Abstract
Objectives
The role of alloplastic materials in maxillofacial reconstruction is still controversial. Determining the utility of porous, high-density, polyethylene implants as a highly stable and flexible, porous alloplast, with properties such as rapid vascularization and tissue ingrowth, is crucial in cases of maxillofacial deformities and aesthetic surgery.
Materials and Methods
Thirty high-density porous polyethylene implants were implanted in 16 patients that had been referred to a private office over a three-year period. These implants were used for correcting congenital deformities, posttraumatic defects and improving the aesthetic in nasal, paranasal, malar, chin, mandibular angle, body and orbital areas.
Results
The outcomes of the cases in this study showed good aesthetic and functional results. The majority of patients had no signs of discomfort, rejection or exposure. Two implants suffered complications: a complicated malar implant was managed by antibiotic therapy, and an infected mandibular angle implant was removed despite antibiotic therapy.
Conclusion
Based on the results, the Medpor implant seems to be an excellent biomaterial for correcting various facial deformities. Advantages include its versatility and relatively ideal pore size that allows for excellent soft tissue ingrowth and coverage. It is strong, flexible and easy to shape.
Keywords: Maxillofacial prosthesis implantation, Reconstructive surgical procedures, Medpor
I. Introduction
Facial harmony and balance may be determined by hard tissues, which support the soft tissues1. In cases of trauma, congenital deformities, and aesthetic surgeries, facial harmony can be achieved by facial implants2. It has been argued that autogenous materials, such as bone or cartilage, are suitable materials for facial augmentation3. However, problems such as donor site morbidity, increased surgical time and complexity, difficulty in shaping the grafts, graft warpage, and resorption when using autogenous materials have resulted in the continuous use of alloplastic implants4,5. Alloplastic biomaterials also have some disadvantages. Hydroxyapatite biomaterial does not promote tissue ingrowth6. Methylmetacrylate and silicone cause resorption of the underlying bone7,8. In addition, these materials do not permit tissue ingrowth and lead to capsulation and migration of the implant7,9.
In recent years, the use of porous implants has received considerable attention. Allowing for tissue ingrowth is the main advantage of porous materials4. Porous high-density polyethylene (PHDPE) as an alloplastic material shows many advantages compared to other biomaterials. PHDPE was developed in the early 1970s and has been available for clinical implantation since 198510,11,12. Polyethylene resins are composed of straight-chain aliphatic hydrocarbons.
The Medpor implant is made of a medical-grade, high density polyethylene that is sintered to create a somewhat flexible framework of interconnecting pores4,11,12. The pore size range from 160 to 368 µm and more than half of these pores are larger than 150 µm in diameter11,12. It has been shown that Medpor stimulates tissue ingrowth and collagen deposition into the pores, which in turn form a stable complex that is resistant to infection, exposure and contractile forces4,13,14. Medpor possesses the following mechanical properties: (1) it is easily formed, (2) it is strong enough to be used in non-load bearing areas, and (3) it is readily available as a sterile implant in various pre-formed shapes13.
Our report reviews the use of PHDPE implants for correcting deformities in the orbit (floor, medial, and lateral wall), nasal, malar, chin, mandibular body and mandibular angle in 16 patients.
II. Materials and Methods
We used 30 PHDPE implants (Medpor Biomaterial; Porex Surgical, Newnan, GA, USA) for 16 patients with different types of deformities between the years 2010 to 2012 in Qazvin University of Medical Sciences. All patients were informed about the advantages and disadvantages of these implants. Six sites of deformity (malar area, orbital floor, mandibular ramus and body, nasal, paranasal and chin area) were corrected with prefabricated Medpor. All surgeries were performed under general anesthesia and through intra- or extra-oral approaches based on the case and minimal manipulation. Implants were inserted in the subperiosteal plane and secured with screws. Before insertion, implants were individually contoured with a scalpel based on deformity geometry, and they were immersed in a gentamicin solution in order to minimize risk of infection. After surgery, regular postoperative protocol, including pain relief and intravenous antibiotic therapy (cefazolin 1 g, four times a day), was prescribed. Patients were discharged with oral antibiotics (cephalexin 500 mg, four times a day) for one week, and mouthwash rinse was prescribed for cases with an intraoral approach.
Patients were recalled routinely after 1, 4, and 12 weeks for postoperative follow-up, and long term follow-up data were collected after 5 to 7 years. Patient satisfaction and objective criteria (asymmetry and displacement, postoperative complications and corrective surgery) were evaluated.
