Abstract
Rationale:
Isolated dissection of the celiac artery (IDCA) is one of isolated visceral artery dissection, which can occur alone, and can also be complicated with superior mesenteric artery dissection and splenic artery pseudoaneurysm. This disease is very rare in clinic. The exact pathogenesis of IDCA remains unknown. At present, no consensus has yet been reached on the best treatment strategy for this rare disease. In the present study, the clinical data of one IDCA patient diagnosed and treated in our hospital was retrospectively analyzed, and related literatures were reviewed, in order to improve the understanding of the disease.
Patient concerns:
The patient was a 49-year-old male, who was admitted in our hospital because of “pain of subxyphoid area for one month”. One month before, the patient presented with persistent pain in the subxyphoid area after he had a cold, on paroxysmal exacerbation occurred. After taking “stomach drug”, the subjective symptoms eased slightly, but the disease attacked again two hours later.
Diagnoses:
The patient was diagnosed with “isolated dissection of the celiac artery” by enhanced CT.
Interventions:
The patient was interventionally treated with bare stent implantation.
Outcomes:
The symptom of the patient disappeared after interventional therapy.
Lessons:
In the present study, the clinical symptoms and treatment process of one patient with IDCA were described. The clinical symptoms of IDCA are often atypical, and its incidence is extremely low, therefore it is extremely easily misdiagnosed. The definite diagnosis depends on imaging examination. Interventional therapy is the first choice for treating this disease due to its advantages of small trauma and good curative effect.
Keywords: celiac artery, isolated dissection, multi-slice spiral computed tomography, vascular interventional therapy
1. Introduction
Isolated dissection of the celiac artery (IDCA) refers to the occurrence of a celiac arterial dissection alone without an aortic dissection, which is very rare in clinic.[1] The exact pathogenesis of IDCA remains unknown, and hypertension, smoking, atherosclerosis, abdominal surgery or trauma, fibromuscular dysplasia, connective tissue disease, pregnancy, vasculitis, tumor, and cystic medial necrosis may be the risk factors of this disease. At present, there is no consensus on the best treatment strategy for this rare disease. In the present study, the clinical data of one case of IDCA, which was diagnosed and treated in our hospital, was retrospectively analyzed, and related literatures were reviewed. IDCA is a rare disease, and its clinical symptoms are often atypical. Its diagnosis has been based on imaging examinations. Due to the advantages of less trauma, better curative effect and shorter hospitalization time, the intravascular technique has gradually become the main treatment for IDCA.
2. Case presentation
The patient was a 49-year old man, who was admitted in our hospital due to “pain at the subxiphoid area for 1 month”. The patient presented with persistent pain in the subxiphoid area after he had a cold at 1 month before admission, without paroxysmal exacerbation. After taking “stomach medicine,” the subjective symptoms slightly eased, but the disease attacked again after 2 hours. Admission examination: blood pressure was 132/77 mmHg, the epigastrium presented with tenderness, no rebound pain and muscle tension occurred, and no percussion pain occurred in the renal region. The patient has a history of hypertension for more than 10 years, but did not regularly take medication, and blood pressure was controlled within 130 to 160/80 to 95 mmHg. Furthermore, the patient has a history of drinking for more than 30 years, and the dose was approximately 150 mL/day (white wine). Routine laboratory examination revealed no abnormality. Enhanced computed tomography (CT) revealed defects in both the proximal and distal ends of the celiac trunk, with the celiac trunk showing a “dual-lumen shadow.” The false lumen communicated with the true lumen. The true lumen was slightly compressed and flat, and no obvious thrombosis occurred in the false lumen. The patient was treated with antihypertensive, anticoagulant and antiplatelet therapies for 1 week, but the symptoms did not improve. Therefore, endovascular treatment was carried out. An 8.0 × 40 mm bare stent of X-pert (Abbott) was placed in the celiac dissection area. After the operation, the patient orally received clopidogrel tablets (75 mg, qd) for 3 months, and received aspirin enteric-coated tablets (100 mg, qd) for a long time. After 3 months, enhanced CT revealed a good patency of the true lumen of the celiac trunk dissection area, the false lumen was not enlarged, and the stent was in good position (Fig. 1). The present study was conducted with the approval of the Ethics Committee of our hospital.
Figure 1.
