Abstract
Significant changes in body composition are known to occur with aging. The aim of the present study was to provide a normative reference of body composition and to investigate age and sex-related differences in healthy subjects by multifrequency bioelectrical impedance analyzer (BIA).
A cross-sectional study was conducted on a sample of 3451 healthy Chinese adults, 1611 males and 1840 females. The volunteers were enrolled in 5 different age bands (18–30, 31–40, 41–50, 51–60, 60+). All subjects were measured for weight and height and submitted to BIA, to determine body composition. Body composition measures accounted for differences between men and women.
A decrease in fat-free mass and increase in percent body fat was observed with aging, although the phenomenon was proved to be attenuated in women. The central and visceral redistribution of fat mass was also shown along lifetime.
This study is a report on body composition of healthy subjects, to be used as an important data for future investigations and differences between nationalities and countries.
Keywords: body composition, fat mass, fat-free mass, healthy adults, reference
1. Introduction
Body composition is a key component of an individual's health and physical fitness profile that can been influenced by environmental (social and cultural), genetic, and ethnicities as well as age and sex.[1] As shown in several studies, the importance of body composition has grown rapidly in the last few years.[2] The clinical significance of reference data of body composition includes several aspects such as understanding of changes in body composition by increasing age and nutritional status according to underweight and obesity conditions within a population.
Fat mass (FM) and fat-free mass (FFM) were considered as important indicators for evaluating nutritional status in clinical practice. In some chronic conditions, body mass index (BMI) and the percentage of weight loss do not provide any insight about the respective contributions of FFM and FM in the body mass changes.[1] The assessment of body composition changes with aging can be helpful for establishing optimal weight for health status and physical performance.[3,4] Obesity and sarcopenia are health problems associated with aging. In the analysis performed by Kyle and colleagues, Mean FM and FM% increased progressively in men and women throughout the ages studied and the higher weight noted in older subjects is due to higher FM.[5] High body fat has been shown to be associated with poorer physical performance in older adults,[6] and fat accumulation within skeletal muscle is associated with muscle weakness[7] and poor function.[8] A study conducted in the West reported that overnutrition, particularly obesity (BMI ≥ 30 kg/m2), was associated with frailty.[9] In addition, overnutrition is directly related to living habits and leads to lifestyle diseases, such as obesity, diabetes mellitus, dyslipidemia, and hypertension.[10]
Although some previous studies of “healthy” people have examined and analyzed age- and sex-dependent changes in body composition, the overwhelming majority samples used to define the changes in body composition were restricted to obese populations,[11] or specific age ranges, such as older individuals,[12] athletes and children,[13,14] few have focused their attention on the “healthy” body composition of the general population across the adult age range. Nevertheless, health standards derived from one population with a specific sex—and age—may not be applicable to the general population due to differentials of body composition, just as standards from adults in one country may not be applicable in other countries. Thus, data should be obtained by country and within countries, from different age and ethnic groups and for men and women separately. In addition, values of body composition of healthy people coming from different ethnicity all over the world will provide special insight into the prevalence of diseases and risks for health.
Thus, the aims of study were to evaluate body composition changes occurring with aging and obtain the reference values for body composition parameters using BIA. In addition, these body composition ranges can be used to provide important data on body composition in healthy Han adults from Shaanxi Province and to investigate age and gender-related differences, while building a normative reference database of body composition on national basis.
2. Methods
2.1. Ethics committee statement
This cross-sectional study was performed in compliance with the principles of the Declaration of Helsinki of the World Medical Association and obtained the permission from the Ethics Committee of Xizang Minzu University and Northwest University. All of the participants were informed of the cross-sectional study, and informed consent was taken from each participant.
2.2. Study design and participants
Healthy Han adults (1840 women and 1611 men), aged 18 to 82 years old, were recruited randomly from Shaanxi Province through a health management center, Kang Cheng Jun Jian International Health City. The participants were informed about the nature of study, procedure, and usefulness of the study to our country. All subjects were living independently and had no known pathologies or physical handicaps. The inclusion criteria were fitness for blood donation. Subjects with acute diseases, severe liver, heart, or kidney dysfunctions cancer or other conditions capable of altering body composition were not recruited. The use of certain drugs (steroids and diuretics) was also a reason for exclusion. Furthermore, pregnant women and subjects with surgical hardware, implantable devices were excluded from the study.
