Abstract
Rationale:
Paraneoplastic cerebellar degeneration (PCD) is an immune-mediated neurological deficit affecting the cerebellum. Anti-Yo antibody positive PCD is a rare occurrence most likely associated with gynecologic or breast malignancies. The identification of the underlying tumor is a diagnostic challenge in many of these patients.
Patient concerns:
We present a 68-year-old woman with acute symptoms of PCD as a first sign of underlying occult malignancy. Further investigation revealed a positive anti-Yo antibody. Although brain magnetic resonance imaging (MRI) was unremarkable, positron emission tomography (PET)/computed tomography (CT) revealed intense hypermetabolism of cerebellum and diffused hypometabolism in the rest of brain. On 1-year follow-up, despite the primary malignancy is still unknown, her symptoms improved significantly after immunotherapy.
Diagnoses:
Paraneoplastic cerebellar degeneration.
Interventions:
The patient was given IV methylprednisolone 500 mg once a day for 5 consecutive days, followed by oral prednisone 60 mg once a day for 3 months.
Outcomes:
The patient's symptoms were gradually improved during the hospitalization period. On one year follow up, she was able to walk independently and perform some simple tasks.
Lessons:
Cerebellar hypermetabolism in PCD suspected patients may help confirming the diagnosis in an earlier stage and may predict a better outcome after immunotherapy.
Keywords: anti-yo antibody, breast cancer, hypermetabolism, paraneoplastic cerebellar degeneration
1. Introduction
Paraneoplastic neurological syndromes (PNS) are rare disorders that present in 1% to 3% of all cancer patients. These syndromes are a heterogeneous set of cancer-related neurologic diseases and it may involve any part of the nervous system. These disorders are associated with cancer, but not caused by a direct malignant tumor infiltration.[1] Paraneoplastic cerebellar degeneration (PCD) is a specific type of PNS, associated with various auto-antibodies, most commonly anti-Yo, which targets neurons and causes extensive loss of Purkinje cells of the cerebellum. Patients typically develop subacute cerebellar ataxia, dysarthria, diplopia, and vertigo, which often predate the cancer diagnosis.[2,3]
In patients with anti-Yo positive PCD, symptoms usually precede the detection of underling cancer by months to years in about 60% of the cases, but sometimes the diagnosis of a malignancy is made before the onset of symptoms.[1,4,5] As the disease progresses, only <10% of patients are able to ambulate without assistance over the long term, while the majority are left bedridden.[5] Cancer was detected in more than 90% of anti-Yo positive PCD patients, with breast and gynecological malignancies being the most common findings.[6]
Early identification and localization of the primary malignancy is essential for an early resection before the occurrence of metastases.[7] Positron emission tomography (PET) using 18F-fluorodeoxyglucose (FDG) is crucial in the early detection of the unknown primary tumors.[8] Most of the recently published studies had reported that positron emission tomography–computed tomography (PET/CT) has significantly high sensitivity and specificity for detecting primary malignancies, thereby high accuracy in confirming the diagnosis of PCD.[9]
PCD patients have poor prognosis with reduced survival rate; in addition, there is only little evidence of neurological improvement with the use of the current treatment strategies. As the occurrence of this syndrome is very rare, evidence-based guidelines for effective treatment still do not exist.[3,10]
Here, we present a case of 68-year-old woman presenting with acute symptoms of PCD as the first sign of occult malignancy. Anti-Yo antibody was detected in serum and cerebrospinal fluid (CSF). Her response to immunotherapy was very good and she had achieved significant improvement on 1-year follow-up. Through the detailed analysis of her course, we aim to bring your attention to the value of PET/CT in the diagnosis of PCD, and the potential effect of immunotherapy on the long-term outcome.
2. Case report
A 68-year-old woman presented with 4 weeks of progressive vertigo, disequilibrium, vertical nystagmus, and diplobia, which gradually worsened over a period of 6 months. On admission to our department, her general examination including breast examination was normal except for slightly enlarged right axillary lymph nodes. Her neurological examination showed alert and oriented patient with bilateral vertical nystagmus, severe ataxia, and positive cerebellar signs. Her medical history was unremarkable except for 10 years hypertension, which was controlled with levamilodipine 5 mg once a day. Enhanced head magnetic resonance imaging (MRI) was unremarkable (Fig. 1 A, B). CSF analysis was also normal. Anti-Yo antibody was detected in both serum and CSF. Thoracic and abdominal CT were performed, but no malignancy was detected. Mammography revealed bilateral cystic masses; breast ultrasound also showed 2 cystic masses and enlarged right axillary lymph nodes. Tumor markers were negative.
