Abstract
Objective
In this study, we tailor a child anxiety cognitive behavior therapy (CBT) program to fit the needs of rural Latino/a Spanish-speaking families, and examine the feasibility, acceptability, tolerability and safety of this intervention using two modes of service delivery.
Methods
Children (n = 31) (age 8–13) with anxiety disorders were recruited from primary care settings and randomized to one of two modes of parent mediated CBT bibliotherapy: 1) telephone delivered, therapist-assisted, bibliotherapy (TTB) (n = 15), and; 2) a more minimal contact, self-directed, bibliotherapy condition (SB) (n = 16). Independent evaluators administered a diagnostic interview at baseline and post-treatment; demographic and engagement related questionnaires were also administered.
Results
In the TTB group, 10 of 15 parents (66.7%) completed the requisite number of therapist-assisted bibliotherapy sessions, and in the SB group, 4 of 16 parents (25%) completed the requisite number of self-directed bibliotherapy modules; this comparison was significant, X2 (1) = 5.43, p = .02. In the TTB condition, treatment length and session duration were longer than reported in previous studies. Barriers that were most strongly endorsed were stressors and obstacles competing with treatment as well as treatment demandingness. Findings revealed good satisfaction across the conditions, although ratings were significantly higher in the TTB group, F = 5.67, p = .028. Remission rates (i.e., no anxiety disorder) for those that provided post-treatment data (N = 25) were 50% and 36% for the TTB and SB groups respectively, X2 (1) = .465, p = .50.
Conclusions
Implications of these feasibility findings and suggestions for future research are discussed. (clinicaltrials.gov unique identifier: NCT01491880)
Research on youth who reside in rural settings is sorely lacking and few studies have focused on anxiety disorders among rural youth. Findings from studies evaluating the prevalence of various mental health problems and psychiatric disorders in rural versus urban settings have been discrepant. While some studies report higher rates of psychiatric disorders in urban areas (Canino et al., 2004; Paykel et al., 2000), other studies report more problems, particularly depression, suicide, and substance use in rural youth (National Center on Addiction and Substance Abuse, 2000; Substance Abuse and Mental Health Services Administration [SAMHSA], 2001; Fontanella et al., 2015).
Despite inconsistencies in prevalence rates of psychiatric disorders, rural residents consistently receive fewer mental health services than their urban counterparts (Alegría et al., 2004; Angold et al., 2002; Elgar, Arlett, & Groves, 2003; Kataoka et al., 2003). In the 2001 National Health Interview Survey, rural residence, low education, and lack of insurance were associated with lack of service use among children with ADHD symptoms (Cuffe, Moore & McKeown, 2009). In another study that examined both ethnicity and urban-rural differences in mental health service use, Latino/a children in both urban and rural areas were less likely to have a mental health visit than European American children (Howell & McFeeters, 2008).
Various barriers deter mental health service utilization in rural communities including clinician shortages, transportation limitations, and long travel distances to clinics (Paul, Gray, Elhai, Massad, & Stamm 2006; US Congress, 1990). Attitudinal factors such as stigma, concerns about confidentiality and anonymity also deter appropriate service seeking (Rost, Fortney, Fischer, & Smith, 2002; Smalley et al., 2010). Further, rural residents often report cultural dissimilarities between themselves and mental health providers, who are often not from the community (Rost, Smith, & Taylor, 1993; Rost et al., 2002) and exhibit a preference for informal networks of care (Rost et al., 2002; Fox, Blank, Rovnyak, & Barnett, 2001). These factors all conspire to lead to lower rates of mental health service use in rural communities.
Low rates of mental health service utilization are also common in Latino/a youth (refs). Underutilization by Latino/a youth has been associated with a variety of barriers including language, logistic factors (e.g., transportation, time, competing priorities), beliefs about causes, and stigma associated with mental health treatment (Cabassa, Zayas, & Hansen, 2006). Findings also suggest that Latino/a parents’ perceptions of barriers, unrealistic expectations of therapy, and perceptions that they should be able to handle their child’s mental health problems on their own affect initial service uptake and ongoing treatment adherence (Yeh et al., 2003; McCabe et al., 2002).
Research examining the conjoint influence of being Latino/a and from a rural community, on mental health service use, are scarce. In one study, qualitative methods were used to examine rural Latina/o parents and mental health providers’ beliefs about mental health services, specifically evidence based treatments (Chavira, Bustos, Garcia, Ng & Camacho, 2017). Findings from this study suggest that time, literacy, stigma, multiple competing priorities, and homework compliance are prominent barriers to service use and treatment adherence in this community. In another study examining knowledge and beliefs about mental health among rural and urban Latino/a immigrant youth, findings suggest that Latino/a rural respondents were less likely to know of mental health resources than urban-based immigrant Latino/as (Garcia, Gilchrist, Vazquez, Liete, & Raymond, 2011). The lack of research focused on rural Latinos/as is concerning given the growing numbers of Latina/os in the United States with the most dramatic increases found in rural communities (Pew Hispanic Center, 2005a,b), the negative mental health outcomes associated with acculturative stress, and extant data suggesting that Latino/a youth experience greater symptoms of anxiety than European American youth (Weems, Hayward, Killen, & Taylor, 2002; Varela, Vernberg, Sanchez, Riveros, Mitchell, & Mashunkashey, 2004).
Various strategies have been suggested to address mental health disparities in underserved communities. The use of telemental health has been identified as one strategy for increasing rural populations’ access to mental health treatment (Farrell & McKinnon, 2003). Telemental health is a broad term that includes all mental health applications that utilize electronic and computer based technologies including interactive televideo communication (videoconferencing), internet, telephone, or facsimile transmission (Myers, Valentine, & Melzer, 2008). In pediatric rural settings, telemental health interventions have often relied on a consultation model, where a psychiatrist meets with a patient via videoconferencing and assists the primary care provider with diagnosis and treatment planning (mostly, medication management). In a study focused on utilization and satisfaction with interactive videoconferencing for rural youth with mental health problems, ratings of satisfaction and return appointments were high, with many families reporting that they otherwise would not have sought services at the local mental health center due to stigma, lack of confidence in the facility’s service, or their perception that they would not be able to obtain the services they needed (Myers et al., 2008). In a different study, videoconferencing was used for diagnostic assessment and treatment planning (mostly medication) and significant improvement was found in clinical symptoms 3-months after the initial evaluation (Yellowlees, Hilty, Marks, Neufield, & Bourgeois, 2008). Data supporting telemental health interventions for rural youth that extend beyond consultation and treatment planning, and actually deliver evidence-based psychosocial interventions, such as cognitive behavior therapy (CBT) are few however existing data support the initial effectiveness of such interventions with rural youth (Lyneham & Rapee, 2006; Feil et al., 2008).
Bibliotherapy has been proposed as another way to increase access to mental health care for rural youth through the provision of self-directed interventions that often require less therapist contact and fewer resources. In bibliotherapy interventions for youth, parents often are taught how to implement CBT strategies in their child’s daily life, with varying degrees of therapist support. At present, data suggest that parent-mediated bibliotherapy interventions, have similar outcomes to more intensive CBT delivered face to face with children and parents (Chavira et al., 2014; Leong, Cobham, de Groot, & McDermott, 2009). However, findings also suggest that greater therapist contact is associated with more favorable symptom outcomes. In a randomized controlled trial with rural Australian youth with anxiety disorders (n = 100) (Lyneham & Rapee, 2006), parent-mediated CBT, supported by therapist initiated telephone sessions, was more effective than therapist-assisted email sessions, or client-initiated telephone sessions; response rates were 79%, 33%, and 31% respectively. Currently, no studies have examined telehealth and bibliotherapy interventions with rural, Latino/a youth.
In general, research examining the efficacy of CBT interventions with ethnic minority youth with anxiety disorders has been limited. Further, few studies have examined whether and to what extent such interventions may need to be modified to be appropriate for ethnic minority youth such as Latino/as. Thus far, findings from randomized clinical trials examining CBT interventions for children with anxiety disorders have found mostly comparable outcomes between Latino/as and European Americans on measures of clinical response, remission, symptom severity and overall functioning (Pina, Silverman, Weems, Kurtines, & Goldman, 2003; Pina, Zerr, Villalta, & Gonzales, 2012; Silverman, Pina, & Viswesvaran, 2008). These studies have varied in the extent to which they have modified the intervention to be culturally appropriate with modifications ranging from Spanish translations of materials, the availability of bilingual therapists, therapist cultural sensitivity training, the inclusion of culturally salient themes, and more prescriptive approaches which tailored the intervention to fit the cultural needs of the individual. To our knowledge, no study has examined the use of culturally responsive minimal contact interventions such as telemental health and bibliotherapy approaches for rural Latino/a youth with anxiety disorders.
