Abstract
Background: Marijuana is the most commonly used illicit drug among older adults. As an older population grows in the United States that has a tolerant attitude toward marijuana use, the dynamics of marijuana use and the effects of marijuana on personal, social, and health outcomes among older adults require attention. Objectives: This review summarizes epidemiological literature on marijuana use among older adults. Method: A literature search was conducted using PubMed, AgeLine, and an online search engine from January 2000 to December 2017, resulting in 18 articles. Results: The greatest increase in marijuana use was observed among those in the older adult population 50 years or older, and those 65 years or older had the greatest increase in marijuana use in the older adult population. Common correlates of marijuana use among those in the older population included being male, being unmarried, having multiple chronic diseases, having psychological stress, and using other substances such as alcohol, tobacco, other illicit drugs, and prescription drugs. Conclusion: The increased use of marijuana in older populations requires surveillance and additional research to understand the use and effects of marijuana in older populations to avoid negative health outcomes.
Keywords: epidemiology, public health, cannabis, marijuana, substance use
Introduction
The older adult population in the United States will dramatically increase in the upcoming decades. By 2050, the population 65 years or older will increase to an estimated 83.7 million people (Colby & Ortman, 2014; Ortman, Velkoff, & Hogan, 2014). The Baby Boomer generation, consisting of births from 1946 to 1964, constitutes a large proportion of the current older adult population (Ortman et al., 2014). The United States will experience a unique set of challenges as the older adult population increases, including increasing disease comorbidities and risk of mortality as well as increased drug use compared with previous older generations (Colliver, Compton, Gfroerer, & Condon, 2006; Wu & Blazer, 2011).
In addition to an increasing older adult population, the United States is experiencing changes in the legalization, perception, and use of marijuana. As of November 2017, 29 states and the District of Columbia have laws that legalize medical marijuana (ProCon.org, 2017), and eight states and the District of Columbia have laws that legalize recreational marijuana (Robinson, 2017). Historically, the perception of marijuana use as a risk to health and limited access to marijuana served as protective factors for marijuana use among older populations in the United States (Salas-Wright et al., 2017). However, as the Baby Boomer generation grew older, people with a tolerant attitude toward marijuana use and higher rates of lifetime drug use than previous generations began to enter the older adult population (Colliver et al., 2006; Wu & Blazer, 2014).
Drug use habits are influenced not only by current political and societal changes in marijuana use but also by past experiences. For instance, in the United States, Baby Boomers came of age during movements such as the Vietnam War protests, the sexual revolution, and the civil rights movement. The large size of the Baby Boomer generation in the United States resulted in increased competition, increased peer pressure, and a changed youth culture (Cross & Kleinhesselink, 1985). In addition, political and social forces, including changes in sex-role expectations and sexual attitudes and organized resistance to the Vietnam War draft, introduced youth to adult roles. Drug use, including marijuana use, was one of the outcomes of these forces and became an additional source of stress (Cross & Kleinhesselink, 1985). As Baby Boomers grew older, their drug use patterns may have persisted.
When asked, most U.S. past-year marijuana users 50 years or older did not perceive marijuana use as a great risk; more than 75% of adults perceived a slight risk or no risk in smoking marijuana once or twice a week (Choi, DiNitto, Marti, & Choi, 2016). Marijuana use seems normalized among the older populations as more of those who ever used marijuana age. As laws legalizing marijuana spread across the United States, and the perception of risk associated with marijuana use decreases, some in the older adult population may (a) continue use, (b) restart marijuana use, or (c) initiate marijuana use for the first time. The impact of marijuana use on the health and social factors of aging adults is largely unknown.
The present review summarizes the available literature on marijuana use among older middle-aged adults (50-64 years old) and older adults (65 years or older), including (a) prevalence of marijuana use, (b) patterns of marijuana use, and (c) correlates of marijuana use. We then summarize the review and discuss the risks and benefits of marijuana, as well as the directions for future research.
Method
A scoping review of the literature was systematically conducted using PubMed and AgeLine from January 1, 2000 to December 8, 2017 (Peters et al., 2015). PubMed includes most health science literature, and AgeLine contains literature related specifically to the older adult population. Literature since the year 2000 was examined to obtain the most recent epidemiological studies related to marijuana use in older populations in the context of marijuana legalization and an increasing older population. Search terms included a combination of the following: cannabis, medical marijuana, marijuana smoking, marijuana abuse, marijuana use, marijuana, hashish, blunts, cannabis use, marijuana use, aging, elder*, geriatric, older adults, and older adult.
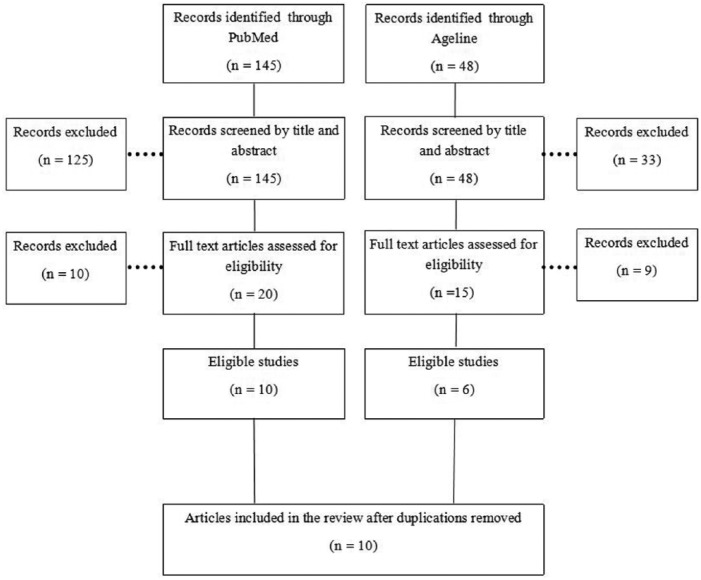
The inclusion criteria for articles in this review included (a) epidemiological studies concerning marijuana use in the older adult population 50 years or older, (b) human subjects, (c) English language, (d) peer-reviewed publications, and (e) U.S. populations. Publications in this review did not include case studies, letters to the editor, essays, and perspective papers. The initial search resulted in 193 articles from both databases (Figure 1). A review of each published title and abstract was completed to select studies that were consistent with the inclusion and exclusion criteria, resulting in the selection of 35 articles from both databases. Most articles excluded from the review reported on younger samples, were written in non-English languages, or were unrelated to marijuana use. Finally, the full text of each published article was reviewed. Articles without relevant information of marijuana use in older U.S. populations or that were nonepidemiological publications (i.e., perspective papers, essays) were excluded. A total of 10 unduplicated articles were obtained from the database search. An Internet search was conducted using the search terms to identify additional articles that were not identified in PubMed and AgeLine, resulting in eight additional articles. Overall, a total of 18 articles were included in this review (Table 1). Study findings were synthesized according to their ability to inform current scientific knowledge about three themes: (a) prevalence of marijuana use, (b) patterns of marijuana use, and (c) correlates of marijuana use.
Figure 1.
Academic database search of published literature related to marijuana use in older adults.
Table 1.
