Abstract
Minor physical anomalies (MPAs) are associated with disruptions of fetal development. We propose that the same genetic compositions that contribute to the presence of MPAs, also predispose individuals to health-compromising behaviors, thus considering MPAs as particular endophenotypes.
We developed a screening questionnaire for problematic conduct, substance abuse, and early sexual practice. A total of 108 adolescents (55 males, 50.9%) aged 11 to 19 years were recruited and further divided into case and control groups according to their answers to the questions of health behaviors mentioned above. We then measured their MPAs that included qualitative and quantitative physical features. Stepwise logistic regression and the receiver operating characteristic (ROC) analyses were used to determine the predictive values of MPAs for behavioral outcomes.
The obliquity of palpebral fissure and the head MPAs were negatively associated with substance use. In the ROC analysis, the model provided an area under curve (AUC) of 0.91 with prediction indices being 0.89 for sensitivity and 0.85 for specificity. In addition, the feet MPAs and outer canthal distance were positively, whereas the obliquity of palpebral fissure and ear rotation was negatively associated with early sexual practices. The AUC for early sexual practice was 0.91 and the prediction indexes were 0.87 for sensitivity and 0.88 for specificity.
Certain MPAs were associated with adolescent substance use and early sex, which suggests a neurodevelopmental etiology for behavioral outcomes
Keywords: adolescent, endophenotype, minor physical anomalies, sexual behavior, substance use
1. Introduction
Adolescence is a unique transitional period that one experiences immense physiological, psychological, and contextual changes in the development course. Contextual influences may interact with personal characteristics to exert differential effects on adolescent health behaviors which may persist through adulthood and determine the overall well-being.[1,2] Another common observation worthy of interest is that risk-taking behaviors, such as substance use, dangerous driving, and delinquent violence, are prevalent among adolescents seeking novelty and experimentation in the socialization process.[3] These behavioral problems may belong to a part of the normal growth trajectory. On the other hand, their vulnerability toward impulsiveness and emotional turbulence can be attributed to subclinical manifestations of certain psychiatric abnormalities. For example, adolescents with attention deficit and hyperactive disorder have a higher tendency toward cigarette smoking, alcohol drinking, and drug abuse.[4,5] From the neurodevelopmental perspective, a biological mechanism may underlie the link between adolescent behaviors and maturation of neurophysiological functioning.[6]
Minor physical anomalies (MPAs) are subtle phenogenetic defects arising from fetal organogenesis but may change along with childhood development until pubertal maturation.[1] Accumulating evidence supports the association between MPAs and an array of neuropsychiatric disorders, such as epilepsy,[7] autism,[8] hyperactivity and attention deficit disorder,[9] schizophrenia,[10] and mental retardation.[9] Some studies also demonstrated an important link between MPAs and behavioral or emotional problems in children without an identifiable syndrome.[2,11–13] However, inconsistent measurement data of MPAs describing the magnitude and region involved in case-control differences presents a problem in diagnostic, prognostic, or epidemiological research. The causes include raters’ inconsistency, ethnic and genetic heterogeneities, or chronological evolutions of the clinical symptoms.[14] There are several studies supportive of a strong correlation between certain craniofacial features and psychotic conditions.[15,16]. Recent meta-analyses also demonstrated the importance of MPAs in the identification of neurodevelopmental disorders.[17,18] Further research should include a larger sample size to validate the most salient phenotypic features so that the genetic association with developmental disorders could be better clarified.
There was limited research discerning the relationship between MPAs and adolescent health-compromising behaviors. In a cohort of French Canadian adolescents, Arseneault et al[19] reported that boys with higher counts of anomalies, and especially with anomalies of the mouth, were found to be at higher risk for violent delinquency. Their recruitment was restricted to low socioeconomic status neighborhoods within a Caucasian population. Beside ethnic differences in the appearance and frequency of MPAs, extrapolation of the findings to a different cultural context also needs cross-cultural validation. The aim of this study is to investigate the role of MPAs as neurodevelopmental endophenotypes of adolescent health-compromising behaviors among Taiwanese youth. We hypothesize that certain MPAs have a predictive value in determining the tendency of adolescent behavioral problems.
