Abstract
Objective
To investigate whether acculturation to U.S. culture is associated with greater post-traumatic stress disorder (PTSD) symptomatology through diminished family cohesion among Latinos living with HIV on the U.S.-Mexico Border.
Method
Baseline survey data were analyzed from a sample of Latinos seeking HIV care from a publically funded HIV clinic in El Paso, Texas. We used a regression-based bootstrapping approach to test our mediation hypothesis.
Results
A total of 248 Latinos living with HIV completed the survey, with 96.4% being of Mexican descent, 19.4% female (gender self-identification), and 63.7% non-heterosexual (sexual orientation self-identification). Family cohesion mediated the relationship between U.S. acculturation and PTSD symptom scores (a1*b1 = .03, 95% CI [.01 – .06]), an effect independent of acculturation to Latino culture.
Conclusions
Acculturation to U.S. culture may negatively impact mental health through weakening family bonds in this vulnerable population.
Keywords: Latino/Hispanic, Acculturation, HIV/AIDS, Post-Traumatic Stress, Family cohesion
Latinos now account for nearly one in four new HIV diagnoses each year in the United States (U.S.) (CDC, 2016). More notably, 60% of all newly HIV-diagnosed Latinos were reported to be born outside the U.S., while men who have sex with men continue to account for a majority of all newly diagnosed Latinos (86.5%) (CDC, 2014a; CDC, 2016; Holtgrave, 2014). Large proportions of Latinos are neither retained in HIV care (42%) nor suppressing the virus (46%), two priorities for the remediation of HIV health disparities in the U.S (Gant et al., 2014).
People living with HIV (PLWH), including Latinos, suffer from alarming rates (range of 33–48%) of diagnosable mood and anxiety-related mental disorders (Bing et al., 2001; Mimiaga et al., 2013). And given the intersection of HIV, trauma, and stress, HIV and non-HIV related post-traumatic stress disorder (PTSD) is also highly prevalent (Applebaum et al., 2015; Machtinger, Wilson, Haberer, & Weiss, 2012). The differentiating factor between HIV and non-HIV related PTSD is the indexing trauma (e.g., trauma stemming from HIV diagnosis vs. sexual assault). However, in general, psychological distress is especially worrisome among PLWH due to its association with disease progression and mortality (Leserman et al., 2008; Lima et al., 2007). And among the growing majority of Latinos living with HIV who are foreign-born (CDC, 2014a), we know little about whether and how acculturation to life in the U.S. is linked to their experience of anxiety and stress-related disorders, particularly PTSD symptomatology.
There is a large and complex literature showing distal and heterogeneous associations between acculturation (in its many conceptual forms) and health (Du & Li, 2015; Lara, Gamboa, Kahramanian, Moralez, & Hayes Bautista, 2005; Rivera et al., 2008; Villatoro, Morales, & Mays, 2014). However, documentation of potential mediators of these effects is scarce. As part of a “new wave” of acculturation research, mechanisms are sought to help explain how the acculturation process may impact health (Abraído-Lanza, Echeverría, & Flórez, 2016).
One potential mechanism to explore is maintenance or reconciliation of family cohesion in response to acculturation to life in the U.S., which may be associated with a greater desire for privacy, increased family conflict, and less familial support (Miranda, Bilot, Peluso, Berman, & Van Meek, 2006; Smokowski, Rose, & Bacallao, 2008). Family cohesion is defined as emotional bond among family members (Rivera et al., 2008). When diminished, family cohesion has been directly associated with psychological distress among Latinos, although only as depressive symptoms and problematic alcohol use (Ekas et al., 2016; Marsiglia, Kulis, Parsai, Villar, & Garcia, 2009; Rivera et al., 2008; Kliewer et al., 2006). What is yet to be tested is whether greater acculturation to life in the U.S. is linked to psychological stress as PTSD symptomatology through diminished family bonds among Latinos living with HIV.