Published Literature on Marijuana Use in Older Adults, 50 Years or Older.
| Reference | Title | Aim(s) | Data source | Sample size | Ages | Findings |
|---|---|---|---|---|---|---|
| Schlaerth, Splawn, Ong, and Smith (2004) | Change in the Pattern of Illegal Drug Use in an Inner City Population Over 50 | To investigate the use of illicit drugs in older adults presenting to an inner-city emergency department. | California Hospital Medical Center in Los Angeles 2001 | n = 3,417 | 50+ years old | ● The average age of marijuana users was 62.8. ● Among drug users who presented to the emergency room, 14% used marijuana and 60% of marijuana users also used other drugs. ● Among emergency room patients who used marijuana, 15.0% were females and 14.9% were males. |
| Degenhardt, Chiu, Sampson, Kessler, and Anthony (2007) | Epidemiological Patterns of Drug Use in the United States: Evidence from the National Comorbidity Survey Replication 2001-2003 | To describe the epidemiological patterns of extra-medical drug use in the United States. | NCS-R 2001-2003 | n = 5,692 | ≥18 years old | ● The estimated cumulative incidence of cannabis use among adults 60-98 years old was 6.4% and among adults 45-59 years old was 45.8%. ● Adults 45-59 years old were 9.4 times more likely to use cannabis than adults 60-98 years old. |
| Blazer and Wu (2009) | The Epidemiology of Substance Use and Disorders Among Middle-Aged and Elderly Community Adults: National Survey on Drug Use and Health (NSDUH) | To estimate the prevalence, distribution, and correlates of drug use among middle-aged and elderly adults in the United States. Drug use was also compared with alcohol use in these age groups. | NSDUH 2005-2006 | n = 10,953 | 50 + years old | ● Past-year prevalence of marijuana use among middle-aged and older adults was 2.6%. ● A larger proportion of past-year marijuana users self-reported the use of marijuana on 30 or more days (49.2%). The mean number of days of marijuana use was 81.2 among past-year users. ● Middle-aged and older adults who self-reported being 50-64 years old (vs. 65+ years old); male; never married, separated, or divorced; and having a past-year major depressive episode were more likely to be past-year marijuana users. |
| Dinitto and Choi (2011) | Marijuana Use among Older Adults in the U.S.A.: User Characteristics, Patterns of Use, and Implication for Interventions | To determine the correlates and patterns of marijuana use among older adults. | NSDUH 2008 | n = 5,325 | 50+ years old | ● Compared with nonrecent users (use more than 12 months ago) and never users, past-year marijuana users were more likely to be between the ages of 50 and 64 years, be Black or multiracial, be unmarried, report better health, have more psychological distress, and use other substances. ● Past-year marijuana users initiated marijuana use before the age of 18 and reported an average frequency of use of nearly 100 days out of the year. ● Approximately 9.0% of past-year marijuana users reported problems due to marijuana use, including emotional or physical problems, low activity, engagement in dangerous activities, problems at home or work, or conflict with family or friends. |
| Satre, Sterling, Mackin, and Weisner (2011) | Patterns of Alcohol and Drug Use Among Depressed Older Adults Seeking Outpatient Psychiatric Services | To investigate the prevalence and correlates of alcohol, drug use, and prescription drug misuse among older adults with depression. | Outpatients at the Langley Porter Adult Psychiatry Clinic, University of California, San Francisco 2005-2009 | n =154 | 60+ years old | ● The past 30-day prevalence of marijuana use among older adults with depression was 12.3% among men and 4.2% among women. ● A higher BDI-II score (≥27) was significantly associated with past 30-day use of marijuana (OR: 15.75, p = .0034). |
| Hasin et al. (2015) | Prevalence of Marijuana Use Disorders in the United States Between 2001-2002 and 2012-2013 | To determine past-year prevalence rates of marijuana use, marijuana use disorder, and marijuana use disorder among past-year marijuana users from 2001 to 2013. | NESARC Wave I (2001-2002) NESARC Wave II (2012-2013) |
NESARC Wave I (n = 43,093) NESARC Wave II (n = 36,309) |
⩾18 years old | ● Among those 18+ years old, past-year marijuana use was 4.1% in 2001-2002 and 9.5% in 2012-2013. Past-year marijuana use by age group: 18-29 (10.5%-21.2%), 30-34 (4.1%-10.1%), 45-64 (1.6%-5.9%), and ≥65 (0.0%-1.3%). ● Among those 18+ years old, past-year marijuana use disorder was 1.5% in 2001-2002 and 2.9% in 2012-2013. Past-year marijuana use disorder by age group: 18-29 (4.4%-7.5%), 30-34 (1.2%- 2.9%), 45-64 (0.4%-1.3%), and ≥65 (0.0%-0.3%). ● Among 18+-year-old past-year marijuana users, past-year marijuana use disorder was 35.6% in 2001-02% and 30.6% in 2012-13. Past-year marijuana use disorder by age group: 18-29 (42.1%-35.4%), 30-34 (27.9%-29.0%), 45-64 (25.8%-22.6%), and ⩾65 (27.3%-23.8%). |
| Ryan-Ibarra, Induni, and Ewing (2015) | Prevalence of Medical Marijuana Use in California, 2012 | To investigate the demographic differences of medical marijuana users and nonusers. | California Behavioral Risk Factor Surveillance System 2012 | n = 7,525 | 18+ years old | ● Medical marijuana use by age group: 18-24 (9.3%), 25-34 (5.5%), 35-44 (4.4%), 45-54 (5.2%), 55-64 (4.6%),v and 65+ (2.2%). |
| Choi, DiNitto, and Marti (2016) | Older Adult Marijuana Users and Ex-Users: Comparisons of Sociodemographic Characteristics and Mental and Substance Use Disorders | To determine whether never users, past-year users, and ex-users differ in respect to sociodemographic factors and past-year and lifetime mental and substance use disorders. Past-year users and ex-users were also compared by patterns of marijuana use and risk factors for mental and substance use disorders. | NESARC 2012-2013 | n =14,715 | 50+ years old | ● The prevalence of past-year marijuana use was as follows: 50+ years (3.9%), 50-64 years old (5.6%), and 65+ years old (1.3%). ● The prevalence of past use was as follows: 50+ years old (21.7%); 50-64 years old (30.2%), and 65+ years old (9.16%). ● In comparison with ex-users, past-year users are more likely to be male, be Black or American Indian (vs. White), reside in the Western United States, have a parent with drug problems, be unmarried, be college graduates, and be employed. ● The age of initiation did not differ significantly between past-users and ex-users (past-year users: 19.0 vs. ex-users: 19.6); however, there were significant differences in the ages when the most marijuana was used (past-year users: 19.0 vs. ex-users: 21.3). ● Past-year users had larger proportions of past-year and lifetime cannabis use disorder and other substance use disorders, lifetime suicide attempts, and one or more past-year and lifetime mental disorders in contrast to ex-users and never users. |
| Choi, DiNitto, and Marti (2016) | Older Marijuana Users: Life Stressors and Perceived Social Support | To investigate the association between marijuana use and marijuana use disorder with life stressors and social support. | NESARC 2012-2013 | n = 14,715 | 50+ years old | ● In comparison with nonmedical marijuana users, medical marijuana users did not differ in life stressors or social support; however, medical marijuana users had a higher prevalence of women, lower employment, higher percentages of Medicaid, more chronic conditions, and more mental disorders. ● Marijuana use was associated with life stressors, including being separated/divorced/broke off steady relationship; personal or family trouble with the police or law; physical assault of family members or close friends; debt; homelessness; problems with friends, neighbors, or relatives; and victim of theft or property destruction. Marijuana use was associated with lower appraisal, belonging, and tangible social support scores. ● Among marijuana users, marijuana use disorder was associated with problems with friends, neighbors, or relatives, and being a victim of theft or property destruction. Marijuana use disorder was associated with appraisal social support. |
| Choi, DiNitto, Marti, and Choi (2016) | Relationships between Marijuana and Other Illicit Drug Use and Depression/Suicidal Thoughts among Late Middle-Aged and Older Adults | To investigate the relationship between marijuana use and/or other illicit drug use and depression and suicidal thoughts. | NSDUH 2008-2012 | n = 29,634 | 50+ years old | ● Among those in the older adult population 50 years or older, the prevalence of past-year marijuana use was 3.9%. ● Among those in the older adult population that used illicit drugs, 51.5% used marijuana only and 15.0% used marijuana and other drugs. ● Older adults who used marijuana only had increased odds of lifetime major depressive episodes (OR: 1.73, 95% CI: [1.36, 2.20]) and past-year major depressive episodes (OR: 1.54, 95% CI: [1.17, 2.03]), but not past-year serious suicidal thoughts (OR: 1.20, 95% CI: [0.81, 1.77]) in comparison with older adults who did not use illicit drugs. ● Older adults who used marijuana and other drugs had increased odds of lifetime major depressive episodes (OR: 2.50, 95% CI: [1.66, 3.76]), past-year major depressive episodes (OR: 2.75, 95% CI: [1.75, 4.33]), and past-year serious suicidal thoughts (OR: 2.44, 95% CI: [1.58 3.77]) in comparison with older adults who did not use illicit drugs. ● Those who used marijuana only were 55% less likely to report past-year serious suicidal thoughts in contrast to those who used marijuana and other drugs. |