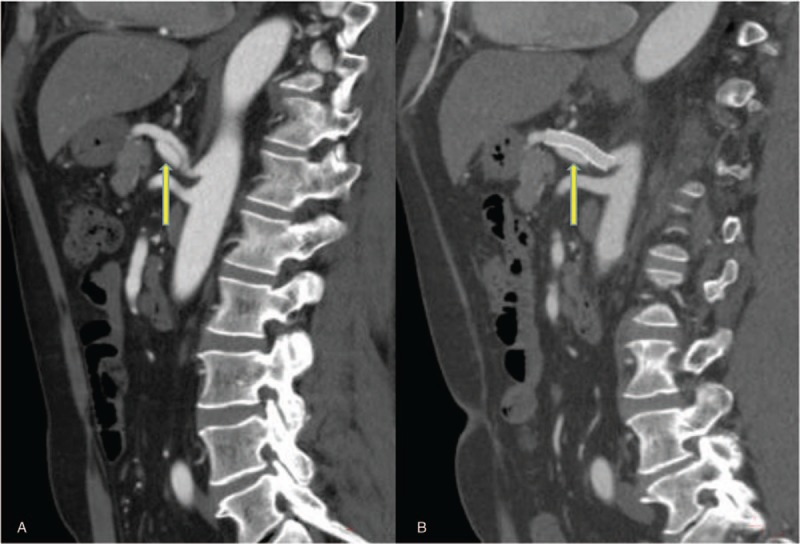
Pre-operative enhanced CT images revealed that the blood vessel separated from the “dual-lumen” by line intimal slices (thin arrows) in the celiac trunk, and the distal ends of the true and false lumens communicated with each other (A). In the post-operative review, enhanced CT reconstruction images revealed that the stent in the celiac trunk was in a good position, blood flow in the true lumen was unobstructed, and the false lumen decreased (B). CT = computed tomography.
3. Discussion
The clinical manifestations of IDCA mainly depend on the dissection-affected range and presence of secondary vascular rupture and bleeding. The typical symptom is sudden upper abdominal or hypochondrium pain, which may be accompanied by nausea, vomiting, and dizziness. This pain can radiate to the back or shoulder, and some patients may present with postprandial pain, chest pain, loss of appetite, weight loss, obstructive jaundice, and intestinal colic.[2–4] The pain in the upper abdomen is mainly due to the tear on the intima of the artery wall and the increase in pressure of the false lumen of dissection. In addition, pancreatitis is also one of the major causes of abdominal pain.[5] If IDCA affects the gastroduodenal artery and splenic artery, pancreatitis is induced by the severe inadequacy of pancreatic blood supply caused by direct blood supply reduction, and even partial blood flow reversely flowing into the spleen.[6] In addition, when aneurysms in the dissection rupture, the clinical manifestation of hemorrhagic shock may occur in some patients. In the present case, the patient manifested with persistent subxiphoid pain.
The diagnosis of IDCA mainly depends on the imaging examination. Computed tomography angiography (CTA) is the preferred method of examination for this disease, because it can clearly display the position, range and collateral circulation distributions of the dissection, and assess secondary changes in abdominal organs, such as necrosis and perforation. In the early stage, the initial segment of the celiac artery had ulcer-like processes, and this can be combined with the formation of mural thrombus in the trunk and branches. In the metaphase, the celiac artery thickens, the true and false dual-lumen forms, and intimal slices and even aneurysms in the dissection can be observed. In the late stage, the dissection and thrombus in the celiac artery disappears, and the vessels in the diseased segment become not smooth enough or returns to normal.[7] In the present case, the patient was given a definite diagnosis by enhanced CT before the operation, and an intimal flap and double cavity shadows were found. Furthermore, the true cavity and sham cavity communicated with each other.
