Abstract
PURPOSE
Maintenance of lifestyle changes after cardiac rehabilitation (CR) is suboptimal. In addition, partners of cardiac patients are invited to participate in CR educational sessions and implicitly expected to assist patients with their lifestyle changes. The purpose of this study was to qualitatively examine patients’ and partners’ perceptions of Phase II CR three months after completion of the program.
METHODS
A purposive sample of 11 couples (post-heart surgery patients and spouses) was interviewed following completion of CR. Semi-structured, in-person interviews were conducted with patients and spouses separately. Data were analyzed using line-by-line coding to identify themes.
RESULTS
Themes were identified in relation to program elements of CR. Exercise themes were (1) benefitted from exercise and (2) felt held back. Education themes were (1) received basic education and (2) needed more personalized information. CR environment themes were: (1) developed confidence; (2) made social comparisons; and (3) helped to have partner there.
CONCLUSION
Overall, participants’ perceptions of exercise, education, and the CR environment were very positive. Nevertheless, there is a need to improve educational efforts within CR to rely less on “canned” presentations and more on participants developing their own self-management methods to maintain a healthy lifestyle after CR.
Keywords: cardiac rehabilitation, exercise, healthy eating, qualitative
Cardiac rehabilitation (CR) participants often report the need for assistance to make behavior changes during CR.1,2 One way to assist participants is through educational sessions focused on heart-healthy eating, exercise, smoking cessation, knowledge of risk factors, and so forth. Most CR programs provide systematic group education. Because education is typically paired with an exercise session, they often deliver the most amount of information in a short time frame (“passive” strategies). In a Cochrane review, Forster et al3 found that interventions that used active strategies (ie, hands-on training, group discussion and workbooks) were more effective than passive strategies (information leaflet, multimedia computer program) in getting patients to continue with initial positive changes in CR.
The experience of CR impacts not only the patient but also the primary caregiver. In CR, it is often assumed that the caregiver will be involved in the patient’s rehabilitation efforts and is invited to educational classes yet, receives minimal support for these efforts. Assessing patient and partner perceptions of educational sessions may provide insight into their experiences in the program and the challenges of applying the information in their everyday lives. Thus, the purpose of this qualitative study was to describe perceptions of participants (patients and partners) of phase 2 CR 3 mo after completion of the program; what they liked best and least about CR, what helped and did not help, and what things could be changed about CR.
METHODS
A qualitative descriptive design5 was used to examine participant perceptions of their CR experiences. This qualitative study was embedded within a larger randomized controlled trial in which partners in the experimental group participated in CR with patients and were asked to make the same physical activity and healthy eating changes as patients.4 The hypothesis tested was that if the couple can develop new physical activity and healthy eating habits together in CR, they can motivate and support each another to engage in these behaviors and adhere long-term.
Sample
A purposive subsample5 of 11 couples (patient and partner) was obtained from the sample of couples (n = 34) that participated in the larger clinical trial.4 All patients had undergone coronary artery bypass graft (CABG) surgery at either an academic medical center or a community hospital in the Midwestern United States. Patients and partners were low to moderate risk for adverse events during exercise. A maximal variation strategy5 was used to recruit the subsample to achieve variation in gender, CR program, ethnicity (Hispanic and non-Hispanic), and role (patients and partners as both husbands and wives).
All patients and partners participated in CR at 1 of 2 clinical sites. Both programs were nationally certified by the American Association of Cardiovascular and Pulmonary Rehabilitation (http://www.aacvpr.org/Program-Certification). At both sites, individualized counseling and education were provided by a multidisciplinary team of healthcare providers. Individualized exercise plans were implemented that included aerobic, strength, and flexibility exercises, 3 d/wk for 6–12 wk. Group classes in nutrition, exercise, smoking cessation, heart disease knowledge, risk factors, stress management, and medications were offered on a regular cycle.
Procedures
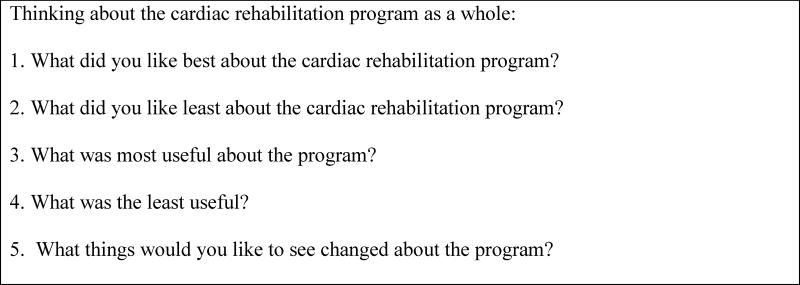
A single investigator conducted in-person interviews with patients and partners separately, in their homes, within 3 mo of completing CR. A semi-structured interview used a priori questions (Figure) and probing6 to identify perceptions of CR. Interviews lasted 30–60 min with each participant. The study was approved by the IRB at both the university and clinical sites where the study was conducted.
