Abstract
Introduction:
The relationship between shoulder function and overall function in the elderly patients is not well understood. It is hypothesized that there is an increased tolerance of shoulder dysfunction in this population. The purpose of our study was to investigate and better understand the relationship between shoulder function, general musculoskeletal health, and frailty in the elderly patients.
Materials and Methods:
The dominant shoulders of 75 individuals aged ≥65 years without known dominant shoulder pathology were assessed. Demographic data were collected. Functional evaluation was conducted by administering the Constant, American Shoulder and Elbow Surgeons (ASES), and the Short Musculoskeletal Function Assessment (SMFA) questionnaires. Shoulder range of motion and strength were measured and the Fried frailty phenotype was calculated. Mean age of the patients was 73.6 years. Sixty-seven percent of the patients were female. Mean body mass index was 31.2 kg/m2.
Results:
Twenty-eight percent of the patients reported the use of an assistive device for ambulation. As frailty increased among the 3 Fried frailty phenotypes (robust, prefrail, and frail), patients had statistically significant lower mean Constant scores (P < .0001), ASES scores (P < .0001), higher overall SMFA scores (P < .0001), and an increase in the use of assistive device for ambulation. Individuals who reported the use of an assistive device for ambulation had lower Constant and ASES scores (P < .0001 and P = .045, respectively) and higher overall SMFA scores (P < .0001). There was no evidence of correlation between body mass index and any of the other measures.
Conclusions:
Frailty and the use of an assistive device for ambulation correlate with poor shoulder function in patients who do not register shoulder complaints and have no known shoulder pathology.
Level of Evidence:
Level IV, Prognostic.
Keywords: geriatric, frailty, assistive device, shoulder function, shoulder complaints
Introduction
Shoulder pathology in the elderly patients is common. Multiple studies have shown that upward of 30% of people older than 65 years may suffer from one of several different shoulder conditions including rotator cuff pathology or arthritis.1–6 These conditions often lead to reduced shoulder function.7–9 However, even when individuals in this population experience notable shoulder symptoms, fewer than 50% seek treatment for them.2,3 Functional evaluation tools were used (Constant and American Shoulder and Elbow Surgeons [ASES] scores) to assess baseline shoulder function, which was characterized in 430 asymptomatic elderly individuals.7–10 Katolik et al found statistically significant age-related differences in the Constant score in both men and women.7 Employing the ASES shoulder questionnaire, Sallay and Reed found a trend of decreasing cumulative activity of daily living (ADL) scores by age.9
Despite the existence of normative data for these shoulder function measures, there is a paucity of literature that provides an understanding of the relationship between shoulder pathology and overall physical function in the elderly population. We observed that patients who complained of lower extremity orthopedic conditions also had upper extremity dysfunction about which little complaint was made. We also observed that fewer shoulder complaints were registered by older and less mobile individuals. In light of these observations, we therefore hypothesized that decreased shoulder function in the elderly patients is associated with a general state of frailty.
The primary aim of this research was to better understand the relationship between shoulder function, general musculoskeletal health, and frailty in the elderly orthopedic patient. This was accomplished by investigating specific variables known to affect physical functioning (frailty, body mass index [BMI], general musculoskeletal health, and the use of an assistive device for ambulation) in a population of elderly patients without specific shoulder complaints or known shoulder pathology.
Secondary aims included the determination of (1) which of the aforementioned variables were stronger predictors of abnormal dominant shoulder function in the elderly population and (2) controlling for strength and range of motion of the dominant shoulder, which of the following—general musculoskeletal health, frailty, BMI, or the use of assistive devices for ambulation—most closely correlated with a decreased ability to attend to ADLs and an increased manifestation of shoulder pain in this population.
Patients and Methods
To determine whether decreased shoulder function is associated with generalized frailty, in this cross-sectional study, we recruited a convenience sample of patients (75 patients) older than 65 years who presented to a community orthopedic practice for a complaint not relating to the shoulder. Between June 2008 and July 2009, patients without known shoulder pathology were recruited from the senior author’s clinical practice that has an emphasis on geriatric orthopedics. We obtained prior institutional review board approval for this study and informed consent from each patient.