2.3. Assessment of body composition
Body composition parameters were examined by using a multifrequency bioelectrical impedance analyzer (MC-980A; Tanita, Tokyo, Japan). The BIA instrument used six electrical frequencies (1, 5, 50, 250, 500, and 1000 kHz). The surface of the hand electrode was placed in contact with each of the 5 fingers, while the heels and forefoot of the participant were placed on the circular-shaped foot electrode. The participants held out their arms and legs to avoid contact with any other body segments during the measurements. The BIA assessment was performed between 10:00 AM and 4:00 PM. The participants were required to fast and avoid vigorous exercise for at least 1 hour before BIA assessment. The measurements were recorded by well-trained staff and completed within 30 seconds.
Height and weight were measured barefoot, with participants wearing underwear and a cloth gown, to the nearest 0.1 cm and 0.1 kg, respectively, using a mechanical balance with altimeter (Seca 711, Seca GmBH & Co Kg, Germany). BMI was calculated by dividing the body weight (kg) by the square of body height (m2).
2.4. Statistical analysis
All data were tested for normal distribution and are presented as continuously distributed variables with means and standard deviations (SD). ANOVA was used to test for differences between age groups. Student's t-test and chi-square test were used to compare differences in measurements between the sexes. The analysis was performed separately in men and women. All statistical analyses were performed with SPSS 15.0. Generally, a P value <.05 was used to denote statistical significance in tests.
3. Results
The participants were separated into 5 groups (18–30, 31–40, 41–50, 51–60 and 60+). Due to the large amount of information available from the collected measurements, results are better displayed in tables. The anthropometric and body composition characteristics of the study participants are reported in Table 1 stratified by sex. Mean values and standard deviations were calculated for body composition by sex and age group (Table 2 and Table 3). The age- and sex-specific percentile distributions for fat mass (FM), percent body fat (PBF), and fat-free mass (FFM) of the subjects are given in Figures 1–3.
Table 1.
Descriptive statistics for all observations of men and women.
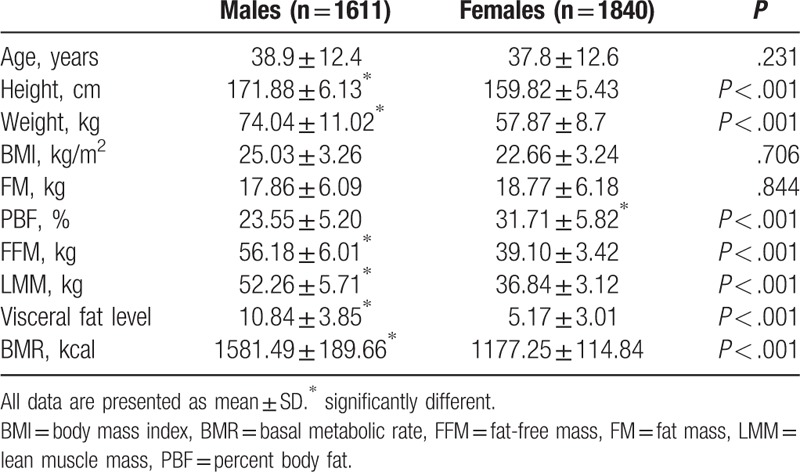
Table 2.
Body composition changes with age in healthy men.
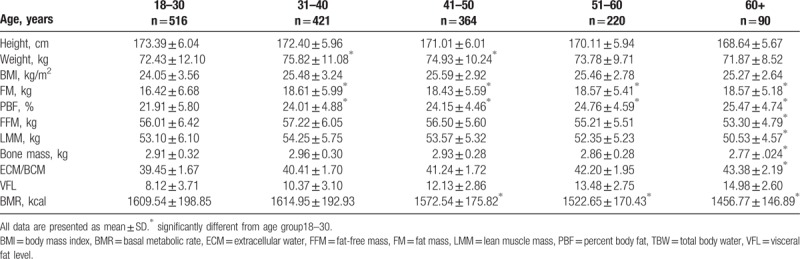
Table 3.
Body composition changes with age in healthy women.