Figure 1.
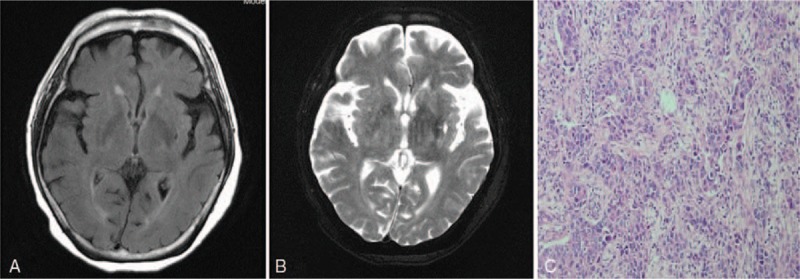
Transversal cranial MRI reveals no abnormal finding (A, B); Immunohistochemistry of right axillary lymph nodes reveals metastatic cancer cells from unknown origin (C).
In order to search for the underlying tumor, whole-body dual-modality PET/CT using [18F]-FDG was performed, which revealed intense hypermetabolism of cerebellum (SUVmax-8.5), with obviously diffused hypometabolism in the rest of the brain (SUV max-3.5) (Fig. 2 A, B); hypermetabolic right axillary lymph nodes (SUVmax-2.3) (Fig. 3: blue arrow; Fig. 2C) and significantly intense hypermetabolism in the lower-end of ileum (SUVmax-8.5) (Fig. 3: back arrow; Fig. 2D); however, no trace of hypermetabolism was detected in breast tissues (Fig. 3; Fig. 2C). As the metabolisms of right axillary lymph nodes were increased, a subsequent biopsy from the same region was taken for immunohistochemistry, which revealed a poorly differentiated metastatic cancer of unknown origin (Fig. 1C); thereafter, 2 bilateral breast biopsies were collected; however, the result did not reveal any sign of cancerous change. Unexpectedly, the metabolism of the lower-end of ileum was also significantly increased, therefore colonoscopy was performed, and an ulcer was found; however, a subsequent immunohistochemistry of intestinal (ulcer) biopsy did not show a malignant change as well. On the basis of these findings and the diagnostic criteria,[3] the diagnosis of anti-Yo PCD associated with intestinal malignancy was highly suspected. The patient was given intravenous (IV) methylprednisolone 500 mg once a day for 5 consecutive days, followed by oral prednisone 60 mg once a day for 3 months as well as other supportive therapies; her symptoms were gradually improved, and then she was discharged. On 1-year follow up, she was able to walk independently and perform some simple tasks. Unfortunately, due to the bad financial condition of her family, they could not afford to pay for any further follow-up imaging studies.
Figure 2.