2. Methods
2.1. Subjects
Adolescents aged 11 to 19 years were eligible for recruitment in the primary care settings or nearby communities. Those who had congenital anomalies (e.g., orofacial clefts) or psychiatric diseases (e.g., schizophrenia) were excluded from the study. A health behavior questionnaire was developed for the purpose of this study, according to the published guidelines for adolescent preventive health assessments.[20] We also invited 3 experts in that field to evaluate the appropriateness of questionnaire used in the local clinical context. Participants were asked to complete the questionnaire confidentially guaranteed and were provided with appropriate consultations and normative developmental guidance for their health behavioral problems. Written informed consents from the adolescents and their parents were obtained in the beginning of study. The entire process was approved by the Institutional Review Board of the National Cheng Kung University Hospital.
2.2. Measurements of behavioral outcomes
Problematic conducts were assessed by asking participants whether they had driven dangerously (e.g., racing or drunk driving), carried weapons, or were involved in deviant behaviors (e.g., damaging properties, skipping class, running away from home, or provoking physical fights) within the past 1 year. The answers to these questions were dichotomous. The case group was comprised of those who gave positive answer to any of these questions.
Substance use was assessed by asking if the participants had used tobacco, illicit drugs, or betel nuts within the past 3 months. The case group was comprised of those with use of any of the 3 substances mentioned.
Early sexual practices were defined by having sexual intercourse before 18 years of age.
2.3. Assessments of minor physical anomalies and craniofacial features
The scale in use, which was developed based on previous studies as described elsewhere,[21–23] assessed both qualitative and quantitative items of MPAs. In short, a total of 25 new items were added to the original 16 qualitative items from the Waldrop scale (totaling to 41). For the reason of finding imperfections in anatomic symmetry, 28 items were measured separately on the right and left sides. Thirty-three items were dichotomous according to the presence or absence of morphological anomalies in 6 regions, including head, eyes, ears, mouth, hands, and feet; while the remaining 8 items were rated with a 3-point Likert scale (0, 1, and 2) to capture the magnitude of anomaly. The ratings of the items on this scale were summed up to represent overall or regional MPA scores. For the quantitative measurements of craniofacial features, there were a total of 27 items like head circumference, canthal distance, and philtrum length. We used calipers, tapes, and protractors in a standardized manner for these anthropometric measurements.
Two research assistants were trained for performing the measurements. Their measurements were first validated (inter-rater reliability ranging between 0.95 and 1.0; intraclass correlation coefficient 0.70–0.99) by a group of 20 healthy subjects.
2.4. Statistical analysis
Within this cohort, we compared sex, age, and anthropometric parameters among cases and controls that were defined according to their answers to the questions of health behaviors mentioned above. Comparative analysis including t tests and χ2 tests were used for continuous and categorical data respectively. Further, we constructed predictive models for behavioral outcomes. Adjustments for covariates such as sex, age, and body mass index (BMI) were applied in univariate and multivariate logistic regression models. Stepwise logistic regression analysis was used with a significance level of 0.1 set for entry and 0.1 for stay in the model. Age, sex, and BMI were also included in the stepwise selection method. For the symmetrical anatomic region, the values of both sides were added and treated as a single variable. We reported adjusted odds ratios (OR) and 95% confidence intervals (CI) with a significant level set at P value <.05. The analysis of receiver operating characteristic (ROC) curve was also included in these logistic regression models to evaluate predictive accuracy, sensitivity, and specificity of these physical variables. All statistical analyses were performed using SAS statistical software, version 9.3 and SAS enterprise miner, version 5.2 (SAS Institute, Cary, NC).
