Abstract
This study examined the correlation between body mass index as independent variable, and body image and fear of negative evaluation as dependent variables, as well as the moderating role of self-esteem in these correlations. A total of 318 Malaysian young adults were conveniently recruited to do the self-administered survey on the demographic characteristics body image, fear of negative evaluation, and self-esteem. Partial least squares structural equation modeling was used to test the research hypotheses. The results revealed that body mass index was negatively associated with body image, while no such correlation was found with fear of negative evaluation. Meanwhile, the negative correlation of body mass index with body image was stronger among those with lower self-esteem, while a positive association of body mass index with fear of negative evaluation was significant only among individuals with low self-esteem.
Keywords: body image, body mass index, fear of negative evaluation, moderation, self-esteem
Introduction
Body mass index (BMI) is one’s weight in kilograms (kg) divided by his or her height in meters squared. BMI has been well documented as a negative biological component contributing to body image (BI) and fear of negative evaluation (FNE) (Claes et al., 2012; Kaminsky and Dewey, 2014; Kantanista et al., 2017; Seidman, 2013). Overweight individuals tend to show negative affective feelings toward their body and are more likely to report the sense of dread associated with being evaluated unfavorably while participating in social situations than their normal weight counterparts.
The reasons for obesity and overweight have been the subject of many studies during the past decades. Recently, The Circle of Discontent theory explained the correlation between BMI, BI, and FNE (Marks, 2015). This theory explains “(a) factors that could be at the origin of weight gain and clarifying how they contribute to the obesity epidemic; (b) highlights the distinction between factors that contribute to initial weight gain; (c) describes the psychological and health problems that result from weight gain and obesity, and (d) proposes prevention strategies” (Pelletier et al., 2016: 1).
The Circle of Discontent theory postulates that overconsumption of high-caloric and low-nutrient foods with low satiating power are the reasons why people initially gain weight. Body dissatisfaction, as a negative affect makes them consume even more high-density foods and beverages. Once people reach that stage, they gain more weight, become even more dissatisfied with their bodies, and feel worse about themselves. “Consequently, they attempt to control their weight through different means, which aggravates the problem and leads to more weight gain and, eventually, obesity” (DiClemente and Delahanty, 2016). One of the key elements of this theory emphasizes the negative perceptions of large body size and the resulting high levels of dissatisfaction among people with excessive weight, which backs the assumption that high BMI leads to negative BI and FNE (Marks, 2015).
Although the correlation of BMI, BI, and FNE are well explored, the mechanism of these impacts is not depicted yet. Self-esteem can be a potential factor alleviating the adverse association of BMI, BI, and FNE. Indeed, higher self-esteem may act as a protective source, minimizing the negative association between individuals’ BMI and feelings about their body and the level of anxiety generated by others’ unfavorable judgments. However, empirical research on the role of self-esteem in the correlation of BMI with BI and FNE is scarce.
BI and FNE are context and culture dependent. In some contexts, appearance may have precedence over insight, while in some other contexts appearance may be accounted as trivial. Moreover, social fear may be perceived as normal in one culture and “unreasonable and excessive” in another (Hofmann et al., 2010). Therefore, in this case every context and culture is worth being explored, particularly if the negative determinants of BI and FNE, such as high BMI, are the subjects of the study.
Malaysia has the highest obesity prevalence at 14 percent in the Southeast Asian region. The 2015 National Health and Morbidity survey showed that about 30 percent of Malaysian adults above the age of 18 were overweight (with a BMI of 25 and above), and the other 17.7 percent were obese (with a BMI of 30 and above; Institute for Public Health (IPH), 2015). However, Malaysians are aware of their excess weight and evaluate themselves as healthy or very healthy (Muda et al., 2015). In fact, they do not label obesity and overweight as disease (Muda et al., 2015). Such a wrong perception calls for attention and prompt actions to address overweight and obesity among Malaysian adults, as it imposes a huge burden to the Malaysian health system and its resources and could disrupt priorities in healthcare. The Second Burden of Disease Study for Malaysia, published by IPH (2015) in 2012, ranked high BMI along with hypertension, smoking, diabetes, and high cholesterol as the biggest contributors to both disability adjusted life-years and deaths.