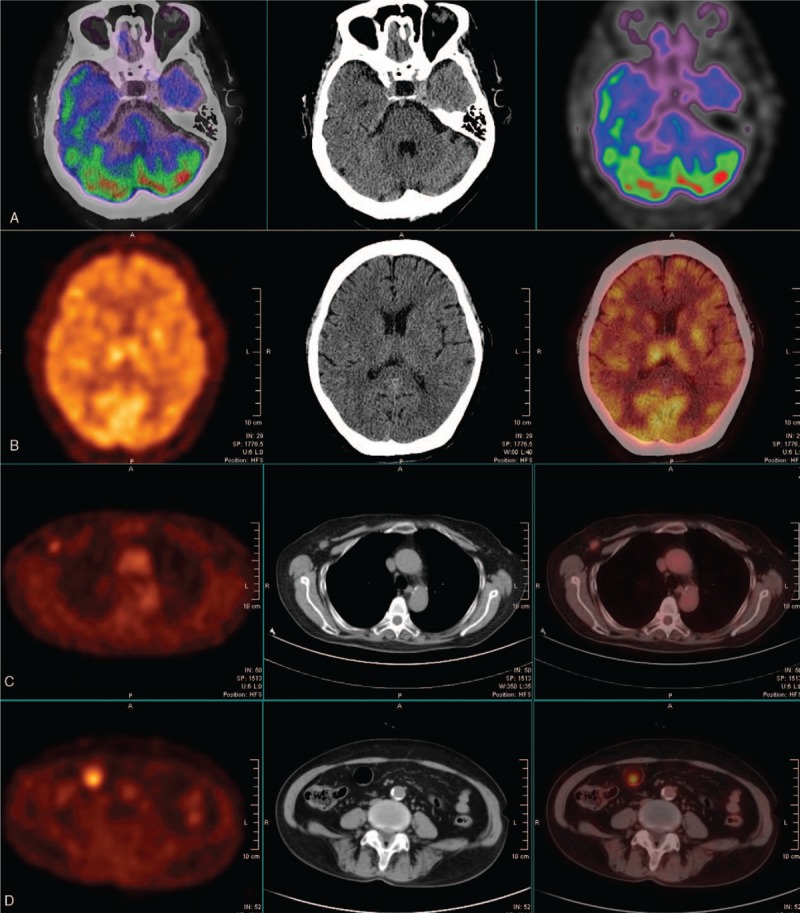
PET/CT images show intense metabolic activity in the cerebellum associated with hypometabolism in the rest of brain (A, B); Right-sided axillary lymph nodes hypermetabolism with the absence of breast tissue hypermetabolism (C); significant metabolic activity in the intestine (D).
Figure 3.
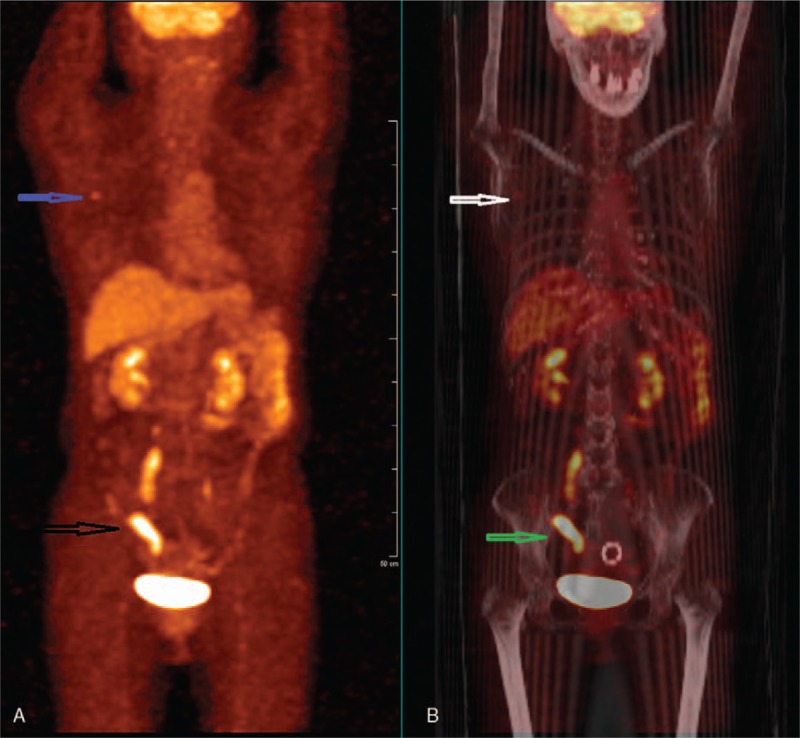
FDG-PET (A) reveals abnormal hot spots in the pelvic (black arrow) and axillary (blue arrow) regions. Coronal PET-CT (B) demonstrates abnormal increased glucose utilization in 2 different regions (white arrow indicates right axillary lymph node hypermetabolism; green arrow indicates significant intestinal hypermetabolism).
