Abstract
A 39-year-old male fell from a forklift and was urgently transported to our hospital. His vital signs were stable at the initial visit. Contrast imaging computed tomography (CT) showed extravasation (Ev) of contrast medium emigrating outside of the renal capsule and hematoma around the right kidney, and he was diagnosed with traumatic right renal injury, Grade IV laceration [American Association for the Surgery of Trauma classification]. When imaging the inferior renal artery branch extremity perfusing the area where Ev was found in the following blood vessel contrast imaging, obvious Ev was not found in the arterial phase; however, massively spreading Ev was found in the area adjacent to the renal laceration in the venous phase after taking a contrast image of the renal parenchyma. Thus, he was diagnosed with a renal vein branch injury. The transcatheter arterial embolization (TAE) was performed to the area, resulting in the disappearance of Ev.
The effectiveness of TAE for renal injury has been established; however, it is only performed for arterial hemorrhage. TAE for venous injury has not previously been considered because a tamponade is supposedly effective for hemostasis of venous hemorrhage due to the anatomy surrounding Gerota's fasciae. This is an extremely rare case in which only venous injury was identified, without obvious arterial hemorrhage. Gerota's fasciae were broken and hemostasis treatment was required. Because the renal artery is the end artery, the venous hemorrhage was controlled with arterial embolization.
In our case, renal vein branch injury was identified on CT and hemorrhage was terminated using TAE for the renal artery branch. TAE can be used as a non-operative management for the successful treatment of renal vein branch injury.
Keywords: Non-operative management, Renal vein branch injury, Transcatheter arterial embolization, Venous hemorrhage
Introduction
Renal injuries account for 8%–10% of all blunt abdominal traumas and are the third major type of abdominal organ injuries after liver and spleen injuries [1]. The kidney is a retroperitoneal organ, and given the anatomical characteristics of Gerota's fasciae, many cases of renal hemorrhage are controlled with a tamponade [2]. Reports on treatment strategies and hemorrhage control for venous hemorrhages are rare, except for renal vein damage with renal pedicle injury [3]. Despite clear arterial hemorrhage, we detected and reported on an extremely rare case of traumatic renal injury with renal vein branch injury as the main hemorrhage origin, as determined by contrast imaging computed tomography (CT) and angiography.
Case-report
A 39-year-old male fell from a forklift, hit his right abdominal area hard, and suffered injuries. Pain gradually worsened, and he was urgently transported to our hospital on the same day. Bruises and tenderness were observed in the right back area only, and his vital signs were stable [respiratory rate was 20 breaths per minute, SpO2 was 98% (room air), blood pressure was 96/50 mmHg, pulse was 70 beats per minute, and awareness was 15 points according to the Glasgow coma scale]. No abnormal findings were detected on chest or pelvis X-ray. A hematoma was revealed around the right kidney on focused assessment with sonography for trauma, so we performed contrast imaging CT. An inferior extremity laceration of the right kidney and hematoma flowing outside of Gerota's fasciae were revealed. Consequently, the patient was diagnosed with a Grade IV laceration (American Association for the Surgery of Trauma classification). The volume of hemorrhage from the hematoma was relatively heavy; however, on imaging, no obvious extravasation of the contrast medium was observed in the early phase, but a delayed extravasation faintly spreading within the hematoma was observed in the delay phase. This delayed extravasation was not considered a symptom of ureteral injury as differing from the timing of the excretory phase (Fig. 1a/b). Angiography was performed for closure treatment. Extravasation from the arteries was not observed in the right kidney artery on imaging (Fig. 2a); however, similar to the findings of the contrast imaging CT, slow extravasation of the contrast medium from the lacerated kidney area was observed after taking a contrast image of the renal parenchyma. Thus, the patient was diagnosed with renal vein branch injury (Fig. 3a/b/c).
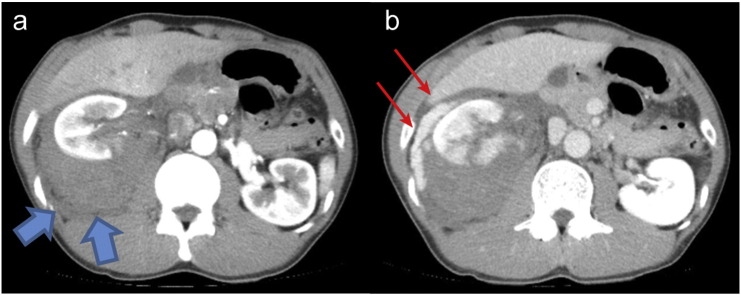
Fig. 1.
Contrast imaging CT at the initial visit (a: Arterial phase, b: Venous phase).
A massive hematoma (⇒) in an inferior extremity laceration of the right kidney and around the right kidney was found, and hematoma was partially found in the abdominal cavity. Obvious extravasation of contrast medium was not found in the early phase (a); however, a massive amount of contrast medium (→) emigrating into the hematoma was found in the delay phase, and hemorrhage continued (b).