The purpose of the IDCA treatment was to cover this defect, reduce or eliminate the false lumen, and prevent the rupture of the dissection. At present, there is no consensus on the timing and method of IDCA treatment. Fuxian Zhang et al[8] considered that for patients with mild clinical symptoms or asymptomatic patients, medical conservative treatment is recommended, such as managing blood pressure and dual-antibiotic therapy. If symptoms are aggravated during conservative treatment, surgical intervention should be immediately performed. In recent years, endovascular techniques have replaced traditional surgery as the preferred treatment for IDCA. The patient was treated by intracavity mode. The true cavity was obviously enlarged and the sham cavity was significantly reduced. Furthermore, blood flow velocity in the sham cavity slowed down after the breaks of the proximal and distal ends of the dissection were covered by the bare stent. It was found that the true cavity of the dissection was unobstructed, and the position of the stent was good after 3 months follow-up post-operation. When intracavity treatment was performed to the celiac trunk dissection, in principle, the stent should cover the proximal or both ends of the dissection. Both the membrane tectoria stent and bare stent can achieve a good therapeutic effect.[9] In the present case, after the intracavity treatment, the abdominal pain disappeared, blood flow in the stent was smooth, and the efficacy was good. After stent implantation, the true cavity was significantly widened, while the sham cavity was significantly narrowed. It was considered that the breaks had been closed by the “tension” of the stent itself.
IDCA patients should receive clinical and imagological follow-ups at 3 to 6 months after treatment, regardless of whether they have undergone surgical treatment. On the basis of strict medical treatment, if non-operated patients continue to have an enlarged dissection range or aggravated clinical symptoms, active interventional, or surgical treatment should be received. After intervention, 3 months of dual-antibiotic therapy and long-term single-antibiotic therapy should be given. In addition, blood pressure needs to be strictly controlled, and controlling blood pressure is even more meaningful than anticoagulation and antiplatelet therapies.[10]
IDCA is a rare disease, and its clinical symptoms are often atypical. The diagnosis depends on imaging examination. Due to its advantages of less trauma, better curative effect, and shorter hospitalization time, the intravascular technique has gradually become the main treatment for IDCA.
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Author contributions
Conceptualization: Hai-Tao Wang, Zhi-Hai Yu, Can Tu, Bin Lu.
Data curation: Hai-Tao Wang, Zhi-Hai Yu, Can Tu, Bin Lu.
Methodology: Hai-Tao Wang.
Writing – original draft: Hai-Tao Wang.
Writing – review & editing: Hai-Tao Wang.
Footnotes
Abbreviations: CT = computed tomography, CTA = computed tomography angiography, IDCA = isolated dissection of the celiac artery.
The authors declare no conflicts of interests.
References
- [1].Takayama T, Miyata T, Shirakawa M, et al. Isolated spontaneous dissection of the splanchnic arteries. J Vasc Surg 2008;48:329–33. [DOI] [PubMed] [Google Scholar]
- [2].Kang TL, Teich DL, Mcgillicuddy DC. Isolated, spontaneous superior mesenteric and celiac artery dissection: case report and review of literature. J Emerg Med 2011;40:e21–5. [DOI] [PubMed] [Google Scholar]
- [3].D’Ambrosio N, Friedman B, Siegel D, et al. Spontaneous isolated dissection of the celiac artery: CT findings in adults. AJR Am J Roentgenol 2007;188:W506–11. [DOI] [PubMed] [Google Scholar]
- [4].Mousa AY, Coyle BW, Affuso J, et al. Nonoperative management of isolated celiac and superior mesenteric artery dissection: case report and review of the literature. Vascular 2009;17:359–64. [DOI] [PubMed] [Google Scholar]
- [5].Kirby JM, Vora P, Midia M, et al. Vascular complications of pancreatitis: imaging and intervention. Cardiovasc Intervent Radiol 2008;31:957–70. [DOI] [PubMed] [Google Scholar]
- [6].Amabile P, Ouaïssi M, Cohen S, et al. Conservative treatment of spontaneous and isolated dissection of mesenteric arteries. Ann Vasc Surg 2009;23:738–44. [DOI] [PubMed] [Google Scholar]
- [7].Cui K, Zhang Y, Luo L, et al. Isolated celiac artery dissection: report of two cases. J Intervent Radiol 2015;5:403–4. [Google Scholar]
- [8].Zhang FX, Zhang H, Ma BB. Diagnosis and treatment strategy of isolated spontaneous dissection splanchnic arteries. Chin J Pract Surg 2009;11:947–8. [Google Scholar]
- [9].Liu DW, Zhang XT, Han XJ, et al. Symptomatic splanchnic artery dissection: imaging diagnosis and interventional treatment. J Interv Radiol 2015;7:582–7. [Google Scholar]
- [10].Song Y, Xiao Q, Liu Q. Isolated spontaneous celiac artery dissection. P R Health Sci J 2015;34:174. [PubMed] [Google Scholar]