Therefore, considering the issues and challenges in the Malaysian context regarding obesity and overweight, the possible risks of ignoring these issues, as well as the theoretical gap in the growing body of literature on the mechanism of correlation between BMI, BI, and FNE, this study aims to test (1) the relationships between BMI and BI, (2) BMI and FNE, (3) and the moderating role of self-esteem in these relationships among Malaysian young adults.
BI index, BI, and FNE
The relationship between BMI and BI has been consistently reported in the body of literature. BI refers to people’s cognitive and emotional evaluation of their body size and shape and the degree to which they place importance on their physical appearance (Cash and Pruzinsky, 2004). The affective dimension of BI is “one’s emotions about one’s appearance,” and it measures feelings related to weight and non-weight appearance issues. The cognitive dimension of BI is the beliefs, thoughts, and attributions related to appearance.
Empirical evidence reveals that BMI is a very important destructive factor in the development of negative BI (Fitzgibbon et al., 2000; Paxton et al., 2006). Watkins et al. (2008) used a randomized sample of 188 college males to explore the association between BMI and cognitive and affective dimensions of BI, and found that overweight and obese participants reported significantly higher levels of negative BI, higher weight and shape concerns, and body dissatisfaction than did normal and underweight participants. In another study, weight and muscularity concerns were also identified as significantly greater among boys with lower BMI and those with more frequent muscle-building conversations (Jones and Crawford, 2005). In a recent study, young women with overweight and obesity issues also reported dejected feelings about their body and appearance (Kantanista et al., 2017). The correlation between BMI and negative BI in women is higher than in men (Yates et al., 2004). In girls with diabetes, a higher BMI is associated with a less positive BI and poorer psychosocial outcomes (Kaminsky and Dewey, 2014). Likewise, the data collected from 110 pregnant women in Israel and the United Kingdom demonstrated high correlations between BI and BMI (Shloim et al., 2015). Another study on White, Hispanic, and Black women revealed that White women reported negative BI at a lower level of BMI and below the criterion for overweight, while Black and Hispanic women experienced unfavorable affective feelings toward their body until they were overweight (Fitzgibbon et al., 2000). Moreover, heavier women who are dissatisfied with their bodies attempt to lose weight, whereas men attempt to gain weight and increase muscle mass (Garousi et al., 2012).
A longitudinal study also traced the developmental trajectories of BI satisfaction from adolescence into the adult years based on the patterns of change in BMI and found the contribution of BMI to the development of BI satisfaction across adolescence and early adulthood (Holsen et al., 2012). Similarly, Paxton et al. (2006) found BMI as a risk factor for increase in body dissatisfaction at the time of first assessment and 5 years follow-up later (over time), particularly among girls.
BMI was also a risk factor for FNE, the “fear that one will be negatively evaluated because of one’s appearance” (Levinson and Rodebaugh, 2012). Social appearance anxiety, the fear of social situations in which individuals perceive themselves vulnerable to other people’s negative evaluation, was positively related to BMI, drive for thinness, and body dissatisfaction in women diagnosed with an eating disorder (Claes et al., 2012). Therefore, imperfections in appearance perceived by individuals can generate fear of public criticism, which in turn may result in unhealthy behaviors, such as eating disorder, particularly among those who highly rely on their appearance (Koskina et al., 2011; Levinson and Rodebaugh, 2012).
Based on the literature reviewed above, the following hypotheses are proposed:
H1: BMI has a negative relationship with BI.
H2: BMI has a positive relationship with negative FNE.
Self-esteem as moderator in correlation between BI index, BI, and FNE
Self-esteem refers to individuals’ overall subjective emotional evaluation of their own worth (Kalat, 2016). Individuals with low self-esteem are more likely to be vulnerable to pressures around body and to be dissatisfied with their body over time (Paxton et al., 2006). They may also suffer from negative comments and feedback they receive from interpersonal sources regarding their appearance (Herbozo and Thompson, 2006; Thompson et al., 2007). Self-esteem, as an intrapersonal disposition, was well documented as a contributor of BI and FNE. Research supported the protective role of self-esteem in negative BI. For example, De Sousa Fortesa et al. (2014) surveyed a female group of 397 adolescents aged 12–17 years and found that negative self-esteem was a negative determinant of favorable affective feelings. In a sample of 425 African American men and women, self-esteem was also identified as a safeguard measure to body dissatisfaction (Oney et al., 2011).