Information about the patient’s age, gender, hand dominance, living situation (independent or in a care facility), use of tobacco, medical comorbidities, presenting complaint, and the use of assistive device for ambulation was recorded. Patients were then asked to complete the Constant questionairres and the ASES (scoring ranges from 0 to 100, with lower scores indicating worse function and these shoulder function questions relating to their dominant shoulder only), while the Short Musculoskeletal Function Assessment (SMFA) questionnaire was used to assess generalized musculoskeletal health (ranges from 0 to 100, with higher scores indicating worse function).10,11 The dominant shoulder examination was then performed per the Constant scoring system.10 In addition, the Fried phenotypic frailty assessment was completed by the principle investigator or a trained research coordinator.12 Quantitative shoulder strength assessment was performed using a handheld dynamometer (microFET2; Hoggan Scientific, Draper, Utah).13–15 Resistance in pounds of force of the dominant shoulder in abduction (90° in scapular plane), in abduction (arm at side), in forward flexion (90°), in external rotation (arm at side), and in bear hug was recorded. Range of motion of the dominant shoulder (in external rotation, arm at side) was measured with a 14-in (36 cm) goniometer. Frailty was calculated using the Fried frailty phenotype assessment, scored on 5 components: unintentional weight loss, weakness, exhaustion, slow gait, and low physical activity.12 Finally, the patient’s height and weight were recorded for the BMI calculation.
The mean age of the 75 patients was 73.6 ± 1.4 years, and 67% (±11.0%) were female. Ninety-two percent of the patients were right-hand dominant (95% confidence interval [CI], 83.4%-97.0%). Twenty-eight percent of the patients (95% CI, 18.2%-39.6%) reported the use of assistive devices for ambulation.
Data Analysis
Our study’s primary aim was to describe our sample of elderly patients who registered no specific complaints and who had no known shoulder pathology. To meet this aim, we performed a descriptive analysis on outcome measures and other patient characteristics, summarizing continuous variables in terms of means and percentiles and summarizing categorical variables in terms of sample proportions. Our secondary aim was to assess the degree of association between shoulder function outcomes (Constant score and ASES) and other indicators of musculoskeletal health in the elderly patients. Associations were estimated using Pearson correlation coefficients when both the predictor and outcome were continuous variables. Mann-Whitney and Wilcoxon tests were used for binary predictors, such as ambulatory assistance device use. One-way analysis of variance was used to determine whether shoulder function outcomes differed among frailty phenotypes. Variability around our estimates was described in terms of 95% CIs. All hypothesis tests were 2 sided, with α = .05. All statistical analyses were performed using the R statistical software platform, v 2.9.2 (R Project, Vienna, Austria). The β statistic in the multiple regression analysis used is a measure of how much we expect a response variable “y” to change when variable “x” moves by a certain amount and all other variables remain constant.
Results
Demographics
The correlations between patient demographics and strength are presented in Table 1. In most cases, age was negatively correlated with strength, while height and weight were positively correlated with strength. Mean BMI was 31.2 ± 1.7 kg/m2. There was no evidence of correlation between BMI and the Constant score, ASES score, SMFA score, or frailty phenotype (P > .05 for all; Table 2).
Table 1.
Patient Demographics.a
| Mean | Standard Deviation | Median | Min | Max | |
|---|---|---|---|---|---|
| Age | 73.6 | 6.0 | 73 | 65 | 91 |
| Height (in) | 65.1 | 4.7 | 64.5 | 51.7 | 75 |
| Weight (lbs) | 187.1 | 46.6 | 177 | 119 | 330 |
| BMI | 31.2 | 7.4 | 29.4 | 20.6 | 55.0 |
| Frequency, N = 75 | Percent of Cohort | ||||
| Gender | |||||
| Female | 50 | 67 | |||
| Male | 25 | 33 | |||
| Currently smoking | |||||
| No | 72 | 96 | |||
| Yes | 3 | 4 | |||
| Fried frailty phenotype | |||||
| Robust | 38 | 51 | |||
| Prefrail | 27 | 36 | |||
| Frail | 10 | 13 | |||
| Use of assistive device | |||||
| No | 63 | 84 | |||
| Yes | 12 | 16 | |||
| Hand dominance | |||||
| Left | 6 | 8 | |||
| Right | 69 | 92 |
Abbreviation: BMI, body mass index.
a N = 75.