In this study, we examine the feasibility of the Cool Kids Outreach program modified for use with rural Latino/as. The Cool Kids Outreach Program (Lyneham and Rapee, 2006) is a good exemplar of a CBT bibliotherapy intervention for children with anxiety disorders that has been tailored to be parent-mediated with varying degrees of therapist contact. As part of these efforts, we have used a “cultural adaptation” framework that relies on a data-driven approach to ensure the cultural fit of the intervention while maintaining treatment fidelity (Lau, 2006). According this framework, adaptations are guided by empirical findings that support differences (e.g., ethnic, rural-urban, etc.) in the social validity of an intervention (e.g., engagement and acceptability), clinical outcomes, and/or risk and resiliency factors that may affect the etiology or course of the disorder. We have also applied a complementary cultural adaptation process (Barrera & Castro, 2006), which includes four phases (information gathering, preliminary adaptation design, preliminary adaptation tests and, adaptation refinement), to understand issues of cultural fit and refine the intervention accordingly. Data pertaining to the information gathering and preliminary adaptation design stages are presented in Chavira et al. (2017), and proposed modifications are reviewed in the Methods section of this paper.
The current study is consistent with the preliminary adaptation test phase of the adaptation process where both qualitative methodologies and pilot studies are used to assess: 1) sources of program non-fit, 2) implementation hurdles, 3) difficulties with program content, and 4) satisfaction with treatment. As such, this study examines the feasibility, tolerability, acceptability, and safety of two modes of service delivery for a translated and adapted version of the Cool Kids Outreach program in an underserved rural Latino/a community. Families were randomized to: 1) telephone delivered, therapist-assisted, bibliotherapy (TTB) and; 2) a more minimal contact, self-directed, bibliotherapy condition (SB). Families were assessed at baseline and post-treatment, using clinician administered diagnostic and self-report measures of engagement and feasibility. Although small sizes precluded formal hypothesis testing, the inclusion of the SB group allowed for the more realistic examination of feasibility related outcomes such as recruitment, randomization, assessment procedures, and retention that can inform larger studies using these interventions (Leon et al., 2011). Based on the available data, it was expected that the TTB condition would have better feasibility related outcomes than the SB condition.
Method
Participants and Procedure
A total of 31 parents and youth (ages 8–13 years) with anxiety disorders participated in this study. Baseline characteristics are presented in Table 1.
Table 1.
Baseline Parent and Child Characteristics
| All N = 31 (n) % | TTB (telephone) N = 15 (n) % | SB (self-directed) N = 16 (n) % | p value | |
|---|---|---|---|---|
| Child Age, mean (SD), y | 31 | M= 11.50, SD = 4.72 | M =11.00, SD = 4.15 | .76 |
| Parent Age, mean (SD), y | 31 | M = 37.66, SD=4.98 | M = 37.86,SD = 7.68 | .97 |
| Female | 29 (93.5) | 15 (100) | 14 (87.5) | .15 |
| Latino/a | 31 (100) | 15 (100) | 16 (100) | 1.00 |
| Parent Education | .89 | |||
| Some high school | 5 (16.1) | 3 (20) | 2 (12.5) | |
| High school graduate | 14 (45.2) | 7 (46.6) | 7 (43.8) | |
| Some college | 9 (29) | 4 (26.7) | 5 (31.3) | |
| College graduate | 3 (9.7) | 1 (6.7) | 2 (12.5) | |
| Married or Living Together | 22 (71) | 10 (66.7) | 12 (75) | .61 |
| Primary Anxiety disorder | ||||
| Specific Phobia | 9 (29) | 4 (26.7) | 5 (31.3) | .78 |
| Generalized anxiety | 14 (45.2) | 7(46.7) | 7 (43.8) | .87 |
| Social anxiety | 23 (74.2) | 13 (86.7) | 10 (62.5) | .12 |
| Separation Anxiety | 18 (58.1) | 9 (56.3) | 9 (60) | .83 |
| Obsessive Compulsive | 1 (3.2) | 0 (0) | 1 (6.3) | .33 |
| Comorbid Conditions | ||||
| Depressive disorders | 2 (6.5) | 1 (6.7) | 1 (6.7) | .96 |
| (Oppositional Defiant Disorder and Conduct Disorder) | 0 (0) | 0 (0) | 0 (0) | 1.00 |
| ADHD | 3 (9.7) | 1 (6.7) | 2 (12.5) | .58 |
Families were recruited from three primary care clinics located in a low-income, rural county of California by the US-Mexico border, through physician or self-referral. This county is considered “mostly rural” according to definitions based on population thresholds, density, land use, and distance (Ratcliffe, Burd, Holder, & Fields, 2016). Further, most health care centers within this county are designated as Health Professional Shortage Areas (HPSA), which applies to both mental health and primary care services, according to federal guidelines (HRSA, 2005). Prior to the start of the study, all pediatricians and allied professionals received information about the study, and symptoms of child anxiety. If a child with anxiety symptoms was identified, providers could describe the study and offer a pamphlet, or a consent to contact form. A research assistant visited each clinic regularly to pass out brochures and speak to interested parents. Recruitment materials were available in waiting areas in all clinics and exam rooms for self-referrals. Recruitment materials were bilingual in English and Spanish and included brochures, flyers, and signs describing the CBT program.
Parent informed consent and assent from the child were obtained at the initial eligibility visit. All parents were required to give permission for the primary care providers to be a part of the intervention, which included pediatrician notification about child’s participation in the study and treatment progress. Families also needed access to a telephone to participate in this study. Families were given demographic and clinical measures at the initial visit, and diagnostic interviews for the parent and child were scheduled to assess eligibility.
Clinical Inclusion/Exclusion: Parents and their child, who was between the ages of 8–13 years, could speak English or Spanish and had a primary diagnosis of social anxiety disorder, separation anxiety disorder, obsessive compulsive disorder, specific phobia, and/or generalized anxiety disorder based on the Anxiety Disorders Interview Schedule for Parent/Children (Silverrman & Albano, 1996), were eligible to participate. Children receiving psychotropic medication were also included; medication dose was required to be stable for at least 3 months prior to study entry and for the duration of the study. Comorbid conditions were permitted provided they were not the child’s predominant (i.e., primary) diagnosis. The appropriate Institutional Review Boards approved all procedures.
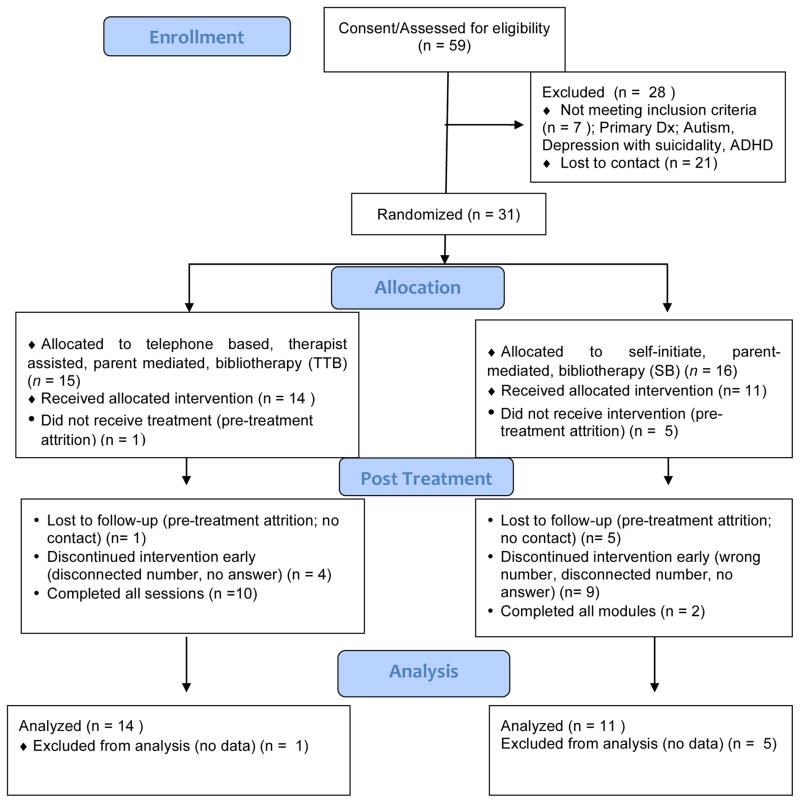
A total of 59 families consented to the study and 37 completed the eligibility/baseline visit (see Figure 1). Of these families, 6 were excluded because anxiety was not the primary diagnosis, and 31 families were randomized. In total, 15 families received the telephone delivered, therapist-assisted, bibliotherapy intervention (TTB) and 16 families received the self-directed, bibliotherapy intervention (SB). Parent-child dyads completed interviews at baseline and post-treatment by an independent evaluator who was blind to treatment condition as well as self-report measures assessing feasibility related outcomes.