3. Discussion
Paraneoplastic cerebellar degeneration typically presents with subacute cerebellar deficits over a period of weeks or months. These deficits include ataxia, nystagmus, dysmetria, dysarthria, vertigo, and diplopia in the absence of brain metastases or central nervous system (CNS) tumor involvement. The syndrome progresses over a period of weeks to months, with probably all patients reaching a plateau in symptoms’ severity within 6 months from the onset of symptoms.[2] Most of these patients are seen in wheelchair or bed-bound during this time. Our patient had progressive vertigo, disequilibrium, vertical nystagmus, and diplobia, which gradually worsened over a period of 6 months. Her symptoms exacerbated over this period to the point of being completely bedridden.
The past medical history, clinical examination, neuroimaging, and laboratory studies help to differentiate PCD from other conditions.[5] Brain MRI and CT are often normal at disease onset and they are not helpful for positive diagnosis of PCD, but essential to exclude metastatic, demyelinating, and cerebrovascular diseases. Sometimes, MRI can reveal cerebellar atrophy in advanced cases.[2,11] In our patient, thoracic and abdominal CT, as well as enhanced brain MRI were unremarkable.
PCD is a rare but devastating paraneoplastic neurologic syndrome most commonly associated with breast and gynecological cancers but has also been found to be associated with Hodgkin lymphoma, small cell lung cancer, gastric cancer, esophageal cancer, prostate cancer, bladder cancer, and melanoma.[2,3] There are at least 12 auto-antibodies that have been reported to be associated with PCD; anti-Yo antibody was the most commonly detected antibody.[2,3] Interestingly, our patient had a positive anti-Yo antibody in both serum and CSF, but none of the previously mentioned cancers were detected.
It has been reported that FDG PET/CT is a highly accurate diagnostic modality for detecting underling primary tumor in PNS-suspected patients.[7,9,10] Although our patient had typical clinical features and a positive anti-Yo antibody, no malignancy was found after comprehensive medical evaluation. Therefore, whole-body dual-modality PET/CT was performed, which revealed intense metabolic activity in the cerebellum associated with diffused hypometabolism in the rest of the brain (Fig. 2A, B). In few recently reported PCD cases, it was noticed that beside the detection of underlying tumors by PET/CT, cerebellar hypermetabolism was founded as well,[12–14] which is consistent with our finding. Choi et al[14] had reported that the inflammatory process induced by an immune reaction in the acute stage may give rise to cerebellar hypermetabolism in PCD patients. So, we suggest that this interesting finding could be used in the future as an imaging biomarker to confirm the diagnosis in PCD suspected patients. Further studies are required to clarify its efficacy in the diagnosis of PCD suspected cases. It was previously reported that the time between disease onset and the detection of primary tumor in Ab-positive patients might be as long as 8 years.[15] In our patient, the primary tumor is still unknown even after performing PET/CT, so further follow-up is required to detect the primary occult cancer.
The underling pathogenic mechanism of PCD is still not clearly understood; it has been found that anti-Yo antibody targets a cytoplasmic antigen in the Purkinje cells of the cerebellum, resulting in extensive destruction of Purkinje cells.[5,11] PCD is believed to be caused by an autoimmune reaction against antigen overexpressed by tumor cells and neurons. In addition to humoral response, cellular response appears to play an important role in the pathogenetic mechanism[5,11]; therefore, various types of treatments had been tried to inhibit or modulate the immune response. Several recently published cases have reported that immunotherapy may improve the associated neurological disorder, which hence improves the patient's survival rate and quality of life.[3,5,11] Our patient had a significant improvement on 1-year follow-up after immunotherapy, which is consistent with the previously published data. On the basis of the follow-up results of our patient, we presume that the presence of cerebellum hypermetabolism on PEC/CT may help to confirm the diagnosis of PCD in an earlier stage.
4. Conclusion
PCD is a rare but devastating neurological disorder most commonly associated with malignancies, many of them are occult primary tumors.
The detection of anti-Yo antibody strongly support the diagnosis of PCD in patients with neurological deficit. Immunotherapy is potentially important for the management of PCD.
Cerebellar hypermetabolism in PCD-suspected patients may help confirm the diagnosis in an earlier stage and may predict better outcomes after immunotherapy.
Author contributions
Conceptualization: Ammar Taha Abdullah Abdulaziz, Le Zhang, Xin Yue Jiang.
Data curation: Ammar Taha Abdullah Abdulaziz, Xiao Qing Yu, Xin Yue Jiang.