1. Presentation of cases
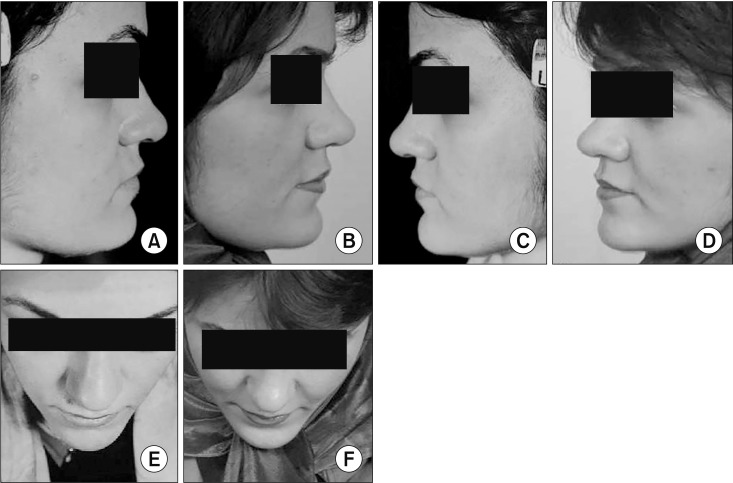
1) Case 1
A 22-year-old woman with malar and paranasal deficiency. A “M” design malar implant and paranasal implant were used and fixed with screws.(Fig. 1)
Fig. 1. Application of a “M” design malar implant and a paranasal implant. A, C. Preoperative lateral view. B, D. Postoperative lateral view. E. Preoperative view from above. F. Postoperative from above.
2) Case 2
A 20-year-old woman with severe saddle nose deformity as well as malar and infraorbital rim depression. Initially, two “M” design malar implants were used to augment the malar area. The nasal dorsum was corrected by nasal radix and columellar strut implants, increasing the nasal projection and elevation. Finally, we reinforced and reconstructed the upper lateral cartilages using a Medpor implant.(Fig. 2)
Fig. 2. Augmentation of malar bones using two “M” design malar implants and addressing the saddle nose with a nasal radix implant. A. Preoperative three-quarter view. B. Postoperative three-quarter view. C. Preoperative lateral view. D. Postoperative lateral view. E. Preoperative frontal view. F. Postoperative frontal view.
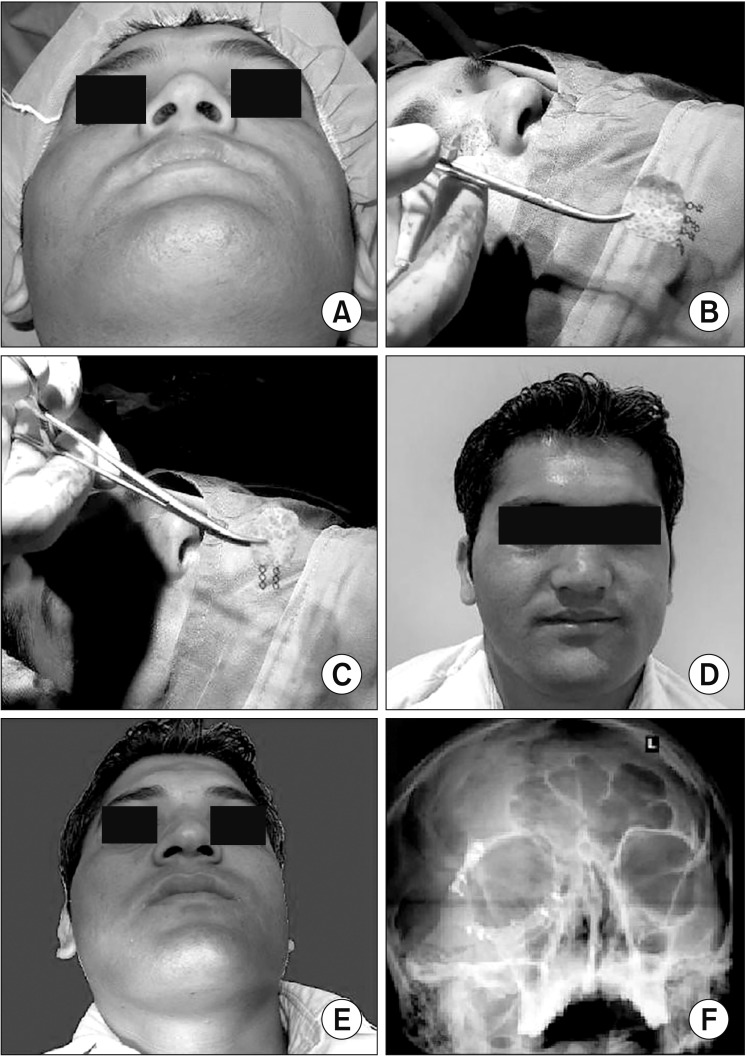
3) Case 3
A 25-year-old man complaining of diplopia with an orbital blowout fracture and enophthalmous following a road traffic accident. At first, the zygomatico-maxillary complex fracture was approached. Next, diplopia and enophthalmous were addressed using a Medpor channel implant which is thicker posteriorly and thinner anteriorly, causing the globe to move forward. We used an infraorbital rim incision for accessing the orbital floor and the medial and lateral wall of the orbit. Orbital defects in the medial and lateral wall were corrected by a Medpor implant reinforced with titanium mesh. After three months, the patient had no diplopia or enophthalmous.(Fig. 3)