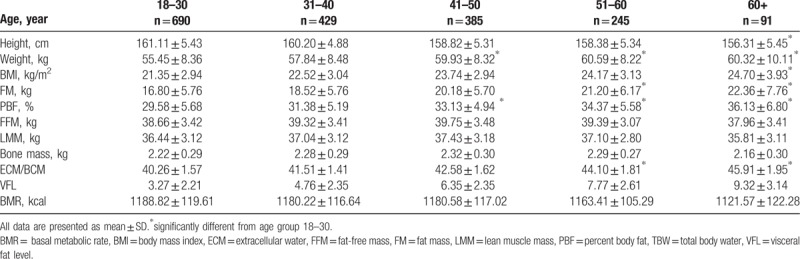
Figure 1.
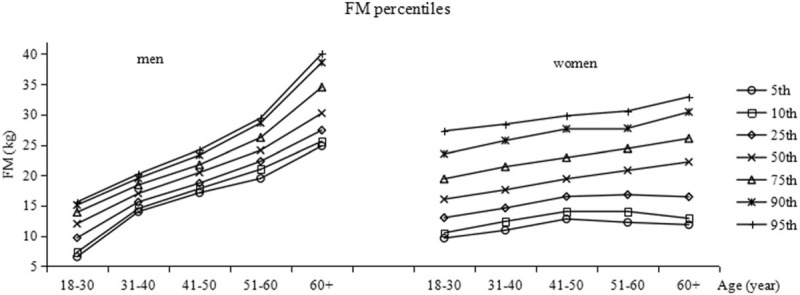
Fat mass (FM) percentile curves by age group in the 2 genders. FM = fat mass.
Figure 3.
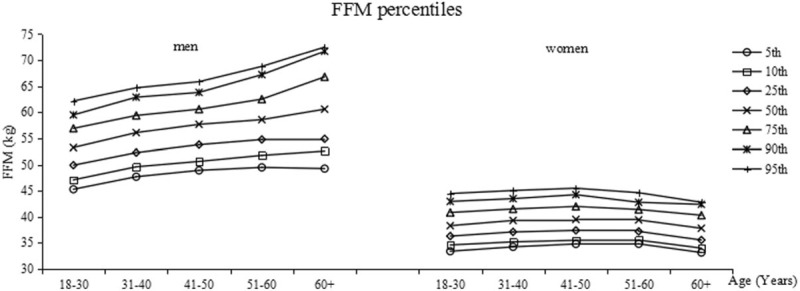
Fat-free mass (FFM) percentile curves by age group in the 2 genders. FFM = fat-free mass.
For men, mean age was 38.9 ± 12.4 years and for women 37.8 ± 12.6 years. In this sample of Han adults, body weight, FFM and lean muscle mass (LMM) were higher in men as expect. Although there was no significant difference in FM between males and females, PBF was higher in females. In addition, no statistically significant difference in BMI was found between men and women. However, the prevalence of overweight (BMI, 25.0–29.9 kg/m2) and obesity (BMI ≥ 30 kg/m2) were 43.70 and 6.62 in males, significant high than 18.81 and 2.73 in females (data were not shown). Visceral fat level and basal metabolic rate (BMR) were higher in males as well.
In both genders, mean height were lower in the oldest age groups compared with the youngest, but there was no significant difference. Weight rose from 18–30 till the 31–40 age brackets, while it dropped in the 41 to 50 years old in men, while it constantly increased in women. In men, there was no significant difference in mean BMI. In women, the BMI ranged from 21.35 ± 2.94 to 24.70 ± 3.93 kg/m2, although a comparison between the different age groups showed that only the 60+ years old differed significantly from the previous age bracket.
In men, FM and PBF rose significantly from the 18–30 to the 31–40 age bracket, then remained without any significant change in the later age group (Table 2). The reference range (25–75th percentile) of FM in men was 9.68–13.9 in the 18–30 age group and 27.4–34.5 for the 60+ age group (Fig. 1). The reference values of PBF in men were 17.9–25.8 in the 18–30 age group and 22.2–30.5 for the 60+ age group (Fig. 2). In women, total FM and PBF constantly increased from the youth to the older age. The reference values of FM for the 18 to 31 age group were 13–19.4 and for the 60+ age group they were 16.5–26.1 (Fig. 1). The reference values of PBF for the youngest age group were 26–33 and 31.5–40.2 for the oldest (Fig. 2). However, PBF was significantly higher in females than males in all groups. Figures 1 and 2 show the trends of the FM and PBF percentiles by age group for the 2 genders, respectively.