Writing – original draft: Ammar Taha Abdullah Abdulaziz.
Writing – review & editing: Dong Zhou, Jin Mei Li.
Footnotes
Abbreviations: CNS = central nervous system, CSF = cerebrospinal fluid, CT = computed tomography, FDG = fluorodeoxyglucose, IV = intravenous, MRI = magnetic resonance imaging, PCD = paraneoplastic cerebellar degeneration, PET/CT = positron emission tomography–computed tomography, PET = positron emission tomography, PNS = paraneoplastic neurological syndrome, SUV = standardized uptake value.
This case report was approved by the Ethical Committee of West China Hospital, Sichuan University. Written informed consent to publish this case was obtained from the patient.
The authors declare no financial or other conflicts of interest.
References
- [1].Dalmau J, Rosenfeld MR. Paraneoplastic syndromes of the CNS. Lancet Neurol 2008;7:327–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Peterson K, Rosenblum MK, Kotanides H, et al. Paraneoplastic cerebellar degeneration. I. A clinical analysis of 55 anti-Yo antibody-positive patients. Neurology 1992;42:1931–7. [DOI] [PubMed] [Google Scholar]
- [3].Shams’ili S, Grefkens J, de Leeuw B, et al. Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: analysis of 50 patients. Brain 2003;126:1409–18. [DOI] [PubMed] [Google Scholar]
- [4].Lorusso L, Hart IK, Giometto B, et al. Immunological features of neurological paraneoplastic syndromes. Int J Immunopathol Pharmacol 2004;17:135–44. [DOI] [PubMed] [Google Scholar]
- [5].Rojas I, Graus F, Keime-Guibert F, et al. Long-term clinical outcome of paraneoplastic cerebellar degeneration and anti-Yo antibodies. Neurology 2000;55:713–5. [DOI] [PubMed] [Google Scholar]
- [6].Graus F, Delattre JY, Antoine JC, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 2004;75:1135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Giannopoulou C. Navigating the paraneoplastic neurological syndromes. Eur J Nucl Med Mol Imaging 2003;30:333–8. [DOI] [PubMed] [Google Scholar]
- [8].Rees JH, Hain SF, Johnson MR, et al. The role of [18F]fluoro-2-deoxyglucose-PET scanning in the diagnosis of paraneoplastic neurological disorders. Brain 2001;124:2223–31. [DOI] [PubMed] [Google Scholar]
- [9].Vatankulu B, Yilmaz Aksoy S, Asa S, et al. Accuracy of FDG-PET/CT and paraneoplastic antibodies in diagnosing cancer in paraneoplastic neurological syndromes. Rev Esp Med Nucl Imagen Mol 2016;35:17–21. [DOI] [PubMed] [Google Scholar]
- [10].Greenlee JE. Treatment of paraneoplastic neurologic disorders. Curr Treat Options Neurol 2010;12:212–30. [DOI] [PubMed] [Google Scholar]
- [11].Finsterer J, Voigtlander T, Grisold W. Deterioration of anti-Yo-associated paraneoplastic cerebellar degeneration. J Neurol Sci 2011;308:139–41. [DOI] [PubMed] [Google Scholar]
- [12].Sharma P, Mazumdar B, Chatterjee P. Cerebellar hypermetabolism on 18F-FDG PET/CT with normal MRI in a case of paraneoplastic cerebellar degeneration with negative antibodies. Rev Esp Med Nucl Imagen Mol 2015;34:79–80. [DOI] [PubMed] [Google Scholar]
- [13].Gheysens O, Deroose CM, Tousseyn T, et al. Hodgkin lymphoma-associated paraneoplastic cerebellar degeneration on FDG-PET/CT. Br J Haematol 2014;164:468. [DOI] [PubMed] [Google Scholar]
- [14].Choi KD, Kim JS, Park SH, et al. Cerebellar hypermetabolism in paraneoplastic cerebellar degeneration. J Neurol Neurosurg Psychiatry 2006;77:525–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lucchinetti CF, Kimmel DW, Lennon VA. Paraneoplastic and oncologic profiles of patients seropositive for type 1 antineuronal nuclear autoantibodies. Neurology 1998;50:652–7. [DOI] [PubMed] [Google Scholar]