Figure.
Semi-structured interview guide used in this qualitative study.
Data Analysis
Interviews were audiotaped and transcribed verbatim. The method for data analysis was a content analysis consisting of line-by-line coding of transcripts and grouping codes into larger categories.6 Transcripts were reviewed by 3 investigators. Each segment of text was coded with a word or short phrase. Initially, text segments were coded in relation to the interview question asked. The next step was to organize the related codes into major themes according to the main programming elements of CR; exercise, education, and environment. Once major themes were generated, definitions of themes were developed and refined to better reflect their meaning. Coding decisions were based on 100% agreement between the 3 coders; disagreement was resolved through discussion.
RESULTS
Eleven couples participated in the study. Couples either were male patients and female partners (n = 9) or female patients and male partners (n = 2). The mean age of the patients was 64.3 ± 3.3 (range 60–70) y; the partner’s age was 62.5 ± 6.0 (range 51–71) y. All participants were married, well educated, and Caucasian except for 1 Hispanic male patient. A summary of the themes that emerged in each area (exercise, education, and environment) along with their definitions, and exemplar quotes are in the Table.
Table.
Summary of the Themes and Definitions based on Main Elements of Cardiac Rehabilitation (CR): Exercise, Education, and Environment
| CR Element | Themes | Definitions of Themes | Exemplar quotes |
|---|---|---|---|
| Exercise | Benefitted from exercise | Started or restarted a regular exercise routine that subsequently improved health. | Patient: “What I liked best [about CR] was the discipline of exercise. I was visibly able to see changes and progress. It got me in better shape. It turned me on to exercise and taught me the importance of regular exercise.” |
| Felt held back | The perceived lack of input or choice about exercise intensity and equipment. | Patient: “The staff didn’t always respond to my requests to change equipment or increase my exercise pace as quickly as I would like. For individuals who come in clueless or scared, they need motivation. But for those who come in motivated, they want to work harder. They want to get more out of CR. Exercise was too easy.” | |
| Education | Received basic education | Educational classes provided basic fundamental content useful for a healthy lifestyle. | Partner: “Of all the education, the thing I was the least aware of was diet and reading labels. You look at a label and there are 12 things on the list--what’s important? They worked with me outside the diet classes because apparently people in the class knew a lot more than I did. For [the patient] losing weight wasn’t really the issue; but for me it was, so how do you balance everything? I got a lot of education there.” |
| Needed more personalized information | Needed more specific and individualized information, particularly in the area of nutrition. | Patient: “Your average cardiac patient could take more technical information. Don’t just say avoid these [foods], tell them why. The basics were good, but a little more detail would be helpful. It was not personal at all. I already knew what my diet should be so maybe they could help me in weaning off of [foods I shouldn’t eat]. Obviously everyone knows to eat more fruits and vegetables [and if the presenter] is hell bent over eating vegetables then they haven’t done any good. Telling people how you can substitute, like a banana for cooking oil. More of that sort of thing is helpful.” | |
| Environment | Developed confidence | Helpful staff assisted participants in increasing their confidence to resume exercise and how much to engage in. | Patient: “If you’re going to fall they catch you. From the time I started to the time I stopped was such a big difference; my confidence level went way up.” |
| Made social comparisons | Upward and downward comparisons with those around them as a way to judge their exercise performance and progress. | Patient: “There was one lady near me who had surgery before me. She never pushed herself; she always did the least amount she could get away with.” Partner: “[The exercise] wouldn’t be hard for me and so I would say I want to go faster. It is my personality to drive myself, whereas other people didn’t drive themselves as much.” | |
| Helped to have partner there | A partnership program that involved patient and partner in which both made the same lifestyle (exercise and diet) changes, thus, allowing them to better understand each other’s experiences and provide support to one another. | Partner: “I think it made it easier for me to understand what he was going through and when I would say something, he would know that there was a basis behind it.” Patient: “We were both there and you take away different things, two sets of ears, so having her there really helped me. She knows what’s best for me and helps me accomplish it. Without her involvement, I would go back to my old ways.” |
Exercise
Two themes emerged about exercise: (1) benefitted from exercise, and (2) felt held back. Many participants stated that exercise was the best part of CR and linked the exercise to subsequent tangible improvements in their health and well-being. They also stated that it was the easiest change to make because of the consistent schedule, guidance of staff members, and easy access to exercise equipment. The second theme, felt held back, was perceived as the lack of input or choice about exercise intensity and equipment. This lack of input made them feel like they were not getting everything out of the CR exercise sessions that they could have.