Figure 2.
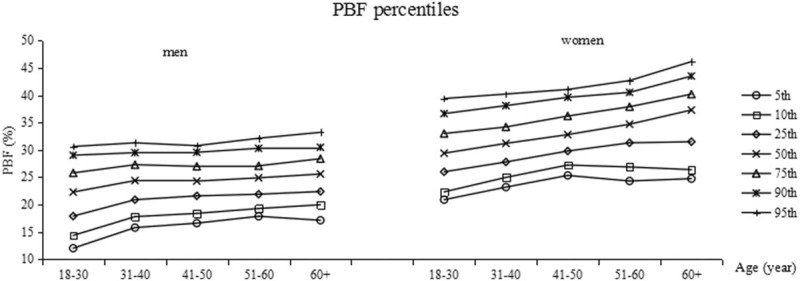
Percent body fat (PBF) percentile curves by age group in the 2 genders. PBF = percent body fat.
Mean FFM was greatest in men 31 to 40 year old and decreased thereafter. It was significantly lower in men older than 60 years compared with other groups. The reference values for the youngest age group were 49.9–56.9 and 54.9–66.8 for the oldest (Fig. 3). For women, the mean FFM was greatest between 41 and 50 year old and decreased thereafter. FFM increased slightly but not significantly in women younger than 30 year old compared with women 31 to 40 y, and decreased slightly in women older than 50 years. The reference range for all subjects was 36.7–41.3 and was much the same in all age groups (Fig. 3).
In women, both LMM and bone mass did not change statistically significantly over the age groups, whereas LMM and bone mass became lower with higher age groups in the male subjects. In males, the 80+ age category had a significantly higher ECW/TBW than all other age categories. For females, significant higher ECW/TBW was observed in the 51–60 and 60+ age categories. Mean VFL was higher in males than in females in all age groups and it was higher with increasing age for both sexes. In men and women, BMR was lower in the oldest age group (60+ years) compared with the youngest. However, when BMR in women of all age was analyzed, there was no difference between the age groups, whereas BMR in men old than 40 years of age was significantly lower compared with the younger.
4. Discussion
This study presents summary values for body composition and anthropometric measurements in a sample of healthy Han adults in Shaanxi province aged 18 y and older. The usefulness of reference data on body composition is that reference samples obtained could be extrapolated to the total population and used for comparison and assessment of adults in other local samples. In addition, it can be compared with samples in other countries with similar social and economic conditions or with similar background.
The assessment of body composition changes with aging is essential in clinical practice as such variations are related to health status and physical function. BMI is frequently used in nutritional and epidemiological studies as a most common indicator of body composition for evaluating body fat and patterns of nutritional status.[15] BMI appears to be a relatively poor predictor of cardiometabolic risk among Taiwanese adults even when applying Asian-specific thresholds.[16] Thus, it has proved an inaccurate measure of fatness and a less reliable indicator to evaluate changes in adiposity in older adults[17] because it is affected by both reduction in height and increase in fat. In the healthy population of this study BMI did not change with aging in both males and females. A limitation of using BMI to evaluate body composition is that changes can be due to either fat mass or fat-free mass.