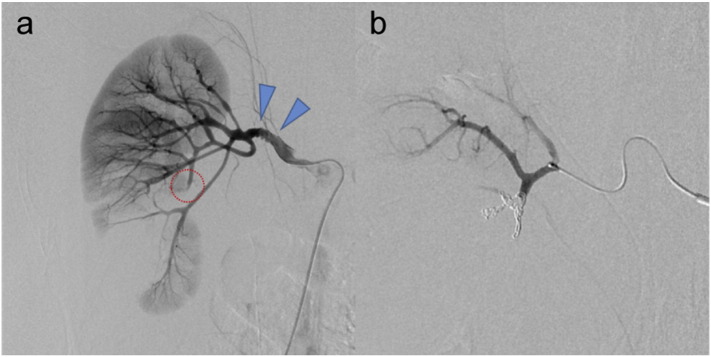
Fig. 2.
Angiography of the right renal artery (a: An image from the stem of the right renal artery, b: After coil embolization).
Obvious extravasation of contrast medium was not found in the arterial phase (a); however, a blood vessel injury was suspected due to an image of a blocked blood vessel in the branch artery flowing into the laceration area of the inferior extremity of the kidney (◌). A microcatheter was used to locate the area and embolize the area with coils (b). An extremely irregular and slight stricture was found in the stem of the renal artery (△), and it was assumed to be a blood vessel injury. After the follow-up, these findings were not observed on CT image.
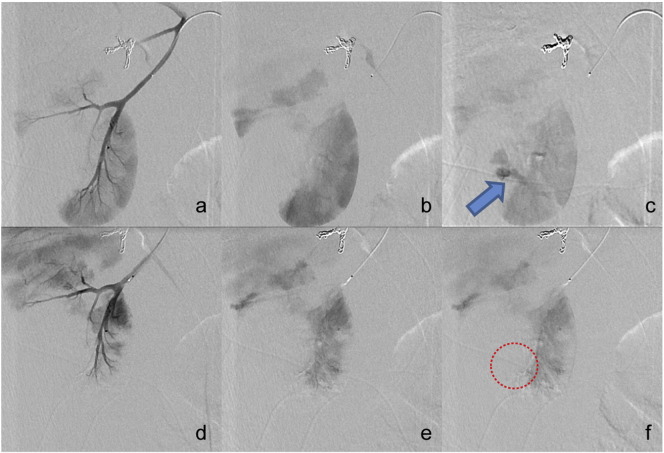
Fig. 3.
Endovascular surgery of the renal vein branch injury (a/b/c: Before TAE, d/e/f: After TAE).
After coil embolization and taking an image while moving a microcatheter toward to the inferior extremity, no extravasation of contrast medium was found in the arterial phase (a). Renal parenchymal was subsequently dyed (b), and the contrast medium (⇒) was found to emigrate from the renal laceration in the venous phase (c). Selectively moving a microcatheter further toward the inferior extremity, TAE was performed with a gelatin sponge on the overall perfused area. In the image taken after embolization, peripheral blood flow of the embolized area decreased (d), an image of the renal parenchymal was taken in the same way as B (e), and the extravasation image of contrast medium found in the venous phase before the embolization disappeared (◌) (f).
Firstly, to assist with the diagnosis of vascular injury, a transcatheter arterial embolization (TAE) was performed using coils because the renal artery branch abutting the lacerated kidney area was irregularly interrupted (Fig. 2b). As for the renal vein branch injury, TAE was performed using a gelatin sponge because extravasation of contrast medium outside of the blood vessels was confirmed during the vein phase while selectively taking a contrast image of the bifurcation of the inferior renal artery corresponding to the damaged area. After TAE, the extravasation disappeared (Fig. 3d/e/f).
Later, the ureteral stent was indwelled and conservative treatment was continued. The patient was discharged on the 26th day of illness.
Discussion
Nowadays, many renal injuries are treated with non-operative management (NOM). NOM provides potential for greater diagnostic accuracy due to the dissemination of initial treatment guidelines for traumatic diagnosis, establishment of treatment strategies, progress of imaging diagnosis, and interventional radiography (IVR). These elements allow patients with unstable hemodynamics, for whom only conventional surgery would traditionally have been considered, to undergo TAE [4]. This benefits kidney conservation with the use of a renal artery stent for damaged renal pedicle [5].