Objective
There is strong precedent for linking PTSD to family cohesion. One 20-year longitudinal study found evidence of a bi-directional relationship between PTSD severity and family cohesion (Solomon, Horesh & Ein-Dor, 2013). That is, over a 20-year period, baseline PTSD severity was predictive of diminished family cohesion, which overtime predicted greater PTSD severity (Solomon, et al., 2013). For Latino/as groups, family cohesion may be a critical area of study as this may be a basis of support in the management of their HIV. Thus, the objective of this study was to test whether family cohesion mediated the relationship between greater acculturation to U.S. culture and higher PTSD symptomatology among Latinos living with HIV on the U.S-Mexico Border, a region of high mobility and marked health disparities (CDC, 2014b).
METHOD
Procedures
Data for this study derive from a randomized controlled trial evaluating an intervention to treat depression and medication non-adherence among Latinos living with HIV. The study was conducted at a publically funded HIV clinic in the U.S.-Mexico Border city of El Paso, Texas (Simoni et al., 2013). Participants were recruited from flyers, front desk staff, and medical providers (only 5 of the 295 recruitment referrals declined to participate, and most referrals deemed ineligible were due to reasons not related to the study; Simoni et al., 2013). Inclusion criteria required that participants be (1) at least 18 years of age (2) HIV-positive, (3) Latino/Hispanic, (4) fluent in Spanish or English, and (5) receiving HIV care at the study site. At the baseline interview before randomization, eligible individuals completed the informed consent process and a one-hour interviewer-administered survey, and received $20. Responses to the measures used in this analysis were from the baseline survey data. The Institutional Review Boards of the two participating universities approved the study.
Survey Measures
Measures captured demographic information, gender self-identification (male, female, or transgender), sexual orientation self-identification from 1 (heterosexual only) to 7 (gay or lesbian only), and other HIV and psychosocial variables. For descriptive purposes, sexual orientation was coded as either “heterosexual exclusively” (score of 1) or “non-heterosexual” (score of 2 through 7). Measures published and validated in Spanish were used when available. Measures not available in Spanish were translated by a certified translator and reviewed and back translated by the research staff and a second independent translator.
Acculturation
The Abbreviated Multidimensional Acculturation Scale (AMAS; Zea, Asner-Self, Birman, & Buki, 2003) is a 42-item measure that assesses biculturalism: 1) acculturation to U.S. culture (21 items), and 2) acculturation to a person’s self-identified culture of origin (i.e., Latino culture; 21 items). Items are scored on a 4-point Likert-type response scale. Total scores were calculated from the acculturation to the U.S. culture subscale, which comprises three dimensions: 1) U.S. cultural identity (e.g., “think of myself as being a U.S. American”), 2) English-language competence (e.g., “understand English on television and movies”), and 3) U.S. cultural competence (e.g., “understand American political leaders/history/television”). Identical dimensions are measured in the acculturation to Latino culture subscale, which was used as a covariate in the mediation model. The AMAS was validated in two separate Latino samples (Zea et al., 2003). Scores range from 1 (low acculturation) to 4 (high acculturation) and were calculated by summing all responses and dividing by the number of items.
Family Cohesion
We used the National Latino and Asian American Study 10-item family cohesion measure (Alegria et al., 2004; Olson, 1989). Items are scored on a 4-point Likert-type scale from 1 (strongly disagree) to 4 (strongly agree). Each item is a statement regarding each respondants’ family closeness (e.g., “confide in each other”), communication (e.g., “express feelings with family”) and cohesion (e.g., “feel very close to one another”). Higher scores represent greater cohesion.
