Abstract
A 24 year old male arrived to our hospital after a motor cycle crash with evidence of a traumatic brain injury and in hemorrhagic shock not responsive to volume administration. Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) was performed in a timely fashion using a new, low profile, wire free device. This lead to rapid reversal of hypotension while his bleeding source was sought and controlled.
Recently, REBOA has emerged as an adjunct in the hypotensive trauma patient with noncompressible torso hemorrhage. As first described, this procedure makes use of commonly available vascular surgery and endovascular products requiring large introducer sheaths (12–14 French) and long guidewires. Concerns regarding this technique center around the safety and feasibility of using such equipment in the emergency setting outside an angiography suite. This has likely limited widespread adoption of this technique. To address these concerns, newer products designed to be placed through a smaller sheath (7 French) and without the use of guidewires have been developed. Here we report on our first clinical use of such a device that we believe represents a significant advance in the care of the trauma patient.
Keywords: REBOA, Resuscitation, Hemorrhage, Endovascular
Introduction
First described in the 1950s, Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) has emerged as a viable treatment modality for non-compressible torso hemorrhage in trauma patients [1], [2], [3], [4]. The goal of REBOA is to obtain aortic occlusion via a common femoral artery access site thus decreasing hemorrhage volume and preserving perfusion to the heart and brain. While this technique has the potential to reduce the need for resuscitative thoracotomy, commonly used devices require large introducer sheaths (12 French or greater) risking significant vascular injury and requiring formal surgical repair of the femoral artery upon removal [2]. Furthermore, the requirement for long guidewires makes the procedure cumbersome anywhere other than an angiography suite. It is likely that the requirement for placing such large sheaths under emergency circumstances in addition to the need for cumbersome guidewires has inhibited the wide adoption of this technique. However, recently approved devices designed to deploy through smaller 7 French sheaths without the need for cumbersome guidewires have become available [5]. In this report, we describe our first experience with a new, low profile, wire free system (Fig. 1).
Fig. 1.
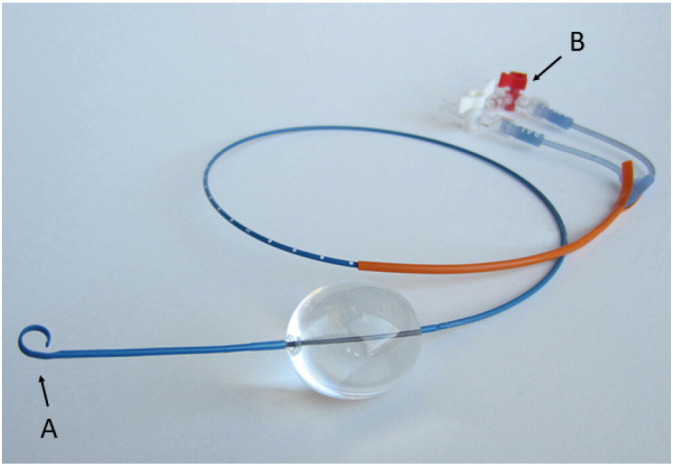
ER-REBOA catheter (Prytime Medical, Boerne TX). A: The “P-tip” on the end of the catheter allows for wire free placement. B: Two ports are present, one for balloon inflation and deflation, one for arterial waveform monitoring proximal to the balloon.
Image courtesy of Prytime Medical.
Case
The patient is a 24 year old male transported to our American College of Surgeons designated Level One trauma center after a motorcycle crash. Per report he was found moaning with a palpable carotid pulse but no obtainable blood pressure in the field. On arrival in the trauma bay, he was unresponsive with a Glasgow Coma Score (GCS) of 3. Breath sounds were diminished on the left and he had a palpable carotid pulse. His heart rate (HR) was 165 beats per minute (bpm). We were unable to obtain a blood pressure (BP). A large Zone 2 soft tissue defect on anterior left neck was hemostatic and his right femur was grossly deformed. Intravenous access was quickly obtained, the patient was intubated, a left tube thoracostomy was performed returning air and 50 ml of blood. The massive transfusion protocol was initiated. Vital signs after 2 units of RBCs and 2 units of plasma were HR of 100 bpm and a BP of 63/36 mm Hg. Chest radiography showed adequate thoracostomy tube placement and no evidence of retained hemothorax or mediastinal widening. A Focused Abdominal Sonography for Trauma (FAST) exam was negative and pelvis X-ray showed no fractures. Since the patient remained severely hypotensive without evidence of blunt aortic injury, REBOA in Zone 1 (Fig. 2) was indicated according to the algorithm described by Moore et al. [3]. Under ultrasound guidance, the left common femoral artery was accessed using a 21 gauge micropuncture kit (Cook Medical, Bloomington IN), a 7 French introducer sheath (Terumo Medical, Somerset NJ) was placed and the guidewire and dilator were removed. Using surface landmarks, an insertion depth of 44 cm was planned. An ER-REBOA catheter (Prytime Medical, Boerne TX) was placed through the 7 French sheath to a depth of 44 cm. Intra-aortic placement was confirmed with chest radiography (Fig. 3) and the balloon was inflated with 15 ml saline until loss of contralateral femoral pulse. The blood pressure showed immediate improvement to 118/98 mm Hg. With improved blood pressure, the neck wound was noted to be bleeding and pressure was applied. The patient was taken directly to the operating room for neck exploration and exploratory laparotomy.