An increasing prevalence of overweight and obesity has been observed in the general population in recent decades.[18] In cross-sectional analyses of European Adult Cohort Populations, the authors also observed a strong increase in obesity prevalence with increasing age, especially among women between the ages of 30 to 65 y.[19] According to our study, associated with age, there is an increase in total fat tissue only in women, while a significant increase in PBF in both sexes. FFM, and specifically muscle mass in men, is generally considered to decrease throughout adult life[20] seemed mainly due to limited ability to carry out routine daily activities. Our findings confirmed an earlier Aerobics Center Longitudinal Study (ACLS) in healthy men that showed an age-dependent decrease in FFM and an increase in PBF.[21] Sarcopenic obesity, a new category of obesity, is characterized by increased FM and reduced FFM with a normal or high body weight.[22] It has been reported that sarcopenic obesity is significantly associated with functional decline and disability,[12] as well as higher levels of cardiovascular risk factors and an increased risk of mortality in general population.[23] In other words, reduced muscle mass is associated with increased physical disability,[24] especially mobility. On the other hand, accumulation fat mass appears to worsen functional disability and physical performance in older adults.[25]
It has been shown that aging is associated with body fat distribution changes, i.e. visceral fat increase, in healthy elderly women.[26] Body fat distribution has been reported to differentially contribute to the development of cardiovascular risk.[27] Abdominal adipose tissue is the best indicator for predicting insulin resistance and other relevant cardiovascular risk factors.[28] Thus it is important to study changes in central fat distribution. Visceral fat level increased since 40 y in both men and women in our study. As in a Chinese population-based study, intra-abdominal fat increased in old men and women with stable weight.[29] Furthermore, central adiposity appears to contribute to a greater extent than general adiposity to the development of cardiovascular risk.[30] Other studies demonstrated that excessive visceral fat rather than obesity per se is related to an increased risk of hypertension[31] and diabetes.[32]
It has been reported that trends toward age-related declines in BMR differ between men and women;[33] our findings supported this (Table 2 and 3). Keys et al.[34] have concluded that BMR decreases by no more than 1% to 2% per decade over the age range from 20 to 75 y and that the rate of decrease is particularly rapid for men. It is assumed that this putative reduction in BMR is a result of the loss of fat free mass, as well as change in cellular metabolic that accompanies aging.[35] In a study of older adults living in a snowy region of Japan, the decrease in BMR stratified by age was significant for both men and women.[36] Contrary to what we had expected based on previous studies, a significant decline in BMR in men was observed in their 40 s and for women in their 50s. This finding is confirmed by a previous study[37] but the causes of these decreases have not been fully explained.
A reduction of the water compartment of the organism or an abnormal accumulation of fluid in the interstitium has been described as being associated with difficulties in maintaining fluid balance.[38] Physiologically, about two-thirds of the total body water of humans is held in the cells, mostly in the cytosol, and the remainder is found in the extracellular compartment. The results of the body composition analysis of the healthy adults indicate that ECW/TBW increased significantly with age for both females (39.45%–43.38%, P < .05) and males (40.26% –45.91%, P < .05), and that this change was greater in men than in women. Similar results have been shown by other studies,[39] which have pointed to ECW/TBW as important biomarkers for diagnosing the state of hydration and nutrition status. Thus, elderly persons are at the highest risk for developing malnutrition and dehydration.
In conclusion, despite the limited recruited volunteers, this is a study on the body composition status of healthy Han adults in Shannxi Province, to be used as an important reference for future investigation and clinical practice on differences between nationalities and countries.
Acknowledgments
The authors acknowledge all participants involved in the study, as well as ZL, XT and LZ for their help in the organization of participant enrollment. XH and TJ were responsible for the study concept and design. ZL, XT, LZ, and XH acquired the data used in the study. All authors were involved in the analysis and interpretation of the data. XH, DY, and TJ drafted the manuscript. All the authors provided critical revision of the manuscript for important intellectual content. DY and TJ supervised the study.
Author contributions
Conceptualization: Dongya Yuan, Tianbo Jin.
Data curation: Zishuai Li, Xunhui Tang, Xue He.
Formal analysis: Lijun Zhang.
Funding acquisition: Tianbo Jin.
Investigation: Zishuai Li.
Methodology: Li Wang, Yongjun He, Dongya Yuan.
Resources: Xunhui Tang.
Software: Yongjun He, Xue He.
Supervision: Lijun Zhang.
Validation: Li Wang, Yongjun He.
Visualization: Li Wang.
Writing – original draft: Xue He.
Writing – review & editing: Dongya Yuan, Tianbo Jin.
Footnotes
Abbreviations: BIA = multifrequency bioelectrical impedance analyser, BMI = body mass index, BMR = basal metabolic rate, ECM = extracellular water, FFM = fat-free mass, FM = fat mass, LMM = lean muscle mass, PBF = percent body fat, TBW = total body water, VFL = visceral fat level.
Funding: This work was supported by Innovation Support Program for College Young Teachers Projects of Xizang (Tibet) Autonomous Region [grant number: QCZ2016-38], and the Natural Science Foundation of Xizang (Tibet) Autonomous Region [grant number: 2016ZR-MY-02].