Fig. 3. Correction of diplopia and enophthalmous after a road traffic accident. A. Preoperative view from below. B. Medpor implant reinforced with titanium mesh for lateral wall of the orbit. C. Medpor implant reinforced with titanium mesh for medial wall of the orbit. D. Postoperative frontal view. E. Postoperative facial view from below. F. Postoperative radiography and reconstruction of medial and lateral wall of the orbit with titanium reinforced medpor implant.
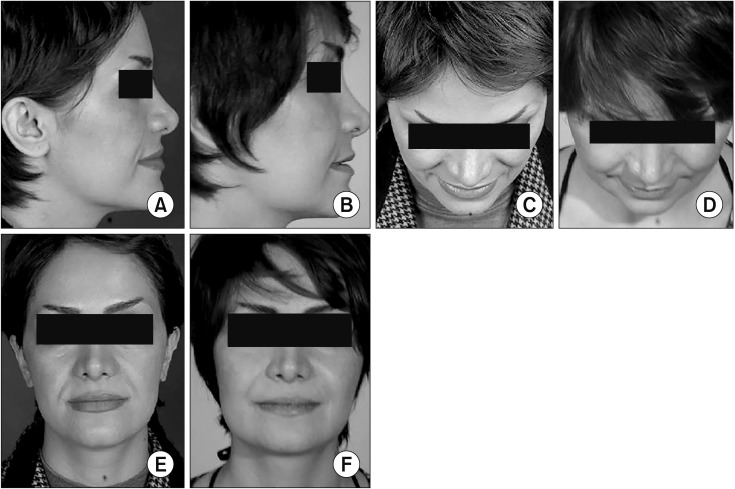
4) Case 4
A 30-year-old woman complaining of malar deficiency and poor facial contour in the mandibular angle and the lower and upper lip area. A “M” design malar implant was used for malar bone augmentation, and autologous fat was injected to refine the angle, ramus, and around the lips.(Fig. 4)
Fig. 4. Using “M” design malar implant to augment malar bone combined with fat injections to the mandibular angle, ramus, and both lips. A. Preoperative lateral view. B. Postoperative lateral view. C. Preoperative view from above. D. Postoperative view from above. E. Preoperative frontal view. F. Postoperative frontal view.
III. Results
A summary of patients is shown in Table 1. This study included 13 females and 3 males, and the mean age was 26.3±4.4 years. There were three indications for the application of PHDPE implants in our clinic: congenital deformity (26.7%), posttraumatic defect (26.7%), and aesthetic (46.7%). (Table 2) Implants were used for different sites of the maxillofacial region according to the following frequencies: malar (50.0%), orbital (10.0%), mandibular body and angle (13.3%), nasal (10.0%), paranasal (6.7%), and chin (10.0%).(Table 3) The mean follow-up was 5.4±0.62 years with complication and satisfaction rates of 12.5% and 87.5%, respectively.