In nonclinical samples, self-esteem was also significantly correlated with fear of social anxiousness and negative evaluation, suggesting that positive self-esteem safeguards against the impact of negative influences, and protects and facilitates better health and positive social behavior (Khanam and Moghal, 2012). Similarly, weight and appearance esteem was a key factor of more positive cosmetic surgery attitudes, and greater fear of negative appearance evaluation in midlife women (Dunaev et al., 2018). College students with and without asthma consistently reported higher levels of self-focused attention, whereby FNE was correlated with lower self-esteem (Junghans-Rutelonis et al., 2015).
Self-esteem also has an indirect impact on the relationship between stress and unpleasant feeling toward body (Murray et al., 2013), and the relationship between negative BI and disordered eating behavior (Brechan and Kvalem, 2015). In addition, self-esteem attenuates the deleterious impacts of negative BI on bulimic symptomatology (Brannan and Petrie, 2011), and the negative impact of internalization on body dissatisfaction (Ricciardelli and McCabe, 2001). Investigating the buffering role of self-esteem in BI, a recent study suggested that Instagram users with high self-esteem are not impinged upon by the exposure to ideal BIs displayed on Instagram and less likely to report body satisfaction as they evaluate their appearance less important or worthy (Ahadzadeh et al., 2017).
Given that self-esteem is a robust predictor of BI and FNE, adverse impact of BMI on BI and FNE can be protected by self-esteem. In other words, self-esteem has a potential to dampen the negative correlation between BMI and BI, as well as the positive relation between BMI and FNE. Indeed, in individuals with high self-esteem, BMI may not be a threat that creates unfavorable feelings toward body and generates fear of negative judgment by others.
Based on the literature reviewed above, the following hypotheses are postulated:
H3: self-esteem moderates the negative relationship between BMI and BI.
H4: self-esteem moderates the positive relationship between BMI and FNE.
Methodology
Design
A cross-sectional design was used to examine the correlation between BMI, BI, and FNE as well as the moderating role of self-esteem in the relationship between BMI as independent variable, and FNE and BI as dependent variables, among students of a private university in Kuala Lumpur, Malaysia. To collect the data, 318 participants were conveniently recruited to complete a set of questionnaires including demographic characteristics and three validated measures of BI, FNE, and self-esteem. The sample consisted of 115 males (36%) and 203 females (64%), aged between 18 and 28 years (mean = 20.37). A majority of the respondents (81%) were Malaysian Chinese and single (87%).
Measurement
Self-esteem
Participants’ self-esteem was assessed by Rosenberg’s (1965) 10-item scale measuring global self-worth with a focus on both positive and negative feelings about the self. All items of these constructs were rated on a 7-point Likert-type scale from 1 (strongly disagree) to 7 (strongly agree).
BI
The Body Influence Assessment Inventory (BIAI) was applied to measure participants’ BI. Proposed by Osman et al. (2006), the instrument comprises four dimensions of positive affect, negative affect, suicide-related thoughts, and behavioral practices related to the influence of the body and physical appearance on psychosocial functioning. The instrument was expanded upon Orbach’s (1996) conceptualization of the role and influence of bodily experiences in self-destructive behaviors. The dimension of suicide-related thought was excluded from the questionnaire due to its irrelevance to this study. Items were scored on a 6-point Likert-type scale ranging from 1 (not at all) to 6 (extremely).
Analysis
The relationships were tested with structural equation modeling (SEM) using the SmartPLS 3.0. PLS-SEM is distinguished from the classical methods by its component-based feature. SEM, as a second-generation technique, is a family of multivariate statistical techniques that assesses direct and indirect relationships between one or more independent latent variables and dependent variables in a more powerful way compared with traditional multivariate techniques. The advantage of SEM is that it is possible to simultaneously model the relationships of multiple independent and dependent constructs.
As recommended by Anderson and Gerbing (1988), the two stages of analytical procedure, including measurement model and structural model were processed to validate the model and test the relationships. As suggested by Hair et al. (2013), in testing measurement model, convergent validity, including factor loading, composite reliability (CR), and average variance extracted (AVE) must be measured.
