symptoms. With further progression of the disease, the later MRI revealed the infarction of the left cerebellar hemisphere and the bilateral occipital lobe. This observation stresses the need to recognize atypical manifestations of TIA in its early stage to provide timely treatment to reverse the neurological symptoms in patients.
Acknowledgments
The authors thank the patient for sharing his medical records and for the consent for publication of his case.
Author contributions
Investigation: Yang Yu.
Project administration: Wenxia Zhang.
Writing – original draft: Xue Wang.
Writing – review and editing: Hongmei Meng.
Footnotes
Abbreviations: MRI = magnetic resonance imaging, TIA = transient ischemic attack.
Departmental Sources
The authors have no conflicts of interest to disclose.
References
- [1].Siket MS, Edlow J. Transient ischemic attack: an evidence-based update. Emerg Med Pract 2013;15:1–26. [PubMed] [Google Scholar]
- [2].Markus HS, van der Worp HB, Rothwell PM. Posterior circulation ischaemic stroke and transient ischaemic attack: diagnosis, investigation, and secondary prevention. Lancet Neurol 2013;12:989–98. [DOI] [PubMed] [Google Scholar]
- [3].Rabadi MH, Beltmann MA. Midbrain infarction presenting isolated medial rectus nuclear palsy. Am J Med 2005;118:836–7. [DOI] [PubMed] [Google Scholar]
- [4].Al-Sofiani M, Lee Kwen P. Isolated medial rectus nuclear palsy as a rare presentation of midbrain infarction. Am J Case Rep 2015;16:715–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