| Choi, DiNitto, and Marti (2016) | Risk Factors for Self-Reported Driving Under the Influence of Alcohol and/or Illicit Drugs Among Older Adults | To investigate risk factors for driving under the influence (DUI) of alcohol or drugs among older adults, as well as the difference between those aged 50-64 and 65+ years. | NSDUH 2008-2012 | n = 29,634 | 50+ years old | ● Among 50- to 64-year-olds who reported a past-year DUI, 22.1% used marijuana use in the past year. ● Among 65+-year-olds who reported a past-year DUI, 8.2% used marijuana use in the past year. ● Past-year marijuana use was a significant predictor of past-year DUI among those 50-64 years old (OR: 3.12, 95% CI: [2.54, 3.82]) and among those 65+ years old (OR: 4.94, 95% CI: [2.12, 11.52]). |
| Fairman (2016) | Trends in Registered Medical Marijuana Participation Across 13 US States and District of Columbia | To describe medical marijuana participation in 13 states in the United States and District of Columbia. | State Medical Marijuana Patient Registries 2001-2015 | Samples varied by state | All ages | ● Alaska: 50-59 (4.4/1,000 persons), 60-69 (4.3/1,000 persons), and 70+ (1.2/1,000 persons). ● Arizona: 51-60 (16.8/1.000 persons), 61-70 (15.7/1,000 persons), and 71+ (4.3/1,000 persons). ● Colorado: 51-60 (30.4/1.000 persons), 61-70 (30.0/1,000 persons), and 71+ (7.4/1,000 persons). ● Montana: 51-60 (19.7/1,000 persons), 61-70 (16.1/1,000 persons), and 71+ (3.4/1,000 persons). ● Nevada: 55-64 (3.3/1,000 persons) and 65+ (1.7/1,000 persons) ● Oregon: 50-59 (30.5/1,000 persons), 60-69 (30.9/1,000 persons), and 70+ (9.0/1,000 persons). ● Rhode Island: 50-59 (17.6/1,000 persons), 60-69 (16.4/1,000 persons), and 70+ (3.7/1,000 persons). ● Vermont: 55-64 (5.3/1,000 persons) and 65+ (2.5/1,000 persons). |
| Han et al. (2017) | Demographic Trends Among Older Cannabis Users in the United States, 2006-13 | To determine the prevalence of past-year cannabis use, patterns and attitudes of cannabis use, and correlates of cannabis use among older users. | NSDUH 2006-2013 | n = 47,140 | 50+ years old | ● The prevalence of past-year cannabis use increased from 2.8% to 4.8% among adults 50+ years old from 2006 to 2013. ● Differences in the prevalence of cannabis use differed among those 50-64 years old (7.1%) and 65+ years old (1.4%) in 2013, but the relative increase in past-year cannabis use was larger among 65+-year-olds (250.0%) than 50- to 64-year-olds (57.8%) from 2006 to 2013. ● Correlates of cannabis use by older adults include being male, being non-Hispanic Black, completing some college, having a household income of less than US$20,000, being unmarried, and initiating use before the age of 18. ● Most past-year users perceived slight risk (37.3%) or no risk (41.7%) of using cannabis once or twice a week. ● From 2006 to 2013, significant increases in past-year cannabis use were identified among past-year alcohol users (63.4%) and tobacco users (55.8%). |
| Choi, DiNitto, Marti, and Choi (2017) | Association between Nonmedical Marijuana and Pain Reliever Uses Among Individuals Aged 50+ | To investigate the association between nonmedical marijuana and pain reliever use and determine the sociodemographic, health, and pain-related correlates of nonmedical marijuana and pain reliever use. | NESARC 2012-2013 | n = 14,715 | 50+ years old | ● Past-year nonmedical use of pain relievers had higher odds of marijuana use in contrast to nonusers (OR: 3.17, 95% CI: [2.28, 4.40]). ● Those with opioid use disorders had higher odds of cannabis use disorders in contrast to those without a disorder (OR: 2.95, 95% CI: [1.11, 7.79]). ● Correlates of dual misuse compared with nonmedical use of marijuana use only included past-year chronic medical conditions, severe pain interference, and alcohol use disorder. |
| Choi, DiNitto, and Marti (2017) | Nonmedical Versus Medical Marijuana Use Among Three Age Groups of Adults: Associations with Mental and Physical Health Status | To investigate mental and physical health correlates of medical versus nonmedical marijuana use among three age groups of adults. | NESARC 2012-2013 | n = 36,309 | 18+ years old | ● Among adults 50-64 years old, 82.2% (531) used marijuana nonmedically, 0.4% (3) had a recommendation for medical use, but did not use marijuana medically, and 17.4% (105) used marijuana medically. ● Among adults 65+ years old, 74.7% (70) used marijuana nonmedically, 4.0% (2) had a recommendation for medical use, but did not use marijuana medically, and 21.3% (17) used marijuana medically. ● Among all adults 50 years or older, 16.9% and 29.8% were nonmedical marijuana users and medical marijuana users, respectively. |
| Choi, DiNitto, and Marti (2017) | Older Adults Driving Under the Influence: Associations with Marijuana Use, Marijuana Use Disorder, and Risk Perceptions | To investigate the association of DUIs with marijuana use, marijuana abuse/dependence, and marijuana risk perception among older adults. | NSDUH 2013-2014 | n = 15,302 | 50+ years old | ● Among past-year marijuana users between the ages of 50 and 64, 33.9% reported a DUI and 26.9% of adults 65 years or older reported a DUI. ● Past-year marijuana users were approximately seven times more likely to report a DUI than those who never used marijuana. ● Adults with past-year marijuana use or use disorder were 2.6 times more likely to report a DUI than those who never used marijuana. |
| Choi, Marti, DiNitto, and Choi (2017) | Older adults’ marijuana use, injuries, and emergency department visits | To determine whether the marijuana use among older adults increased emergency room utilization through injury and whether patterns of marijuana use was associated with injury and marijuana use. | NESARC 2012-2013 | n =14,715 | 50+ years old | ● In comparison with nonusers, injury was associated with marijuana use among older adults, and injury was associated with emergency department visits. Injury among marijuana users was a mediator for an increased likelihood of emergency department utilization. ● Patterns of marijuana use were not associated with injury or emergency department visit. |
| Salas-Wright et al. (2017) | Trends and Correlates of Marijuana Use among Late Middle-Aged and Older Adults in the United States, 2002-2014 | To examine the trends and correlates of marijuana use among older middle-aged and older adults. | NSDUH 2002-2014 | n = 76,018 | 50+ years old | ● The prevalence of past-year marijuana use significantly increased from approximately 3.0% to 9.1% among those 50-64 years old, and from 0.2% to 2.0% among those 65+ years old from 2002 to 2014. ● The likelihood of marijuana use increased 10.1% annually among those 50-64 years old and 15.3% annually among those 65+ years old from 2002 to 2014, after adjusting for sociodemographic factors and substance use risk factors. ● Past-year marijuana users between the ages of 50 and -64 were more likely to be male, complete some college, be non-Hispanic White, be divorced, separated, or never married, be uninsured, use other substances, participate in risk behaviors, and have past-year anxiety and depression. ● Past-year marijuana users 65+ years were more likely to be male, be African American, be divorced or separated, have less education, use other substances, report DUI, being involved in the criminal justice system, and have past-year depression and anxiety. |
Note. NCS = National Comorbidity Survey; BDI-II = Beck Depression Inventory–II; OR = Odds ratio; NESARC = National Epidemiologic Survey on Alcohol and Related Conditions; CI = confidence interval.
Result
Review of the Literature
The prevalence of marijuana use and associated factors and behaviors in the older adult population 50 years or older was examined in several population-based studies, including the National Survey on Drug Use and Health (NSDUH), the National Comorbidity Survey–Replication (NCS-R), and the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Additional studies that addressed marijuana use in the older adult population analyzed data from the State Medical Marijuana Patient Registries, California Behavioral Risk Factor Surveillance System, California Hospital Medical Center in Los Angeles, and the Langley Porter Adult Psychiatry Clinic of the University of California, San Francisco. The years of data included in this review ranged from 2001 to 2014 with sample sizes from 154 to 79,402.
