Abstract
Background and Objective:
The aim of this study was to compare the outcome of using tibial nails inserted by the suprapatellar approach with tibial nails inserted by the infrapatellar approach in a meta-analysis of randomized controlled trials (RCTs).
Methods:
The following electronic databases were searched: PubMed (1966 to January 2018), EMBASE (1974 to January 2018), Cochrane Library (January 2018), Web of Science (1990 to January 2018). We also used Google Search Engine to search more potentially eligible studies until January 2018. The methodological qualities of included studies were assessed in accordance with the guidelines provided by the Cochrane Collaboration for Systematic Reviews. The statistical analysis all of included studies were performed by STATA 13.0 software. The outcomes were total blood loss, postoperative pain, range of motion (ROM), Lysholm knee score, fluoroscopy time, operation time, and postoperative complications.
Results:
Four RCTs published between 2015 and 2017 were selected in the meta-analysis. There was a significant difference between suprapatellar and infrapatellar approach surgery in total blood loss, postoperative pain, ROM, Lysholm knee scores, and fluoroscopy times.
Conclusions:
The suprapatellar approach for intramedullary nailing appears superior to the infrapatellar approach, with a reduction in total blood loss, improved postoperative pain, shorter fluoroscopy time, and better knee functionality outcomes. There was no increased incidence of postoperative complications between the 2 groups. Further research remains necessary.
Keywords: approach randomized controlled trials, infrapatellar, meta-analysis, suprapatellar, tibia intramedullary nailing
1. Introduction
Tibial shaft fractures are a common traumatic injury with an annual incidence of approximately 75,000 in the United States,[1] comprising roughly 2% of all fractures in adults.[2,3] Traditional infrapatellar intramedullary nailing is a popular surgical procedure used in the treatment of tibial shaft fractures, as it is minimally invasive and allows for early functional rehabilitation.[4] However, this procedure may lead to proximal fracture fragment displacement with the knee in flexion, resulting in valgus and procurvatum.[5] Additionally, postoperative anterior knee pain is a common postoperative complication after intramedullary nail insertion with a reported incidence ranging from 10% to 80%.[6]
Recently, the suprapatellar approach has attracted the attention of orthopedists, as it seems to offer fewer complications and re-operations. It is an approach that is modified from the semiextended approach proposed in 2000.[7] It is shown to facilitate reduction in knee fractures in a semi-extended position, and the extended position of the lower leg allows for easier fluoroscopic imaging. Wang et al[8] reported that the suprapatellar approach is superior to the infrapatellar approach, as it may reduce blood loss and improve functional recovery. However, intra-articular injury might be a potential complication of this approach. There is no reliable evidence on the incidence of patellofemoral joint damage, limiting its clinical application.
Whether the suprapatellar approach provides a superior clinical outcome for tibial shaft fractures compared with the infrapatellar approach remains controversial. Until now, only a few clinical studies have compared the functional outcomes between the 2 approaches. However, the sample size has been small and follow-up intervals have been short. To our knowledge, no meta-analysis has been reported that compares the efficacy between the suprapatellar and infrapatellar approaches for intramedullary nailing of tibial shaft fractures. Therefore, we have conducted this meta-analysis of randomized controlled trials (RCTs) to determine whether the suprapatellar approach is associated with less postoperative pain and improved functional outcome compared with the infrapatellar approach.
2. Materials and methods
Ethical approval or patient consent was not required as the present study was a review of previously published articles.
2.1. Search methodology
The following electronic databases were searched: PubMed (1966 to January 2018), EMBASE (1974 to January 2018), Cochrane Library (January 2018), and Web of Science (1990 to January 2018). We also used Google Search Engine to search more potentially eligible studies until January 2018. The following key words were used for these databases: “tibia shaft fracture,” “intramedullary nail,” “infrapatellar,” and “suprapatellar.” We did not apply any language and geographical restrictions. References from retrieved articles were also assessed to extend the search strategy.