Figure 1.
Consort Chart
Treatments
Cool Kids Outreach-Telephone-Delivered, Therapist-assisted, Bibliotherapy (TTB) (Lyneham & Rapee, 2006; Rapee, Abbott, & Lyneham, 2006). For this study, we translated all materials into Spanish, with appropriate adaptations made to meet the needs of rural Latino/a families as suggested by our initial qualitative studies (see Table 2). A certified translator and team of bilingual MH experts translated all materials to Spanish; community stakeholders and consumers also reviewed intervention materials. As part of this program, families received a parent workbook and a child workbook, as well as an audiobook based on the book, Helping Your Anxious Child, 2nd Edition (Rapee, Wignall, Spence, Cobham, & Lyneham, 2008). Materials were provided to parents in either English or Spanish, and children were provided with bilingual workbooks in order to address generational differences between parents and children related to language fluency. The major components of the intervention included psychoeducation, changing unhelpful thoughts, exposures, problem solving exercises, parent management exercises, and assertiveness skills. Each week parents and children were directed to read a chapter on a given CBT skill, complete activities designed to help them apply what they learned to their child’s fears and worries, and conduct various activities with their child. During telephone sessions, the therapist followed a protocol to review what parents worked on in the previous week in both their parent workbook, as well as with their child in the child’s workbook. This provided an opportunity to clarify concepts, review material, and provide feedback and support to the parent. The original Cool Kids Outreach program consists of 10 sessions covered over three to four months. In the current study, we included an additional session at the beginning of treatment to address potential engagement issues that emerged in the qualitative phase of this study (i.e., demystifying treatment, practical and attitudinal barriers). TTB sessions occurred exclusively with the caregiver/parent.
Table 2.
Adaptations based on qualitative studies (Chavira et al., 2015)
| Qualitative Theme | Adaptation for Service Delivery and Treatment |
|---|---|
| Treatment as inconvenient and time-consuming |
|
| Literacy & language barriers |
|
| Need for face-to-face contact and trust |
|
| Uncertainty regarding telephone based, parent-mediated, interventions |
|
| Treatment as stigmatizing |
|
Cool Kids Outreach-Self-Directed, Bibliotherapy (SB) (Lyneham & Rapee, 2006; Rapee, Abbott, & Lyneham, 2006). Families randomized to the SB condition received program materials along with instructions for completing weekly assignments. They received the same materials as families in the TTB condition, however, in the SB group, parents and children were expected to read the materials for that week and complete the workbook activities without planned therapist involvement. These families were given the option to initiate a telephone call to the therapist if they had questions or needed extra support. Families in this condition also received the initial engagement session.
Modifications
Modifications were informed by an initial series of literature reviews and qualitative studies discussed in Chavira et al., 2017. Modifications were mostly focused on improving the acceptability of the intervention and included mostly surface level modifications such as translation of study materials, tailoring of examples to be culturally appropriate to Latino/a families and to the rural context, simplifying workbook materials, and addressing issues of literacy (see Table 2). All intervention materials were translated by a certified translator with experience in mental health, as well as clinicians with expertise in Latino mental health. These materials were also reviewed by Latino/a, Spanish-speaking parents from the rural community where the study was conducted. Workbook materials were revised for a 6th grade reading level. Audiobook versions of the parent and child workbooks as well as video exemplars (presented on CDs and DVDs) of the core CBT skills were also developed to address issues with literacy in the community and to facilitate learning. Salient barriers such as stigma, time, literacy, multiple competing demands and homework (Chavira et al., 2017) were addressed in an adjunctive engagement session that was included at the beginning of the intervention. Per our qualitative studies, the core CBT skills (e.g., exposure, cognitive restructuring, use of rewards, etc.) were examined by a sample of parents and considered to be both acceptable and understandable and therefore were not modified for this pilot study (Chavira et al., 2017). Additionally, based on qualitative findings, neither parents nor providers suggested that intervention content needed to be modified in a systematic way to address acculturative stress and migration issues.
Supplemental Engagement Session
All families participated in a session focused on engagement strategies at session 1. These strategies addressed many of the barriers that emerged from the qualitative studies (see Table 2), and broadly focused on psychoeducation about the treatment process, increasing the family’s confidence in their ability to successfully complete the treatment, addressing attitudes about the program and mental health care that may affect treatment, and problem solving regarding potential logistical barriers to services (McKay, 1996; 1998; Nock & Kazdin, 2005). This supplemental engagement session was limited to 20–30 minutes.
Independent Evaluator Training
One PhD level and two masters-level research assistants served as independent evaluators and administered the Anxiety Disorders Interview Schedule for Children (ADIS-C/P: Silverman & Albano, 1996). Training included 10-hours of didactics, the review and scoring of multiple (i.e., 5–6) mock interviews, observation of two in-person interviews conducted by a senior evaluator, and the administration of at least two in-person interviews while being observed. A final 80% agreement rate on severity ratings, and all diagnoses (including comorbid diagnoses) were required for certification.
Therapist Training
Child anxiety specialists (CAS), the therapists who provided the CBT, were bilingual, and had at least a Masters level education in a counseling-related doctoral program. All CASs were trained to fidelity using preparatory self-study, a 2-day didactic workshop, viewing of exemplar case sessions from a previous trial, proficiency exams, supervised administration of at least two full cases, and ongoing supervision. Adherence with at least 80% of the core components/skills of the protocol (were the components administered or not), and a mean score reflecting good competence (a score of 6 or above) for each skill (range from 0–7) were required to be a therapist in this study. Further, mean ratings consistent with good competence were required on non-specific therapy components including rapport, empathy, and goal consensus.
Cultural Sensitivity Training
All independent evaluators, therapists, and study staff received cultural sensitivity training relevant to working with rural, Latino/a, and low-income families. Issues discussed that were specific to diagnostic interviewing included how to query and determine threshold for anxiety for realistic worries such as: 1) poverty related stressors (lack of financial resources), 2) separation anxiety stemming from parent’s seasonal work, and 3) immigration related stress. Similarly, clinicians were sensitized to consider issues of cultural context when discussing parenting behaviors (e.g., overprotectiveness vs. warmth), use of reward systems, co-sleeping, and assertiveness.
Measures
Demographic Measures
Literacy
Parental literacy was assessed in both English and Spanish by two items adapted from prior studies which demonstrated that even one screening question can help identify individuals with inadequate health literacy (Chew, Bradly, & Boyko, 2004). One of the items was; “How often do you need to have someone help you when you read instructions, pamphlets, or other written material in [English/Spanish] from your doctor or from your child’s school?” Items were scored on a 5-point scale ranging from 1 (never) to 5 (often), with higher scores indicating more difficulties with literacy. Scores on these items were used to inform whether tailoring efforts to address literacy issues would be necessary.
Acculturation
The Acculturation Rating Scale for Mexican Americans-II (ARSMA-II; Cuellar et al., 1995) is a 30-item self-report questionnaire assessing acculturation/acculturation related behaviors (e.g., language use and preference, ethnicity identity, cultural heritage, and ethnic interaction) (e.g., “I enjoy listening to Spanish language music,” “My friends are of Mexican origin”). Responses are provided on a 5-point Likert scale, with higher scores indicating greater endorsement of the construct. The scale consists of two independent subscales, American Orientation and Mexican Orientation, which allows for a multidimensional perspective to acculturation, where it is possible for an individual to orient toward one culture without necessarily distancing themselves from the other. The ARSMA also allows the participant to select the appropriate generation using operationalized definitions for generation levels ranging from first through fourth. The ARSMA-II demonstrates good construct validity and internal consistency (0.86–0.88) (Cuellar et al., 1995). The ARSMA-II was developed in English and Spanish. In this study, parents completed the ARSMA-II with regard to their own level of acculturation. In the current sample of parents, the internal consistency coefficient for the Mexican Orientation subscale was .896 and for the Anglo Orientation subscale, it was .941. The Cronbach alpha for the Spanish version of the full scale was .81, and for the English version, the alpha was .73.