3. Results
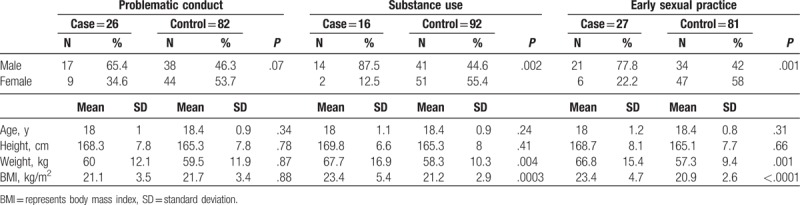
A total of 108 adolescents with 55 (50.9%) males and a mean of age 18.3 (±0.93) years (Table 1). In general, male participants had a higher prevalence of problematic conducts (30.9% in males vs. 17% in females), substance use (25.5% in males vs. 3.8% in females), and early sexual practices (38.2% in males vs. 11.3% in females).
Table 1.
Characteristics of study subjects.
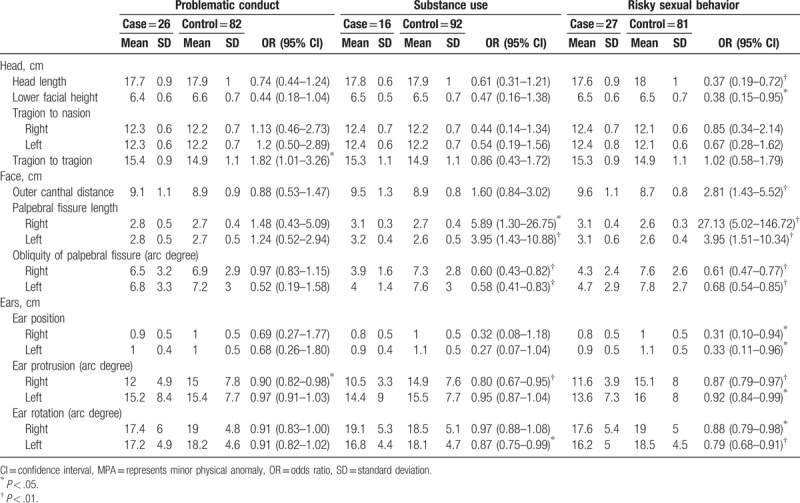
In univariate comparison, participants with substance use had a significantly lower qualitatively measured MPA score in the global head but higher in the mouth region than their controls after adjusting for age, sex, and BMI (Table 2). On the other hand, the MPA scores were higher in the mouth, hand, and foot regions among those with reported early sexual practices than among those without. Regarding the quantitative MPAs, a longer length and less obliquity of the palpebral fissures were noted among adolescents with substance use and early sexual practices than among their controls (Table 3). In addition, early sexual practices were also marked by a lesser degree of ear protrusion.
Table 2.
Qualitative MPA scores for adolescent with and without health-compromising behaviors.
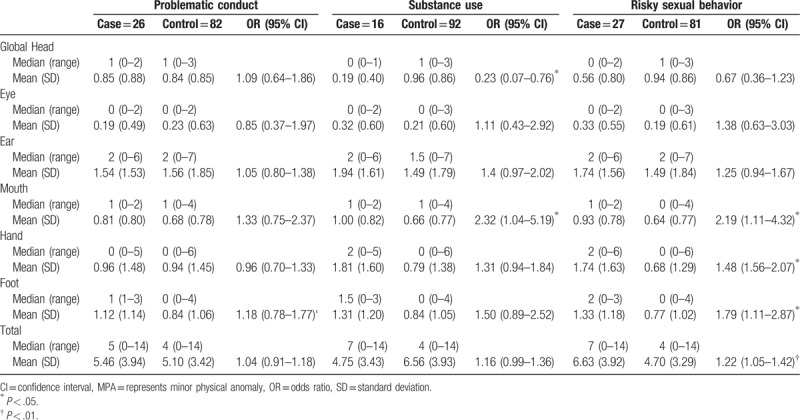
Table 3.
Quantitative MPA scores for adolescent with and without health-compromising behaviors.