PTSD Symptomatology
The PTSD Checklist - Civilian version (PCL-C) is a 17-item, past 30-day, self-report measure (Ruggiero, Del Ben, Scotti, & Rabalais, 2003). Each item is mapped to a PTSD diagnostic symptom within one of three clusters in the DSM-IV: 1) re-experiencing the event (e.g., “repeated disturbing dreams of the stressful event”), 2) avoidance and numbing response (e.g., “avoid activities or situations because they remind you of a stressful experience”), or 3) hyperarousal (e.g., “feeling super alert or watchful on guard”). Instructions are as follows: “Below is a list of problems and complaints that people sometimes have in response to stressful experiences. Please read each one carefully and put an “X” in the box to indicate how much you have been bothered by that problem in the past month. The response options range from 1 (not at all) to 5 (extremely). Total scores are reported for descriptive purposes, but six non-specific items (e.g., “having trouble falling or staying asleep” and “having difficulty concentrating”) were removed from the mediation analysis to improve the specificity of the PCL-C measure and to remove any confound with HIV or other mental health symptoms (see Kalichman, Rompa, & Marjorie, 2000). These scores are referred to as adjusted PCL-C scores.
Statistical Analysis
Basic descriptive statistics and inferential statistics (i.e., bivariate association test) were used. To test the mediation hypothesis, we used a regression-based bootstrapping approach (k = 10,000 bootstrap samples) with the bias correction feature and 95% confidence intervals as the indicator for statistical significance via the SPSS PROCESS macro (Hayes, 2009). The mediation model included the covariates of age (continuous variable), years since HIV diagnosis (continuous variable), language the survey was completed in (Spanish = 0, English = 1), and acculturation to Latino culture subscale scores.
Results
Descriptive Statistics
A total of 248 surveys were analyzed. Overall, 96% of the total Latino sample was of Mexican descent, 79.4% identified as male, and 63.7% identified as not exclusively heterosexual. The sample had a mean age of 45.3 years (SD = 11.3) and over nine years living with HIV (SD = 6.4). Over 60% of the sample completed the survey in Spanish and 18% lived in Mexico during the past year. Participants reported a mean of 23.2 (SD = 55) roundtrip border crossings in the past year.
In summary, average scores (shown in Table 1) were moderately high on the acculturation to U.S. subscale (M = 2.88, SD = .80). According to two original validation studies, our sample scored lower on the acculturation to U.S. culture subscale than a U.S.-born Latino college sample (M = 3.5, SD = .41) and similarly to a Latin American-born immigrant sample (M = 2.91, SD = .54; Zea et al., 2003). The mean PCL-C total score was relatively high (M = 36.45, SD = 25.27). Total PCL-C scores in or above the range of 35–50 (20.8% of our sample scored >49) have high specificity and sensitivity for a PTSD diagnosis, although a diagnostic interview is needed to make a diagnosis (Brewin, 2005).
Table 1.
Participant Characteristics
| Total Sample N = 248 Mean (SD) or % |
|
|---|---|
| Age | 45.3 (11.3) |
| Years living with HIV | 9.3 (6.35) |
| Residence | |
| Renting | 46% |
| Homeowner | 18.5% |
| Living in family home | 24.2% |
| Living in non-family home | 6.9% |
| Other | 4% |
| Employment | |
| Full-time | 12.5% |
| Part-time | 12.1% |
| Odd jobs | 14.5% |
| Not currently working | 60.9% |
| Language Preference | |
| Spanish | 60.5% |
| English | 34.5% |
| Gender Self-Identification | |
| Male | 79.4% |
| Female | 19.4% |
| Transgender Female | 0.8% (n = 2) |
| Transgender Male | 0.4% (n = 1) |
| Sexual Orientation Responses | |
| Heterosexual only | 26.3% |
| Non-Heterosexual | 63.7% |
| Income | |
| < $20,000 | 74.6% |
| $20,000 to $39,999 | 14.9% |
| $40,000 to $59,999 | 3.2% |
| > $60,000 | 5.2% |
| Post-Traumatic Checklist – Civilian Version | |
| PCL Total Severity Score | 36.45 (25.27) |
| PCL A - Re-experiencing Events subscale score | 10.37 (4.95) |
| PCL B – Avoidance/Numbness subscale score | 14.59 (6.60) |
| PCL C – Symptoms of Arousal subscale score | 11.48 (4.86) |
| *PCL Adjusted Score | 20.93 (8.93) |
| † Multidimensional Acculturation Scale | |
| U.S. Acculturation Total Score | 2.88 (0.80) |
| U.S. Identity Subscale Score | 3.08 (1.02) |
| U.S. English-language Competence Subscale Score | 2.92 (0.98) |
| U.S. Cultural Competence Subscale Score | 2.61 (0.77) |
Note.