The authors have no conflicts of interest to disclose.
References
- [1].Thibault R, Genton L, Pichard C. Body composition: why, when and for who? Clin Nutr 2012;31:435–47. [DOI] [PubMed] [Google Scholar]
- [2].Muller MJ, Bosy-Westphal A, Later W, et al. Functional body composition: insights into the regulation of energy metabolism and some clinical applications. Eur J Clin Nutr 2009;63:1045–56. [DOI] [PubMed] [Google Scholar]
- [3].Genton L, Karsegard VL, Chevalley T, et al. Body composition changes over 9 years in healthy elderly subjects and impact of physical activity. Clin Nutr 2011;30:436–42. [DOI] [PubMed] [Google Scholar]
- [4].Guo S, Zeller C, Wc, et al. Aging, body composition, and lifestyle: the Fels Longitudinal Study. Am J Clin Nutr 1999;70:405. [DOI] [PubMed] [Google Scholar]
- [5].Kyle UG, Genton L, Slosman DO, et al. Fat-free and fat mass percentiles in 5225 healthy subjects aged 15 to 98 years. Nutrition 2001;17:534–41. [DOI] [PubMed] [Google Scholar]
- [6].Stefano FD, Zambon S, Giacometti L, et al. Obesity, muscular strength, muscle composition and physical performance in an elderly population. J Nutr Health Aging 2015;19:785. [DOI] [PubMed] [Google Scholar]
- [7].Tseng LA, Delmonico MJ, Visser M, et al. Body composition explains sex differential in physical performance among older adults. J Gerontol A Biol Sci Med Sci 2014;69:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Visser M, Kritchevsky SB, Goodpaster BH, et al. Leg muscle mass and composition in relation to lower extremity performance in men and women aged 70 to 79: The Health, Aging and Body Composition Study. J Am Geriatr Soc 2002;50:897–904. [DOI] [PubMed] [Google Scholar]
- [9].Hajek A, Brettschneider C, Posselt T, et al. Predictors of frailty in old age–results of a longitudinal study. J Nutr Health Aging 2016;20:952. [DOI] [PubMed] [Google Scholar]
- [10].Hozawa A, Okamura T, Oki I, et al. Relationship between BMI and all-cause mortality in Japan: NIPPON DATA80. Obesity (Silver Spring) 2008;16:1714–7. [DOI] [PubMed] [Google Scholar]
- [11].Poggiogalle E, Migliaccio S, Lenzi A, et al. Treatment of body composition changes in obese and overweight older adults: insight into the phenotype of sarcopenic obesity. Endocrine 2014;47:699–716. [DOI] [PubMed] [Google Scholar]
- [12].Makizako H, Shimada H, Doi T, et al. Age-dependent changes in physical performance and body composition in community-dwelling Japanese older adults. J Cachexia Sarcopenia Muscle 2017;8:607–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Nikolaidis PT, Busko K, Clemente FM, et al. Age- and sex-related differences in the anthropometry and neuromuscular fitness of competitive taekwondo athletes. Open Access J Sports Med 2016;7:177–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Staiano AE, Broyles ST, Gupta AK, et al. Ethnic and sex differences in visceral, subcutaneous, and total body fat in children and adolescents. Obesity (Silver Spring) 2013;21:1251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].JuneStevens Impact of age on associations between weight and mortality. Nutr Rev 2000;58:129–37. [DOI] [PubMed] [Google Scholar]
- [16].Baniyash M, Sade-Feldman M, Kanterman J. Chronic inflammation and cancer: Suppressing the suppressors. Cancer Immunol Immunother 2014;63:11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 2012;13:275–86. [DOI] [PubMed] [Google Scholar]
- [18].Hajek A, Lehnert T, Ernst A, et al. Prevalence and determinants of overweight and obesity in old age in Germany. BMC Geriatr 2015;15:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].von Ruesten A, Steffen A, Floegel A, et al. Trend in obesity prevalence in European adult cohort populations during follow-up since 1996 and their predictions to 2015. PLoS One 2011;6:e27455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Buffa R, Floris GU, Putzu PF, et al. Body composition variations in aeging. Collegium Antropologicum 2011;35:259. [PubMed] [Google Scholar]