Table 2.
Correlation Between Strength and Age, Weight, Height, and BMI.
| Strength in Abduction (90°, Plane of Scapula) | Strength in Abduction (Arm at Side) | Strength in Forward Flexion (90°) | Strength in External Rotation (Arm at Side) | Strength in Bear Hug | Strength in Adduction (90°) | Degrees of External Rotation (Arm at Side) | |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| Correlation value | −0.42331 | −0.30873 | −0.41094 | −0.31532 | −0.18644 | −0.19368 | −0.16923 |
| P value | .0008 | .0083 | .0002 | .0062 | .117 | .1416 | .1467 |
| Weight (lbs) | |||||||
| Correlation value | 0.32583 | 0.40305 | 0.24826 | 0.3013 | 0.2898 | 0.38062 | −0.17439 |
| P value | .0118 | .0004 | .0317 | .0091 | .0123 | .0029 | .1345 |
| Height (in) | |||||||
| Correlation value | 0.42409 | 0.36263 | 0.3436 | 0.36389 | 0.31105 | 0.44574 | 0.00002 |
| P value | .008 | .0019 | .0027 | .0016 | .0074 | .0004 | .998 |
| BMI | |||||||
| Correlation value | 0.10534 | 0.19487 | 0.05525 | 0.08718 | 0.07844 | 0.19401 | −0.20809 |
| P value | .4272 | .1034 | .6401 | .4633 | .5095 | .1409 | .0752 |
Abbreviation: BMI, body mass index.
Functional Evaluation
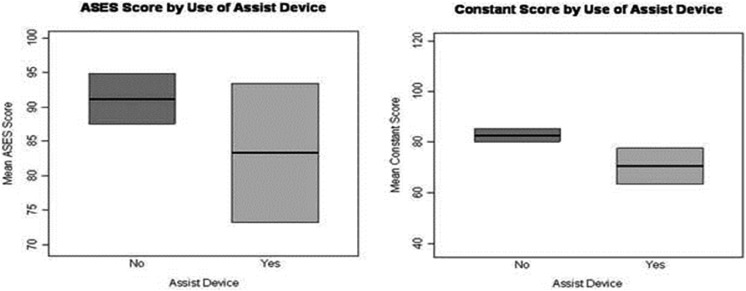
The mean Constant score of the patient cohort was 79.4 ± 2.9. The ASES scores were generally high, with half of scores being greater than 95 and with 28 (37.3%) patients scoring 100. The lowest observed ASES score was 16.7. Higher Constant and ASES scores were associated with higher function and decreased pain. We observed a strong correlation between the Constant and ASES scores (r = 0.70; 95% CI, 0.56-0.80). Individuals who reported the use of an assistive device for ambulation had lower Constant and ASES scores (P < .0001 and P = .045, respectively; Figure 1).
Figure 1.
Assistive device versus ASES and Constant score. ASES indicates American Shoulder and Elbow Surgeons.
The mean overall SMFA score was 22.4 ± 3.2, and the mean SMFA bother index was 23.6 ± 4.0. Higher overall SMFA scores were associated with lower Constant scores (r = −0.46, 95% CI, −0.62 to −0.26) as well as with lower ASES scores (r = −0.42, 95% CI, −0.59 to −0.22). This relationship also existed between the SMFA bother index and Constant and ASES scores (r = −0.25 and −0.28, respectively; Table 3).
Table 3.
Correlation Between ADLs and ASES, Frailty, SMFA, and Constant Score.