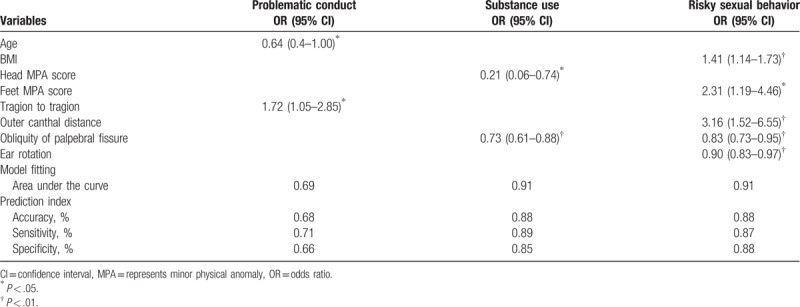
After multivariate adjusting for possible relevant physical features, the head MPA score (OR = 0.21, 95% CI 0.06–0.74) and the obliquity of palpebral fissure (OR = 0.73, 95% CI 0.61–0.88) were negatively associated with substance use in surveyed adolescents. In the ROC analysis, the area under curve (AUC) was 0.91 and the overall prediction indices were 0.89 for sensitivity and 0.85 for specificity (Table 4). On the other hand, early sexual practices were associated with higher BMI (OR = 1.41, 95% CI 1.14–1.73), higher feet MPA score (OR = 2.31, 95% CI 1.19–4.46), and greater outer canthal distance (OR = 3.16, 95% CI 1.52–6.55). The obliquity of palpebral fissure (OR = 0.83, 95% CI 0.73–0.95) and degree of ear rotation (OR = 0.9, 95% CI 0.83–0.97) were negatively associated with early sexual practice. The AUC in the ROC analysis for early sexual practice was 0.91 and the prediction indexes were 0.87 for sensitivity and 0.88 for specificity. The prediction indices of MPAs for problematic conducts were not as remarkable, though, as the results showed a significant association between the intertragion distance and problematic conducts (OR = 1.72, 95% CI 1.05–2.08).
Table 4.
Multivariate stepwise logistic regression analysis on the MPAs associated with adolescent health-compromising behaviors.
4. Discussion
In this study, the results showed that MPAs were different in adolescents with health-compromising behaviors as compared with their controls. MPAs in the head, eye, ear, and feet regions were most salient associative factors of adolescent substance use and early sexual practices. Overall, the predictive values of MPAs were high for sensitivity and specificity in serving as neurodevelopmental endophenotypes of adolescent health-compromising behaviors.
Adolescents with substance use had less MPAs in the global head region, and they also differed quantitatively in the obliquity and length of palpable fissures, and their ear configurations. Contrary to previous research,[19] the qualitative MPA score in the mouth region was only marginally associated with adolescent substance use; the significance of association was canceled by other competitive physical variables after multivariate adjustment. Only the intertragion distance was significantly associated with adolescent deviant conducts. Ethnic difference may explain this cross-ethnic discrepancy. Another possible reason may lie within the variation of qualitative measurement. Unlike in Arseneault's study where only high-arched palate, furrowed tongue, and smooth-rough tongue spots were described,[19] we measured a total of 6 items of mouth anomalies further including thin lip, cleft lip, and cleft palate. The 3 newly added items may attenuate the association between the mouth anomalies and violent delinquency in adolescence.
An unexpected finding was the negative correlation between head MPA and substance use. We looked back at the items of MPA in the head region among the recruited cohort and only found that substance users were less representative in having thin and curly hair than controls. Fine hair has been reported as one of the common physical anomalies in patients with first-episode psychosis, which underlines its potential role of endophenotype in neuropsychiatric diseases.[24] This correlation is less remarkable in Arseneault's research,[19] where fine hair was not associated with violent or nonviolent delinquent behaviors. A contradictory finding in our study should be interpreted with cautions to ethnic differences in the study population. The other possible reason is the subjectivity regarding the measurement of qualitative phenotypes, despite that frequency scale was applied to eliminate the judgement bias. How genetic backgrounds of hair quality contribute to adolescent behavior may require further research to validate.