PCL Adjusted score was calculated by removing items that measure non-specific post-traumatic stress symptoms to eliminate any confounding stress symptoms (e.g., “trouble falling or staying asleep”).
Acculturation scores range from 1 (Strongly disagree/not at all well) through 4 (strongly agree/extremely well), with higher scores representing greater acculturation to the U.S.
Bivariate Associations
As expected, acculturation to the U.S. was negatively associated with family cohesion (r = −.19, p = .001) and positively associated with adjusted PCL-C scores (r = .22, p = .001). Acculturation to Latino culture was positively correlated with family cohesion (r = −.16, p = .02) and negatively correlated with adjusted PCL-C scores (r = −.19, p = 003). There was no association between the acculturation to U.S. culture and acculturation to Latino culture subscales (r = .05, p = .94).
Mediation
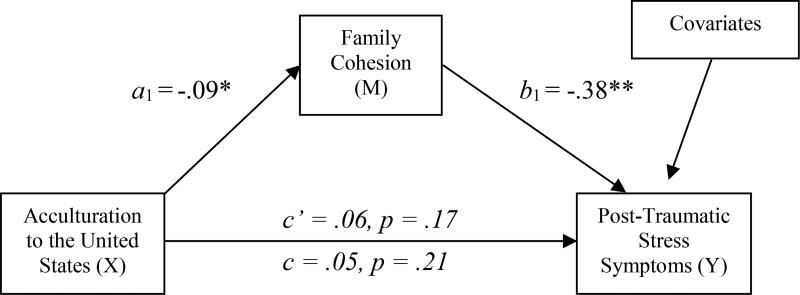
As seen in Figure 1, greater acculturation to the U.S. culture (X) was associated with lower family cohesion (M) (a1 path, b = −.09, p = .005) and not directly associated with adjusted PCL-C scores (Y) (c path, b = .05, p = .21). Greater family cohesion (M) was associated with lower adjusted PCL-C scores (Y) (b1 path, b = −.38, p < .001). Family cohesion evidenced a statistically significant mediating effect between acculturation to U.S. culture and adjusted PCL-C scores (a1*b1 = .03, 95% CI [.01 – .06] with an adjusted R2 value of .21 (p < .001). Among the covariates, older age and greater acculturation to Latino culture were associated with lower adjusted PCL-C scores, respectively (bs = −.11 & −.10, ps < .04). The covariate of language (English vs. Spanish) was not associated with adjusted PCL-C scores.
Figure 1. Family cohesion mediates the relationship between acculturation and post-traumatic stress symptoms.
K = 10,000 bootstrap samples. Post-traumatic stress symptoms (Y) are adjusted PCL scores (i.e., unique PTSD symptom items). Covariates included age, years since HIV diagnosis, language the interview was completed in, and acculturation to Latino culture. Note. *p< .05, ** p< .01
Discussion
This study of Latinos living with HIV in the U.S-Mexico Border region yielded two major findings. First, greater acculturation to the U.S. was associated with higher PTSD-specific symptoms through diminished family cohesion, controlling for the level of acculturation to Latino culture. Second, the total sample had high levels of both acculturation to U.S. culture and to Latino culture, and showed elevated PTSD symptomatology, respectively. Because the HIV epidemic continues to disproportionately impact Latinos in the U.S., especially those who are foreign-born (CDC, 2014a), the application of acculturation research findings may help understand how evolving family relationships affect the mental health and the management of HIV.