Table 1. Summary of patients.
| No. | Age (yr) | Sex | Site of defects | Etiology | Follow-up (yr) | Complication | Corrective | Asymmetry | Patient satisfaction | No. of implants used |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 23 | F | Malar | Aesthetic | 5 | No | No | No | Yes | 1 |
| 2 | 28 | F | Malar | Aesthetic | 7 | No | No | No | Yes | 2 |
| 3 | 32 | F | Malar | Aesthetic | 5 | No | No | No | Yes | 2 |
| 4 | 25 | F | Malar | Congenital | 5 | No | No | No | Yes | 2 |
| 5 | 22 | F | Malar | Congenital | 5 | No | No | No | Yes | 2 |
| Paranasal | ||||||||||
| 6 | 30 | F | Malar | Trauma | 6 | No | No | No | Yes | 2 |
| 7 | 35 | F | Malar | Trauma | 5 | No | No | No | Yes | 1 |
| 8 | 32 | F | Malar | Aesthetic | 5 | No | No | No | Yes | 2 |
| 9 | 20 | M | Malar | Trauma | 5 | No | No | No | Yes | 4 |
| Nasal | ||||||||||
| 10 | 25 | M | Orbit | Aesthetic | 7 | No | No | No | Yes | 3 |
| 11 | 30 | F | Mandibular body & angle | Aesthetic | 6 | No | No | No | Yes | 2 |
| 12 | 26 | F | Mandibular body & angle | Aesthetic | 6 | Infection | Angle implant removed | Yes | No | 2 |
| 13 | 20 | F | Malar | Congenital | 5 | Displacement & infection | Incision and drainage | Yes | No | 1 |
| 14 | 24 | F | Paranasal | Congenital | 5 | No | No | No | Yes | 1 |
| 15 | 24 | M | Chin | Aesthetic | 5 | No | No | No | Yes | 1 |
| 16 | 26 | F | Chin | Trauma | 6 | No | No | No | Yes | 2 |
(F: female, M: male)
Table 2. Etiology of deformities.
| Reason for implant | No. of implants (%) | No. of cases |
|---|---|---|
| Posttraumatic | 8 (26.7) | 4 |
| Aesthetic | 14 (46.7) | 8 |
| Congenital | 8 (26.7) | 4 |
Table 3. Sites and number of implants used in patients.
| Region | No. of patients | No. of implants (%) |
|---|---|---|
| Malar | 8 | 15 (50.0) |
| Orbit | 1 | 3 (10.0) |
| Mandibular body and angle | 2 | 4 (13.3) |
| Nasal | 1 | 3 (10.0) |
| Chin | 2 | 3 (10.0) |
| Paranasal | 2 | 2 (6.7) |
In the postoperative period, two patients suffered complications in the malar and mandibular angle areas. We administered an intravenous antibiotic to these patients, and their wounds were incised and drained. This protocol was successful in one patient, but we had to remove the angle implant in the second patient. All other patients were satisfied with their treatment.
IV. Discussion
Facial implants are frequently used for aesthetic purposes, correction of congenital deformities and restoring anatomical harmony after trauma15. Facial implants became popular around the turn of the century, but Roussett was using gold implants in the nose as early as 182815. Joseph16 used ivory inlays for the nose in 1907. In 1896, Israel used tibial bone for nasal reconstruction17, and in 1900, costal cartilage was used for reconstructive purposes by Von Mangold18. Brown et al.19 reported the advantages of silicone implants in 1953, and silicon is one of the most widely used implant materials today.
An ideal alloplastic implant should be inert, non-carcinogenic, non-inflammatory and non-allergenic. In addition, it should resist mechanical strain and be easy to fabricate and shape. An optimal implant should integrate with the surrounding soft tissue, bone and cartilage2.
Autologous materials, despite some disadvantages, still remain the gold standard for craniofacial reconstruction. Increased time and complexity of surgery, donor site morbidity, difficulty in graft shaping, warpage and resorption have been referred to as disadvantages of autologous materials5,20,21.
This report describes our experience with PHDPE implants (Medpor Biomaterial), an alloplastic implant material that may offer advantages when compared with previously used materials.