For the quantitative traits, our finding revealed a critical link between the length and obliquity of the palpebral fissures and substance use. This observation has not been reported yet elsewhere. In addition, the above 2 palpebral features were also significantly related to early sexual practices. The interpretation of this finding gives rise to 2 different hypotheses. First, a neurodevelopmental abnormity marked by the palpebral features could be the cause of adolescent externalizing behavioral problems. As previous research stated, the slant of palpebral fissure and the shape of eye were prominently different in certain types of neurodevelopmental disorders like Down syndrome and schizophrenia.[22,23,25,26] These affected patients usually have a higher propensity for behavioral disturbances. The subjects surveyed in this study are healthy but may have minor neuropsychiatric problems undiagnosed yet or subclinical levels of neurodevelopmental deficits. The second hypothesis reverses cause and consequence. As the eye region is one of the expression centers on the face, its size, shape, and position play an important role in defining physical attractiveness.[27,28] Large eyes and pupils are generally considered more expressive and attractive in both men and women. Facial attractiveness has also been shown to contribute to enhanced sexual activity, especially for short-term relationships.[29,30] Body attractiveness is accompanied with an earlier age of first sex and multiple sex partners;[30,31] this is supported by our finding on the correlation between the palpebral features and early sexual practices in adolescence. As early sex and substance use potentially coexist in adolescents living in complicated social contexts, the palpebral features are indirectly linked to these delinquent behaviors. This way, the look of the eye is not an endophenotype, but the reason of driving the occurrence of delinquency, itself.
From neurodevelopmental perspective, the results of the link between physical features and adolescent behavioral outcomes imply that genetic compositions, which contribute to the presence of minor physical anomalies, also predispose individuals to health-compromising behaviors. As these behaviors do not appear suddenly during adolescence, their etiological factors should be thoroughly studied and targeted at when it comes to early identification and prevention. Obtaining a global view of behavioral profiles should be the first step toward guiding the health community to pay attention to and attend adolescent health and development needs.
There were some limitations that need be addressed along with these findings. One problem we have not completely solved is the time dependence of certain MPAs. As the age increases, some craniofacial anthropometric measurements change their meaning, while the others are invariably throughout life. With other words, quantitative measurements are less stable than qualitative ones. This requires the researcher to create same-age and -sex cohorts, or to adjust the actual data as if they belonged to the same cohorts, particularly important in children and adolescents who may grow at different paces. Although we adjusted participants’ age, sex, and body mass index in the regression analysis, this may attenuate but not totally eliminate this limitation inherent to individual growth. Second, inter-rater variance in MPAs and craniofacial measurements may exist but could be ameliorated by premeasurement training and standardized procedures. Third, we will also have to modify the screening questionnaires to reflect extent, frequency, and regularity. For example, we neither assessed the frequency of alcohol drinking or cigarette smoking, nor described the additivity of their use. The rating of these aspects will change the categorical border between the case and control classes. To retune our analysis, further research is required to gradually vary this (multidimensional) border to maximize significance. Further, parental lifestyle[32] and socio-economic status[33] that could be associated with both occurrences of physical anomalies and adolescent health behaviors are potential confounders that were however not controlled in this study. We may need more research to elaborate the role of these factors in the association between MPAs and adolescent health behaviors.
5. Conclusion
Adolescents with substance use might have certain MPAs that are different from those in controls. High predictive values of MPAs for substance use and early sexual practice may suggest a neurodevelopmental etiology of these behaviors in adolescence. The etiological complexity of adolescent neurobehavioral development is highlighted and requires further investigations to elucidate.
Author contributions
Conceptualization: Meng-Che Tsai, Chih-Ting Lee, I-Ning Tsai, Yi-Lin Liang, Sheng-Hsiang Lin.
Data curation: I-Ning Tsai, Shu-Ting Gan, Sheng-Hsiang Lin.
Formal analysis: Meng-Che Tsai, Chih-Ting Lee, I-Ning Tsai, Shu-Ting Gan, Sheng-Hsiang Lin.
Funding acquisition: Meng-Che Tsai, Yi-Lin Liang.
Investigation: Meng-Che Tsai, Chih-Ting Lee, I-Ning Tsai, Shu-Ting Gan, Yi-Lin Liang, Sheng-Hsiang Lin.