Furthermore, the levels of acculturation to U.S. culture and Latino culture (i.e., maintenance of culture of origin) were not correlated with one another in this sample. Thus, these findings support the bilinear and multidimensional conception of acculturation, which posits that Latinos engage in two, context-dependent acculturative processes (Félix-Ortiz, Newcomb, & Myers, 1994; Zea et al., 2003). One process is the learning and adopting non-native cultural behaviors and customs, which in our sample is associated with greater PTSD symptomatology indirectly through less family cohesion. The other process is the maintenance of Spanish language proficiency and a Latino cultural identity; the latter protected against PTSD symptomatology directly in our sample. It is therefore possible that acculturative stress contributes to a loosening of family bonds over time and through family generations (Miranda, Estrada, Firpo-Jimenez, 2000), which may then exacerbate or trigger a vulnerability to stress-related psychiatric disorders.
However, a strong attachment to a person’s culture of origin, irrespective of the acculturation to U.S. culture, may provide a protective health effect. Given the cross-cultural context of the study setting (18% of participants reported living in Mexico for some time), it is not surprising to have observed high scores on each acculturation subscale given the ease with which residents in this region can travel between El Paso, Texas and Ciudad Juárez, Chihuahua, Mexico. Latinos living in this region exemplify the bilinear process to acculturation not only psychologically, but also socially and culturally.
We strengthened the validity of our mediation analysis by removing general distress items from our PTSD measure, such as “trouble falling or staying asleep” or “loss of interest in things you used to enjoy,” and only including items that assessed unique PTSD symptom clusters: 1) avoidance/numbing, 2) re-experiencing the event, and 3) hyperarousal symptoms. Thus, diminished family cohesion was associated with unique PTSD symptoms, which may compound the effects of abuse and trauma commonly reported among PLWH (Sherr et al., 2011) or the effects of recent violence across the border in Ciudad Juárez (Borunda, 2010; Carter & Kodrich, 2013). However, we were not able to directly assess exposure to trauma in Ciudad Juárez or surrounding areas of Mexico, and can only speculate about the nature of our participants’ exposures.
There is also literature to suggest that Latinos have a slightly higher “conditional” risk for the onset, persistence, and severity of PTSD, compared to other racial/ethnic groups, and perhaps a different symptom structure (i.e., greater re-experiencing cluster symptoms; Alcántara, Casement, & Lewis-Fernández, 2013). In one analysis (not specific to HIV), the distinguishing factor between White and Latino police officers’ PTSD severity was that Latinos demonstrated greater peritraumatic dissociation (i.e., detachment, depersonalization, time distortion) at the time of the traumatic event and greater use of self-blame and wishful thinking coping strategies (Pole, Best, Metzler, & Marmar, 2006). However, the authors did not measure potential mediators and could only offer speculations around fatalism and religiosity as to why Latinos were more likely to use avoidant coping strategies. In a review of PTSD among Latinos, the strongest evidence (albeit only correlational and small) suggests that increased risk for PTSD may be attributable to both avoidance coping and structural determinants, such as lack of health insurance, poverty and limited education (Alcántara et al., 2013).
One strategy that could mitigate poorer coping skills and structural factors is the use of cognitive and behavioral-based therapies (CBT) for PTSD in HIV care. CBT has been tailored to Latinos with HIV and depression, and more generally to PLWH with trauma histories (Applebaum et al., 2015; Sikkema et al., 2007; Simoni et al., 2013). Given the call to integrate behavioral health programs into primary care settings, CBT-type programs for PTSD within HIV care could help overcome structural factors that interfere with Latinos engagement in specialized care (Alegría et al., 2007; Patel et al., 2013). Furthermore, because our findings suggest the importance of family cohesion when considering pathways to prevent the development of PTSD symptomatology, one option is to weave issues of family and social support throughout an intervention program, as done in a CBT efficacy trial for Latinos with HIV (Simoni et al., 2013).