DSM Diagnosis
The Anxiety Disorders Interview Schedule for Children (ADIS-C/P: Silverman & Albano, 1996)-Child and Parent Report is a semi-structured diagnostic interview designed to assess DSM-IV childhood anxiety disorders as well as depressive and behavioral disorders. The ADIS-C/P has been translated into Spanish. In a single psychometric study of the Spanish translated ADIS-C/P, test-retest reliability was good to excellent (kappa coefficients ranged from 0.64–0.96) (Piña and Silverman, 2004). Clinical severity ratings (CSR) range from 0–8 and a CSR of at least 4 is required for a clinical diagnosis. Clinical judgment is used to integrate information from both parent and child interviews and derive a final CSR rating based on both diagnostic interviews. In this study, remission from a disorder was defined as a CSR rating of <= 3 based on both the parent and child ADIS. The ADIS was administered by telephone at baseline to determine eligibility and at post-treatment. Previous findings suggest that diagnoses established during telephone administration are comparable to diagnoses obtained during standard administration of the ADIS-C-IV using both Child and Parent versions (Lyneham & Rapee, 2005).
Feasibility Measures
Barriers
The Barriers to Treatment Participation Scale (BTPS; Kazdin et al., 1997) consists of 44 items and assesses parents’ experiences of obstacles to participating in their child’s treatment. There are four subscales: 1) stressors or obstacles that compete with treatment (e.g., family stress, time etc., “My job got in the way of working on the program”); 2) treatment demands and issues (e.g., treatment as too difficult, confusing, long etc., “My child was not willing to do practice tasks”); 3) perceived relevance of treatment (e.g., “I felt treatment did not seem as important as the sessions continued), and; 4) relationship with therapist (e.g., “The therapist did not seem confident in my ability to carry out the program”). Items are rated on a 5 point Likert scale; 1 = never a problem, 2 = occasionally, 3 = sometimes, 4 = often; 5 = very often. Internal validity has been found to be robust (alphas = 0.86 and 0.93, respectively). Criterion and discriminant validity of the BTPS appear good (Kazdin et al., 1997; Nanninga et al., 2015). The BTPS was translated into Spanish and back translated. For this study, the BTPS was modified to be appropriate for both treatment conditions. The Cronbach alpha was .94 for the Spanish version, and .88 for the English version of the scale.
Satisfaction
The Parent Consumer Satisfaction Scale (March, 1999) consists of 14 items in which parents rate their level of satisfaction with the intervention related to treatment length, satisfaction, and problem resolution. Eleven of the items use a 7-point Likert response scale, with higher ratings indicating a higher degree of satisfaction; the remaining 3 items are open-ended questions regarding the intervention. The questionnaire consists of items with good face validity and has been used in previous studies (Chiu et al., 2008). This measure was translated into Spanish and back translated for use in this study. The Cronbach alpha was .82 for the Spanish version, and .81 for the English version of the scale.
Adherence
The Treatment Adherence Questionnaire (TAQ; Nock et al., 2007) is a 2-item scale that assesses parents’ adherence to treatment recommendations by assessing the quantity and quality of parent adherence to the treatment recommendations in the previous week (“During the past week, in what percentage of your interactions with [child’s name] did you use the skills learned so far?”). This item is completed by both the parent and the therapist and is scored on a five-point scale: 0 = 0%, 1 = 25%, 2 = 50%, 3 = 75%, and 4 = 100%. In addition, the therapist completes one item regarding the overall quality of the parent adherence to treatment recommendations using a five-point scale ranging from 0 (no adherence/ mastery) to 4 (perfect adherence/ mastery). The TAQ was translated into Spanish and back translated for use in this study. This questionnaire was only used in the TTB condition.
Data Analysis Plan
Using SPSS 24 statistical software, variables were tested for normality. Analyses were performed to assess baseline differences between the treatment conditions (see Table 1). Chi-square analyses were used to examine response rates. Given the feasibility focus of this study, and the small sample size, formal hypothesis testing was not part of the data analytic plan.
Results
Demographic and Clinical Characteristics
Descriptive findings are presented in Table 1. All children were Latino/a (primarily of Mexican descent). Parents were mostly first generation (80%) (e.g., born in Mexico or other country), and 92% identified as Mexican/Mexican American as reported in the ARSMA-II. Based on the ARSMA-II, using a scale of 1–5, parents had a mean score of M = 4.22 (SD =.75) on Mexican Orientation and M = 2.8 (SD = 1.0) on Anglo Orientation, such scores indicate a more “traditional” (as opposed to bicultural or assimilated) orientation style (Cuellar et al., 1995). Most parents were married or living together (71%), and 61.3% had the equivalent of a high school degree (45.2%) or less; 29% had attended some college, and 9.7% had a college degree or greater. Mean family income was $35,000, with an average of 2.55 children in each household. The unemployment rate was 15%. Social anxiety disorder was the most common primary disorder and the majority of participants had more than one anxiety disorder diagnosis (75%). There were no pre-treatment differences on any demographic or clinical variable across treatment conditions.
Feasibility Related Outcomes
Feasibility related outcomes are based on a sample size of 25 participants; 14 in the TTB group and 11 in the SB group. Of these participants, 13 completed the measures in Spanish and 12 in English.
Overall Feasibility
The overall feasibility of the Cool Kids Program was defined as the ability to complete the study procedures and goals in the proposed time frame. Participants were recruited from each of the three clinics and the majority of referrals came from pediatricians, rather than other allied professionals at the clinic. There was one pediatrician at each of the three clinics; each of the three pediatricians provided referrals. During this RCT, recruitment lasted 13 months; 59 families consented to participate (5 per month), 37 completed the eligibility interviews, and 31 families were randomized (2–3 per month). A significant number of the consented families were “lost to contact” (n = 21) due to disconnected phone numbers, wrong phone numbers, re-location (which was common given that some of our families were seasonal workers), loss of interest, and other unknown reasons which affected overall recruitment rates. The majority of families preferred study materials and telephone contacts in Spanish; 18 parents (58%) preferred study materials in Spanish, 10 parents (32%) preferred English, and 3 (8.6%) had no preference. All youth spoke and read English but were given bilingual workbooks to facilitate understanding of intervention materials by the parents (who may have been Spanish monolinguals). Treatment duration for the TTB group was longer than the expected 3 – 4 months with most participants completing treatment in 5 – 6 months. Specifically, the length of time it took for patients to complete the program was M = 136.7 days (SD = 11.31) (approximately 5 months); range = 103 – 204 days. Table 3 presents mean number of minutes per session and frequency of participants who needed extra sessions for those in the TTB group.
Table 3.
Length of telephone sessions and extra sessions required for those in TTB condition
| Session | Mean Session Length in Minutes | SD | # participants who requested extra contact to complete a session |
|---|---|---|---|
| Session 1: Psychoeducation | 49.00 | 19.81 | 1 |
| Session 2: Setting Goals | 51.50 | 16.20 | 1 |
| Session 3: Feelings | 46.43 | 9.43 | 0 |
| Linking Thoughts and Feelings | |||
| Session 4: Thoughts | 57.0 | 30.50 | 2 |
| Finding evidence for worries | |||
| Session 5: Thoughts and Rewards | 76.33 | 22.47 | 4 |
| Finding evidence for worries and rewards | |||
| Session 6: Exposure | 93.50 | 52.96 | 3 |
| Fear and worries list and stepladders | |||
| Session 7: Exposure | 75.70 | 30.78 | 2 |
| Revising stepladders | |||
| Session 8: Exposure | 57.0 | 24.24 | 1 |
| Stepladders and Problem Solving | |||
| Session 9: Social Skills | 57.25 | 12.55 | 1 |
| Session 10: Consolidation of all Skills | 30.5 | 12.66 | 0 |
| Session 11: Relapse/Future goals | 43.0 | 23.37 | 0 |
The feasibility of the program was also gauged by participants’ report on the Barriers to Treatment Participation Scale (Kazdin et al., 1997). Mean scores on the treatment barriers subscales for the total sample ranged from M = 1.04 to 1.67 (1 = never a problem to 5 = very often a problem), suggesting that barriers ranged from “never a problem” to “occasionally a problem”. The highest mean scores were on the treatment demandingness (M = 1.47) and the stressors and obstacles competing with treatment subscales (M = 1.67). There were no significant differences between the TTB and SB groups on endorsement of barriers (see Table 4).