Education
Two themes emerged about education: (1) received basic education and (2) need for more personalized information. Overall, comments about education were positive and mainly focused on dietary information. Participants indicated that making dietary changes was the most difficult lifestyle change for them. Participants also identified the need for more personalized information and wanted more details about how to incorporate healthy eating into their everyday lifestyle.
Environment
Three themes emerged about the environment: (1) developed confidence, (2) made social comparisons, and (3) it helped to have a partner present. The first theme was centered on helpful staff who assisted participants in increasing confidence to resume exercise and how much to do. The monitoring and reassurance by the staff that the activity was safe and was not going to result in heart damage contributed to this confidence. None of the partners voiced this same feeling as they were already confident in their exercise abilities.
The next theme involved social comparisons. This involved participants making upward and downward comparisons with those around them to judge their exercise performance and progress. These comparisons were made primarily about exercise because this was the main behavior that participants observed others doing. In multiple instances, participants commented that their exercise workload was more or less strenuous compared to others. These comparisons allowed the participants to adjust their views of how they were performing and facilitated adherence.
The third and final theme focused on a partnership program where both the patient and partner were asked to make the same exercise and diet changes; thus, allowing them to better understand and provide support to one another. It also provided the partners with an opportunity to improve their own cardiovascular health.
DISCUSSION
Participants overwhelmingly reported positive perceptions of CR. Restarting a regular exercise routine was a key feature they benefitted from similar to an earlier study.7 Tangible improvement in their health (improved serum lipids and functioning) was attributed to exercise habits that CR helped them establish. The findings highlight the need for healthcare providers to call attention to improvements in clinical values which will reinforce and motivate participants to continue their exercise program after CR.
In contrast, the exercise protocol was also perceived as limiting at times. The lack of input by participants about exercise intensity and equipment contributed to a feeling of being held back in their exercise performance. Often times CABG patients are restricted from using various equipment especially involving arm work (ie, Airdyne [Schwinn], lifting weights) until the chest incision heals. However, it was not just patients who experienced “being held back” but it was also healthy partners. There may be a conservative approach to exercise in CR programs which limits exercise levels for participants.
Overall, education was highly valued in CR and well attended by both patients and partners. The educational content was viewed as essential but basic. It was interesting that the vast majority of comments expressed about the educational sessions were related to eating behavior; both the difficulties of making changes and the need for more individualized information. It is unlikely that “one size fits all” participant learning is the best approach; yet this is often how information is delivered.3 Perhaps a better role for CR staff is not the “sage on the stage” but rather the “guide on the side.” Participants could be assigned homework about lifestyle changes and discuss adherence difficulties with other patients rather than observe a slide presentation. Often patients are in a better position to encourage and motivate other participants to make lifestyle changes because they are living proof of successful change.8 In addition, CR participants need an opportunity to discuss their stories, what did and did not work, and challenge others who are skeptical of making lifestyle changes.
Individualized nutrition information (eg, sample menus, recipes, and lists of healthy snacks, desserts, and food substitutions) was requested for daily use. Participants also wanted rationales for requested changes, were concerned about costs of new food items, did not like redundancies between classes, and preferred to have presenters in the room with them during the presentation. If the participant understands the rationale for changes and receives the skills and tools to make them, long-term adherence may be higher.
The CR environment was perceived by participants as confidence building which was found in prior studies.9–11 Similarly, making social comparisons was effective in a prior study.12 Stroke patients made social comparisons with other stroke patients who had slower recoveries than themselves which increased their wellbeing.12 Participants in this study who made downward comparisons were eager to engage in more activity than to the person they were comparing themselves. Participants new to CR made upward comparisons with participants about to graduate from the program which provided them with a vision of what they would attain in a few weeks. Some patients simply did not push themselves and settled for the minimum. Perhaps 1 way to get “minimizers” to work harder is to have other patients be their exercise buddy. The importance of comparisons is often underestimated by CR staff and could be harnessed to model appropriate exercise, eating, and other behaviors.