The findings are limited by the self-report and cross-sectional nature of our methods. Furthermore, Latinos living with HIV in this study were primarily of Mexican descent and living in a unique border setting, so their experiences may not generalize to other Latino groups who live in less culturally integrated cities. Also, we did not capture the originating traumatic event associated with each PTSD symptom score but, as described above, removed all non-specific items to better capture the unique burden of PTSD symptomatology in this sample. Nonetheless, our findings have important implications for work with this population. The results underscore the need for access to mental health treatment, which is limited in the region under study. Moreover, bolstering natural familial support networks may have a direct impact on mental health outcomes (Snowden, 2007). This is especially important as PLWH become acculturated to U.S. norms and values, as a potential preventative measure against psychological distress.
In conclusion, Latinos living with HIV on the U.S.-Mexico border are a vulnerable group with significant psychological distress, yet limited access to quality mental health care. Providing this care, as well as supporting indigenous family social networks and cohesion, are needed to promote mental health, which can improve HIV treatment outcomes overall and reduce health disparities.
Acknowledgments
We are grateful to the patients and staff of Centro de Salud Familiar la Fe CARE Center, Inc. for their participation and facilitation of this study. We thank members of our community and administrative advisory boards as well as research consultants Jaime Anaya, Kurt C. Organista, Steffanie A. Strathdee, Karina Walters, and Randolph Whitworth. We would also like to thank those who aided with project implementation, including Jessica Armendariz, Teresa Frias, Carolina Lara, Chrisie Lemon, Virginia Longoria, Elsa Martin, Antonio Martinez, Miriam Pando, Tatiana Rodriguez, and Cesar Villareal Ramos from the University of Texas at El Paso, and Kimberly Nelson, Cynthia Pearson, and Samantha Yard from the University of Washington.
Funding
This research project was supported by the National Institute of Mental Health (NIMH) grants 1R34-MH08674 and minority research supplement award R34-MH084674-S1, and in part by the Center for AIDS Research (P30 AI027757). The first author completed the manuscript with support by grant T32-MH19105 and 3R01-MH102198-04S1 from the NIMH. The third author was supported by grant 4R25-MH097591-05.
Footnotes
Conflict of interest
None
References
- Abraído-Lanza AF, Echeverría SE, Flórez KR. Latino immigrants, acculturation, and health: Promising new directions in research. Annual Review of Public Health. 2016;37:219–236. doi: 10.1146/annurev-publhealth-032315-021545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcántara C, Casement MD, Lewis-Fernández R. Conditional risk for PTSD among Latinos: A systematic review of racial/ethnic differences and sociocultural explanations. Clinical Psychology Review. 2013;33:107–119. doi: 10.1016/j.cpr.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American Study. American Journal of Public Health. 2007;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Vila D, Woo M, Canino G, Takeuchi D, Shrout P. Cultural relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods in Psychiatric Research. 2004;13:270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Applebaum AJ, Bedoya CA, Hendriksen ES, Wilkinson JL, Safren SA, O’Cleirigh C. Future directions for interventions targeting PTSD in HIV-infected adults. Journal of the Association of Nurses in AIDS Care. 2015;26:127–138. doi: 10.1016/j.jana.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, Shapiro M. Psychiatric disorders and drug use among Human Immunodeficiency Virus–Infected adults in the United States. Archives of General Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Borunda D. Special report: Juarez deserves the title of most dangerous city in the world. El Paso Times. 2010 Jun 7; Retrieved from http://www.elpasotimes.com/Juarez/ci_15241689?source=pkg.
- Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. Journal of Traumatic Stress. 2005;18:53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- Carter C, Kodrich K. Challenges and dangers of reporting in a tumultuous border region. How journalist at the El Paso Times deal with violence in neighboring Ciudad Juarez. Journals and Mass Communication Quarterly. 2013;90:331–346. [Google Scholar]
- Centers for Disease Control and Prevention. HIV Surveillance Report. 2014a;26 2014; Retrieved from http://www.cdc.gov/hiv/ [Google Scholar]
- Center for Disease Control and Prevention. Improving HIV Surveillance and Prevention Intervention Efforts among Hispanic or Latino Migrant Communities in United States-Mexico Border States: Arizona, California, New Mexico and Texas. 2014b Retrieved from http://www.cdc.gov/hiv/pdf/policies_nhas_improving_hiv_surveillance.pdf.
- Center for Disease Control and Prevention. HIV and AIDS Among Latinos. 2016 Retrieved from, https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/Cdc-hiv-latinos-508.pdf.
- Du H, Li X. Acculturation and HIV-related sexual behaviours among international migrants: A systematic review and meta-analysis. Health Psychology Review. 2015;9:103–122. doi: 10.1080/17437199.2013.840952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekas NV, Ghilain C, Pruitt M, Celimli S, Gutierrez A, Alessandri M. The role of family cohesion in the psychological adjustment of non-Hispanic White and Hispanic mothers of children with autism spectrum disorder. Research in Autism Spectrum Disorders. 2016;21:10–24. doi: 10.1016/j.rasd.2015.09.002. [DOI] [Google Scholar]
- Felix-Ortiz M, Newcomb MD, Myers H. A multidimensional measure of cultural identity for Latino and Latina adolescents. Hispanic Journal of Behavioral Sciences. 1994;16:99–115. doi: 10.1177/07399863940162001. [DOI] [Google Scholar]
- Gant Z, Bradley H, Hu X, Skarbinksi J, Hall H, Lansky A. Hispanics or Latinos living with diagnosed HIV: Progress along the Continuum of HIV Care – United States, 2010. Morbidity and Mortality Weekly Report. 2014;63:886–890. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6340a2.htm. [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76:408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Holtgrave DR. Development of year 2020 goals for the National HIV/AIDS Strategy for the United States. AIDS and Behavior. 2014;18:638–643. doi: 10.1007/s10461-013-0579-9. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. Journal of Nervous and Mental Disease. 2000;188:662–670. doi: 10.1097/00005053-200010000-00004. Retrieved from http://journals.lww.com/jonmd/Pages/default.aspx. [DOI] [PubMed] [Google Scholar]
- Kliewer W, Murrelle L, Prom E, Ramirez M, Obando P, Sandi L, del Carmen Karenkeris M. Violence exposure and drug use in Central American youth: Family cohesion and parental monitoring as protective factors. Journal of Research on Adolescence. 2006;16:455–478. doi: 10.1111/j.1532-7795.2006.00502.x. [DOI] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosomatic Medicine. 2008;70:539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Lima VD, Geller J, Bangsberg DR, Patterson TL, Daniel M, Hogg RS. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS. 2007;21:1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Wilson TC, Haberer JE, Weiss DS. Psychological trauma and PTSD in HIV-Positive Women: A meta-analysis. AIDS and Behavior. 2012;16:2091–2100. doi: 10.1007/s10461-011-0127-4. [DOI] [PubMed] [Google Scholar]
- Marsiglia FF, Kulis S, Parsai M, Villar P, Garcia C. Cohesion and conflict: Family influences on adolescent alcohol use in immigrant Latino families. Journal of Ethnicity in Substance Abuse. 2009;8:400–412. doi: 10.1080/15332640903327526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Reisner SL, Grasso C, Crane HM, Safren SA, Mayer KH. Substance use among HIV-infected patients engaged in primary care in the United States: Findings from the Centers for AIDS Research Network of Integrated Clinical Systems Cohort. American Journal of Public Health. 2013;103:1457–1467. doi: 10.2105/AJPH.2012.301162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A, Bilot J, Peluso P, Berman K, Van Meek L. Latino families: The relevance of the connection among acculturation, family dynamics, and health for family counseling research and practice. The Family Journal. 2006;14:268–273. doi: 10.1177/1066480706287805. [DOI] [Google Scholar]