| Can You Throw a Ball Overhead? | Can You Sleep on Your Shoulder Comfortably? | Can You Put on Your Coat Unassisted? | Can You Wash Your Back or Fasten Your Bra? | Can You Use Toilet Tissue? | Can You Comb or Wash Your Hair? | Can You Life a 10 lb Weight (a Full Gallon of Milk) Above the Level of Your Shoulder? | Can You Reach a Shelf Over Your Head? | Does Your Shoulder Allow You to Do Your Normal Activities? | Does Your Shoulder Allow You to Do Your Regular Sport? | On Average, How Much Pain Have You Experienced in the Past Week? | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ASES | |||||||||||
| Correlation value | 0.53408 | 0.70411 | 0.50009 | 0.5865 | 0.2896 | 0.2249 | 0.65305 | 0.5462 | 0.48847 | 0.5295 | −0.8915 |
| P value | <.0001 | <.0001 | <.0001 | <.0001 | 0.0117 | 0.0523 | <.0001 | <.0001 | <.0001 | <.0001 | <.0001 |
| Fried frailty phenotype | |||||||||||
| Correlation value | −0.18233 | −0.22119 | −0.37147 | 0.306 | −0.3077 | 0.0788 | −0.18062 | 0.3848 | −0.35771 | 0.1993 | 0.40826 |
| P value | .1253 | .0619 | .0013 | .0089 | .0086 | .5101 | .1289 | .0008 | .002 | .0932 | .0004 |
| SMFA | |||||||||||
| Correlation value | −0.23619 | −0.24916 | −0.35409 | 0.4178 | 0.2147 | 0.0883 | −0.28106 | 0.3578 | −0.39289 | 0.2789 | 0.28716 |
| P value | .0413 | .0311 | .0018 | .0002 | .0643 | .451 | .0146 | .0016 | .0005 | .0154 | .0125 |
| Constant score | |||||||||||
| Correlation value | 0.28294 | 0.3893 | 0.37563 | 0.309 | 0.1441 | 0.0565 | 0.40873 | 0.4633 | 0.33219 | 0.2368 | −0.48255 |
| P value | .0139 | .0006 | .0009 | .007 | .2174 | .6297 | .0003 | <.0001 | .0036 | .0408 | <.0001 |
Abbreviations: ADL, activity of daily living; ASES, American Shoulder and Elbow Surgeons; SMFA, Short Musculoskeletal Function Assessment.
Frailty Phenotype
The 3 Fried frailty phenotypes—robust (score = 0), prefrail (score = 1-2), frail (score = 3-5)—had statistically significantly different mean Constant, ASES, and SMFA scores as well as required the use of an assistive device for ambulation (Table 4). The lowest mean Constant score was recorded for the frail phenotype (58.0 ± 18.1), followed by the prefrail phenotype (78.1 ± 3.4) and then the robust phenotype (84.4 ± 3.1). A similar relationship was also observed between the Fried frailty phenotypes and the ASES scores (P < .0001). Likewise, large differences in overall SMFA scores were observed among robust, prefrail, and frail patients (P < .0001). There was also an increased use of assistive device for ambulation among the robust, prefrail, and frail patients (P < .0001; Table 4).
Table 4.
Frailty Associated With Constant, ASES, SMFA, and Use of Assistive Device.
| Fried Frailty Phenotype | Robust, n = 38 | Prefrail, n = 27 | Frail, n = 10 | P Value |
|---|---|---|---|---|
| Use of assistive device | 3 | 10 | 7 | <.0001 |
| Constant score | 84.4 | 78.1 | 58 | <.0001 |
| ASES | 95.9 | 85.6 | 66.4 | <.0001 |
| SMFA | 16.6 | 25.2 | 44.7 | <.0001 |
Abbreviations: ASES, American Shoulder and Elbow Surgeons; SMFA, Short Musculoskeletal Function Assessment.
The results of our secondary aims showed that general musculoskeletal health, measured by SMFA score, frailty phenotype, measured by phenotypic frailty assessment (PFA) score, and the use of an assistive device, were all found to be the strong predictors of abnormal dominant shoulder function (Constant), with SMFA score having the best predictive value (β = .41, range: 1-100, P ≤ .001), frailty (β = 5.49, range: 1-5, P ≤ .001), and the use of an assistive device (β = 12.4, binary value, P ≤ .001; Table 5).
Table 5.