Fig. 2.
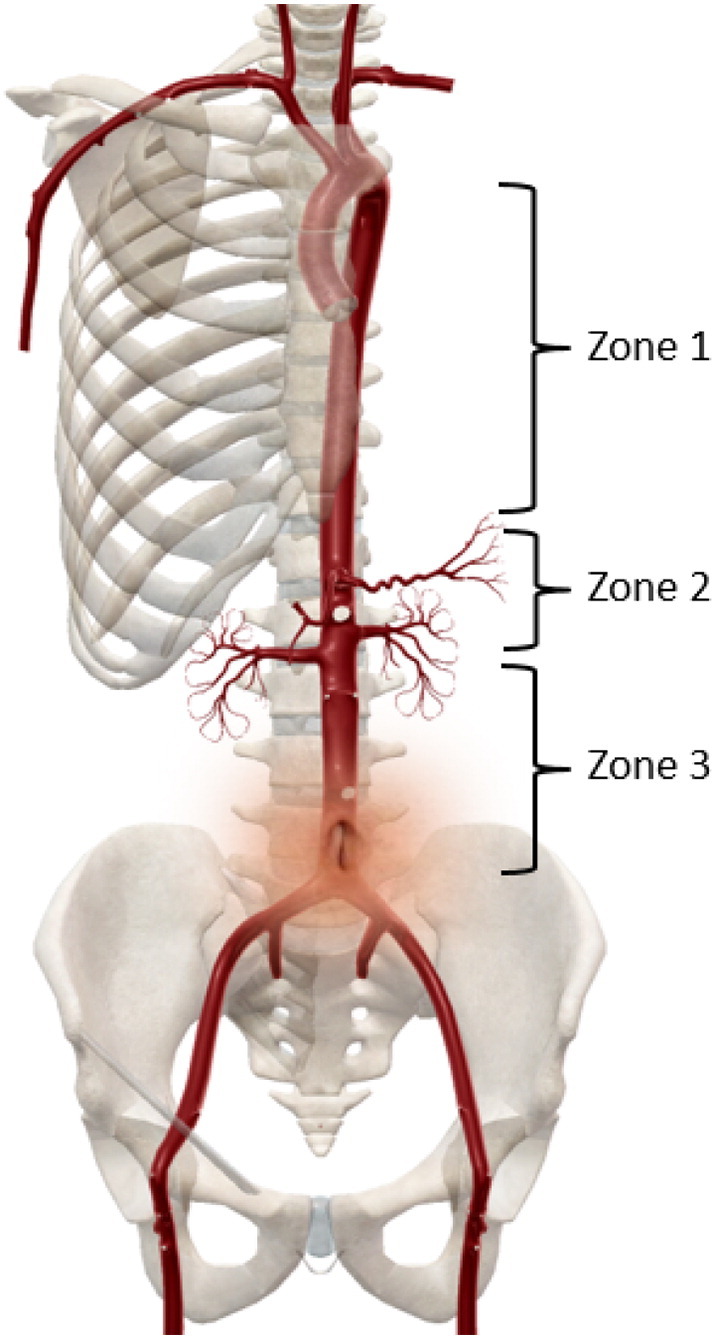
Aortic zones for REBOA placement with overlying surface landmarks. Zone 1: descending aorta above the celiac artery. Zone 2: Abdominal aorta between celiac artery and lowest renal artery. Zone 3: Abdominal aorta between lowest renal artery and aortic bifurcation. Zone 1 surface landmark is the xiphoid process. Zone 3 surface landmark is the umbilicus.
Image courtesy of Visible Body (www.visiblebody.com).
Fig. 3.