- Miranda AO, Estrada D, Firpo-Jimenez M. Differences in family cohesion, adaptability, and environment among Latino families in dissimilar stages of acculturation. Family Journal. 2000;8:341–350. doi: 10.1177/1066480700084003. [DOI] [Google Scholar]
- Olson DH. Family assessment and intervention: The circumplex model of family systems. Child & Youth Services. 1989;11:9–48. doi: 10.1300/J024v11n01_02. [DOI] [Google Scholar]
- Patel V, Belkin GS, Chockalingam A, Cooper J, Saxena S, Unützer J. Grand challenges: Integrating mental health services into priority health care platforms. PLoS Medicine. 2013;10:e1001448. doi: 10.1371/journal.pmed.1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pole N, Best SR, Metzler T, Marmar CR. Why are Hispanics at greater risk for PTSD? Cultural Diversity and Ethnic Minority Psychology. 2005;11:144–161. doi: 10.1037/1099-9809.11.2.144. [DOI] [PubMed] [Google Scholar]
- Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, Alegria M. Family cohesion and its relationship to psychological distress among Latino groups. Hispanic Journal of Behavioral Sciences. 2008;30:357–378. doi: 10.1177/0739986308318713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero KJ, Ben KD, Scotti JR, Rabalais AE. Psychometric properties of the PTSD checklist—civilian version. Journal of Traumatic Stress. 2003;16:495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Sherr L, Nagra N, Kulubya G, Catalan J, Clucas C, Harding R. HIV infection associated post-traumatic stress disorder and post-traumatic growth – A systematic review. Psychology, Health, & Medicine. 16:612–629. doi: 10.1080/13548506.2011.579991. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Tarakeshwar N, Neufeld S, Fox AM. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: Reductions in traumatic stress. AIDS and Behavior. 2007;11:49–60. doi: 10.1007/s10461-006-9149-8. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Wiebe JS, Sauceda JA, Huh D, Sanchez G, Longoria V, Safren SA. A preliminary RCT of CBT-AD for adherence and depression among HIV-positive Latinos on the U.S.-Mexico Border: The Nuevo Día Study. AIDS and Behavior. 2013;17:2816–2829. doi: 10.1007/s10461-013-0538-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smokowski PR, Rose R, Bacallao ML. Acculturation and Latino family processes: How cultural involvement, biculturalism, and acculturation gaps influence family dynamics. Family Relations. 2008;57:295–308. [Google Scholar]
- Snowden LR. Explaining mental health treatment disparities: Ethnic and cultural differences in family involvement. Culture, Medicine and Psychiatry. 2007;31:389–402. doi: 10.1007/s11013-007-9057-z. [DOI] [PubMed] [Google Scholar]
- Solomon Z, Horesh D, Ein-Dor T. The longitudinal course of posttraumatic stress disorder symptom clusters among war veterans. The Journal of Clinical Psychiatry. 2009;70:837–843. doi: 10.4088/jcp.08m04347. Retrieved from http://www-psychiatrist-com.ucsf.idm.oclc.org/jcp/article/Pages/2009/v70n06/v70n0607.aspx. [DOI] [PubMed] [Google Scholar]
- Villatoro AP, Morales ES, Mays VM. Family culture in mental health help-seeking and utilization in a nationally representative sample of Latinos in the United States: The NLAAS. American Journal of Orthopsychiatry. 2014;84:353–363. doi: 10.1037/h0099844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zea MC, Asner-Self KK, Birman D, Buki LP. The Abbreviated Multidimentional Acculturation Scale: Empirical validation with two Latino/Latina samples. Cultural Diversity & Ethnic Minority Psychology. 2003;9:107–126. doi: 10.1037/1099-9809.9.2.107. [DOI] [PubMed] [Google Scholar]