2.2. Inclusion criteria
The following criteria for the inclusion of studies were used: RCTs that compared the infrapatellar approach intramedullary nailing of tibial shaft fractures with a control group in whom the suprapatellar approach was applied; human studies; the outcomes of each RCT providing adequate information on total blood loss, postoperative pain score, knee functional outcome, fluoroscopy time, operation time, and postoperative complications. Moreover, prospective cohort studies and retrospective comparative studies were excluded. Two reviewers independently scanned titles and abstracts to search for potential studies, finally identifying eligible studies for inclusion based on further review of the full text. Disagreements were resolved by consensus after discussion or by consulting a third reviewer if necessary.
2.3. Assessment of methodological quality
The methodological qualities of the included studies were assessed independently by the two reviewers according to the guidelines provided by the Cochrane Collaboration for Systematic Reviews. This table comprises 7 items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other biases. The methodological quality of each RCT study was assessed as low (low risk of bias), high (high risk of bias), or unclear (unclear risk of bias). Disagreements were resolved by consensus after discussion, and if necessary, a third reviewer was consulted. The evidence grade was determined using guidelines from the GRADE (Grading of Recommendations, Assessment, Development, and Evaluation) working group.[9]
2.4. Data extraction
Data were independently extracted using a standard data form of the first author's name, year of publication, sample size, sex, age, intervention, country, study design, follow-up, and relevant outcomes. The primary outcomes in this meta-analysis included total blood loss, postoperative pain score and knee functional outcome. In addition, we also used fluoroscopy times, operation time, and postoperative complications as secondary outcomes for comparison between the 2 groups. Missing or insufficient information was obtained via e-mail communication with the original author. Any disagreement was resolved via consensus after discussion, and the third reviewer was consulted.
2.5. Data synthesis
The statistical analyses of all included studies were performed by STATA 13.0 software (Version: 5.3, the Cochrane Collaboration, UK). For continuous data, the mean difference and 95% confidence interval (CI) were calculated. For dichotomous data, the risk difference (RD) and 95% CI were calculated respectively. The χ2 test and I2 statistic was used to assess statistical heterogeneity. The fixed-effects model was chosen if the χ2 test >0.1 or the I2 <50%. Otherwise, the random-effects model was used.
3. Results
3.1. Search result
Figure 1 shows the process of including studies, in which 359 potentially relevant studies were screened. After scanning titles and abstracts, 349 studies were excluded for duplication, leaving 10 to be read in full. Of those 10, 6 studies were excluded, as they failed to meet certain inclusion criteria. As a result, 4 RCTs[10–13] published between 2016 and 2017 were selected for the meta-analysis. No gray literature was included.
Figure 1.
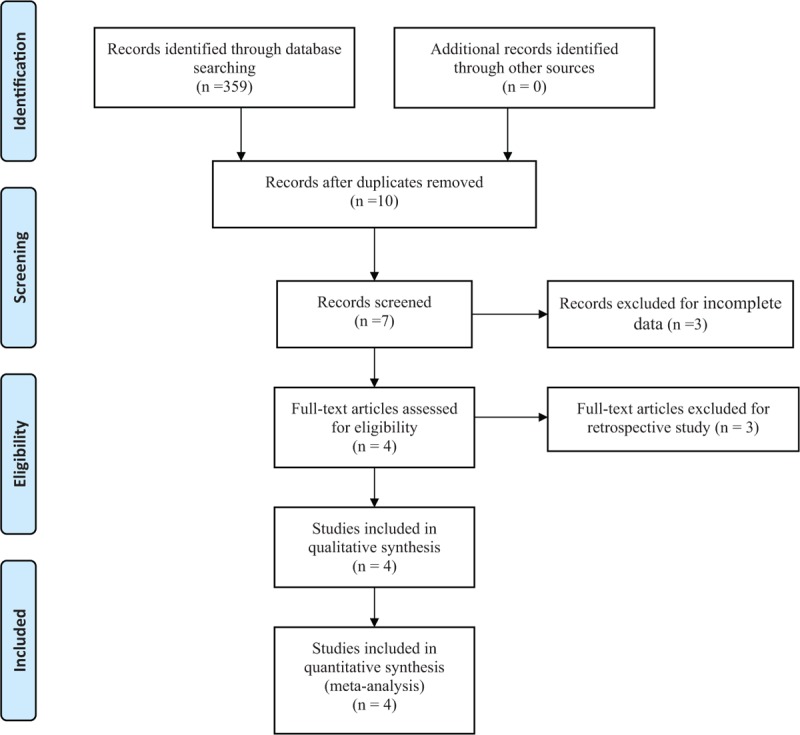
Flow chat shows article selection strategy.