Table 4.
Mean comparisons between SB and TTB groups on Barriers to Treatment Participation Scale (BTPS) (means (M) and standard deviations (SD)).
| All M (SD) | SB M (SD) | TTB M (SD) | P value | |
|---|---|---|---|---|
| Stressors and Obstacles (that compete with treatment) with | 1.67 (.56) | 1.62 (.55) | 1.72 (.60) | .70 |
| Treatment Demands and Issues | 1.47 (.41) | 1.46 (.40) | 1.49 (.46) | .86 |
| Perceived Relevance of Treatment | 1.15 (.28) | 1.16 (.27) | 1.14 (.31) | .87 |
| Relationship with Therapist | 1.04 (.09) | 1.02 (.05) | 1.07 (.12) | .20 |
SB = self-directed, bibliotherapy; TTB = telephone delivered, therapist-assisted, bibliotherapy
Acceptability
The construct of acceptability was assessed by parents’ reports on the Parent Consumer Satisfaction Scale (March et al., 1999) (range = 1–7), with higher scores reflecting greater satisfaction (e.g., 5 = slightly satisfied, 6 = satisfied, and 7 = very satisfied). The overall parent satisfaction mean for the TTB group was 6.57 (SD = .42), with a range from M = 5.88 to M = 7.00 at post-treatment. The overall mean score for the SB condition was 6.04 (SD = .57), with a range of M = 5.25 to M = 6.63 at post-treatment. Using a one-way ANOVA, families in the TTB condition had higher total satisfaction scores than the SB condition, F = 5.67, p = .028.
Tolerability
Tolerability was defined in two ways: (1) attendance at sessions for TTB participants/completion of modules for SB group, and (2) adherence to treatment procedures for TTB participants. Completion of modules in the SB group was determined by parents report on a summary sheet that was completed at post-treatment indicating how many modules (which aligned with telephone supported sessions) they completed. Parents were asked to reference the workbooks to determine how many modules they completed. Participation in at least 8 out of 11 sessions/completion of 8 out of the 11 modules, within the specified time frame was considered a therapeutic dose of skills. In the TTB group, 10 of 15 parents (66.7%) completed the requisite number of therapist-assisted bibliotherapy sessions, and in the SB group, 4 of 16 parents (25%) completed the requisite number of self-directed bibliotherapy modules X2 = 5.43, p = .02. Alternatively, 33.3 and 75% were non-completers in the TTB and SB groups, respectively. The mean number of sessions completed by those in the TTB condition was 7.93 (SD = 4.17), and the mean number of modules (paralleling TTB sessions) completed by those in the SB condition was 4.12 (SD = 3.92).
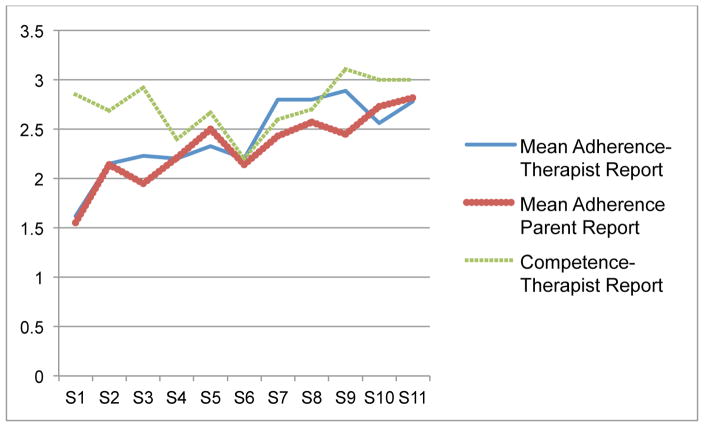
Adherence was only measured for those in the TTB group as this construct was largely based on therapist perception of task completion and mastery of skills. Adherence to the intervention was monitored using the Treatment Adherence Questionnaire (Nock et al., 2007), a 3-item scale which queries both parent and therapist’s report of completion (i.e., adherence) of assigned readings, worksheets and practice tasks, as well as therapist rating of how well the parent implemented the skill (i.e., competence). Adherence ratings ranged from 0–4 (0 = 0%, 1 = 25%, 2 = 50%, 3 = 75%, and 4 = 100%). Competence ratings also ranged from 0–4 (0 = no adherence - 4 = perfect adherence). Mean adherence scores based on therapist and parent report were M = 2.77 (SD = .93), and M = 2.53 (SD = .98), respectively. The mean competence rating, based on therapist report was 2.98 (SD = .87). These ratings are plotted by session in Figure 2, with highest adherence and competence ratings noted during the final sessions of treatment.
Figure 2.
Mean Adherence and Competence Ratings by Session (S). Note on Y axis; Adherence ratings (0 = 0%, 1 = 25%, 2 = 50%, 3 = 75%, and 4 = 100%) and Competence ratings (0 = no adherence - 4 = perfect adherence).
Safety
Safety was defined by the occurrence of serious/adverse events and the worsening of symptoms during the intervention. Serious adverse events were considered life-threatening events, hospitalization, or events leading to major incapacity. Harm-related adverse events were defined as endorsement of active suicidality (active ideation, suicidal plan, self-harm, etc.), disclosure of child abuse, or harm to others, which included aggressive or violent ideation or actions against others. None of the parents reported serious adverse or adverse events in this study or a worsening of symptoms that required referral or discontinuation from the study. While safety is included as a feasibility related outcome, it is important to note that feasibility studies provide limited information regarding safety due to low base rates of serious adverse events and small sample sizes.
Responder Status and Remission Rates
Response rates, defined as remission of all anxiety disorders (i.e., CSR <=3 on all disorders) based on parent and child report on the ADIS (n = 25), were 50% for the TTB group, and 36.4% for the SB group; X2 (1) = .465, p = .50. Response rates, defined as remission of primary anxiety disorder based on parent and child report on the ADIS (n=25), were 61.5% for the TTB group and 36.4% for the SB group; X2 (1) = 1.51, p = .22.
Post exit Interview (Qualitative Feedback)
Participants in both conditions mentioned that it was hard for them to complete the sessions according to the initial schedule due to their busy schedules and time constraints (i.e., having to work, taking care of house chores, school homework). Similarly, participants mentioned that they did not have time to “sit down and read the whole book [workbooks],” and others mentioned they were not good at reading. Participants reported that the material was easy to understand at first, but “it started getting more hard.” A number of parents reported that the audiobook was very helpful and that they listened to it during their commute, or at home with their family. Other participants reported technical difficulties while trying to play the audiobook and DVD: The most common technical difficulty was that participants did not have a CD player or earphones. Several participants reported that face-to-face interaction with their specialist would have been helpful. Barriers unique to the SB self-help group included lack of guidance and difficulty engaging their child (e.g., child not paying attention or completing workbook readings). One participant mentioned that there were times where she felt like the “doctor” when trying to explain the program to her child. Most participants in the SB group mentioned that they did not call their specialist because they did not feel like they needed to do so (i.e., not having any problems with program). Participants in the TTB condition reported that their specialist was “very helpful,” “polite,” and “available.” According to the parents, the specialist explained and clarified the content of the workbooks and provided strategies to facilitate children’s engagement.
Discussion
Findings from the feasibility focused RCT are promising, and suggest that the parent mediated CBT with therapist support by telephone can be feasible, acceptable, tolerable and safe in an underserved rural community, where mental health disparities are prominent. Findings have affirmed that parents in a rural, primarily Spanish speaking community are receptive to parent mediated, bibliotherapy interventions, with many reporting favorable satisfaction ratings, good adherence, and treatment gains, particularly for the telephone delivered, therapist-assisted condition (TTB). However, the feasibility of this study was limited in many ways and modifications were necessary to meet the needs of many families.