Factor loading represents indicators’ reliability. As shown in Table 1, factor loadings are varied from 0.602 to 0.938. According to Chin (1998), the items that exceeded the recommended value of 0.6 were retained, and no items were found below the cutoff value. CR, as a better estimate than Cronbach’s alpha, represents internal consistency of constructs. Internal consistency is reliable once the value is at least 0.7 and above (Hair et al., 2017). As shown in Table 1, CR is varied from 0.7 to 0.911, which represents an appropriate indication of internal consistency. AVE reflects that at least 50 percent of items explain the construct if it is greater than 0.5 (Hair al., 2017). As shown in Table 1, AVE ranges from 0.501 to 0.0.629, acceptable for the variables.
Table 1.
Convergent validity.
| Construct | Item | Factor loading | CR | AVE |
|---|---|---|---|---|
| BMI | BMI | SEM | NA | NA |
| Fear of negative evaluation | F1 | 0.729 | 0.909 | 0.629 |
| F2 | 0.715 | |||
| F3 | 0.857 | |||
| F4 | 0.648 | |||
| F5 | 0.883 | |||
| F6 | 0.893 | |||
| Body image | BN | 0.787 | 0.700 | 0.534 |
| BN2 | 0.821 | |||
| BN3 | 0.819 | |||
| BN4 | 0.787 | |||
| BN5 | 0.826 | |||
| BN6 | 0.773 | |||
| BN7 | 0.827 | |||
| BP8 | 0.878 | |||
| BP9 | 0.918 | |||
| BP10 | 0.917 | |||
| BP11 | 0.938 | |||
| BP12 | 0.879 | |||
| BP13 | 0.848 | |||
| Self-esteem | SE1 | 0.814 | 0.911 | 0.501 |
| SE2 | 0.669 | |||
| SE3 | 0.844 | |||
| SE4 | 0.602 | |||
| SE5 | 0.687 | |||
| SE6 | 0.648 | |||
| SE7 | 0.767 | |||
| SE8 | 0.682 | |||
| SE9 | 0.733 | |||
| SE10 | 0.642 |
BMI: body mass index; CR: composite reliability; AVE: average variance extracted; SEM: structural equation modeling; NA: not applicable.
To test measurement model and discriminant validity, two methods of Fornell and Larcker (1981) and Henseler et al. (2015) were utilized. The results of discriminant validity using the method of Fornell and Larcker (1981) show that all square roots of AVE are more than the off-diagonal elements within their corresponding columns and rows. Based on Table 2, all off-diagonal values are lower than the AVE’s square roots (bold on the diagonal). This indicates that the Fornell and Larcker criterion is met and discriminant validity is achieved.
Table 2.
Discriminant validity (Fornell and Larcker, 1981).
| Latent variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. BMI | 1.000 | |||
| 2. Body image | −0.048 | 0.731 | ||
| 3. Fear of negative evaluation | −0.016 | −0.475 | 0.793 | |
| 4. Self-esteem | −0.039 | 0.529 | −0.269 | 0.708 |
BMI: body mass index.
Discriminant validity using Henseler et al.’s (2015) method is widely used and accepted by researchers recently as an advanced criterion in testing validity. Henseler et al. (2015) suggested two thresholds of 0.85 and 0.9 for heterotrait–monotrait (HTMT) criterion to establish discriminant validity. Using this method, HTMT results are below the critical value of 0.85 and the discriminant validity is met (Table 3).
Table 3.
Discriminant validity (Henseler et al., 2015).
| Latent variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. BMI | ||||
| 2. Body image | 0.084 | |||
| 3. Fear of negative evaluation | 0.057 | 0.512 | ||
| 4. Self-esteem | 0.082 | 0.565 | 0.210 |
BMI: body mass index.
Results
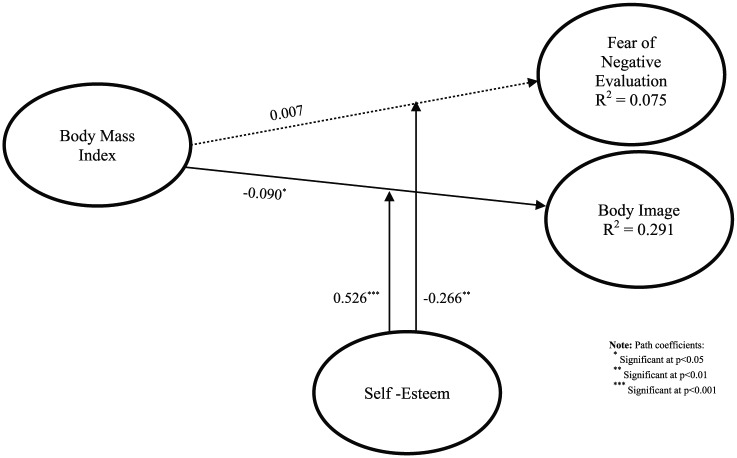
The relationships and hypotheses were tested using bootstrapping method with resampling of 5000 (Hair et al., 2017) to estimate the significance of the path coefficients. The result of path coefficients is shown in Table 4.