3.2. Characteristics of included studies
All studies were RCTs that had been published in English with trials sample sizes ranging from 25 to 162, and the mean age of included patients ranged between 40 and 47 years. All RCTs offered complete outcome data and inclusion criteria. Experimental groups were treated using the infrapatellar approach for intramedullary nailing for tibal shaft fractures, and the control groups received the suprapatellar approach. Baseline characteristics of the included studies are shown in Table 1.
Table 1.
The basic information of included studies.

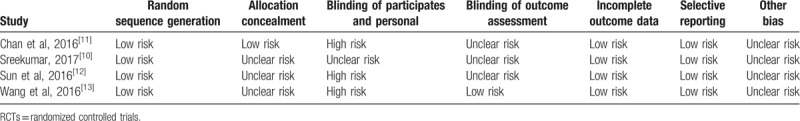
3.3. Risk of bias
Methodological quality assessment of the 4 included studies is presented in Table 2. Each RCT describes the random sequence generation procedure, but 3 studies do not describe allocation concealment. The blinding of participants and personnel was conducted with a high or unclear risk of bias. Only 1 study showed that the assessor was blinded. A low risk of bias due to incomplete outcome data and selective outcome reporting was detected.
Table 2.
Assessment of the risk of bias in the included RCTs.
3.4. Outcomes of meta-analysis
3.4.1. Total blood loss
Four studies reported total blood loss after operation. There was no significant heterogeneity among the studies (χ2 = 3.42, df = 3, I2 = 12.3%, P = .331) and a fixed-effects model was adopted. The pooled results of the studies showed that suprapatellar approach was associated with a significant reduction of total blood loss compared with infrapatellar approach (weighted mean difference [WMD] = 7.886, 95% CI: 1.129–14.642, P = .022; Fig. 2).
Figure 2.

Forest plot for total blood loss.
3.4.2. Postoperative pain score
A total of 4 RCTs reported the postoperative pain score after surgical procedure. Heterogeneity testing showed that there was low heterogeneity between the studies (χ2 = 5.10, df = 3, I2 = 41.2%, P = .164), so the fixed-effect model was used. The overall estimate showed that there was significant difference regarding the postoperative pain score between groups (WMD = 0.707, 95% CI: 0.558–0.847, P < .001; Fig. 3).
Figure 3.

Forest plot for postoperative pain score.
3.4.3. Lysholm knee score
Three RCTs showed Lysholm knee scors. There was no significant heterogeneity among the studies (χ2 = 0.90, df = 2, I2 = 0%, P = .638) and a fixed-effects model was adopted. The present meta-analysis revealed that there was significant difference between 2 groups in terms of Lysholm knee score (WMD = −3.212, 95% CI: −4.964 to −1.459, P < .001; Fig. 4).
Figure 4.

Forest plot for Lysholm knee scores.
3.4.4. Range of motion
A total of 3 studies reported the range of motion (ROM). Heterogeneity testing showed that there was low heterogeneity between the studies (χ2 = 1.91, df = 2, I2 = 0%, P = .385), so the fixed-effect model was used. The overall estimate showed that there was no significant difference regarding the ROM between groups (WMD = −1.284, 95% CI: −3.160 to 0.593, P = .180; Fig. 5).
Figure 5.
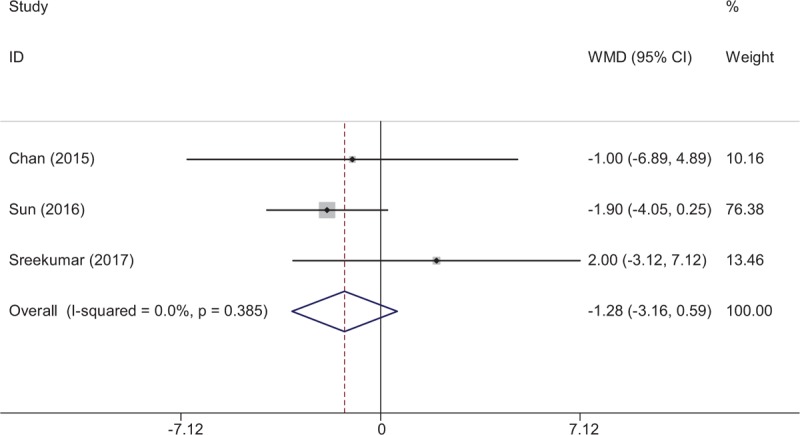
Forest plot for knee range of motion.