Prevalence of Marijuana Use
Marijuana
In comparison with younger age groups, fewer people in the older adult population (50+ years old) currently use marijuana (Azofeifa et al., 2016; Degenhardt, Chiu, Sampson, Kessler, & Anthony, 2007; Hasin et al., 2015). Among those in the older adult population, the prevalence of past-year marijuana use ranged from 3.9% to 4.8% based on data from the NESARC and NSDUH (Choi, DiNitto, & Marti, 2016a). Nonetheless, the greatest increase in marijuana use was observed in the older adult population (Azofeifa et al., 2016). From 2006 to 2013, the past-year prevalence of marijuana use among those 50 years or older significantly increased by 71.4% (Han et al., 2017).
Differences in past-year prevalence were also found among age cohorts. Past-year prevalence of marijuana use ranged from 5.6% to 9.1% among those 50 to 64 years old and 1.3% to 2.0% among those 65 years or older (Choi et al., 2016a; Han et al., 2017; Salas-Wright et al., 2017). Trend analysis determined that past-year marijuana use among those 50 to 64 years old increased 10.1% annually, and past-year marijuana use among those 65 years or older increased 15.3% annually after adjusting for sociodemographic factors, substance use, and risk factors (Salas-Wright et al., 2017). Prevalence is higher among marijuana users in the 50 to 64 age group; however, the largest increase in use has been found among those 65 years or older (Han et al., 2017; Salas-Wright et al., 2017).
Medical marijuana
There is a paucity of studies examining marijuana use among older adults. However, even fewer studies have examined medical marijuana use (MMU) in the older adult population. Medical marijuana is used as self-treatment for medical conditions and symptoms that do not improve with traditional treatment (American College of Physicians [ACP], 2008). Choi and colleagues used data from the 2012-2013 NESARC to determine that marijuana users in the older adult population were more likely to report marijuana use for medicinal purposes than nonmedicinal reasons. Among medical marijuana users, 18 years or older, 29.8% of users were adults, 50 years or older. Adults 50 years or older represented 16.9% of nonmedical marijuana users (Choi, DiNitto, & Marti, 2017a).
In addition to the examination of MMU in a national survey, MMU has been investigated in individual states. In California, middle-aged (45-64 years old) and older adults (65+) had a point prevalence MMU of approximately 12.0%, resulting in a higher prevalence than the youngest age group, 18-24 (9.28%) (Ryan-Ibarra, Induni, & Ewing, 2015). Fairman (2016) determined that the proportion of medical marijuana users in the older adult population, 50 years or older, ranged from 34.6% to 50.9% in eight U.S. States, including Alaska, Arizona, Colorado, Montana, Nevada, Oregon, Rhode Island, and Vermont. Adults, 50 years or older, had the highest rates of MMU in Alaska (ages 50-59; 4.4/1,000 persons), Arizona (ages 51-60; 16.8/1,000 persons), Nevada (ages 55-64; 3.3/1,000 persons), Oregon (ages 60-69; 30.9/1,000 persons), and Vermont (ages 55-64; 5.3/1,000 persons) (Fairman, 2016).
Patterns of marijuana use
Most marijuana users (past-year users) in the older adult population initiated marijuana use before the age of 18; more than 50% of older marijuana users may be long-term users (Dinitto & Choi, 2011; Han et al., 2017). Older marijuana users and past marijuana users had similar initiation dates; however, older marijuana users began using the most marijuana near age 19, but older past marijuana users started using the most marijuana near age 21 (Choi et al., 2016a). In addition, older marijuana users also used more marijuana (3.19 joints/day) in comparison with older past marijuana users (1.90 joints/day) during the time of most marijuana use. The average quit age of past marijuana users was approximately 32 years old among those in the older adult population (Choi et al., 2016a).
In the older adult population, marijuana was usually purchased, received free, or shared with a friend; the main source of marijuana was a friend (Dinitto & Choi, 2011; Han et al., 2017). Older users commonly used marijuana at least 100 days out of the year. More than 26% of older marijuana users reported marijuana use 1 to 4 times a week, and an average of 1.67 joints per day was reported (Choi et al., 2016a). Nearly 55% of older marijuana users reported no efforts to decrease marijuana use (Dinitto & Choi, 2011).
In addition to marijuana use, the past-year use of other substances, including alcohol, tobacco, and other illicit drugs, and misuse of prescription drugs were more likely to be reported among older marijuana users (Choi et al., 2016; Choi, DiNitto, Marti, & Choi, 2017; Dinitto & Choi, 2011; Han et al., 2017; Salas-Wright et al., 2017). From 2006 to 2013, significant increases in alcohol (63.4%) and tobacco (55.8%) use were identified among marijuana users in the older population (Han et al., 2017). Marijuana use patterns were similar between those who used marijuana only and those who used marijuana with other illicit drugs in regard to marijuana use recency and frequency (Choi et al., 2016). Moreover, those who used pain relievers nonmedically were more than three times as likely to be marijuana users in comparison with those who did not use pain relievers nonmedically (Choi, DiNitto et al., 2017).
Correlates of marijuana use
Among marijuana users in the older adult population, demographics, health characteristics, and social and behavioral characteristics play a vital role in the use of marijuana. Males were more likely to use marijuana than females (Choi et al., 2016a; Dinitto & Choi, 2011; Han et al., 2017; Salas-Wright et al., 2017). However, the prevalence of marijuana use in females doubled from 2006 to 2013 (Han et al., 2017). Moreover, older marijuana users were more likely to report being never married, divorced, or separated than older nonusers (Choi et al., 2016a; Dinitto & Choi, 2011; Han et al., 2017; Salas-Wright et al., 2017). The race and ethnicity of marijuana users differed in epidemiological studies. Marijuana users in the older adult population were more likely to report being non-Hispanic Black, multiracial, or American Indian in comparison with older nonusers (Choi et al., 2016a; Dinitto & Choi, 2011; Han et al., 2017). Salas-Wright and colleagues (2017) determined that racial differences existed among marijuana users in the older adult population based on age cohorts. Marijuana users between the ages of 50 and 64 years were more likely to be non-Hispanic White, but marijuana users 65 years old or above were more likely to be African American (Salas-Wright et al., 2017).
Furthermore, differences in the levels of education among older marijuana users exist. Han and colleagues (2017) found that older marijuana users reported the completion of some college. Choi and colleagues (2016) determined that older marijuana users were more likely than older past marijuana users to complete college. Salas-Wright and colleagues (2017) found differences in the educational status of marijuana users based on age. Marijuana users 50 to 64 years old completed some college, and marijuana users 65 years or older had less education, including the completion of a high school education or lower (Salas-Wright et al., 2017).
In addition, the physical and mental health of older marijuana users differs from older nonusers. Based on data from 2006 to 2013, Han and colleagues (2017) determined that older marijuana users reported an increase in the prevalence of two or more chronic diseases; however, in comparison with older nonusers, marijuana users self-reported better health (Dinitto & Choi, 2011). Older marijuana users in the sample were also younger, which may explain why users reported better health. Although better health was reported, older marijuana users have reported utilization of the emergency department (Choi, Marti, DiNitto, & Choi, 2017; Schlaerth, Splawn, Ong, & Smith, 2004). In contrast to nonusers, marijuana use has been associated with injury among those in the older adult population, and injury has been associated with emergency department visits (Choi, Marti, et al., 2017). Injury served as a mediator for the increased likelihood of emergency department utilization among marijuana users.