While many families agreed to participate in this study, many who initially consented were lost to contact prior to eligibility assessments being completed. Some of the families could not be contacted for practical reasons such as disconnected phone numbers, wrong phone numbers, and re-location (which was common given that some of our families were seasonal workers). Previous research also has suggested that “soft refusals” may account for issues with low rates of initial uptake (Roosa et al., 2008) and this phenomenon may have extended to other phases of a study. Explanations for “soft refusals” are embedded within discussions of cultural values that emphasize interpersonal agreement and respect for authority however additional research is necessary in this regard. The influence of changing perceptions of study/therapy burden, decreasing treatment relevance, and input from social networks have been noted as barriers to initial uptake in previous studies with ethnic minority families (McKay et al., 1996; 1998) and may have also influenced patterns of service uptake in this study.
The length of time it took participants to finish the treatment program was longer than the suggested 3 months reported by the treatment developers, as well as the duration of treatment reported in a previous study of the same intervention with a middle-income, European American sample (Chavira et al., 2014). As suggested on the measure of treatment barriers, and exit interview feedback, this extended length of treatment was related to practical barriers experienced while participating in the program, which often resulted in “no-shows” and rescheduling of appointments. It was also related to the fact that some participants required content from a single session to be distributed over two sessions, resulting in longer session length. This most often occurred in the middle phase of treatment (sessions 5, 6, and 7), when skills such as cognitive restructuring, planning rewards, and exposure were the treatment foci (See Table 3). While these sessions were by far the longest, all sessions were longer than the expected 30–40 minutes, reported in previous studies using the Cool Kids Outreach intervention (Chavira et al., 2014; Lyneham et al., 2006), which raises concerns about the ease of understanding CBT principles for some rural Latino/a families. Difficulties with skill acquisition in evidence based treatments have been noted in other studies with ethnic minority families, specifically Chinese immigrant families (Lau et al., 2011). For example, in a pilot study of parent management training with Chinese immigrants, therapists reported that is was difficult for parents to acquire some of the skills, and suggested that slowing the pace of skill lessons and increasing the dosage of behavioral rehearsal may be useful adaptations for evidence based interventions with immigrant families (Lau et al., 2011). Our pilot study offers further support in this regard, and in general such adaptations (e.g., slowing pace, increased dosage) may be useful to consider when implementing evidence based treatment with less acculturated families.
Tolerability findings in this study, as defined by attendance at sessions (i.e., attrition), and adherence, were somewhat mixed. Attrition rates for child treatment studies vary greatly depending on how the construct is defined; rates of 15–30% are typical in efficacy trials and often extend to 40–50% in community effectiveness trials (de Haan, Boon, de Jong, Hoeve, & Vermeiren, 2013). In the current study, the attrition rate (as defined by completing less than 8 of the required sessions) for the TTB group was 33.3%, which is somewhat consistent with rates from previous community based studies. The attrition/non-completion rate for the SB group status was significantly higher (75%). Further, despite being advised to contact their therapist as necessary when working on the bibliotherapy program with their child, none of the parents in the SB group initiated contact with their therapist. This is in contrast to previous studies using a similar design (Lyneham & Rapee, 2006) where 31% of parents in the self-directed, condition initiated phone calls to their therapist. In general, such contact rates are low and suggest that completely self-directed bibliotherapy, may not be useful for many families.
With regard to adherence, findings suggest an acceptable and steady percentage of participants completed activities (> = 50%) across the 11 sessions with lowest adherence reported at session 6, when exposure activities were introduced, and highest adherence reported near the end of treatment (see Figure 2). With regard to competence, highest ratings were noted at the beginning and end of treatment, and lowest ratings in the middle phase of treatment. This pattern likely reflects the complexity of materials delivered during the Cool Kids Outreach intervention with more basic psychoeducation and review of skills being the core content at beginning and end of treatment, and skills such as cognitive restructuring, exposure, and the use of rewards being introduced in the middle phase of treatment. Correspondingly, the middle sessions also were the longest sessions, and occasionally it was necessary to deliver these sessions across two appointments to facilitate understanding of the materials. As previously suggested, new skills and unfamiliar content, may require a slower pace and greater dosage to facilitate competence, particularly in immigrant and less-acculturated individuals, similar to the rural Latino/a parents in the current study.
Findings from a standardized measure of barriers suggested that “competing stressors and obstacles to treatment” as well as “treatment demandingness” were the most frequently endorsed barriers, and may have contributed to attrition, as well as lower adherence/competence ratings during sessions that required more activities. These findings were further supported by interview feedback at post-treatment, where families in both conditions mentioned that it was hard for them to complete the sessions due to their busy schedules and competing responsibilities (i.e., having to work, taking care of household chores, school homework). Previous studies with Latino/as have noted logistic barriers, patient-provider communication, cultural fit, and attitudinal factors (e.g., stigma) as deterrents of appropriate service utilization (Cabassa, Zayas, & Hansen, 2006; Tarshis, Jutte, & Huffman, 2006). In rural samples, concerns about anonymity, given smaller communities and intertwined social networks, also deter appropriate help seeking (Rost et al., 2002; Smalley et al., 2010).
In the current study, cultural attunements, additions to evidence based interventions that are intended to increase engagement and retention (Falicov et al., 2009), were included to address some of these barriers. Specifically, we included an engagement session at the beginning of treatment to address attitudinal as well as practical barriers such as stigma, concerns about anonymity, lack of time, difficulty scheduling, and homework compliance. While this study did not empirically examine the efficacy of the engagement strategies, it is plausible that these supplemental strategies were better able to address issues of cultural fit and attitudinal barriers than practical barriers such as competing stressors and lack of time. It may also be that our engagement strategies were not intensive enough to achieve the desired goals.
Additional modifications included the creation of media adjuncts such as CD recordings of all the intervention materials and DVDs with video exemplars of the skills, to facilitate learning and reduce emphasis on written materials, which was particularly important in a community context where limited literacy was identified as a potential barrier to treatment. While we were not able to examine the usefulness of these technological adjuncts specifically, qualitative findings suggested that some families found these media adjuncts to be very helpful. In our opinion, we believe it is important for future studies to consider including technological adjuncts such as these to address barriers with literacy and to increase convenience for family with multiple competing stressors. The widespread use of smartphones in low income and low resourced areas may provide additional options in this regard.
Despite these barriers, many parents reported favorable satisfaction ratings for the intervention. Overall, parents reported better satisfaction, as well as higher rates of adherence and completion if they received the TTB condition, compared to the SB condition. These findings are consistent with meta-analytic findings that support the need for self-directed therapies to include some human contact to be maximally effective (Johansson & Andersson, 2014; Spek, Cuijpers, Nyklicek, Riper, Keyzer, & Pop 2007). Further, completely self-directed, bibliotherapy approaches may be considerably less effective in communities where issues of literacy and contextual stressors (e.g., poverty, unemployment, childcare, etc.) are common. At the same time, it is also important to note that satisfaction ratings from families in the SB were somewhat favorable with mean scores ranging from neutral to satisfied. It is possible that families in the SB condition were satisfied with receiving these resources, and with more time, would have been able to more fully utilize the intervention.
Response rates are presented here, however, given the feasibility focus of this study and small sample size, they are not a primary outcome of this trial and should be interpreted with caution. In the current study, remission rates for “all anxiety disorders” (i.e., anxiety free) were 50% and 36% for the TTB and SB groups respectively. Response rates, as defined by “free of their primary anxiety disorder” were higher (61% for TTB and 36% for SB). These remission rates are lower than studies of telephone delivered, parent mediated, bibliotherapy, in other settings (e.g., specialty clinics) where 69–79% of children were without any anxiety disorder diagnosis at post-treatment (Leong et al., 2009; Lyneham & Rapee, 2006). Participants from these previous studies have been mostly middle income, college educated, English speaking, and European American. The TTB remission rate is somewhat consistent with the average remission rate of 56% from efficacy trials (Cartwright-Hatton, Roberts, Chitsabesan, Fothergill, & Harrington, 2004; Ginsburg et al., 2011), and more favorable than previous studies with primary care pediatric patients (Creswell et al., 2010; Thirlwall et al., 2013).