3.4.5. Fluoroscopy time
Fluoroscopy time after operation were reported in 2 RCTs, and pooled result indicated that there was significant difference between groups in terms of the fluoroscopy time (WMD = 17.949, 95% CI: 8.320–27.577, P < .001; Fig. 6).
Figure 6.
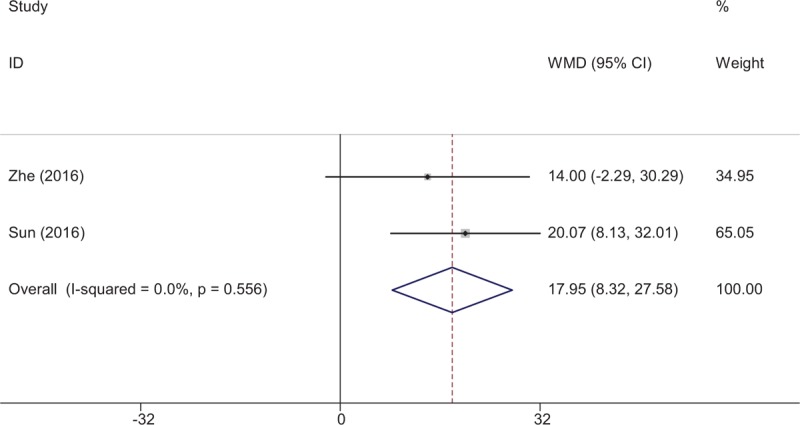
Forest plot for fluoroscopy times.
3.4.6. Operation time
Three studies reported the operation time. A fixed-effects model was used (χ2 = 1.17, df = 2, I2 = 0%, P = .577). There was no significant difference between the 2 groups in terms of operation time (WMD = −7.271, 95% CI: −22.332 to 7.791, P = .344; Fig. 7).
Figure 7.

Forest plot for operation time.
3.4.7. Postoperative complications
Three RCTs reported the postoperative complications. No significant difference was found between groups regarding the incidence of the postoperative complications (RD = 0.020, 95% CI: −0.059 to 0.098, P = .624; Fig. 8).
Figure 8.

Forest plot for postoperative complications.
3.4.8. Evidence level
Quality evidence for each result is evaluated by the GRADE system. The overall evidence is moderate, which indicated that further research is likely to significantly change confidence in the effect estimate but may change the estimate (Table 3).
Table 3.
Evidence level by GRADE.

4. Discussion
In our study, we compared the infrapatellar and suprapatellar approaches for nailing of tibial shaft fractures. This was the initial systematic review of RCTs to determine the optimal approach for tibial nail insertion. We demonstrate that the suprapatellar approach for intramedullary nailing is superior to the infrapatellar approach in terms of reduced total blood loss, postoperative pain, and improved knee functional outcome. No significant difference in operation time or incidence of postoperative complications was discovered. The quality of the evidence for each result was evaluated by the GRADE system and the overall evidence is moderate.
Tibial shaft fractures are common and comprise about 2% of all fractures in adults.[2,3] With the advantages of stable internal fixation and less damage to surrounding tissue, intramedullary nailing is considered the criterion standard for the treatment of tibial shaft fractures.[14] Some experts indicated that the infrapatellar approach to intramedullary nailing is associated with patellar tendon injury.[15] The suprapatellar approach involves an incision proximal to the patella, and the intramedullary nail passes through the trochlear groove. Theoretically, this approach could reduce the risk to both the patellar tendon and infrapatellar nerve damage, as well as decrease perioperative blood loss. Currently, there is no reliable evidence for the comparison of the 2 approaches; therefore, we performed this meta-analysis of RCTs. We found that the suprapatellar intramedullary nailing can significantly reduce total blood loss.