Table 4.
Results of hypotheses testing.
| Hypothesis | Std beta | Std error | t value | Decision | f 2 | VIF | R 2 | Q 2 |
|---|---|---|---|---|---|---|---|---|
| H1: BMI → fear of negative evaluation | 0.007 | 0.090 | 0.080 | Not supported | 0.000 | 1.076 | 0.075 | 0.023 |
| H2: BMI → body image | −0.090 | 0.071 | 1.961* | Supported | 0.021 | 1.076 | 0.291 | 0.134 |
| H3: Self-esteem → body image | 0.526 | 0.043 | 12.195*** | Supported | 0.388 | 1.006 | ||
| H4: Self-esteem → fear of negative evaluation | −0.266 | 0.068 | 3.0886** | Supported | 0.076 | 1.006 |
BMI: body mass index.
Path coefficients are as follows:
Significant at p < 0.05.
Significant at p < 0.01.
Significant at p < 0.001.
The results indicate that BMI has a negative correlation with BI (β = −0.090, p < 0.05), while it has no correlation with FNE (β = 0.007, p > 0.05). Moreover, self-esteem as a moderator in the relationship between BMI and BI and FNE is supported (β = 0.526, p < 0.001) and (β = −0.266, p < 0.01).
To measure effect size, Cohen’s (1988) guidelines were followed. The guidelines for the measurement of effect size are 0.35 for large, 0.15 for medium, and 0.02 for small effect, respectively. The results showed that FNE had no effect size while BI had small effect size. On the other hand, self-esteem as a moderator in the model had large effect size toward BI and medium effect size toward FNE.
The R2 value for FNE was 0.075 and 0.291 for BI. This shows that BMI was justifiable only for a very weak amount of 0.07 percent variance on FNE, and a weak amount of 29 percent variance on BI based on the cutoff suggested by Cohen (1988). Using blindfolding method, if Q2 is larger than zero, the model has predictive relevance for endogenous constructs (Hair et al., 2017). Both Q2 values for FNE (Q2 = 0.023) and BI (Q2 = 0.134) are more than zero, suggesting that the model has predictive relevance (Figure 1).
Figure 1.
PLS structural model.
Discussion
The study was designed to investigate the associations between measures of BMI as input, and BI and FNE as outcomes. In addition, the study explored whether self-esteem could moderate these associations. Analysis of the data yielded a negative relationship between scores on BMI and BI scale, indicating that an increase in BMI creates a negative feeling about body and appearance (H1). This result is in line with previous studies, which show that overweight and obese individuals tend to report negative BI, body shape concerns, and poorer psychological outcomes, thus leading to efforts to lose weight or unhealthy behaviors (Holsen et al., 2012; Kaminsky and Dewey, 2014; Kantanista et al., 2017; Paxton et al., 2006; Shloim et al., 2015; Watkins et al., 2008). Data also underpin one of the postulations in the theory of Circle of Discontent, which correlates excessive weight to individuals’ negative BI (Marks, 2015).
Furthermore, while BMI was found as an adverse determinant of BI, data did not support the correlation between BMI and FNE (H2). This contrasts with the results of studies which indicated that a higher BMI contributes to more panic of being judged negatively by others, as individuals avoid from being exposed to situations in which their look may be criticized and commented (Claes et al., 2012; Koskina et al., 2011; Levinson and Rodebaugh, 2012). This contradictory result could be due to the prevalence of obesity and excess weight among Malaysians and their wrong perception of obesity and overweight, as for Malaysians obesity is symbolized as “being happy” (Muda et al., 2015). This seemingly reflects that “it’s alright to be obese, and only happy people have good appetite” (Muda et al., 2015). Therefore, such perception of obesity and excess weight may not lead to dread of being present in public, or any subsequent social disconnectedness.