- [21].Jackson AS, Janssen I, Sui X, et al. Longitudinal changes in body composition associated with healthy aeging: men, aged 20-96 years. Br J Nutr 2012;107:1085–91. [DOI] [PubMed] [Google Scholar]
- [22].Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci 2000;904:437–48. [DOI] [PubMed] [Google Scholar]
- [23].Wannamethee SG, Atkins JL. Muscle loss and obesity: the health implications of sarcopenia and sarcopenic obesity. Proc Nutr Soc 2015;74:405–12. [DOI] [PubMed] [Google Scholar]
- [24].Reid KF, Naumova EN, Carabello RJ, et al. Lower extremity muscle mass predicts functional performance in mobility-limited elders. J Nutr Health Aging 2008;12:493–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Shin H, Panton LB, Dutton GR, et al. Relationship of physical performance with body composition and bone mineral density in individuals over 60 years of age: a systematic review. J Aging Res 2011;2011:191896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Fantin F, Rossi AP, Cazzadori M, et al. Central and peripheral fat and subclinical vascular damage in older women. Age Ageing 2013;42:359. [DOI] [PubMed] [Google Scholar]
- [27].Rhéaume C, Arsenault BJ, Després JP, et al. Impact of abdominal obesity and systemic hypertension on risk of coronary heart disease in men and women: the EPIC-Norfolk Population Study. J Hypertens 2014;32:2224. [DOI] [PubMed] [Google Scholar]
- [28].Paradisi G, Smith L, Burtner C, et al. Dual energy X-ray absorptiometry assessment of fat mass distribution and its association with the insulin resistance syndrome. Diabetes Care 1999;22:1310. [DOI] [PubMed] [Google Scholar]
- [29].Thomas GN, Ho SY, Lam KS, et al. Impact of obesity and body fat distribution on cardiovascular risk factors in Hong Kong Chinese. Obes Res 2004;12:1805–13. [DOI] [PubMed] [Google Scholar]
- [30].Lee CC, Glickman SG, Dengel DR, et al. Abdominal adiposity assessed by dual energy X-ray absorptiometry provides a sex-independent predictor of insulin sensitivity in older adults. J Gerontol 2005;60:872. [DOI] [PubMed] [Google Scholar]
- [31].Lukich A, Gavish D, Shargorodsky M. Normal weight diabetic patients versus obese diabetics: relation of overall and abdominal adiposity to vascular health. Cardiovasc Diabetol 2014;13:141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Meisinger C, Döring A, Thorand B, et al. Body fat distribution and risk of type 2 diabetes in the general population: are there differences between men and women? The MONICA/KORA Augsburg cohort study. Am J Clin Nutr 2006;84:483–9. [DOI] [PubMed] [Google Scholar]
- [33].Careau V. Energy intake, basal metabolic rate, and within-individual trade-offs in men and women training for a half marathon: a reanalysis. Physiol Biochem Zool 2017;90:392. [DOI] [PubMed] [Google Scholar]
- [34].Keys A, Taylor HL, Grande F. Basal metabolism and age of adult man. Metabolism 1973;22:579–87. [DOI] [PubMed] [Google Scholar]
- [35].Henry CJK, Schürch B, Scrimshaw NS. Mechanisms of changes in basal metabolism during aeging. Eur J Clin Nutr 2000;54(suppl 3):S77. [DOI] [PubMed] [Google Scholar]
- [36].Shimoda T, Suzuki T, Takahashi N, et al. Nutritional status and body composition of independently living older adults in a snowy region of Japan. Gerontol Geriatr Med 2017;3:2333721417706854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Volpi E, Mittendorfer B, Rasmussen BB, et al. The response of muscle protein anabolism to combined hyperaminoacidemia and glucose-induced hyperinsulinemia is impaired in the elderly. J Clin Endocrinol Metab 2000;85:4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Avantaggiato A, Bertuzzi G, Pascali M, et al. The theories of aging: reactive oxygen species and what else? J Biol Regul Homeost Agents 2015;29(3 suppl 1):156. [PubMed] [Google Scholar]
- [39].Malczyk E, Dziegielewska-Gesiak S, Fatyga E, et al. Body composition in healthy older persons: role of the ratio of extracellular/total body water. J Biol Regul Homeost Agents 2016;30:767–72. [PubMed] [Google Scholar]