The multidetector CT (MDCT) has become a necessary diagnostic tool for serious traumatic treatments [6], in which the damaged area and damaged figure can be better understood, thereby helping to determine the correct treatment, namely conventional surgery or NOM [7]. By taking separate images in the arterial, venous, and excretory phases, we can diagnose arterial hemorrhage, venous hemorrhage, or urinary fistula. However, renal blood flows through the somatic, lobar arterial, interlobar, arcuate, interlobar hepatic, afferent, and efferent arteries, perfuses them through the venous system, and flows into the inferior vena cava. Veins run through each branch artery, and blunt injuries with renal parenchymal laceration generally tend to combine both and represent quite complicated damage. Thus, it is not easy to distinguish arterial hemorrhage as venous hemorrhage or expanded extravasation as time elapses. However, this is generally not considered a clinical issue, perhaps due to the flowing reasons: (1) when Gerota's fasciae is maintained, many venous hemorrhages can be naturally discontinued with the tamponade effect under low pressure, and (2) when arterial hemorrhage and extravasation of contrast medium in the CT image are found together, TAE can be performed for hemostasis in the acute period. In addition, even if venous hemorrhage is found, venous hemorrhage is unintentionally controlled by TAE, as with our patient. In this case, we predicted that some hemostasis was required as Gerota's fasciae were broken and hemorrhage was observed in the abdominal cavity. Because the renal artery is the end artery, venous blood flow depends on the perfused arteries. Thus, even with the venous injury, it was easy to terminate the bleeding in such areas by embolizing the perfused renal artery branches.
Past reports on the extravasation of contrast medium only in the renal artery branch despite no arterial hemorrhage do not exist, which makes this case extremely rare. This is possibly because of the following reasons: (1) arterial damage not being found simultaneously because the arterial matches with the tangential direction of the renal laceration, or (2) the combined damage of the arterial branch was found; however, the arterial hemorrhage was naturally controlled. The former possibility is unlikely because a rupture of blood vessels in the renal artery branch adjacent to the renal damage area was found and a coil embolism was required. Some reports [8], [9] have stated that 1%–4% of blunt abdominal trauma involves thrombus imperforation with renal vessel injury. Combined damage in the partial artery branch of the perfused area to the venous branch injury was found instead; however, it may have been assumed that the arterial hemorrhage was controlled with the thrombus formation.
Conclusion
In this renal vein branch injury patient, hemorrhage stopped with TAE treatment of the renal artery perfusing the damaged area. Because a tamponade was not effective due to the patient's broken Gerota's fasciae, a positive hemostasis was required; however, it was easy to terminate the bleeding with TAE to the renal artery branch in the perfused area. Thus, TAE is an effective NOM for the treatment of renal vein branch injury.
Conflict of interest statement
There are no conflicts of interest to declare, and the report did not receive any funding.
Acknowledgements
The authors would like to thank Enago (www.enago.jp) for the English language review.
References
- 1.Baverstock R., Simons R., McLoughlin M. Severe blunt renal trauma: a 7-year retrospective review from a provincial trauma centre. Can. J. Urol. 2001;8:1372–1376. [PubMed] [Google Scholar]
- 2.Charbit J., Manzanera J., Millet I. What are the specific computed tomography scan criteria that can predict or exclude the need for renal angioembolization after high-grade renal trauma in a conservative management strategy? J. Trauma. 2011;70:1219–1227. doi: 10.1097/TA.0b013e31821180b1. [DOI] [PubMed] [Google Scholar]
- 3.Sturm J.T., Perry J.F., Jr., Cass A.S. Renal artery and vein injury following blunt trauma. Ann. Surg. 1975;182:696–698. doi: 10.1097/00000658-197512000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsumoto J., Lohman B.D., Morimoto K. Damage control interventional radiology (DCIR) in prompt and rapid endovascular strategies in trauma occasions (PRESTO): a new paradigm. Diagn. Interv. Imaging. 2015;96:687–691. doi: 10.1016/j.diii.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Kushimoto S., Shiraishi S., Miyauchi M. Traumatic renal artery occlusion treated with an endovascular stent–the limitations of surgical revascularization: report of a case. Surg. Today. 2011;41:1020–1023. doi: 10.1007/s00595-010-4368-z. [DOI] [PubMed] [Google Scholar]
- 6.Huber-Wagner S., Lefering R., Qvick L.M. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet. 2009;25:1455–1461. doi: 10.1016/S0140-6736(09)60232-4. [DOI] [PubMed] [Google Scholar]
- 7.Szmigielski W., Kumar R., Al Hilli S. Renal trauma imaging: diagnosis and management. A pictorial review. Pol. J. Radiol. 2013;78:27–35. doi: 10.12659/PJR.889780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haas C.A., Dinchman K.H., Nasrallah P.F. Traumatic renal artery occlusion: a 15-year review. J. Trauma. 1998;45:557–561. doi: 10.1097/00005373-199809000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Jawas A., Abu-Zidan F.M. Management algorithm for complete blunt renal artery occlusion in multiple trauma patients: case series. Int. J. Surg. 2008;6:317–322. doi: 10.1016/j.ijsu.2008.05.004. [DOI] [PubMed] [Google Scholar]