The findings support the idea that possessing high self-esteem intensifies the negative relationship between BMI and BI and explains failure in the correlation between BMI and FNE. The moderating effect of self-esteem supports the contention that self-esteem may be an important resource in reducing the magnitude of the negative relationship between BMI and BI (H3), and justifying the absence of an association between BMI and FNE (H4). These results are consistent with studies which demonstrate that self-esteem protects individuals against their own negative feelings about their body and others’ negative evaluation of their body (Ahadzadeh et al., 2017; Dunaev et al., 2018; Junghans-Rutelonis et al., 2015). Individuals with high self-esteem are more likely to report less negative feelings about their body and appearance and show less fright of others’ judgment regarding their body as to whether they are overweight, underweight, or normal weight. They tend to feel positive about their body, while those with low self-esteem tend to appraise their appearance in a more negative and critical light. High self-esteem brings about individuals to accept imperfection in their look and body, and makes them feel that they deserve to be valued and respected by themselves and others regardless of their appearance. Indeed, people with high self-esteem appreciate their strengths, invest on their abilities and competencies, and do not put themselves down if they are not happy with their appearance. They feel that they are good enough to express themselves in public, even dealing with difficult feelings or situations. In other words, self-esteem directly influences people’s feelings, thoughts, and behaviors related to their appearance. If individuals feel good about their whole self, particularly their body, and place importance on themselves, they are more likely to notice the good things of their body and respect their body. In fact, people with high self-esteem venerate themselves, tend to think realistically, and attempt to get along with the dissatisfactory feeling of their appearance.
Given that BMI is a negative determinant of BI, the blueprint of a systematic approach toward obesity, and implementation of clinical and public health-related policies are strongly suggested to highlight the detrimental consequences of this problem, as a risk factor in non-communicable diseases. Findings also indicate that self-esteem protects individuals, particularly the overweight and the obese, from the negative impact of high BMI on BI and FNE. These results underscore the significance of intervention programs to boost young adults’ self-esteem against being negatively affected by high BMI. However, overreliance on self-esteem as a protective source against the adverse correlation between BMI and BI and FNE in the long term may bring along some unpleasant biological consequences, such as cardiovascular diseases (Ahadzadeh et al., 2017; Mandviwala et al., 2016), which is the leading cause of deaths worldwide (Lüscher, 2016). Therefore, the seamy side of high self-esteem in the case under investigation should be considered in designing intervention programs.
The results could contribute to the enhancement of other psychological problems such as low self-esteem. Low self-esteem could be due to a poor or negative self-image, and could turn into a subconscious prophecy to expect failure during individuals’ lives all the time. The effective and affective elements in the development of positive BI could be utilized in fortifying the manifestation of self-esteem. Therefore, obliteration of negative emotional and psychological factors could lead to more enhanced social support, more efficient social performance, and less intrapersonal like self-appreciation and interpersonal deficiency like building relationships.
This study has several limitations. No causal relationship between the measures of BMI, BI, and FNE was implied, as this study used a cross-sectional design to examine relationships among the measures and moderating effect of self-esteem. Additional research is required to examine a causal path model, including more specific measures of appearance self-schema, appearance self-discrepancy, and other measurements of BI. Future studies could assess the possible influence of some confounding variables, such as gender in the correlation between BMI, BI, and FNE. Bearing in mind that self-reported data on BMI may affect the validity and reliability of the results, future studies may look for actual BMI to achieve better reliability and validity. Another limitation was the location of the study, that is, a Chinese private university in Kuala Lumpur, Malaysia. Therefore, investigating BMI, BI, and FNE in a more diverse setting with more equal and various ethnic distribution would provide a more representative sample.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this.