Medpor is user friendly, and it may easily be fixed for restoration of a three-dimensional structure. From a physical point of view, Medpor is a pure complex, and it is composed of biocompatible material that is strong and does not easily undergo degradation14,22. These qualities, along with an ability to maintain its initial volume, make Medpor a suitable alternative for autogenous graft or other alloplastic materials23. By forming interconnecting pores, the Medpor implants are suitable materials for orbital reconstruction24. These pores size range from 160 to 368 µm, and more than half of these pores are larger than 150 µm in diameter11. Klawitter et al.25 and Spector et al.26 stated that pore size larger than 100 µm promote tissue ingrowth. For example, materials such as Polytef (Gore-tex) have pore sizes much less than 100 µm26. Such porosity results in the ingrowth of vascularized tissues into the implant, eventually forming a highly stable complex which is resistant to infection and deformation14,20,22. But, on the other hand, this soft tissue ingrowth can make surgical removal of porous polyethylene extremely complicated27.
Extensive vascular ingrowth into the implant transfers cellular production deep into the implant, which can promote infection resistance. However, Romano et al. managed facial fractures in 140 patients with Medpor implants, and infection was observed in only one case14. In another study by RidwanPramana et al.28, they reported 7.2% infection rate in 69 implants that have been used in 40 post trauma patients.
Medpor implants have been used for nasal deformities. Niechajev29 used 118 implants in 102 patients for nose deformities, chin hypoplasia and malar hypoplasia. Three rhinoplasty cases were infected, two cases were faced with partial extrusion, and two dorsal and two chin implants were trimmed. Mohammadi et al. used PHDPE in open rhinoplasty. Medpor can be used as a dorsal and spreader graft in the correction of severe nose deformity without noticeable complications, such as infection and extrusion30. In the current study, we used 3 implants for nasal reconstruction (dorsal, columellar, and upper lateral cartilage implants) without any complications.
Medpor implants have been used for orbital deformities as well. In a study by Rubin et al.24, only one orbital implant was infected 1-week postoperatively, and other minor complications included under correction, a symptomatically palpable implant, and transient postoperative chemosis. In different studies by Baj et al.31 and Rapidis and Day32, high density polyethylene implants were recommended for reconstruction of the temporal defect after temporalis myofascial flap transposition. It is an easy and safe method with excellent functional and aesthetic results, and the method has a success rate of 90%. Studies by Rubin et al.24 and Xu et al.33 have shown that porous polyethylene sheets are very reliable materials for reconstruction of orbital blow-out fractures, restoration of orbital volume, and treatment and correction of diplopia and enophthalmous.
Xu et al.33 explained that overcorrection of 1 to 2 mm is necessary during surgery due to soft tissue swelling or atrophy. They observed no sign of infection in their study. Some authors reported risk of patient dissatisfaction because the rigid nature of porous polyethylene makes it difficult to contour. The current use of computer-aided design/computeraided manufacturing (CAD/CAM) techniques have facilitated the rapid and precise construction of customized implants34. Sun et al.35 showed that customized titanium mesh can accurately correct enophthalmous accompanying orbital fractures. He et al.36 stated that computer-assisted surgery can improve the treatment outcomes in delayed orbito-zygomatic fracture with enophthalmous.
In two separate studies by Yilmaz et al.37 and Lin et al.38, 26 and 21 patients, respectively, with orbital floor fractures were treated by porous polyethylene implants. The patients had problems such as enophthalmous, diplopia, limited extrinsic ocular motility, hypoglobus and impairment of the infraorbital nerve. They concluded that porous polyethylene sheets are safe, reliable and effective implants. In addition, they reported that the sheets could be used for orbital floor fracture reconstruction without donor site morbidity or need for implant fixation. In a study conducted by Lin et al.38, orbital infection and/or worsening of diplopia weren't observed in any of the patients studied. In a study by Yilmaz et al.37, 4 postoperative infections in 4 patients were managed with antibiotics, and ectropion was formed in 2 cases. Cenzi et al.39 and Yaremchuk40, used 285 Medpor implants in 187 patients and 370 implants in 162 patients, respectively. They concluded that porous polyethylene implants have favorable properties for craniofacial skeletal reconstruction. None of their patients developed complications, such as extrusion, migration and infection.
Use of Medpor implants for areas like the ear, nose and maxilla in syndromic patients is associated with a higher risk of implant failure39. A study by Gosau et al.41 showed fibrovascular integration without encapsulation under light microscopy for the Medpor implant. They detected giant cells on the surface of the implants and evidence of implant material resorption.