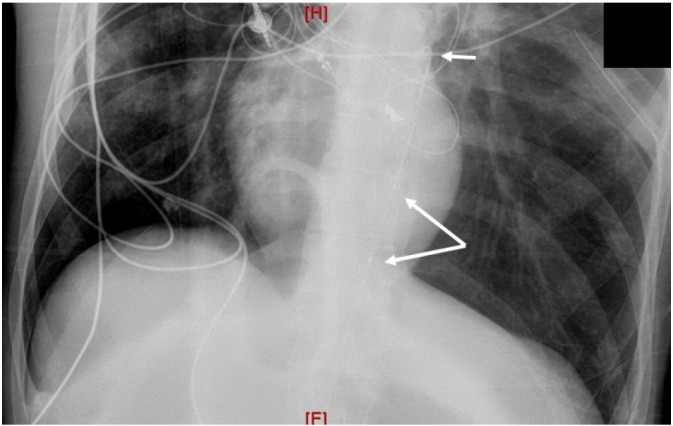
Chest X-ray showing Zone 1 ER-REBOA (Prytime Medical, Boerne TX) placement. Note “P-tip” of catheter for wire free placement (short arrow) and superior and inferior boarder of balloon (long arrows).
In the operating room, the patient was found to have bleeding from superficial neck veins that were ligated. Laparotomy was negative for intraperitoneal or retroperitoneal bleeding. In conjunction with our anesthesia colleagues the ER-REBOA balloon was slowly deflated resulting in profound hypotension that recovered with re-inflation of the balloon. A transesophageal echocardiogram was performed noting no pericardial effusion and good function without wall motion abnormality. After further volume administration, the REBOA balloon was successfully deflated without hemodynamic compromise. However, during closure of the laparotomy, hypotension recurred and thoracostomy tube output was noted to be nearly 1 l of frank blood. The left chest was explored and the patient found to have ongoing bleeding from soft tissue destruction secondary to multiple displaced posterior rib fractures and costovertebral joint disruptions. This was controlled with packing.
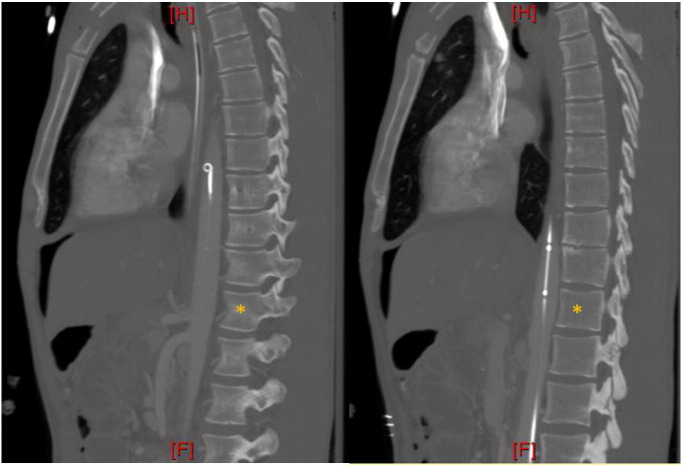
Postoperatively, patient was taken for computed tomography (CT) with the deflated ER-REBOA catheter serving as his arterial line for monitoring (Fig. 4). Imaging diagnosed a severe traumatic brain injury (TBI). CT angiography of the abdomen with runoff showed no complications from femoral artery access or ER-REBOA balloon inflation. The patient was transported to the intensive care unit for further resuscitation. The ER- REBOA catheter and the 7 French sheath were removed and pressure held for 30 min. The patient had symmetric and bounding pedal pulses. The peak lactate was 5.8 mmol/l from his trauma bay blood sample. Peak creatinine was 0.92 mg/dl, and his liver function tests remained normal. The patient was discharged to a long term care facility with a GCS of 6T.
Fig. 4.
Computed tomography. A: showing the “P-tip” of the ER-REBOA catheter (Prytime Medical, Boerne TX) for wire free insertion. B: the radio-opaque markers of the balloon, deflated and resting in Zone 1 above celiac artery. Asterisks denotes T12 vertebral body.
Discussion
In this case report, we describe the use of a new, low profile, REBOA device designed to be inserted without a guidewire through a 7 French introducer sheath. The procedure entails gaining common femoral artery access with a 7 French sheath followed by placing the ER-REBOA device through the sheath with no need for a guidewire due to the integrated “P-tip” on the ER-REBOA device (Fig. 1). This two-step process is an improvement over our previous technique using a 12 French sheath and a Coda balloon (Cook Medical, Bloomington IN) necessitating a much larger sterile area, a cumbersome 260 cm guidewire that must remain in place, and the eventual need for surgical repair of the arteriotomy. In our first clinical use of this device, aortic occlusion was achieved less than 3 min after arterial puncture, the rate limiting step being chest X-ray to confirm correct placement. The ER-REBOA catheter self-guided into the aorta as designed without the use of a guidewire.
After obtaining hemostasis and regaining hemodynamic stability, our patient was diagnosed with a severe traumatic brain injury. In patients with severe TBI, prevention of secondary injury by avoiding hypotension and hypoxia is key to early management [6]. A single episode of hypotension in patients with severe TBI has been shown increase mortality up to two fold. The prognosis becomes even worse with multiple, or prolonged episodes of hypotension [7]. While our patient did suffer a severe TBI, the ability to quickly obtain occlusion of the aorta lead to a relatively shorter duration of his hypotension than would have occurred with traditional resuscitation methods; and potentially improved chances of survival and neurologic function.