References
- Ahadzadeh AS, Pahlevan Sharif S, Ong FS. (2017) Self-schema and self-discrepancy mediate the influence of Instagram usage on body image satisfaction among youth. Computers in Human Behavior 68: 8–16. [Google Scholar]
- Anderson JC, Gerbing DW. (1988) Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin 103(3): 411–423. [Google Scholar]
- Brannan ME, Petrie TA. (2011) Psychological well-being and the body dissatisfaction-bulimic symptomatology relationship: An examination of moderators. Eating Behaviors 12(4): 233–241. [DOI] [PubMed] [Google Scholar]
- Brechan I, Kvalem IL. (2015) Relationship between body dissatisfaction and disordered eating: Mediating role of self-esteem and depression. Eating Behaviors 17: 49–58. [DOI] [PubMed] [Google Scholar]
- Cash TF, Pruzinsky T. (2004) Body Image: A Handbook of Theory, Research, and Clinical Practice. New York: Guilford Press. [Google Scholar]
- Chin WW. (1998) The partial least squares approach to structural equation modeling. Modern Methods for Business Research 295(2): 295–336. [Google Scholar]
- Claes L, Hart TA, Smits D, et al. (2012) Validation of the social appearance anxiety scale in female eating disorder patients. European Eating Disorders Review 20(5): 406–409. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- DiClemente CC, Delahanty J. (2016) Homeostasis and change: A commentary on homeostatic theory of obesity by David Marks. Health Psychology Open 3(1): 2055102916634366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunaev JL, Schulz JL, Markey CN. (2018) Cosmetic surgery attitudes among midlife women: Appearance esteem, weight esteem, and fear of negative appearance evaluation. Journal of Health Psychology 23(1): 59–66. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Blackman LR, Avellone ME. (2000) The relationship between body image discrepancy and body mass index across ethnic groups. Obesity Research 8(8): 582–589. [DOI] [PubMed] [Google Scholar]
- Fornell C, Larcker DF. (1981) Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research 18(1): 39–50. [Google Scholar]
- Garousi S, Garrusi B, Divsalar F, et al. (2012) Body satisfaction and management in Iranian students. Materia Socio-Medica 24(1): 34–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair JF, Ringle CM, Sarstedt M. (2013) Editorial-partial least squares structural equation modeling: Rigorous applications, better results and higher acceptance. Long Range Planning 46(1–2): 1–12. [Google Scholar]
- Hair JF, Jr, Hult GTM, Ringle C, et al. (2017) A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM) (2nd edn). Thousand Oaks, CA: SAGE. [Google Scholar]
- Henseler J, Ringle CM, Sarstedt M. (2015) A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science 43(1): 115–135. [Google Scholar]
- Herbozo S, Thompson JK. (2006) Appearance-related commentary, body image, and self-esteem: Does the distress associated with the commentary matter? Body Image 3(3): 255–262. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Hinton DE. (2010) Cultural aspects in social anxiety and social anxiety disorder. Depression and Anxiety 27(12): 1117–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holsen I, Jones DC, Birkeland MS. (2012) Body image satisfaction among Norwegian adolescents and young adults: A longitudinal study of the influence of interpersonal relationships and BMI. Body Image 9(2): 201–208. [DOI] [PubMed] [Google Scholar]
- Institute for Public Health (IPH) (2015) National Health & Morbidity Survey 2015: Non-Communicable Diseases, Risk Factors & Other Health Problems, vol. II Kuala Lumpur, Malaysia: Institute for Public Health, National Institutes of Health, Ministry of Health. [Google Scholar]
- Jones DC, Crawford JK. (2005) Adolescent boys and body image: Weight and muscularity concerns as dual pathways to body dissatisfaction. Journal of Youth and Adolescence 34(6): 629–636. [Google Scholar]
- Junghans-Rutelonis AN, Suorsa KI, Tackett AP, et al. (2015) Self-esteem, self-focused attention, and the mediating role of fear of negative evaluation in college students with and without asthma. Journal of American College Health 63(8): 554–562. [DOI] [PubMed] [Google Scholar]
- Kalat JW. (2016) Introduction to Psychology. Pacific Grove, CA: Brooks Publishing. [Google Scholar]
- Kaminsky LA, Dewey D. (2014) The association between body mass index and physical activity, and body image, self esteem and social support in adolescents with type 1 diabetes. Canadian Journal of Diabetes 38(4): 244–249. [DOI] [PubMed] [Google Scholar]