Additionally, psychological stress was elevated in older marijuana users compared with older nonusers (Choi et al., 2016; Dinitto & Choi, 2011). Marijuana users were more likely to report past-year and lifetime depression (Choi et al., 2016a; Choi et al., 2016; Han et al., 2017; Salas-Wright et al., 2017). From 2006 to 2013, past-year depression increased by 100.0% among older marijuana users (Han et al., 2017). Choi and Colleagues (2016) determined that higher rates of one or more of the following past-year and lifetime mental health issues were more likely to be reported among older marijuana users compared with nonusers, including major depressive disorder (MDD), anxiety disorder, post-traumatic stress disorder (PTSD), and bipolar disorder with manic or hypomanic episodes. Lifetime suicide attempts were also more likely to occur in older marijuana users than older nonusers (Choi et al., 2016a). The use of marijuana with other drugs can further exacerbate psychological distress. Those in the older adult population who used marijuana and other drugs were significantly more likely than those who did not use drugs to have lifetime and past-year major depressive episodes and past-year serious suicidal thoughts (Choi et al., 2016).
Although past-year mental health treatment increased by 73.6% among older marijuana users, mental health treatment was less likely to be reported among older marijuana users when compared with older nonusers (Dinitto & Choi, 2011; Han et al., 2017). Among older adults seeking treatment for depression, a high Beck Depression Inventory–II score was significantly associated with past-month marijuana use (Satre, Sterling, Mackin, & Weisner, 2011). Furthermore, marijuana and other substance use disorders were common among older marijuana users in contrast to older nonusers (Choi et al., 2016a). The prevalence of cannabis abuse or dependence was approximately 6.9% (Han et al., 2017). Medical marijuana users were more likely than nonmedical marijuana users to have a cannabis use disorder (Choi et al., 2017a). A larger proportion of older marijuana users than nonusers also reported lifetime alcohol and drug treatment (Choi et al., 2016a).
Four studies were identified that examined differing social and behavioral factors among older marijuana users and nonusers. Family members of marijuana users, including biological parents, siblings, and offspring, were more likely to use drugs than older nonusers (Choi et al., 2016a). Moreover, marijuana use in the older population was associated with life stressors (i.e., trouble with family and personal relationships, personal or family trouble with the police or law, debt, homelessness, and theft or property destruction victimization) and decreased appraisal, belonging, and tangible social support (Choi, DiNitto, & Marti, 2016b). Salas-Wright and colleagues (2017) found that marijuana users 50 to 64 years old were more likely to participate in risky activities, including driving while intoxicated, selling drugs, theft, and attacking to harm in comparison with older nonusers. In contrast, marijuana users 65 years or older were more likely to drive while intoxicated but were not involved in other risky activities. In addition, Choi and colleagues also found that older marijuana users were more likely to drive under the influence (DUI) in comparison with older nonusers (Choi, DiNitto, & Marti, 2016c, 2017b). Among adults 50 years or older, marijuana users were more likely to be involved in the criminal justice system in the past year. However, as the prevalence of marijuana increased and the perception of risk-associated marijuana use decreased, the relationship between marijuana use and risky behaviors (i.e., other illicit drug use, involvement in the criminal justice system) weakened (Salas-Wright et al., 2017).
Discussion
Summary of Review
This review summarized the peer-reviewed published literature on marijuana use in the older adult population 50 years or older, including the prevalence of marijuana use, patterns of marijuana use, and correlates of marijuana use. The greatest increase in marijuana use was observed among those in the older adult population 50 years or older, and those 65 years or older had the greatest increase in marijuana use among all older users. A larger proportion of adults in the older adult population used marijuana medicinally in contrast to recreational use; MMU differed from state to state among older marijuana users. In addition, older marijuana users were more likely to initiate marijuana use before the age of 18, and it is possible that some in the older adult population have continued marijuana use since then. Common correlates of marijuana use among those in the older adult population included factors such as being male, being unmarried, having multiple chronic diseases, and having psychological stress; findings for factors such as race and education level varied in the reviewed studies. Marijuana use was also reported with the use of other substances and drugs, including alcohol, tobacco, other illicit drugs, and misused prescription drugs. The majority of older marijuana users reported no efforts to decrease marijuana use. For many, marijuana use may continue even as older ages are reached.
Marijuana Benefits and Risks
As marijuana use becomes more prevalent in the United States, evidence is gradually revealing negative marijuana-associated outcomes involving both medicinal and recreational marijuana use. As the legalization of medicinal and recreational marijuana increases in the United States, the percentage of older marijuana users may increase, including both aging lifetime marijuana users and new users. A larger percentage of older marijuana users reported MMU than recreational marijuana use (Choi, DiNitto et al., 2017). Common reasons for medicinal marijuana use include pain, anxiety, loss of appetite or weight loss, depression, and insomnia (Hazekamp, Ware, Muller-Vahl, Abrams, & Grotenhermen, 2013).
Lau and colleagues (2015) conducted a qualitative study among Baby Boomers and determined that marijuana users perceived marijuana as having less adverse effects, a lower risk for addiction, and better effectiveness for treating symptoms of medical conditions. Marijuana has been described as a safer alternative to substances and drugs such as alcohol, other illicit drugs, and prescription drugs (Lau et al., 2015). It has even been suggested that marijuana use may reduce the use of opioids (Boehnke, Litinas, & Clauw, 2016). As the United States battles an opioid epidemic, marijuana use may help reduce the loss of life, but a complete picture of the outcomes associated with marijuana use among older populations has yet to be elucidated.
Although marijuana may have medicinal properties, additional research is needed to understand its effects among older users. A clinical review found that only a few conditions have high-quality evidence to support the use of medical marijuana, including chronic pain, neuropathic pain, and spasticity due to multiple sclerosis (Hill, 2015). A review of the efficacy and safety of medical cannabinoids, such as psychoactive ingredients in marijuana like tetrahydrocannabinol (THC), in older subjects found that adverse events were common among those who used medical cannabinoids in contrast to controls (Ameri, 1999; van den Elsen et al., 2014). Currently, there is not enough evidence to corroborate the safety of marijuana use and the effectiveness of marijuana use for many medical conditions (Hill, 2015; van den Elsen et al., 2014).
Along with the potential benefits of marijuana use, the negative health outcomes associated with marijuana use in the older adult population should be considered by users and potential users. First, medical marijuana has been legalized without testing for efficacy and safety as required by the Food and Drug Administration (FDA; “The Compassionate Use Act of 1996: The Medical Marijuana Initiative,” 2011). There are only two cannabinoids approved by the FDA, including dronabinol and nabilone (FDA, 2006a, 2006b, 2017; National Institute on Drug Abuse [NIDA], 2017). Dronabinol is marketed as Marinol and Syndros, which are used to treat anorexia-associated weight loss in patients with acquired immunodeficiency syndrome (AIDS) and nausea and vomiting associated with chemotherapy in cancer patients (FDA, 2006b, 2017). Nabilone is marketed as Cesamet, which is used to treat nausea and vomiting associated with chemotherapy (FDA, 2006a). Second, older adults experience many changes associated with aging that increase susceptibility to adverse events associated with any drug. For example, physiological changes result in differences in pharmacokinetics, leading to increased drug serum levels (Dowling, Weiss, & Condon, 2008). However, a thorough scope of age-related changes in adults is beyond the scope of this review. The potency of THC varies and may increase the likelihood of experiencing adverse events (Ge, Zhang, & Zuo, 2014). A wide range of THC has been found in marijuana sold illegally, ranging from 3% to 29% (Mehmedic et al., 2010). There is no evidence base to determine the appropriate strains and dosage of marijuana to use, even for medical marijuana users (Borgelt, Franson, Nussbaum, & Wang, 2013).