An important disadvantage of Medpor implants is their invisibility in radiographic studies, because the Medpor implant shows no contrast41. Menderes et al.42 placed 83 implants in 71 patients for craniofacial reconstruction. Their study showed an increased risk of early and late exposure if the Medpor implant was placed directly under the skin instead of the subperiosteal plane. They preferred autogenous grafts, instead of allogenic materials, for reconstruction of the nasal dorsum and microtia. Romo et al.43 stated that if autogenous materials are inadequate or undesirable, the surgeon could use the Medpor implant to reconstruct and support the external nasal valve. On the other hand, Emsen44 supported the use of E-M shaped septal encircling with Medpor grafts as a safe, effective, reliable and permanent method for crooked nose reconstruction.
In this study, 16 patients with 30 Medpor implants were evaluated. We achieved good aesthetic and facial contour in all patients treated with PHDPE implants. None of the patients developed implant exposure. Two cases of postoperative infection in the malar and mandibular angle area were managed by incision and drainage and antibiotic therapy. Only the mandibular angle implant was removed due to unsuccessful medical treatment.
Based on the findings of this study, we can suggest PHDPE implants, having a low incidence of infection and acceptable aesthetic and functional outcomes.
V. Conclusion
The PHDPE alloplastic implant has a low incidence of infection and excellent cosmetic and functional results, and the implant is an acceptable alternative to existing alloplastic materials.
Footnotes
Authors' Contributions: M.K. organized the survey, designed the study, and treated the patients together with P.J. and F.R. M.K. and P.J. revised the manuscript. All authors read and approved the final manuscript.
Ethics Approval and Consent to Participate: This study was approved by the Qazvin University of Medical Sciences Ethics Committee (no. IR.QUMS.REC.1394.809). There is no conflict with ethical considerations.
Consent for Publishing Photographs: Written informed consent was obtained from all patients for publication of this article and accompanying images.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Rees TD. Physical considerations for the aesthetic surgery of the neck and face. In: Rees TD, editor. Aesthetic plastic surgery. Philadelphia: W.B. Saunders; 1980. p. 587. [Google Scholar]
- 2.Maas CS, Merwin GE, Wilson J, Frey MD, Maves MD. Comparison of biomaterials for facial bone augmentation. Arch Otolaryngol Head Neck Surg. 1990;116:551–556. doi: 10.1001/archotol.1990.01870050051005. [DOI] [PubMed] [Google Scholar]
- 3.Wolfe SA, Berkowitz S. Plastic surgery of the facial skeleton. Boston: Little, Brown; 1989. p. 687. [Google Scholar]
- 4.Spector M, Harmon SL, Kreutner A. Characteristics of tissue growth into proplast and porous polyethylene implants in bone. J Biomed Mater Res. 1979;13:677–692. doi: 10.1002/jbm.820130502. [DOI] [PubMed] [Google Scholar]
- 5.Breadon GE, Kern EB, Neel HB., 3rd Autografts of uncrushed and crushed bone and cartilage. Experimental observations and clinical implications. Arch Otolaryngol. 1979;105:75–80. doi: 10.1001/archotol.1979.00790140021004. [DOI] [PubMed] [Google Scholar]
- 6.Gosain AK Plastic Surgery Eductional Foundation DATA Committee. Biomaterials for reconstruction of the cranial vault. Plast Reconstr Surg. 2005;116:663–666. doi: 10.1097/01.prs.0000176289.05374.5b. [DOI] [PubMed] [Google Scholar]
- 7.Wellisz T, Lawrence M, Jazayeri MA, Golshani S, Zhou ZY. The effects of alloplastic implant onlays on bone in the rabbit mandible. Plast Reconstr Surg. 1995;96:957–963. doi: 10.1097/00006534-199509001-00029. [DOI] [PubMed] [Google Scholar]
- 8.Gui L, Huang L, Zhang Z. Genioplasty and chin augmentation with Medpore implants: a report of 650 cases. Aesthetic Plast Surg. 2008;32:220–226. doi: 10.1007/s00266-007-9106-6. [DOI] [PubMed] [Google Scholar]