Predictive Value of Abnormal Shoulder Function (Constant Score).
| Model | Mean Square | R 2 | β | P Value |
|---|---|---|---|---|
| SMFA (0-100) | 2540.47 | 0.21 | −0.41 | <.001 |
| Assist (0-1) | 2325.84 | 0.2 | −12.4 | <.001 |
| PFA (0-5) | 3815.94 | 0.33 | −5.49 | <.001 |
| SMFA + assist | 1577.7 | 0.27 | −0.28 | .01 |
| −7.6 | .02 | |||
| SMFA + PFA | 2000 | 0.34 | −0.15 | .2 |
| −4.52 | .004 | |||
| Assist + PFA | 1974.05 | 0.34 | −3.8 | .28 |
| −4.71 | .002 | |||
| SMFA + assist + PFA | 1356.59 | 0.35 | −0.12 | .3 |
| −2.86 | .42 | |||
| −4.09 | .003 |
Abbreviations: PFA, Phenotypic Frailty Assessment; SMFA, Short Musculoskeletal Function Assessment.
When we controlled for strength and range of motion of the dominant shoulder, SMFA (β = .50, P ≤ .001) and frailty phenotype (β = 6.3, P ≤ .001) closely correlated with decreased ability to attend to the ADLs but were not found to correlate with increased shoulder pain in this population. The use of an assistive device was similarly not found to be predictive in our cohort (Table 6).
Table 6.
Daily Living Activities Score With Respect to ROM and Pain Adjustment.
| Model | Mean Square | R 2 | β | P Value |
|---|---|---|---|---|
| SMFA | 26522.8 | 0.72 | 1.34 | <.001 |
| Assist | 14881.92 | 0.4 | 31.38 | <.001 |
| PFA | 13445.57 | 0.39 | 10.32 | <.001 |
| SMFA + assist | 14053.4 | 0.77 | 1.13 | <.001 |
| 12.2 | .001 | |||
| SMFA + PFA | 12677.91 | 0.74 | 1.17 | <.001 |
| 2.5 | .06 | |||
| Assist + PFA | 8287.55 | 0.48 | 18.52 | .001 |
| 6.51 | .001 | |||
| SMFA + assist + PFA | 8741.71 | 0.77 | 1.08 | <.001 |
| 10.09 | .008 | |||
| 0.98 | .48 |
Abbreviations: ROM, range of motion; SMFA, Short Musculoskeletal Function Assessment.
Discussion
This study was conducted to better understand the relationship between shoulder function, general musculoskeletal health, and frailty in the elderly patients. Older patients may tolerate shoulder dysfunction and choose not to seek medical attention for their shoulder pathology either because of an acceptance to or disregard for their shoulder pain. To better guide clinical decision-making regarding the aggressiveness of detecting and treating musculoskeletal complaints in the elderly patients, we sought to determine which physical function-altering variable (frailty, BMI, general musculoskeletal health, and the use of an assistive device for ambulation) was a stronger predictor of abnormal dominant shoulder function. We postulated the existence of a correlation between shoulder function and frailty in the elderly patients.
Normative data for shoulder function in the elderly patients exist, although very few total patients have been studied.7,13,16,17 In a study that included 114 patients aged 60 years and older, Kim et al reported a correlation between weight, BMI, and shoulder strength. They also found an age-dependent decrease in abduction strength and external rotation strength in male patients and an age-dependent decrease in abduction strength in female patients. Chakravarty and Webley et al described an age-dependent reduction in range of motion in a cohort of 100 patients aged 65 years and older.18 In another study that included 25 patients aged 60 years and older, Sallay and Reed reported mean ASES to be 94.9 Not surprisingly, Sallay and Reed also found that advanced age predicted increased ADL impairment, specifically in regard to the patients’ ability to wash their backs and to lift an 9 lb weight above their heads.9 Chakravarty and Webley also reported that pain causing disturbance at night was present in 24% of patients studied (14 in the 65-74 age-group and 10 in the >75 age-group).3,18
Our study supported many of the findings of the above investigators. We found that increasing age correlated with decreased shoulder strength across 6 strength measurements7,8,13 (Table 2). Sallay and Reed reported that patients aged ≥60 years had a significantly lower ability to lift 9 lb above shoulder level (P = .0003) and wash their backs (P = .03) when compared to younger cohorts.9 Similarly, our study found that the ability to put one’s coat unassisted, to wash one’s back, to lift a 10 lb weight above the level of the shoulder, and to reach a shelf over one’s head each significantly correlated with worse scores on the ASES, Fried frailty phenotype, SMFA, and Constant scores (P < .05; Table 3). The BMI did not correlate significantly with any of the outcomes in either men or women.