Marijuana use can negatively affect the health of those in the older adult population beyond abuse and dependence. Marijuana use has been associated with injury (Asbridge et al., 2014; Blows et al., 2005; Choi, Marti, et al., 2017; Wettlaufer et al., 2017), mental health problems (Choi et al., 2016; Choi et al., 2016a; Hall & Degenhardt, 2009; Manrique-Garcia et al., 2012), cardiovascular disease (Alshaarawy & Elbaz, 2016; Hackam, 2015; Hemachandra, McKetin, Cherbuin, & Anstey, 2016; Lindsay, Foale, Warren, & Henry, 2005; Reece, Norman, & Hulse, 2016), respiratory problems (Howden & Naughton, 2011; Macleod et al., 2015; Martinasek, McGrogan, & Maysonet, 2016; Moore, Augustson, Moser, & Budney, 2005), metabolic syndrome (B. A. Yankey, Rothenberg, Strasser, White, & Okosun, 2017; B. N. Yankey, Strasser, & Okosun, 2016), cancer (Aldington et al.,2008a, 2008b; Zhang et al., 1999), unhealthy diet (Foltin, Fischman, & Byrne, 1988; Smit & Crespo, 2001), and drug–drug interactions (Lasota, 2015; Mahvan et al., 2017). In addition, the use of marijuana with other substances, including prescription drugs, tobacco, alcohol, and other illicit substances, may exacerbate the negative effects of marijuana use in aging bodies. A thorough scope of all negative health outcomes associated with marijuana use is beyond the scope of this review. However, some areas of concern among older adults will be discussed, including unhealthy diets, injuries, and mental health problems.
A healthy diet is an important prevention factor in the fight against disease. Aging increases the risk of one or more chronic diseases and degenerative diseases (Centers for Disease Control and Prevention [CDC], 2013). Therefore, marijuana may be used for medicinal purposes. Marijuana use stimulates the appetite, and marijuana users have a higher intake of energy and nutrients than nonusers (Foltin et al., 1988; Smit & Crespo, 2001). Smit and Crespo (2001) found that marijuana users 20-59 years old self-reported a higher intake of alcohol, sodium, pork, cheese, and salty snacks, but fewer fruits and vegetable than nonusers. Although the nutritional status of the marijuana users and nonusers did not differ, the long-term effects of diet among marijuana users are unknown. The stimulation of appetite for patients with HIV/AIDS and cancer may be beneficial, but it could be life-threatening for someone with diseases such as diabetes and cardiovascular disease, where a healthy diet may be vital to improved health outcomes.
Moreover, marijuana use can increase the risk of injury among those in the older adult population. Choi and colleagues (2017) determined that marijuana use increased injury among older marijuana users, and injury was a mediator for the utilization of the emergency department. Older marijuana users may be at an increased risk of vehicular accidents and falls; however, studies that address injuries related to marijuana use among those in the older adult population are scarce. Previous studies have found that marijuana use increased the risk of vehicular accidents (Asbridge et al., 2014; Blows et al., 2005; Wettlaufer et al., 2017). As the aging process occurs, cognitive processing speed and visual skills decrease (Eckert, Keren, Roberts, Calhoun, & Harris, 2010; Harada, Natelson Love, & Triebel, 2013). A combination of the effects of marijuana, including sedation, and cognitive changes in older marijuana users can have deleterious consequences for older drivers. Vehicular accidents not only cause harm to human life but can also result in high costs due to health care utilization and property damage (Wettlaufer et al., 2017). Furthermore, those in the older adult population are at risk of falls, and the use of drugs may increase the risk of falls. Most research regarding drug use and falls have focused on prescription drugs, not marijuana use (Musich, Wang, Ruiz, Hawkins, & Wicker, 2017).
In addition, mental health problems have been associated with marijuana use. Marijuana use is strongly associated with depression (Choi et al., 2016a; Choi et al., 2016) and schizophrenia (Hall & Degenhardt, 2009; Manrique-Garcia et al., 2012). Current and lifetime older marijuana users were more likely to report past-year and lifetime mental disorders in contrast to those who never used marijuana (Choi et al., 2016a). Choi and colleagues (2016a) found that lifetime marijuana users were more likely to report past-year MDD, anxiety disorder, post-traumatic stress disorder, alcohol use disorder, and tobacco or nicotine use disorder in comparison with those who never used marijuana. Current marijuana users were more likely to have past-year other drug use disorders, alcohol use disorders, and tobacco or nicotine use disorder in comparison with lifetime marijuana users (Choi et al., 2016a). Marijuana use is significantly associated with substance use disorders among current marijuana users (Blanco et al., 2016; Choi et al., 2016a). In addition, among patients seeking treatment for mental health and substance use problems, marijuana use may negatively affect recovery (Bahorik et al., 2018; Bahorik et al., 2017).
Directions for Future Research
The paucity of research examining marijuana use in the older adult population leaves many questions unanswered. Additional research is needed to learn about marijuana use in the older adult population. The increasing use of marijuana is an issue that requires surveillance and scientific investigation of marijuana use and related behaviors, including (a) trends in marijuana use as legalization increases, (b) motivations and opportunities to initiate and continue marijuana use, (c) differences in MMU versus non-MMU, (d) prevalence of marijuana use among institutionalized older adults (i.e., correctional facilities, nursing homes), and (d) real and perceived health and social outcomes related to marijuana use. Biological indicators are also needed to confirm marijuana use, because underreporting of drug use is common in the older adult population (Rockett, Putnam, Jia, & Smith, 2006).
Limitations and Strengths
This review has limitations that should be noted. First, this review examined the scope of available epidemiologic literature; the quality and the differences in measurements, variables, and methods included in the studies were not assessed. Second, only peer-reviewed, published literature was included in the review. The gray literature was not examined to identify unpublished studies. Nonetheless, this review has strengths. PubMed and AgeLine databases were utilized to systemically identify studies that met the inclusion criteria of the review. In addition, an Internet search was used to identify other studies that were not identified in the PubMed and AgeLine databases. This review investigates a timely topic as the aging population increases and the legalization and use of marijuana increase in the United States.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Institute on Drug Abuse (NIDA) T32 training grant at the University of Florida Substance Abuse Training Center in Public Health from the National Institutes of Health under Grant T32DA035167.
ORCID iD: Catherine W. Striley  https://orcid.org/0000-0003-2973-7842
https://orcid.org/0000-0003-2973-7842
References
- Aldington S., Harwood M., Cox B., Weatherall M., Beckert L., Hansell A., . . . Respiratory Disease Research, G. (2008. a). Cannabis use and cancer of the head and neck: Case-control study. Otolaryngology–Head and Neck Surgery, 138, 374-380. doi: 10.1016/j.otohns.2007.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldington S., Harwood M., Cox B., Weatherall M., Beckert L., Hansell A., . . . Respiratory Disease Research, G. (2008. b). Cannabis use and risk of lung cancer: A case-control study. European Respiratory Journal, 31, 280-286. doi: 10.1183/09031936.00065707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshaarawy O., Elbaz H. A. (2016). Cannabis use and blood pressure levels: United States National Health and Nutrition Examination Survey, 2005-2012. Journal of Hypertension, 34, 1507-1512. doi: 10.1097/hjh.0000000000000990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameri A. (1999). The effects of cannabinoids on the brain. Progress in Neurobiology, 58, 315-348. [DOI] [PubMed] [Google Scholar]
- American College of Physicians. (2008). Supporting research into the therapeutic role of marijuana. Retrieved from https://www.acponline.org/acp_policy/policies/supporting_research_therapeutic_role_of_marijuana_2016.pdf