Methodology: Meng-Che Tsai, Chih-Ting Lee, I-Ning Tsai, Shu-Ting Gan, Sheng-Hsiang Lin.
Project administration: Meng-Che Tsai, Yi-Lin Liang, Sheng-Hsiang Lin.
Resources: Meng-Che Tsai, Chih-Ting Lee, Yi-Lin Liang, Sheng-Hsiang Lin.
Software: I-Ning Tsai, Shu-Ting Gan, Sheng-Hsiang Lin.
Supervision: Sheng-Hsiang Lin.
Validation: Meng-Che Tsai, Sheng-Hsiang Lin.
Writing – original draft: Meng-Che Tsai, Chih-Ting Lee, Sheng-Hsiang Lin.
Writing – review & editing: Meng-Che Tsai, Chih-Ting Lee, Sheng-Hsiang Lin.
Footnotes
Abbreviations: AUC = area under curve, BMI = body mass index, CI = confidence intervals, MPAs = minor physical anomalies, OR = odds ratio, ROC = receiver operating characteristic.
This study was supported by the research grants from the National Cheng Kung University Hospital (NCKUH-10205017 and NCKUH-10706002).
The authors have no conflicts of interest to disclose.
References
- [1].Lerner RM, Castellino DR. Contemporary developmental theory and adolescence: developmental systems and applied developmental science. J Adolesc Health 2002;31(6 suppl):122–35. [DOI] [PubMed] [Google Scholar]
- [2].Patton GC, Viner R. Pubertal transitions in health. Lancet 2007;369:1130–9. [DOI] [PubMed] [Google Scholar]
- [3].Chen CF. Personality, safety attitudes and risky driving behaviors—evidence from young Taiwanese motorcyclists. Accid Anal Prev 2009;41:963–8. [DOI] [PubMed] [Google Scholar]
- [4].Fond G, Loundou A, Guillaume S, et al. Smoking behavior characteristics of non-selected smokers with childhood attention-deficit/hyperactivity disorder (AD/HD) history: a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci 2014;264:379–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Wilens TE, Biederman J. Alcohol, drugs, and attention-deficit/hyperactivity disorder: a model for the study of addictions in youth. J Psychopharmacol 2006;20:580–8. [DOI] [PubMed] [Google Scholar]
- [6].McClernon FJ, Kollins SH. ADHD and smoking. Ann N Y Acad Sci 2008;1141:131–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Csabi G, Zsuppan R, Jeges S, et al. Minor physical anomalies are more common in children with idiopathic epilepsy. Neuropsychopharmacol Hung 2014;16:115–20. [PubMed] [Google Scholar]
- [8].Angkustsiri K, Krakowiak P, Moghaddam B, et al. Minor physical anomalies in children with autism spectrum disorders. Autism 2011;15:746–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Firestone P, Peters S, Rivier M, et al. Minor physical anomalies in hyperactive, retarded and normal children and their families. J Child Psychol Psychiatry 1978;19:155–60. [DOI] [PubMed] [Google Scholar]
- [10].Hata K, Iida J, Iwasaka H, et al. Minor physical anomalies in childhood and adolescent onset schizophrenia. Psychiatry Clin Neurosci 2003;57:17–21. [DOI] [PubMed] [Google Scholar]
- [11].Pomeroy JC, Sprafkin J, Gadow KD. Minor physical anomalies as a biologic marker for behavior disorders. J Am Acad Child Adolesc Psychiatry 1988;27:466–73. [DOI] [PubMed] [Google Scholar]
- [12].Firestone P, Peters S. Minor physical anomalies and behavior in children: a review. J Autism Dev Disord 1983;13:411–25. [DOI] [PubMed] [Google Scholar]
- [13].Cheng H, Chang CC, Chang YC, et al. A pilot study: association between minor physical anomalies in childhood and future mental problems. Psychiatry Investig 2014;11:228–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Krouse JP, Kauffman JM. Minor physical anomalies in exceptional children: a review and critique of research. J Abnorm Child Psychol 1982;10:247–64. [DOI] [PubMed] [Google Scholar]