In addition to the objective shoulder function evaluations (Constant, ASES, and SMFA) that focus on specific musculoskeletal measures such as strength in abduction or pain with specific ADLs, our study found that increased frailty is significantly associated with decreasing shoulder function and worse Constant, ASES, and SMFA scores (Table 4). Frailty is a common condition in the elderly patients that stems from decreased physiologic reserve and increased vulnerability to adverse outcomes, including loss of independence, increased hospitalization, and death.12,19,20 Given that frailty is a constellation of signs and symptoms, it is often a challenge for clinicians to assess.21 Pursuant to our secondary aims, it was found that SMFA score was the best predictor of abnormal shoulder function (Table 5) and that SMFA score was most predictive of decreased ability to attend to ADLs when strength and range of motion were controlled for (Table 6).
In our cohort of elderly patients without known shoulder pathology, those who required an assistive device for ambulation had an increase in Fried frailty phenotype (P < .0001) as well as lower Constant (P < .0001) and ASES (P = .045) scores (Figure 1). This finding supports a study by Tomita et al. who reported that physical disability level was the strongest overall predictor of assistive device usage in the frail elderly patients.22 Identifying individuals without shoulder complaints but with decreasing shoulder function may be one way to provide early identification of frail patients who are at risk for that which frailty may bring, namely, a decline in function, increased hospitalizations, and early death.
Given the fact that the elderly patients are often unknowingly frail,23,24 it is imperative that their musculoskeletal concerns are addressed with a patient-centered focus that is sensitive to frailty as well as to more traditional problem- or extremity-focused approach.20,21,25,26 In summary, we found that decreased ADLs, specifically the ability to put on a coat unassisted, to wash one’s back, and to reach a shelf over one’s head, corresponded with poor scores on shoulder assessments (Constant, ASES, and SMFA) and with increased Fried frailty scores. Due to the numerous challenges of a busy clinic (over booking, short visit time, decreased time for documentation/charting, decreased staffing and decreased patient function due to dementia, and decreased physical strength and range of motion), it is not always possible to administer and score formal shoulder function assessments and to assess for frailty, and although our study reveals the superior predictive value that the SMFA and Fried frailty phenotype assessments offer, an effective frailty screening option in an orthopedic clinic might be to focus on asking questions specific to the abovementioned ADLs and to inquiring about the use of an assistive device.
There are limitations to this study. First, it represents a cross section of predominately white, English-speaking elderly individuals who were seen in an outpatient orthopedic clinic in the Midwest. Therefore, it may not represent the larger general population. Second, we recruited only patients who denied having a history of shoulder problems, yet 17.3% (13) stated that their dominant shoulder was not normal on the ASES. Third, we did not perform imaging on our patients or review any previous shoulder images. Therefore, some patients in the study with significant structural shoulder pathology may have been included. Given that the mean age of our patients was 73.6 years (standard deviation = 6), we assume that some would demonstrate pathology on imaging.13
Conclusion
Decreased ADLs and the required use of an assistive device for ambulation corresponded with poor scores on shoulder assessments (Constant, ASES, and SMFA) and increased frailty. Additionally, SMFA score was found to be the best predictor of abnormal shoulder function and most predictive of decreased ability to attend to ADLs.