Limitations
This study is limited by its small sample size. As a feasibility study, it did not include a control group or long-term follow-up assessments. Many of the feasibility measures used in this study have not been validated with Latina/os and Spanish speaking parents. Also, much of the information regarding adherence and completion of study materials for parents in the self-directed bibliotherapy condition is based on parent self-report, rather than a combination of parent and therapist report. Further, the focus on anxiety and the use of mental health specialists does not directly address the issue of clinician shortages in rural communities; however, the remote and self-directed options provide potential alternatives to local providers. Important to note, in this study, sample sizes were too small to conduct within group analyses examining the impact of variables such as acculturation and acculturative stress on treatment engagement and clinical outcomes. Further we did not inquire about the parents’ or child’s country of birth or years living in the US. Additionally, this is a sample of rural parents from a low-income, predominantly Spanish speaking community, who self-identified as mostly Mexican/Mexican-American and therefore findings may not generalize to other communities.
Conclusions
To our knowledge, this is the first child anxiety, parent-mediated bibliotherapy intervention to be delivered in a rural Latino/a community, as well as one of the first studies to address the feasibility of innovative modes of treatment delivery including telephone-based/therapist-assisted bibliotherapy, and completely self-directed bibliotherapy for Spanish-speaking families. While the therapist-assisted approach with telephone contacts may not offer the same intensity of gains as traditional, in person treatment, it appears to be a feasible mode of service delivery, with favorable satisfaction ratings, as well as modest treatment gains. The feasibility of the self-directed intervention is more limited. However, given the significant tailoring required to improve the feasibility of this intervention, ongoing research efforts and novel designs are required to develop accessible treatment options for underserved groups in a timely manner. Findings from this study are a first step in developing feasible and ecologically valid interventions for underserved groups from rural communities.
References
- Alegria M, Canino G, Lai S, Ramirez RR, Chavez L, Rusch D, Shrout PE. Understanding caregivers’ help-seeking for Latino children's mental health care use. Medical Care. 2004;42(5):447–455. doi: 10.1097/01.mlr.0000124248.64190.56. [DOI] [PubMed] [Google Scholar]
- Angold A, Erkanli A, Farmer EM, Fairbank JA, Burns BJ, Keeler G, Costello EJ. Psychiatric disorder, impairment, and service use in rural African American and white youth. Archives of General Psychiatry. 2002;59(10):893–901. doi: 10.1001/archpsyc.59.10.893. [DOI] [PubMed] [Google Scholar]
- Barrera M, Castro FG. A heuristic framework for the cultural adaptation of interventions. Clinical Psychology: Science and Practice. 2006;13(4):311–316. [Google Scholar]
- Cabassa LJ, Zayas LH, Hansen MC. Latino adults’ access to mental health care: A review of epidemiological studies. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(3):316–330. doi: 10.1007/s10488-006-0040-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canino G, Shrout PE, Rubio-Stipec M, Bird HR, Bravo M, Ramirez R, Chavez L, Alegria M, Bauermeister JJ, Hohmann A, Ribera J, Garcia P, Martinez-Taboas A. The DSM-IV Rates of Child and Adolescent Disorders in Puerto Rico: Prevalence, Correlates, Service Use, and the Effects of Impairment. Archives of General Psychiatry. 2004;61(1):85–93. doi: 10.1001/archpsyc.61.1.85. [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, Roberts C, Chitsabesan P, Fothergill C, Harrington R. Systematic review of the efficacy of cognitive behaviour therapies for childhood and adolescent anxiety disorders. British Journal of Clinical Psychology. 2004;43(4):421–436. doi: 10.1348/0144665042388928. [DOI] [PubMed] [Google Scholar]
- Chavira DA, Bustos CE, Garcia MS, Ng B, Camacho A. Delivering CBT to rural Latino children with anxiety disorders: a qualitative study. Community Mental Health Journal. 2017;53(1):53–61. doi: 10.1007/s10597-015-9903-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavira DA, Drahota A, Garland AF, Roesch S, Garcia M, Stein MB. Feasibility of two modes of treatment delivery for child anxiety in primary care. Behaviour Research and Therapy. 2014;60:60–66. doi: 10.1016/j.brat.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):588–594. [PubMed] [Google Scholar]
- Chiu AW, McLeod BD, Har K, Wood JJ. Child–therapist alliance and clinical outcomes in cognitive behavioral therapy for child anxiety disorders. Journal of Child Psychology and Psychiatry. 2009;50(6):751–758. doi: 10.1111/j.1469-7610.2008.01996.x. [DOI] [PubMed] [Google Scholar]
- Creswell C, Hentges F, Parkinson M, Sheffield P, Willetts L, Cooper P. Feasibility of guided cognitive behaviour therapy (CBT) self-help for childhood anxiety disorders in primary care. Mental Health in Family Medicine. 2010;7(1):49. [PMC free article] [PubMed] [Google Scholar]
- Cuffe SP, Moore CG, McKeown R. ADHD and health services utilization in the national health interview survey. Journal of Attention Disorders. 2009;12(4):330–340. doi: 10.1177/1087054708323248. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, Arlett C, Groves R. Stress, coping, and behavioural problems among rural and urban adolescents. Journal of Adolescence. 2003;26(5):574–585. doi: 10.1016/s0140-1971(03)00057-5. [DOI] [PubMed] [Google Scholar]
- Falicov CJ. Commentary: on the wisdom and challenges of culturally attuned treatments for Latinos. Family Process. 2009;48(2):292–309. doi: 10.1111/j.1545-5300.2009.01282.x. [DOI] [PubMed] [Google Scholar]
- Farrell S, McKinnon C. Technology and rural mental health. Archives of Psychiatric Nursing. 2003;17(1):20–26. doi: 10.1053/apnu.2003.4. [DOI] [PubMed] [Google Scholar]
- Feil EG, Baggett KM, Davis B, Sheeber L, Landry S, Carta JJ, et al. Expanding the reach of preventive interventions: Development of an Internet-based training for parents of infants. Child Maltreatment. 2008;13(4):334–346. doi: 10.1177/1077559508322446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, Campo JV. Widening Rural-Urban Disparities in Youth Suicides, United States, 1996–2010. JAMA Pediatrics. 2015;169(5):466–473. doi: 10.1001/jamapediatrics.2014.3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox JC, Blank M, Rovnyak VG, Barnett RY. Barriers to help seeking for mental disorders in a rural impoverished population. Community Mental Health Journal. 2001;37(5):421–36. doi: 10.1023/a:1017580013197. [DOI] [PubMed] [Google Scholar]
- Garcia C, Gilchrist L, Vazquez G, Leite A, Raymond N. Urban and Rural Immigrant Latino Youths’ and Adults’ Knowledge and Beliefs about Mental Health Resources. (2011) Journal of Immigrant and Minority Health / Center for Minority Public Health. 2011;13(3):500–509. doi: 10.1007/s10903-010-9389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, Walkup JT, Sherrill J, Coffey KA, Rynn MA, Keeton CP. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. Journal of Consulting and Clinical Psychology. 2011;79(6):806. doi: 10.1037/a0025933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell E, McFeeters J. Children's mental health care: Differences by race/ethnicity in urban/rural areas. Journal of Health Care for the Poor and Underserved. 2008;19(1):237–247. doi: 10.1353/hpu.2008.0008. [DOI] [PubMed] [Google Scholar]
- Health Resources and Services Administration. Mental health and rural America: 1994–2005. Rockville: MD: Author; 2005. [Google Scholar]
- Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Review of Neurotherapeutics. 2012;12(7):861–870. doi: 10.1586/ern.12.63. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Steain BD, Jaycox LH, Wing M, Escudero P, Tu W, Zaragoza C, Fink N. A school-based mental health program for traumatized Latino immigrant children. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(3):311–318. doi: 10.1097/00004583-200303000-00011. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley M, Breton S. Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry. 1997;38(8):1051–1062. doi: 10.1111/j.1469-7610.1997.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Sugarman A. Attrition in the treatment of childhood anxiety disorders. Journal of Consulting and Clinical Psychology. 1997;65(5):883–888. doi: 10.1037//0022-006x.65.5.883. [DOI] [PubMed] [Google Scholar]