Once femoral access was obtained, the rate limiting step in obtaining occlusion of the aorta was the need for chest X-ray to confirm intra-aortic placement of the ER-REBOA catheter. While some propose REBOA devices can be placed without confirmation of intra-aortic positioning, we feel that step remains important until more data are available [8]. One method to further reduce the time it takes to obtain occlusion of the aorta is to confirm intra-aortic placement by ultrasound rather than X-ray. Ultrasound is readily available in the trauma bay, and, in unstable patients, often already in use performing a FAST exam. Early work has shown ultrasound use for intra-aortic guide wire confirmation and Zone 3 balloon deployment is feasible [9], [10]. However, more work is needed to show ultrasound offers an advantage to X-ray or fluoroscopy in terms of accuracy or procedure duration.
In conclusion, we feel that a REBOA balloon that can be placed without guidewires through a lower profile 7 French introducer sheath offers an improvement in both the time it takes to achieve occlusion of the aorta and the morbidity associated with the arterial entry site. While we believe imaging confirmation of intra-aortic REBOA balloon placement is necessary, ultrasonography is an attractive alternative to radiography.
References
- 1.Hughes C.W. Use of an intra-aortic balloon catheter tamponade for controlling intra-abdominal hemorrhage in man. Surgery. 1954;36(1):65–68. [PubMed] [Google Scholar]
- 2.Stannard A., Eliason J.L., Rasmussen T.E. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as an adjunct for hemorrhagic shock. J. Trauma. 2011;71(6):1869–1872. doi: 10.1097/TA.0b013e31823fe90c. [DOI] [PubMed] [Google Scholar]
- 3.Moore L.J., Brenner M., Kozar R.A., Pasley J., Wade C.E., Baraniuk M.S. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J. Trauma Acute Care Surg. 2015;79(4):523–530. doi: 10.1097/TA.0000000000000809. (discussion 30-2) [DOI] [PubMed] [Google Scholar]
- 4.Martinelli T., Thony F., Declety P., Sengel C., Broux C., Tonetti J. Intra-aortic balloon occlusion to salvage patients with life-threatening hemorrhagic shocks from pelvic fractures. J. Trauma. 2010;68(4):942–948. doi: 10.1097/TA.0b013e3181c40579. [DOI] [PubMed] [Google Scholar]
- 5.Belenkiy S.M., Batchinsky A.I., Rasmussen T.E., Cancio L.C. Resuscitative endovascular balloon occlusion of the aorta for hemorrhage control: past, present, and future. J. Trauma Acute Care Surg. 2015;79(4 Suppl. 2):S236–S242. doi: 10.1097/TA.0000000000000770. [DOI] [PubMed] [Google Scholar]
- 6.Bratton S.L., Chestnut R.M., Ghajar J., McConnell Hammond F.F., Harris O.A., Hartl R. Guidelines for the management of severe traumatic brain injury. I. Blood pressure and oxygenation. J. Neurotrauma. 2007;24(Suppl. 1):S7–13. doi: 10.1089/neu.2007.9995. [DOI] [PubMed] [Google Scholar]
- 7.Manley G., Knudson M.M., Morabito D., Damron S., Erickson V., Pitts L. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch. Surg. (Chicago, IL: 1960) 2001;136(10):1118–1123. doi: 10.1001/archsurg.136.10.1118. [DOI] [PubMed] [Google Scholar]
- 8.Scott D.J., Eliason J.L., Villamaria C., Morrison J.J., Houston R., Spencer J.R. A novel fluoroscopy-free, resuscitative endovascular aortic balloon occlusion system in a model of hemorrhagic shock. J. Trauma Acute Care Surg. 2013;75(1):122–128. doi: 10.1097/ta.0b013e3182946746. [DOI] [PubMed] [Google Scholar]
- 9.Guliani S., Amendola M., Strife B., Morano G., Elbich J., Albuquerque F. Central aortic wire confirmation for emergent endovascular procedures: as fast as surgeon-performed ultrasound. J. Trauma Acute Care Surg. 2015;79(4):549–554. doi: 10.1097/TA.0000000000000818. [DOI] [PubMed] [Google Scholar]
- 10.Chaudery M., Clark J., Morrison J.J., Wilson M.H., Bew D., Darzi A. Can contrast-enhanced ultrasonography improve Zone III REBOA placement for prehospital care? J. Trauma Acute Care Surg. 2016;80(1):89–94. doi: 10.1097/TA.0000000000000863. [DOI] [PubMed] [Google Scholar]