Acknowledgments
The authors would like to thank Michael Knudsen, MD, Timothy Galan, MD, Logan Stuck, Andrew Martin, MD, Harsh R. Parikh, Sandy Vang, Aaron Jacobson, and Jeanne Dutkowski RN, MS,C-ANP.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Julie A. Switzer, MD  http://orcid.org/0000-0002-4834-1643
http://orcid.org/0000-0002-4834-1643
References
- 1. Chard MD, Hazleman BL. Shoulder disorders in the elderly (a hospital study). Ann Rheum Dis. 1987;46(9):684–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34(6):766–769. [DOI] [PubMed] [Google Scholar]
- 3. Chakravarty KK, Webley M. Disorders of the shoulder: an often unrecognised cause of disability in elderly people. BMJ. 1990;300(6728):848–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg. 1999;8(4):296–299. [DOI] [PubMed] [Google Scholar]
- 5. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10–15. [DOI] [PubMed] [Google Scholar]
- 6. Oh JH, Chung SW, Oh CH, et al. The prevalence of shoulder osteoarthritis in the elderly Korean population: association with risk factors and function. J Shoulder Elbow Surg. 2011;20(5):756–763. doi:10.1016/j.jse.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 7. Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the constant score. J Shoulder Elbow Surg. 2005;14(3):279–285. doi:10.1016/j.jse.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 8. Yian EH, Ramappa AJ, Arneberg O, Gerber C. The constant score in normal shoulders. J Shoulder Elbow Surg. 2005;14(2):128–133. doi:10.1016/j.jse.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 9. Sallay PI, Reed L. The measurement of normative American Shoulder and Elbow Surgeons scores. J Shoulder Elbow Surg. 2003;12(6):622–627. doi:10.1016/S105827460300209X. [DOI] [PubMed] [Google Scholar]
- 10. Constant C, Murley A. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;(214):160. [PubMed] [Google Scholar]
- 11. Swiontkowski MF, Engelberg R, Martin DP, Agel J. Short Musculoskeletal Function Assessment questionnaire: validity, reliability, and responsiveness. J Bone Joint Surg Am. 1999;81(9):1245–1260. [DOI] [PubMed] [Google Scholar]
- 12. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M157. [DOI] [PubMed] [Google Scholar]
- 13. Kim HM, Teefey SA, Zelig A, Galatz LM, Keener JD, Yamaguchi K. Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91(2):289–296. doi:10.2106/JBJS.H.00219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11(1):33–39. doi:10.1067/mse.2002.119852. [DOI] [PubMed] [Google Scholar]
- 15. Leggin BG, Neuman RM, Iannotti JP, Williams GR, Thompson EC. Intrarater and interrater reliability of three isometric dynamometers in assessing shoulder strength. J Shoulder Elbow Surg. 1996;5(1):18–24. [DOI] [PubMed] [Google Scholar]
- 16. Hughes RE, Johnson ME, O’Driscoll SW, An KN. Age-related changes in normal isometric shoulder strength. Am J Sports Med. 1999;27(5):651–657. [DOI] [PubMed] [Google Scholar]
- 17. Kuhlman JR, Iannotti JP, Kelly MJ, Riegler FX, Gevaert ML, Ergin TM. Isokinetic and isometric measurement of strength of external rotation and abduction of the shoulder. J Bone Joint Surg Am. 1992;74(9):1320–1333. [PubMed] [Google Scholar]
- 18. Chakravarty K, Webley M. Shoulder joint movement and its relationship to disability in the elderly. J Rheumatol. 1993;20(8):1359–1361. [PubMed] [Google Scholar]
- 19. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi:10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: a review. Age Ageing. 2012;41(2):142–147. doi:10.1093/ageing/afr182; 10.1093/ageing/afr182. [DOI] [PubMed] [Google Scholar]
- 21. Fairhall N, Langron C, Sherrington C, et al. Treating frailty—a practical guide. BMC Med. 2011;9:83 doi:10.1186/1741-7015-9-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tomita MR, Mann WC, Fraas LF, Stanton KM. Predictors of the use of assistive devices that address physical impairments among community-based frail elders. J Appl Gerontol. June 2016. doi:10.1177/0733464804265606. [Google Scholar]
- 23. Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210(6):901–908. doi:10.1016/j.jamcollsurg.2010.01.028. [DOI] [PubMed] [Google Scholar]
- 24. Penrod JD, Litke A, Hawkes WG, et al. Heterogeneity in hip fracture patients: age, functional status, and comorbidity. J Am Geriatr Soc. 2007;55(3):407–413. doi:10.1111/j.1532-5415.2007.01078.x [pii]. [DOI] [PubMed] [Google Scholar]
- 25. Weinstein SL. Nothing about you…without you. J Bone Joint Surg Am. 2005;87(7):1648–1652. doi:10.2106/JBJS.E.00317. [DOI] [PubMed] [Google Scholar]
- 26. Youm J, Chenok KE, Belkora J, Chiu V, Bozic KJ. The emerging case for shared decision making in orthopaedics. Instr Course Lect. 2013;62:587–594. [PubMed] [Google Scholar]