- 9.Rubin JP, Yaremchuk MJ. Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 1997;100:1336–1353. doi: 10.1097/00006534-199710000-00043. [DOI] [PubMed] [Google Scholar]
- 10.Yaremchuk MJ. Infraorbital rim augmentation. Plast Reconstr Surg. 2001;107:1585–1592. doi: 10.1097/00006534-200105000-00047. [DOI] [PubMed] [Google Scholar]
- 11.Shanbhag A, Friedman HI, Augustine J, von Recum AF. Evaluation of porous polyethylene for external ear reconstruction. Ann Plast Surg. 1990;24:32–39. doi: 10.1097/00000637-199001000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Frodel JL, Lee S. The use of high-density polyethylene implants in facial deformities. Arch Otolaryngol Head Neck Surg. 1998;124:1219–1223. doi: 10.1001/archotol.124.11.1219. [DOI] [PubMed] [Google Scholar]
- 13.Wellisz T, Dougherty W. The role of alloplastic skeletal modification in the reconstruction of facial burns. Ann Plast Surg. 1993;30:531–536. doi: 10.1097/00000637-199306000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Romano JJ, Iliff NT, Manson PN. Use of Medpor porous polyethylene implants in 140 patients with facial fractures. J Craniofac Surg. 1993;4:142–147. doi: 10.1097/00001665-199307000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Nélaton C, Ombrédanne L, Berger P, Hartmann H. La rhinoplastie. Paris: G. Steinheil; 1904. [Google Scholar]
- 16.Joseph J. Treatise on rhinoplasty. Berl Klin Wochenschr. 1907;44:470. [Google Scholar]
- 17.Israel J. Two new methods of rhinoplasty. Plast Reconstr Surg. 1970;46:80–83. [PubMed] [Google Scholar]
- 18.Von Mangold H. Correction of saddle nose by cartilage transplant. Gesell Chir. 1900;29:460–463. [Google Scholar]
- 19.Brown JB, Fryer MP, Randall P, Lu M. Silicones in plastic surgery; laboratory and clinical investigations, a preliminary report. Plast Reconstr Surg (1946) 1953;12:374–376. doi: 10.1097/00006534-195311000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Niazi TN, Coppens J, Liu JK, Couldwell WT. Medpor implant in cranioorbitomaxillary reconstruction: institutional experience and a review of the literature. J Oral Maxillofacial Surg. 2008;7:444–448. [Google Scholar]
- 21.Deshpande S, Munoli A. Long-term results of high-density porous polyethylene implants in facial skeletal augmentation: an Indian perspective. Indian J Plast Surg. 2010;43:34–39. doi: 10.4103/0970-0358.63955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ram H, Singh RK, Mohammad S, Gupta AK. Efficacy of Iliac crest vs. Medpor in orbital floor reconstruction. J Maxillofac Oral Surg. 2010;9:134–141. doi: 10.1007/s12663-010-0047-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cenzi R, Guarda-Nardini L. [Use of porous plyethylene (Medpor) in maxillofacial surgery] Minerva Stomatol. 1995;44:559–582. Italian. [PubMed] [Google Scholar]
- 24.Rubin PA, Bilyk JR, Shore JW. Orbital reconstruction using porous polyethylene sheets. Ophthalmology. 1994;101:1697–1708. doi: 10.1016/s0161-6420(94)31113-4. [DOI] [PubMed] [Google Scholar]
- 25.Klawitter JJ, Bagwell JG, Weinstein AM, Sauer BW. An evaluation of bone growth into porous high density polyethylene. J Biomed Mater Res. 1976;10:311–323. doi: 10.1002/jbm.820100212. [DOI] [PubMed] [Google Scholar]
- 26.Spector M, Flemming WR, Sauer BW. Early tissue infiltrate in porous polyethylene implants into bone: a scanning electron microscope study. J Biomed Mater Res. 1975;9:537–542. doi: 10.1002/jbm.820090514. [DOI] [PubMed] [Google Scholar]
- 27.Kim HS, Park SS, Kim MH, Kim MS, Kim SK, Lee KC. Problems associated with alloplastic materials in rhinoplasty. Yonsei Med J. 2014;55:1617–1623. doi: 10.3349/ymj.2014.55.6.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ridwan-Pramana A, Wolff J, Raziei A, Ashton-James CE, Forouzanfar T. Porous polyethylene implants in facial reconstruction: outcome and complications. J Craniomaxillofac Surg. 2015;43:1330–1334. doi: 10.1016/j.jcms.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 29.Niechajev I. Facial reconstruction using porous high-density polyethylene (Medpor): long-term results. Aesthetic Plast Surg. 2012;36:917–927. doi: 10.1007/s00266-012-9911-4. [DOI] [PubMed] [Google Scholar]