Postoperative pain is an important surgical outcome after orthopedic surgery. A majority of patients complained of moderate to severe pain, which may delay functional rehabilitation and increase opioid consumption. Although its etiology is unclear, this pain may be associated with injury of the knee structure and saphenous nerve.[16,17] Moreover, it is also caused by the surgical stress response, including inflammatory components. Whether the suprapatellar approach contributes to pain relief remains controversial. Leliveld et al[18] showed that an infrapatellar incision is more likely to cause chronic knee pain because of iatrogenic damage to the infrapatellar nerve after intramedullary nailing. Courtney et al[19] reported that the infrapatellar nerve is well protected when using the suprapatellar approach; however, they found no significant difference in knee pain scores between the suprapatellar and infrapatellar approaches for intramedullary nailing. Wang et al[8] demonstrateed that that the overall incidence of articular structure injury is lower when using the suprapatellar approach than it is with the infrapatellar approach, suggesting that suprapatellar nailing achieves a significantly improved pain score. Meta-analysis is used as the main statistical method in our study, enhancing its statistical power. The present meta-analysis indicates that the suprapatellar group is associated with a significant reduction in knee pain.
The Lysholm knee scale was first introduced in 1982[20] and contained eight measurements of the function and symptomatology of the knee. The Lysholm knee scoring scale has been used frequently in outcome studies of knee injuries, such as those related to patellofemoral pain. The present meta-analysis demonstrates that there is an improvement in Lysholm knee score in suprapatellar group when compared with infrapatellar group.
Tibial nail insertion for tibial shaft fractures may result in a reduction of the ROM of the affected knee joint.[21,22] Various factors may influence that reduced ROM, including damage to the vascularity and soft tissue. Lefaivre et al[23] showed that the knee ROM is equivalent to the unaffected side when using the infrapatellar approach. However, some authors hold the opposite view point. Chan et al[11] reported an improved range of motion with the suprapatellar approach; however, there was no significant difference. The present meta-analysis provides similar results. More RCTs are required. Fluoroscopy time is shown to be significantly shorter with the suprapatellar insertion compared with the infrapatellar insertion. The semiextended position may facilitate manipulation of the knee during the surgical procedure.[24] This position may simplify the reduction of the fracture and make it easier to maintain during nailing.
The limitations of this study were as follows: only 4 RCTs were included, the small sample size might lower the reliability of the conclusions; methodological weakness existed in all RCTs which may influence the results; the heterogeneity for included outcomes cannot be avoided because of objective differences existed among patients; short-term follow-up may cause underestimation of complications; publication bias is an inherent weakness that exists in all meta-analyses.
Despite the limitations above, this is the first meta-analysis from RCTs to determine the efficacy of suprapatellar versus infrapatellar approach for tibia intramedullary nailing. More quality RCTs with long-term follow-up are necessary.
5. Conclusion
The suprapatellar approach for intramedullary tibial nailing may be superior to the infrapatellar approach, with a reduction in total blood loss, reduced postoperative pain, shorter fluoroscopy time, and better knee functionality outcomes. There is no increased incidence of postoperative complications between the 2 groups. Further research remains necessary.
Author contributions
Haigang Jia designs the study. Zhixue Gao and Wei Han collects the data and finishes the manuscript. All authors read and approved the final manuscript.
Conceptualization: Haigang Jia.
Writing – original draft: Zhixue Gao, Wei Han.
Footnotes
Abbreviations: CI = confidence interval, RCT = randomized controlled trials, ROM = range of motion.
ZG and WH equally contributed to the article.
The authors report no conflicts of interests.