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clinical psychology: Science and practice. 2006;13(4):295–310. [Google Scholar]
- Leong J, Cobham VE, De Groot J, McDermott B. Comparing different modes of delivery: A pilot evaluation of a family-focused, cognitive-behavioral intervention for anxiety-disordered children. European Child & Adolescent Psychiatry. 2009;18(4):231–239. doi: 10.1007/s00787-008-0723-7. [DOI] [PubMed] [Google Scholar]
- Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behaviour Research and Therapy. 2006;44(9):1287–1300. doi: 10.1016/j.brat.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Lyneham HJ, Rapee RM. Agreement Between Telephone and In-Person Delivery of a Structured Interview for Anxiety Disorders in Children. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(3):274–282. doi: 10.1097/00004583-200503000-00012. [DOI] [PubMed] [Google Scholar]
- March JS. Unpublished scale developed. Duke University; 1999. Consumer Satisfaction scale. [Google Scholar]
- McCabe K. Factors that predict premature termination among Mexican-American children in outpatient psychotherapy. Journal of Child and Family Studies. 2002;11(3):347–359. [Google Scholar]
- McKay MM, McCadam K, Gonzales JJ. Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal. 1996;32(4):353–361. doi: 10.1007/BF02249453. [DOI] [PubMed] [Google Scholar]
- McKay MM, Stoewe J, McCadam K, Gonzales J. Increasing access to child mental health services for urban children and the caregivers. Health and Social Work. 1998;23(1):9–15. doi: 10.1093/hsw/23.1.9. [DOI] [PubMed] [Google Scholar]
- Myers KM, Valentine JM, Melzer SM. Child and adolescent telepsychiatry: Utilization and satisfaction. Telemedicine and E-Health. 2008;14(2):131–137. doi: 10.1089/tmj.2007.0035. [DOI] [PubMed] [Google Scholar]
- Nanninga M, Jansen DEMC, Kazdin AE, Knorth EJ, Reijneveld SA. Psychometric properties of the barriers to treatment participation Scale–Expectancies. Psychological Assessment. 2016;28(8):898–907. doi: 10.1037/pas0000229. [DOI] [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse. No place to hide: Substance abuse in mid-size cities and rural America. New York: Author; 2000. [Google Scholar]
- Nock MK, Kazdin AE. Randomized controlled trial of a brief intervention for increasing participation in parent management training. Journal of Consulting and Clinical Psychology. 2005;73(5):872–879. doi: 10.1037/0022-006X.73.5.872. [DOI] [PubMed] [Google Scholar]
- Nock MK, Ferriter C, Holmberg E. Parent beliefs about treatment credibility and expectancies for improvement: Assessment and relation to treatment adherence. Journal of Child and Family Studies. 2007;16(1):27–38. [Google Scholar]
- Paul LA, Gray MJ, Elhai JD, Massad PM, Stamm BH. Promotion of Evidence-Based Practices for Child Traumatic Stress in Rural Populations Identification of Barriers and Promising Solutions. Trauma, Violence, & Abuse. 2006;7(4):260–273. doi: 10.1177/1524838006292521. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Abbott R, Jenkins R, Brugha TS, Meltzer H. Urban–rural mental health differences in Great Britain: findings from the National Morbidity Survey. Psychological Medicine. 2000;30(2):269–280. doi: 10.1017/s003329179900183x. [DOI] [PubMed] [Google Scholar]
- Pew Hispanic Center. The new Latino south: The context and consequences of rapid population growth. Washington, DC: 2005a. [Google Scholar]
- Pew Hispanic Center. Hispanics: A people in motion. Washington, DC: 2005b. [Google Scholar]
- Pina AA, Silverman WK. Clinical phenomenology, somatic symptoms, and distress in Hispanic/Latino and European American youths with anxiety disorders. Journal of Clinical Child and Adolescent Psychology. 2004;33(2):227–236. doi: 10.1207/s15374424jccp3302_3. [DOI] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Weems CF, Kurtines WM, Goldman ML. A comparison of completers and noncompleters of exposure-based cognitive and behavioral treatment for phobic and anxiety disorders in youth. Journal of Consulting and Clinical Psychology. 2003;71(4):701–705. doi: 10.1037/0022-006x.71.4.701. [DOI] [PubMed] [Google Scholar]
- Pina AA, Zerr AA, Villalta IK, Gonzales NA. Indicated prevention and early intervention for childhood anxiety: A randomized trial with Caucasian and Hispanic/Latino youth. Journal of Consulting and Clinical Psychology. 2012;80(5):940. doi: 10.1037/a0029460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Pina AA, Viswesvaran C. Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):105–130. doi: 10.1080/15374410701817907. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Spence SH, Cobham V, Wignall A. Helping Your Anxious Child: A Step-by-Step Guide. 1. Oakland, CA: New Harbinger Publications; 2000. [Google Scholar]
- Rapee RM, Abbott MJ, Lyneham HJ. Bibliotherapy for children with anxiety disorders using written materials for parents: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74(3):436–44. doi: 10.1037/0022-006X.74.3.436. [DOI] [PubMed] [Google Scholar]
- Rapee R, Wignall A, Spence S, Lyneham H, Cobham V. Helping your anxious child: A step-by-step guide for parent. 2. Oakland, CA: New Harbinger Publications; 2008. [Google Scholar]
- Ratcliffe M, Burd C, Holder K, Fields A. Defining Rural at the US Census Bureau, ACSGEO-1. U.S. Census Bureau; Washington, DC: 2016. [Google Scholar]
- Roosa MW, Liu FF, Torres M, Gonzales NA, Knight GP, Saenz D. Sampling and recruitment in studies of cultural influences on adjustment: A case study with Mexican Americans. Journal of Family Psychology. 2008;22(2):293–302. doi: 10.1037/0893-3200.22.2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rost K, Smith GR, Taylor JL. Rural-Urban Differences in Stigma and the Use of Care for Depressive Disorders. The Journal of Rural Health. 1993;9(1):57–62. doi: 10.1111/j.1748-0361.1993.tb00495.x. [DOI] [PubMed] [Google Scholar]
- Rost K, Fortney J, Fischer E, Smith J. Use, quality, and outcomes of care for mental health: The rural perspective. Medical Care and Review. 2002;59(3):231–265. doi: 10.1177/1077558702059003001. [DOI] [PubMed] [Google Scholar]
- Shore JH, Brooks E, Savin DM, Manson SM, Libby AM. An economic evaluation of telehealth data collection with rural populations. Psychiatric Services. 2007;58(6):830–835. doi: 10.1176/ps.2007.58.6.830. [DOI] [PubMed] [Google Scholar]
- Silverman W, Albano AM. Anxiety Disorders Interview Schedule for Children Using DSM-IV. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Smalley KB, Yancey CT, Warren JC, Naufel K, Ryan R, Pugh JL. Rural mental health and psychological treatment: a review for practitioners. Journal of Clinical Psychology. 2010;66(5):479–489. doi: 10.1002/jclp.20688. [DOI] [PubMed] [Google Scholar]
- Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychological Medicine. 2007;37(3):319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Summary of findings from the 2001 National Household Survey on Drug Abuse. Rockville, MD: Office of Applied Studies; 2001. [Google Scholar]
- Tarshis TP, Jutte DP, Huffman LC. Provider recognition of psychosocial problems in low-income Latino children. Journal of Health Care for the Poor and Underserved. 2006;17(2):342–357. doi: 10.1353/hpu.2006.0070. [DOI] [PubMed] [Google Scholar]
- Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C. Treatment of child anxiety disorders via guided parent-delivered cognitive-behavioural therapy: randomised controlled trial. The British Journal of Psychiatry. 2013;203(6):436–444. doi: 10.1192/bjp.bp.113.126698. [DOI] [PubMed] [Google Scholar]
- U. S. Congress. Office of Technology Assessment, Healthcare in rural America (OTA-H-434) Washington, DC: 1990. [Google Scholar]
- Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J. Anxiety reporting and culturally associated interpretation biases and cognitive schemas: A comparison of Mexican, Mexican American, and European American families. Journal of Clinical Child and Adolescent Psychology. 2004;33(2):237–247. doi: 10.1207/s15374424jccp3302_4. [DOI] [PubMed] [Google Scholar]
- Weems CF, Hayward C, Killen J, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. Journal of Abnormal Psychology. 2002;111(3):471–417. [PubMed] [Google Scholar]
- Yeh M, McCabe K, Hough RL, Dupuis D, Hazen A. Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Mental Health Services Research. 2003;5(2):65–77. doi: 10.1023/a:1023286210205. [DOI] [PubMed] [Google Scholar]
- Yellowlees PM, Hilty DM, Marks SL, Neufield J, Bourgeois J. A retrospective analysis of a child and adolescent eMental health program. Journal of American Academy of Child and Adolescent Psychiatry. 2008;47:103–107. doi: 10.1097/chi.0b013e31815a56a7. [DOI] [PubMed] [Google Scholar]