- 30.Mohammadi S, Mohseni M, Eslami M, Arabzadeh H, Eslami M. Use of porous high-density polyethylene grafts in open rhinoplasty: no infectious complication seen in spreader and dorsal grafts. Head Face Med. 2014;10:52. doi: 10.1186/1746-160X-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baj A, Spotti S, Marelli S, Beltramini GA, Giannì AB. Use of porous polyethylene for correcting defects of temporal region following transposition of temporalis myofascial flap. Acta Otorhinolaryngol Ital. 2009;29:265–269. [PMC free article] [PubMed] [Google Scholar]
- 32.Rapidis AD, Day TA. The use of temporal polyethylene implant after temporalis myofascial flap transposition: clinical and radiographic results from its use in 21 patients. J Oral Maxillofac Surg. 2006;64:12–22. doi: 10.1016/j.joms.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 33.Xu JJ, Teng L, Jin XL, Ji Y, Lu JJ, Zhang B. Porous polyethylene implants in orbital blow-out fractures and enophthalmos reconstruction. J Craniofac Surg. 2009;20:918–920. doi: 10.1097/scs.0b013e3181a2d728. [DOI] [PubMed] [Google Scholar]
- 34.Tsouknidas A, Maropoulos S, Savvakis S, Michailidis N. FEM assisted evaluation of PMMA and Ti6Al4V as materials for cranioplasty resulting mechanical behaviour and the neurocranial protection. Biomed Mater Eng. 2011;21:139–147. doi: 10.3233/BME-2011-0663. [DOI] [PubMed] [Google Scholar]
- 35.Sun L, Xiao J, Lan Y, Xiong Y, Zhang L, Zhou H, et al. [Reconstruction of the orbital fracture with enophthalmos using customized titanium mesh combined with Medpor] Hua Xi Kou Qiang Yi Xue Za Zhi. 2015;33:272–275. doi: 10.7518/hxkq.2015.03.012. Chinese. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.He D, Li Z, Shi W, Sun Y, Zhu H, Lin M, et al. Orbitozygomatic fractures with enophthalmos: analysis of 64 cases treated late. J Oral Maxillofac Surg. 2012;70:562–576. doi: 10.1016/j.joms.2011.02.041. [DOI] [PubMed] [Google Scholar]
- 37.Yilmaz M, Vayvada H, Aydin E, Menderes A, Atabey A. Repair of fractures of the orbital floor with porous polyethylene implants. Br J Oral Maxillofac Surg. 2007;45:640–644. doi: 10.1016/j.bjoms.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 38.Lin IC, Liao SL, Lin LL. Porous polyethylene implants in orbital floor reconstruction. J Formos Med Assoc. 2007;106:51–57. doi: 10.1016/S0929-6646(09)60216-3. [DOI] [PubMed] [Google Scholar]
- 39.Cenzi R, Farina A, Zuccarino L, Carinci F. Clinical outcome of 285 Medpor grafts used for craniofacial reconstruction. J Craniofac Surg. 2005;16:526–530. doi: 10.1097/01.scs.0000168761.46700.dc. [DOI] [PubMed] [Google Scholar]
- 40.Yaremchuk MJ. Facial skeletal reconstruction using porous polyethylene implants. Plast Reconstr Surg. 2003;111:1818–1827. doi: 10.1097/01.PRS.0000056866.80665.7A. [DOI] [PubMed] [Google Scholar]
- 41.Gosau M, Schiel S, Draenert GF, Ihrler S, Mast G, Ehrenfeld M. [Craniofacial augmentation with porous polyethylene implants (Medpor): first clinical results] Mund Kiefer Gesichtschir. 2006;10:178–184. doi: 10.1007/s10006-006-0688-y. German. [DOI] [PubMed] [Google Scholar]
- 42.Menderes A, Baytekin C, Topcu A, Yilmaz M, Barutcu A. Craniofacial reconstruction with high-density porous polyethylene implants. J Craniofac Surg. 2004;15:719–724. doi: 10.1097/00001665-200409000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Romo T, 3rd, Litner JA, Sclafani AP. Management of the severe bulbous nasal tip using porous polyethylene alloimplants. Facial Plast Surg. 2003;19:341–348. doi: 10.1055/s-2004-815654. [DOI] [PubMed] [Google Scholar]
- 44.Emsen IM. E-M shaped septal encircling with Medpor reconstruction on crooked noses: personal technique and postoperative results. J Craniofac Surg. 2008;19:216–226. doi: 10.1097/scs.0b013e31815c9477. [DOI] [PubMed] [Google Scholar]