References
- [1].Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37:691–7. [DOI] [PubMed] [Google Scholar]
- [2].Weiss RJ, Montgomery SM, Ehlin A, et al. Decreasing incidence of tibial shaft fractures between 1998 and 2004: information based on 10,627 Swedish inpatients. Acta orthopaedica 2008;79:526–33. [DOI] [PubMed] [Google Scholar]
- [3].Larsen P, Lund H, Laessoe U, et al. Restrictions in quality of life after intramedullary nailing of tibial shaft fracture: a retrospective follow-up study of 223 cases. J Orthop Trauma 2014;28:507–12. [DOI] [PubMed] [Google Scholar]
- [4].Bode G, Strohm PC, Sudkamp NP, et al. Tibial shaft fractures–management and treatment options. A review of the current literature. Acta Chir Orthop Traumatole Cech 2012;79:499–505. [PubMed] [Google Scholar]
- [5].Bhandari M, Tornetta P, 3rd, Sprague S, et al. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma 2003;17:353–61. [DOI] [PubMed] [Google Scholar]
- [6].Toivanen JA, Vaisto O, Kannus P, et al. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nail-insertion techniques. J Bone Joint Surg Am 2002;84-A:580–5. [DOI] [PubMed] [Google Scholar]
- [7].Hernigou P, Cohen D. Proximal entry for intramedullary nailing of the tibia. The risk of unrecognised articular damage. J Bone Joint Surg Br 2000;82:33–41. [DOI] [PubMed] [Google Scholar]
- [8].Wang C, Chen E, Ye C, et al. Suprapatellar versus infrapatellar approach for tibia intramedullary nailing: a meta-analysis. Int J Surg 2018;51:133–9. [DOI] [PubMed] [Google Scholar]
- [9].Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. Bmj 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sreekumar K. Suprapatellar versus infrapatellar tibial nail insertion: a prospective, randomised control pilot study. J Evid Based Med Healthcare 2017;9:401–9. [DOI] [PubMed] [Google Scholar]
- [11].Chan DS, Serrano-Riera R, Griffing R, et al. Suprapatellar versus infrapatellar tibial nail insertion: a prospective randomized control pilot study. J Orthop Trauma 2016;30:130–4. [DOI] [PubMed] [Google Scholar]
- [12].Sun Q, Nie X, Gong J, et al. The outcome comparison of the suprapatellar approach and infrapatellar approach for tibia intramedullary nailing. Int Orthop 2016;40:2611–7. [DOI] [PubMed] [Google Scholar]
- [13].Wang Z, Li S, Wang X, et al. Supra-patellar versus infra-patellar intramedullary nailing in treatment of tibial shaft fractures. Chin J Orthop Trauma 2016;18:283–9. [Google Scholar]
- [14].Labronici PJ, Santos Pires RE, Franco JS, et al. Recommendations for avoiding knee pain after intramedullary nailing of tibial shaft fractures. Patient Saf Surg 2011;5:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Morandi M, Banka T, Gaiarsa GP, et al. Intramedullary nailing of tibial fractures: review of surgical techniques and description of a percutaneous lateral suprapatellar approach. Orthopedics 2010;33:172–9. [DOI] [PubMed] [Google Scholar]
- [16].Katsoulis E, Court-Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br 2006;88:576–80. [DOI] [PubMed] [Google Scholar]
- [17].Court-Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary tibial nailing: its incidence, etiology, and outcome. J Orthop Trauma 1997;11:103–5. [DOI] [PubMed] [Google Scholar]
- [18].Leliveld MS, Verhofstad MH. Injury to the infrapatellar branch of the saphenous nerve, a possible cause for anterior knee pain after tibial nailing? Injury 2012;43:779–83. [DOI] [PubMed] [Google Scholar]
- [19].Courtney PM, Boniello A, Donegan D, et al. Functional knee outcomes in infrapatellar and suprapatellar tibial nailing: does approach matter? Am J Orthop 2015;44:E513–516. [PubMed] [Google Scholar]
- [20].Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982;10:150–4. [DOI] [PubMed] [Google Scholar]
- [21].Duan X, Al-Qwbani M, Zeng Y, et al. Intramedullary nailing for tibial shaft fractures in adults. Cochrane Database Syst Rev 2012;1:CD008241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wood GW., 2nd Intramedullary nailing of femoral and tibial shaft fractures. J Orthop Sci 2006;11:657–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lefaivre KA, Guy P, Chan H, et al. Long-term follow-up of tibial shaft fractures treated with intramedullary nailing. J Orthop Trauma 2008;22:525–9. [DOI] [PubMed] [Google Scholar]
- [24].Cole JD. Distal tibia fracture: opinion: intramedullary nailing. J Orthop Trauma 2006;20:73–4. [DOI] [PubMed] [Google Scholar]