One of the unique contributions of this study was the significance that patients and partners placed on being able to participate in CR together. There are few partner programs available in CR that allow partners to exercise with patients. Most of the existing couple-oriented interventions involve spouses helping to improve patient adherence or in illness management13 with limited opportunity for partner health promotion. When spouses participated in CR with their partners in the larger study, they were able to significantly reduce their cardiovascular risk.14
Study limitations included the small sample size and the homogenous sample of primarily Caucasian, married, well-educated males. Although it was representative of the larger sample for this pilot study, women and minorities may have unique issues and barriers to adherence that were not captured in this study. Future research examining perceptions of CR from varied populations (women, minorities, same-sex couples) is needed.
In summary, participants reported benefitting from the CR exercise sessions and environment. However, they desired more personalized information from educational sessions. Programmatic changes in CR are needed to engage participants in educational efforts. A variety of active learning strategies could be used such as cooking demonstrations, hands-on training in self-monitoring methods (eg, MyFitnessPal), and workbooks that require application of learning. Participants who are near completion of the program could serve as role models for discussion groups to motivate and coach other patients. Nutrition information could be provided such as sample menus, recipes, and lists of healthy snacks, desserts, and food substitutions. Mosca et al15 described the early time post-cardiac event as a “motivational moment” for including the family in risk factor education. Future research is needed to test these alternate strategies to determine if they improve adoption and adherence to healthy lifestyle changes.
Acknowledgments
Funding for this study was provided by grant NR010923, National Institutes of Nursing Research, National Institutes of Health, and by the Research Support Fund, Clinical Research Center, University of Nebraska Medical Center awarded to Dr. Yates.
Footnotes
Conflict of interest: All authors declare no conflicts of interest.
All authors have read and approved the manuscript.
References
- 1.Pinto BM, Goldstein MG, Papandonatos GD, et al. Maintenance of exercise after phase II cardiac rehabilitation: a randomized controlled trial. Am J Prev Med. 2011;41(3):274–283. doi: 10.1016/j.amepre.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scotto CJ, Waechter DJ, Rosneck J. Adherence to prescribed exercise and diet regimens two months post-cardiac rehabilitation. Can J Cardiovasc Nurs. 2011;21(4):11–17. [PubMed] [Google Scholar]
- 3.Forster A, Smith J, Yang J, et al. Information provision for stroke patients and their caregivers (Cochrane Review) The Cochrane Library. 2004;1:1–74. [Google Scholar]
- 4.Yates BC, Norman J, Meza J, et al. Effects of Partners Together in Health Intervention on physical activity and healthy eating behaviors: a pilot study. J Cardiovasc Nurs. 2015;30(2):109–120. doi: 10.1097/JCN.0000000000000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 6.Morse JM, Field PA. Nursing Research: The Application of Qualitative Approaches. Nelson Thornes; 1995. [Google Scholar]
- 7.Milligan F. Cardiac rehabilitation: an effective secondary prevention intervention. British J Nurs. 2011;21(13):782–785. doi: 10.12968/bjon.2012.21.13.782. [DOI] [PubMed] [Google Scholar]
- 8.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 9.Jones MI, Greenfield S, Jolly K. Patients' experience of home and hospital based cardiac rehabilitation: a focus group study. Eur J Cardiovasc Nurs. 2009;8:9–17. doi: 10.1016/j.ejcnurse.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Sutton EJ, Rolfe DE, Landry M, et al. Cardiac rehabilitation and the therapeutic environment: the importance of physical, social, and symbolic safety for programme participation among women. J Advanced Nurs. 2012;68(8):1834–1846. doi: 10.1111/j.1365-2648.2012.06041.x. [DOI] [PubMed] [Google Scholar]
- 11.Wingham J, Dalal HM, Sweeney KG, et al. Listening to patients: choice in cardiac rehabilitation. Eur J Cardiovasc Nurs. 2016;5:289–294. doi: 10.1016/j.ejcnurse.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Hillsdon KM, Kersten P, Kirk HJ. A qualitative study exploring patients’ experiences of standard care or cardiac rehabilitation post minor stroke and transient ischaemic attack. Clin Rehabil. 2013;27(9):845–853. doi: 10.1177/0269215513478956. [DOI] [PubMed] [Google Scholar]
- 13.Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals Behav Med. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yates BC, Rowland S, Mancuso K, et al. Reducing cardiovascular risk in spouses of cardiac patients: a randomized controlled trial. West J Nurs Res. 2015;37(1):85–102. doi: 10.1177/0193945914551390. [DOI] [PubMed] [Google Scholar]
- 15.Mosca L, Mochari H, Liao M, et al. A novel family-based intervention trial to improve heart health: FIT heart: results of a randomized controlled trial. Circ Cardiovasc Qual Outcomes. 2008;1(2):98–106. doi: 10.1161/CIRCOUTCOMES.108.825786. [DOI] [PMC free article] [PubMed] [Google Scholar]