- Asbridge M., Mann R., Cusimano M. D., Trayling C., Roerecke M., Tallon J. M., . . . Rehm J. (2014). Cannabis and traffic collision risk: Findings from a case-crossover study of injured drivers presenting to emergency departments. International Journal of Public Health, 59, 395-404. doi: 10.1007/s00038-013-0512-z [DOI] [PubMed] [Google Scholar]
- Azofeifa A., Mattson M. E., Schauer G., McAfee T., Grant A., Lyerla R. (2016). National estimates of marijuana use and related indicators—National Survey on drug use and health, United States, 2002-2014. Morbidity and Mortality Weekly Report, 65(11), 1-25. [DOI] [PubMed] [Google Scholar]
- Bahorik A. L., Campbell C. I., Sterling S. A., Leibowitz A., Travis A., Weisner C. M., Satre D. D. (2018). Adverse impact of marijuana use on clinical outcomes among psychiatry patients with depression and alcohol use disorder. Psychiatry Research, 259, 316-322. doi: 10.1016/j.psychres.2017.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahorik A. L., Leibowitz A., Sterling S. A., Travis A., Weisner C., Satre D. D. (2017). Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. Journal of Affective Disorders, 213, 168-171. doi: 10.1016/j.jad.2017.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C., Hasin D. S., Wall M. M., Florez-Salamanca L., Hoertel N., Wang S., . . . Olfson M. (2016). Cannabis use and risk of psychiatric disorders: Prospective evidence from a U.S. national longitudinal study. JAMA Psychiatry, 73, 388-395. doi: 10.1001/jamapsychiatry.2015.3229 [DOI] [PubMed] [Google Scholar]
- Blows S., Ivers R. Q., Connor J., Ameratunga S., Woodward M., Norton R. (2005). Marijuana use and car crash injury. Addiction, 100, 605-611. doi: 10.1111/j.1360-0443.2005.01100.x [DOI] [PubMed] [Google Scholar]
- Boehnke K. F., Litinas E., Clauw D. J. (2016). Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. The Journal of Pain, 17, 739-744. doi: 10.1016/j.jpain.2016.03.002 [DOI] [PubMed] [Google Scholar]
- Borgelt L. M., Franson K. L., Nussbaum A. M., Wang G. S. (2013). The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy, 33, 195-209. doi: 10.1002/phar.1187 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). The state of aging and health in America 2013. Retrieved from https://www.cdc.gov/aging/pdf/State-Aging-Health-in-America-2013.pdf
- Choi N. G., DiNitto D. M., Marti C. N. (2016. a). Older-adult marijuana users and ex-users: Comparisons of sociodemographic characteristics and mental and substance use disorders. Drug Alcohol Dependence, 165, 94-102. doi: 10.1016/j.drugalcdep.2016.05.023 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N. (2016. b). Older marijuana users: Life stressors and perceived social support. Drug and Alcohol Dependence, 169, 56-63. doi: 10.1016/j.drugalcdep.2016.10.012 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N. (2016. c). Risk factors for self-reported driving under the influence of alcohol and/or illicit drugs among older adults. Gerontologist, 56, 282-291. doi: 10.1093/geront/gnu070 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N. (2017. a). Nonmedical versus medical marijuana use among three age groups of adults: Associations with mental and physical health status. The American Journal on Addictions, 26, 697-706. doi: 10.1111/ajad.12598 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N. (2017. b). Older adults driving under the influence: Associations with marijuana use, marijuana use disorder, and risk perceptions. Journal of Applied Gerontology. Advance online publication. doi: 10.1177/0733464817745379 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N., Choi B. Y. (2016). Relationship between marijuana and other illicit drug use and depression/suicidal thoughts among late middle-aged and older adults. International Psychogeriatrics, 28, 577-589. doi: 10.1017/S1041610215001738 [DOI] [PubMed] [Google Scholar]
- Choi N. G., DiNitto D. M., Marti C. N., Choi B. Y. (2017). Association between nonmedical marijuana and pain reliever uses among individuals aged 50. Journal of Psychoactive Drugs, 49, 267-278. doi: 10.1080/02791072.2017.1342153 [DOI] [PubMed] [Google Scholar]
- Choi N. G., Marti C. N., DiNitto D. M., Choi B. Y. (2017). Older adults’ marijuana use, injuries, and emergency department visits. The American Journal of Drug and Alcohol Abuse, 44, 215-223. doi: 10.1080/00952990.2017.1318891 [DOI] [PubMed] [Google Scholar]
- Colby S. L., Ortman J. M. (2014). The baby boom cohort in the United States: 2012 to 2060. Retrieved from https://www.census.gov/prod/2014pubs/p25-1141.pdf
- Colliver J. D., Compton W. M., Gfroerer J. C., Condon T. (2006). Projecting drug use among aging baby boomers in 2020. Annals of Epidemiology, 16, 257-265. doi: 10.1016/j.annepidem.2005.08.003 [DOI] [PubMed] [Google Scholar]
- The Compassionate Use Act of 1996: The medical marijuana initiative. (2011). Retrieved from http://cannabisclinicians.org/wp-content/uploads/2011/09/CUA-Jan-2011.pdf
- Cross H. J., Kleinhesselink R. R. (1985). The impact of the 1960s on adolescence. Journal of Early Adolescence, 5, 517-531. [Google Scholar]
- Degenhardt L., Chiu W. T., Sampson N., Kessler R. C., Anthony J. C. (2007). Epidemiological patterns of extra-medical drug use in the United States: Evidence from the national Comorbidity Survey Replication, 2001-2003. Drug and Alcohol Dependence, 90, 210-223. doi: 10.1016/j.drugalcdep.2007.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinitto D. M., Choi N. G. (2011). Marijuana use among older adults in the U.S.A.: User characteristics, patterns of use, and implications for intervention. International Psychogeriatrics, 23, 732-741. doi: 10.1017/S1041610210002176 [DOI] [PubMed] [Google Scholar]
- Dowling G. J., Weiss S. R., Condon T. P. (2008). Drugs of abuse and the aging brain. Neuropsychopharmacology, 33, 209-218. doi: 10.1038/sj.npp.1301412 [DOI] [PubMed] [Google Scholar]
- Eckert M. A., Keren N. I., Roberts D. R., Calhoun V. D., Harris K. C. (2010). Age-related changes in processing speed: Unique contributions of cerebellar and prefrontal cortex. Frontiers in Human Neuroscience, 4, 10. doi: 10.3389/neuro.09.010.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman B. J. (2016). Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug and Alcohol Dependence, 159, 72-79. doi: 10.1016/j.drugalcdep.2015.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foltin R. W., Fischman M. W., Byrne M. F. (1988). Effects of smoked marijuana on food intake and body weight of humans living in a residential laboratory. Appetite, 11(1), 1-14. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. (2006. a). CESAMET™. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/018677s011lbl.pdf
- Food and Drug Administration. (2006. b). MARINOL®. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/018651s025s026lbl.pdf
- Food and Drug Administration. (2017). Highlights of prescribing information: Syndros. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/205525s003lbl.pdf
- Ge B., Zhang Z., Zuo Z. (2014). Updates on the clinical evidenced herb-warfarin interactions. Evidence-Based Complementary and Alternative Medicine, 2014, 957362. doi: 10.1155/2014/957362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackam D. G. (2015). Cannabis and stroke: Systematic appraisal of case reports. Stroke, 46, 852-856. doi: 10.1161/strokeaha.115.008680 [DOI] [PubMed] [Google Scholar]
- Hall W., Degenhardt L. (2009). Adverse health effects of non-medical cannabis use. The Lancet, 374, 1383-1391. doi: 10.1016/S0140-6736(09)61037-0 [DOI] [PubMed] [Google Scholar]
- Han B. H., Sherman S., Mauro P. M., Martins S. S., Rotenberg J., Palamar J. J. (2017). Demographic trends among older cannabis users in the United States, 2006-13. Addiction, 112, 516-525. doi: 10.1111/add.13670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada C. N., Natelson Love M. C., Triebel K. L. (2013). Normal cognitive aging. Clinics in Geriatric Medicine, 29, 737-752. doi: 10.1016/j.cger.2013.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. S., Saha T. D., Kerridge B. T., Goldstein R. B., Chou S. P., Zhang H., . . . Grant B. F. (2015). Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry, 72, 1235-1242. doi: 10.1001/jamapsychiatry.2015.1858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazekamp A., Ware M. A., Muller-Vahl K. R., Abrams D., Grotenhermen F. (2013). The medicinal use of cannabis and cannabinoids-an international cross-sectional survey on administration forms. Journal of Psychoactive Drugs, 45, 199-210. doi: 10.1080/02791072.2013.805976 [DOI] [PubMed] [Google Scholar]