- [15].Campbell M, Geller B, Small AM, et al. Minor physical anomalies in young psychotic children. J Abnorm Child Psychol 1978;135:573–5. [DOI] [PubMed] [Google Scholar]
- [16].Gourion D, Goldberger C, Bourdel MC, et al. Minor physical anomalies in patients with schizophrenia and their parents: prevalence and pattern of craniofacial abnormalities. Psychiatry Res 2004;125:21–8. [DOI] [PubMed] [Google Scholar]
- [17].Ozgen HM, Hop JW, Hox JJ, et al. Minor physical anomalies in autism: a meta-analysis. Mol Psychiatry 2010;15:300–7. [DOI] [PubMed] [Google Scholar]
- [18].Xu T, Chan RC, Compton MT. Minor physical anomalies in patients with schizophrenia, unaffected first-degree relatives, and healthy controls: a meta-analysis. PLoS One 2011;6:e24129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Arseneault L, Tremblay RE, Boulerice B, et al. Minor physical anomalies and family adversity as risk factors for violent delinquency in adolescence. Am J Psychiatry 2000;157:917–23. [DOI] [PubMed] [Google Scholar]
- [20].Salerno J, Marshall VD, Picken EB. Validity and reliability of the rapid assessment for adolescent preventive services adolescent health risk assessment. J Adolesc Health 2012;50:595–9. [DOI] [PubMed] [Google Scholar]
- [21].Waldrop MF, Pedersen FA, Bell RQ. Minor physical anomalies and behavior in preschool children. Child Dev 1968;39:391–400. [PubMed] [Google Scholar]
- [22].Lin AS, Chang SS, Lin SH, et al. Minor physical anomalies and craniofacial measures in patients with treatment-resistant schizophrenia. Psychol Med 2015;45:1839–50. [DOI] [PubMed] [Google Scholar]
- [23].Ismail B, Cantor-Graae E, McNeil TF. Minor physical anomalies in schizophrenic patients and their siblings. Am J Psychiatry 1998;155:1695–702. [DOI] [PubMed] [Google Scholar]
- [24].Hindley D, Medakkar S. Diagnosis of Down's syndrome in neonates. Arch Dis Child Fetal Neonatal Ed 2002;87:F220–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Loos HS, Wieczorek D, Wurtz RP, et al. Computer-based recognition of dysmorphic faces. Eur J Hum Genet 2003;11:555–60. [DOI] [PubMed] [Google Scholar]
- [26].Volpe CR, Ramirez OM. The beautiful eye. Facial Plast Surg Clin North Am 2005;13:493–504. [DOI] [PubMed] [Google Scholar]
- [27].Cunningham MR. Measuring the physical in physical attractiveness: quasi-experiments on the sociobiology of female facial beauty. J Personality Soc Psychol 1986;50:925. [Google Scholar]
- [28].Rhodes G, Simmons LW, Peters M. Attractiveness and sexual behavior: does attractiveness enhance mating success? Evolut Hum Behav 2005;26:186–201. [Google Scholar]
- [29].Johnston VS, Franklin M. Is beauty in the eye of the beholder? Ethol Sociobiol 1993;14:183–99. [Google Scholar]
- [30].Weeden J, Sabini J. Subjective and objective measures of attractiveness and their relation to sexual behavior and sexual attitudes in university students. Arch Sex Behav 2007;36:79–88. [DOI] [PubMed] [Google Scholar]
- [31].Mhalla A, Boussaid N, Gassab L, et al. Minor neurological and physical anomalies in patients with first-episode psychosis. Encephale 2013;39:149–54. [DOI] [PubMed] [Google Scholar]
- [32].Pei L, Kang Y, Cheng Y, et al. The association of maternal lifestyle with birth defects in Shaanxi province, Northwest China. PLoS One 2015;10:e0139452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Carmichael SL, Nelson V, Shaw GM, et al. Socio-economic status and risk of conotruncal heart defects and orofacial clefts. Paediatr Perinat Epidemiol 2003;17:264–71. [DOI] [PubMed] [Google Scholar]