- Kantanista A, Król-Zielińska M, Borowiec J, et al. (2017) Is underweight associated with more positive body image? Results of a cross-sectional study in adolescent girls and boys. Spanish Journal of Psychology 20: E8. [DOI] [PubMed] [Google Scholar]
- Khanam SJ, Moghal F. (2012) Self-esteem as a predictor of fear of negative evaluation and social anxiety. Pakistan Journal of Psychology 43(1): 91–100. [Google Scholar]
- Koskina A, Van den Eynde F, Meisel S, et al. (2011) Social appearance anxiety and bulimia nervosa. Eating and Weight Disorders–Studies on Anorexia, Bulimia and Obesity 16(2): e142–e145. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL. (2012) Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eating Behaviors 13(1): 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüscher TF. (2016) Prevention: Some important steps forward, but many unmet needs in a world with cardiovascular disease as the leading cause of death. European Heart Journal 37(42): 3179–3181. [DOI] [PubMed] [Google Scholar]
- Mandviwala T, Khalid U, Deswal A. (2016) Obesity and cardiovascular disease: A risk factor or a risk marker? Current Atherosclerosis Reports 18(5): 21. [DOI] [PubMed] [Google Scholar]
- Marks DF. (2015) Homeostatic theory of obesity. Health Psychology Open 2(1): 2055102915590692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muda WAMW, Kuate D, Jalil RA, et al. (2015) Self-perception and quality of life among overweight and obese rural housewives in Kelantan, Malaysia. Health and Quality of Life Outcomes 13(1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray K, Rieger E, Byrne D. (2013) A longitudinal investigation of the mediating role of self-esteem and body importance in the relationship between stress and body dissatisfaction in adolescent females and males. Body Image 10: 544–551. [DOI] [PubMed] [Google Scholar]
- Oney CN, Cole ER, Sellers RM. (2011) Racial identity and gender as moderators of the relationship between body image and self-esteem for African Americans. Sex Roles 65(7–8): 619–631. [Google Scholar]
- Osman A, Barrios FX, Kopper BA, et al. (2006) The body influence assessment inventory (BIAI): Development and initial validation. Journal of Clinical Psychology 62(7): 923–942. [DOI] [PubMed] [Google Scholar]
- Orbach I. (1996) The role of body experience in self-destruction. Clinical Child Psychology and Psychiatry 1(4): 607–619. [Google Scholar]
- Paxton SJ, Eisenberg ME, Neumark-Sztainer D. (2006) Prospective predictors of body dissatisfaction in adolescent girls and boys: A five-year longitudinal study. Developmental Psychology 42(5): 888–899. [DOI] [PubMed] [Google Scholar]
- Pelletier LG, Guertin C, Pope JP, et al. (2016) Homeostasis balance, homeostasis imbalance or distinct motivational processes? Comments on Marks (2015) “homeostatic theory of obesity.” Health Psychology Open 3(1): 2055102915624512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricciardelli LA, McCabe MP. (2001) Self-esteem and negative affect as moderators of sociocultural influences on body dissatisfaction, strategies to decrease weight, and strategies to increase muscles among adolescent boys and girls. Sex Roles 44(3–4): 189–207. [Google Scholar]
- Rosenberg M. (1965) Society and Adolescent Self-Image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Seidman G. (2013) Self-presentation and belonging on Facebook: How personality influences social media use and motivations. Personality and Individual Differences 54(3): 402–407. [Google Scholar]
- Shloim N, Hetherington MM, Rudolf M, et al. (2015) Relationship between body mass index and women’s body image, self-esteem and eating behaviours in pregnancy: A cross-cultural study. Journal of Health Psychology 20(4): 413–426. [DOI] [PubMed] [Google Scholar]
- De Sousa Fortesa L, Ciprianib F, Coelhob F, et al. (2014) Does self-esteem affect body dissatisfaction levels in female adolescents? Revista Paulista de Pediatria 32(3): 236–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK, Shroff H, Herbozo S, et al. (2007) Relations among multiple peer influences, body dissatisfaction, eating disturbance, and self-esteem: A comparison of average weight, at risk of overweight, and overweight adolescent girls. Journal of Pediatric Psychology 32(1): 24–29. [DOI] [PubMed] [Google Scholar]
- Watkins JA, Christie C, Chally P. (2008) Relationship between body image and body mass index in college men. Journal of American College Health 57(1): 95–100. [DOI] [PubMed] [Google Scholar]
- Yates A, Edman J, Aruguete M. (2004) Ethnic differences in BMI and body/self-dissatisfaction among Whites, Asian subgroups, Pacific Islanders, and African-Americans. Journal of Adolescent Health 34(4): 300–307. [DOI] [PubMed] [Google Scholar]