- Hemachandra D., McKetin R., Cherbuin N., Anstey K. J. (2016). Heavy cannabis users at elevated risk of stroke: Evidence from a general population survey. Australian and New Zealand Journal of Public Health, 40, 226-230. doi: 10.1111/1753-6405.12477 [DOI] [PubMed] [Google Scholar]
- Hill K. P. (2015). Medical marijuana for treatment of chronic pain and other medical and psychiatric problems a clinical review. Journal of the American Medical Association, 313, 2474-2483. doi: 10.1001/jama.2015.6199 [DOI] [PubMed] [Google Scholar]
- Howden M. L., Naughton M. T. (2011). Pulmonary effects of marijuana inhalation. Expert Review of Respiratory Medicine, 5, 87-92. doi: 10.1586/ers.10.87 [DOI] [PubMed] [Google Scholar]
- Lasota S. (2015). Role of the pharmacist in the care of patients using cannabis. Background paper prepared for the 2014-2015 APhA policy committee (2014-2015 APhA Policy Committee Report). Retrieved from https://www.pharmacist.com/sites/default/files/files/Role%20of%20the%20Pharmacist%20in%20the%20Care%20of%20Patients%20Using%20Cannabis%20.pdf
- Lau N., Sales P., Averill S., Murphy F., Sato S. O., Murphy S. (2015). A safer alternative: Cannabis substitution as harm reduction. Drug and Alcohol Review, 34, 654-659. doi: 10.1111/dar.12275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay A. C., Foale R. A., Warren O., Henry J. A. (2005). Cannabis as a precipitant of cardiovascular emergencies. International Journal of Cardiology, 104, 230-232. doi: 10.1016/j.ijcard.2004.10.038 [DOI] [PubMed] [Google Scholar]
- Macleod J., Robertson R., Copeland L., McKenzie J., Elton R., Reid P. (2015). Cannabis, tobacco smoking, and lung function: A cross-sectional observational study in a general practice population. The British Journal of General Practice, 65(631), e89-95. doi: 10.3399/bjgp15X683521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahvan T. D., Hilaire M. L., Mann A., Brown A., Linn B., Gardner T., Lai B. (2017). Marijuana use in the elderly: Implications and considerations. The Consultant Pharmacist, 32, 341-351. doi: 10.4140/TCP.n.2017.341 [DOI] [PubMed] [Google Scholar]
- Manrique-Garcia E., Zammit S., Dalman C., Hemmingsson T., Andreasson S., Allebeck P. (2012). Cannabis, schizophrenia and other non-affective psychoses: 35 years of follow-up of a population-based cohort. Psychological Medicine, 42, 1321-1328. doi: 10.1017/S0033291711002078 [DOI] [PubMed] [Google Scholar]
- Martinasek M. P., McGrogan J. B., Maysonet A. (2016). A systematic review of the respiratory effects of inhalational marijuana. Respiratory Care, 61, 1543-1551. doi: 10.4187/respcare.04846 [DOI] [PubMed] [Google Scholar]
- Mehmedic Z., Chandra S., Slade D., Denham H., Foster S., Patel A. S., . . . ElSohly M. A. (2010). Potency trends of Δ9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. Journal of Forensic Sciences, 55, 1209-1217. doi: 10.1111/j.1556-4029.2010.01441.x [DOI] [PubMed] [Google Scholar]
- Moore B. A., Augustson E. M., Moser R. P., Budney A. J. (2005). Respiratory effects of marijuana and tobacco use in a U.S. sample. Journal of General Internal Medicine, 20(1), 33-37. doi: 10.1111/j.1525-1497.2004.40081.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musich S., Wang S. H. S., Ruiz J., Hawkins K., Wicker E. (2017). Falls-related drug use and risk of falls among older adults: A study in a U.S. medicare population. Drugs & Aging, 34, 555-565. doi: 10.1007/s40266-017-0470-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. (2017). Marijuana as medicine. Retrieved from https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine
- Ortman J. M., Velkoff V. A., Hogan H. (2014). An aging nation: The older population in the United States (Current Population Reports). Washington, DC: United States Census Bureau. [Google Scholar]
- Peters M. D. J., Godfrey C., Mclnerney P., Baldini Soares C., Khalil H., Parker D. (2015). Joanna Briggs Institute reviewers’ manual 2015 edition/supplement. Adelaide, South Australia: The Joanna Briggs Institute; Retrieved from http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v2.pdf [Google Scholar]
- ProCon.org. (2017). 29 legal medical marijuana states and DC. Retrieved from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881
- Reece A. S., Norman A., Hulse G. K. (2016). Cannabis exposure as an interactive cardiovascular risk factor and accelerant of organismal ageing: A longitudinal study. BMJ Open, 6(11), Article e011891. doi: 10.1136/bmjopen-2016-011891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M. (2017). It’s 2017: Here’s where you can legally smoke weed now. Retrieved from http://www.businessinsider.com/where-can-you-legally-smoke-weed-2017-1
- Rockett I. R., Putnam S. L., Jia H., Smith G. S. (2006). Declared and undeclared substance use among emergency department patients: A population-based study. Addiction, 101, 706-712. doi: 10.1111/j.1360-0443.2006.01397.x [DOI] [PubMed] [Google Scholar]
- Ryan-Ibarra S., Induni M., Ewing D. (2015). Prevalence of medical marijuana use in California, 2012. Drug and Alcohol Review, 34, 141-146. doi: 10.1111/dar.12207 [DOI] [PubMed] [Google Scholar]
- Salas-Wright C. P., Vaughn M. G., Cummings-Vaughn L. A., Holzer K. J., Nelson E. J., AbiNader M., Oh S. (2017). Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002-2014. Drug and Alcohol Dependence, 171, 97-106. doi: 10.1016/j.drugalcdep.2016.11.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre D. D., Sterling S. A., Mackin R. S., Weisner C. (2011). Patterns of alcohol and drug use among depressed older adults seeking outpatient psychiatric services. The American Journal of Geriatric Psychiatry, 19, 695-703. doi: 10.1097/JGP.0b013e3181f17f0a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlaerth K. R., Splawn R. G., Ong J., Smith S. D. (2004). Change in the pattern of illegal drug use in an inner city population over 50: An observational study. Journal of Addictive Diseases, 23, 95-107. doi: 10.1300/J069v23n02_07 [DOI] [PubMed] [Google Scholar]
- Smit E., Crespo C. J. (2001). Dietary intake and nutritional status of US adult marijuana users: Results from the Third National Health and Nutrition Examination Survey. Public Health Nutrition, 4, 781-786. [DOI] [PubMed] [Google Scholar]
- van den Elsen G. A., Ahmed A. I., Lammers M., Kramers C., Verkes R. J., van der Marck M. A., Rikkert M. G. (2014). Efficacy and safety of medical cannabinoids in older subjects: A systematic review. Ageing Research Reviews, 14, 56-64. doi: 10.1016/j.arr.2014.01.007 [DOI] [PubMed] [Google Scholar]
- Wettlaufer A., Florica R. O., Asbridge M., Beirness D., Brubacher J., Callaghan R., . . . Rehm J. (2017). Estimating the harms and costs of cannabis-attributable collisions in the Canadian provinces. Drug and Alcohol Dependence, 173, 185-190. doi: 10.1016/j.drugalcdep.2016.12.024 [DOI] [PubMed] [Google Scholar]
- Wu L. T., Blazer D. G. (2011). Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health, 23, 481-504. doi: 10.1177/0898264310386224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L. T., Blazer D. G. (2014). Substance use disorders and psychiatric comorbidity in mid and later life: A review. International Journal of Epidemiology, 43, 304-317. doi: 10.1093/ije/dyt173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yankey B. A., Rothenberg R., Strasser S., White K. R., Okosun I. S. (2017). Relationship between years of marijuana use and the four main diagnostic criteria for metabolic syndrome among United States adults. Journal of Addiction Research & Therapy, Suppl. 11:017. doi: 10.4172/2155-6105.1000S11-017 [DOI] [Google Scholar]
- Yankey B. N., Strasser S., Okosun I. S. (2016). A cross-sectional analysis of the association between marijuana and cigarette smoking with metabolic syndrome among adults in the United States. Diabetes & Metabolic Syndrome, 10(2 Suppl. 1), S89-95. doi: 10.1016/j.dsx.2016.03.001 [DOI] [PubMed] [Google Scholar]
- Zhang Z. F., Morgenstern H., Spitz M. R., Tashkin D. P., Yu G. P., Marshall J. R., . . . Schantz S. P. (1999). Marijuana use and increased risk of squamous cell carcinoma of the head and neck. Cancer Epidemiology, Biomarkers & Prevention, 8, 1071-1078. [PubMed] [Google Scholar]