Abstract
Background:
Intramedullary epidermoid cyst (IEC), typically associated with spinal dysraphism, is rare, with fewer than 80 such cases reported in the literature. Here we present an adult with an IEC without spinal dysraphism.
Case Description:
A 41-year-old female presented with the gradual onset of a progressive spastic paraparesis attributed to a magnetic resonance imaging (MRI)-documented D8-9 intramedullary lesion. Following microsurgical excision of the IEC, she fully recovered.
Conclusion:
IECs are rare lesions, typically found in conjunction with spinal dysraphism. Utilizing MRI studies to document the lesion location, gross total microsurgical excision is the procedure of choice. Early excision of these benign lesions maximizes functional recovery.
Keywords: Dysraphism, epidermoid, intramedullary, spinal
INTRODUCTION
Inclusion of ectodermal tissue remnants, entrapped during the 3rd and 5th week of gestation during neural tube closure, gives rise to epidermoid cysts.[1] An intramedullary epidural cyst (IEC) composed of stratified squamous epithelium rarely occurs without spinal dysraphism; there are less than 80 such cases reported in the literature.[5]
Here, we present an adult with an IEC identified on magnetic resonance (MR) at the D8-9 level that was successfully excised without residual neurological deficit or recurrence (e.g., at 6 months.)
CASE REPORT
A 41-year-old female presented with a progressive spastic paraparesis (e.g., left greater than right) of 2 years duration accompanied by 1 month of urinary incontinence. The examination revealed right lower extremity motor function at 2/5, left at 4/5, diffuse lower extremity hyperreflexia, bilateral Babinski responses, and a relative bilateral T12 sensory level.
The MR image revealed a well-defined intramedullary lesion at the D8-9 level, measuring 3.1 × 1.2 × 1.2 cm (vertical, anterior–posterior, transverse diameter). It was hypointense on T1, hyperintense on T2-weighted images, with a faint rim of enhancement with post gadolinium diethylenetriamine pentaacetate (GD-DTPA) injection [Figure 1]. The computed tomography (CT) was unremarkable. Following a D8-9 laminectomy and durotomy, performed under somatosensory evoked potential and motor evoked potential monitoring, the tumor surfaced on the left side of the cord. It was pearly white and had a well-defined plane except posteriorly where capsule was densely adherent to the cord/parenchyma [Figure 2]. The lesion was excised except for the posterior capsule that could not be safely dissected away from the cord. Histopathology confirmed the diagnosis of an IEC; the epidermoid contained lamellated keratinous flakes, dystrophic calcification without adnexal structures, and an inflammatory response/giant cell formation [Figure 3]. Six months postoperatively, the patient ambulated without support, having regained 4+/5 function in both lower extremities. The follow-up contrast-enhanced MRI showed no residual/recurrent lesion [Figure 4].
Figure 1.
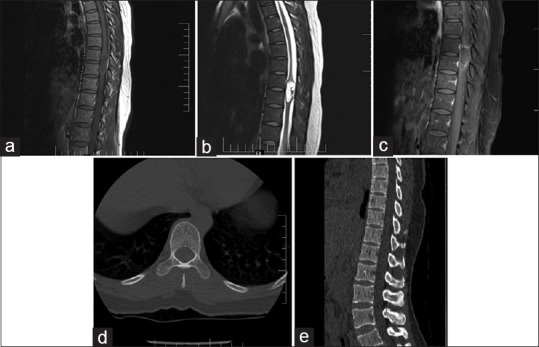
Preoperative CT and MRI. (a-c) T1 and T2 weighted sagittal images showing intramedullary lesion at D8-9 level with faint peripheral enhancement on gadolinium contrast. (d and e) Preoperative CT dorsal spine axial and sagittal images: not showing any abnormality
Figure 2.
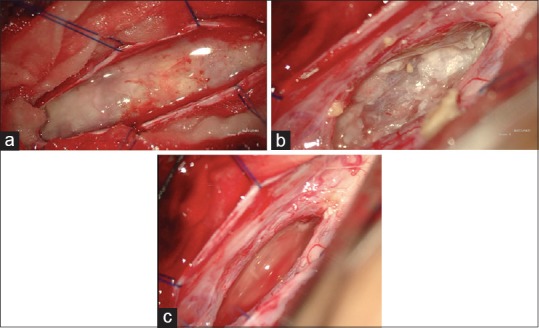
Intraopeartive images. (a) Lesion surfacing after durotomy, (b) pearly white material seen during decompression of the tumor and (c) tumor cavity after decompression
Figure 3.
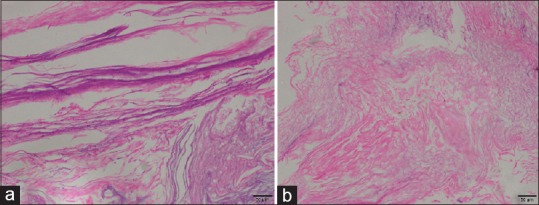
Histological images. (a and b): Photomicrograph of an epidermoid cyst with lamellated keratin. Adnexal structures were not seen. (H&E, ×100)
Figure 4.
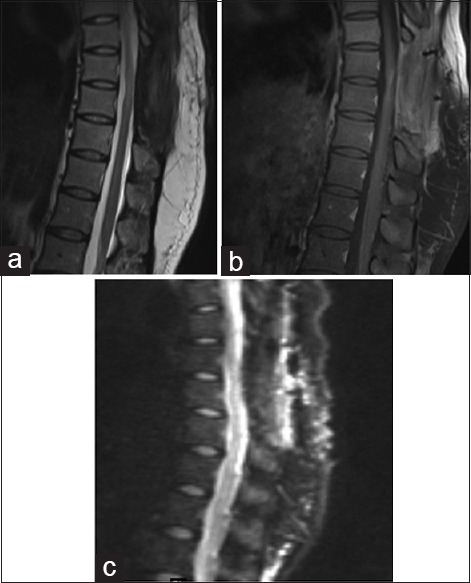
Follow up MRI at 6 months. (a-c) T2 weighted sagittal, T1 gadolinium contrast and diffusion images: no evidence of recurrence. Post op changes noted. (Preoperative diffusion sequence was not available)
DISCUSSION
Spinal IEC in adults constitutes <1% of intramedullary tumors.[5] IECs are either congenital or acquired; some of the latter have attributed to lumbar punctures (e.g., resulting from iatrogenic skin fragment penetration).[5] These lesions are diagnosed late in the clinical course as the onset of subacute/acute paraparesis with/without sphincter dysfunction is often delayed. Here the patient presented with a spastic paraparesis of 2 years duration with urinary incontinence for just one month's duration. The MR diagnosis of IEC is difficult and major differential diagnostic considerations include arachnoid cyst, ependymoma, and astrocytoma.[6] As noted in this case, IEC on MRI is typically hypo or isointense on T1, hyperintense on T2, with variable enhancement of the cyst wall (T1 with GD-DTPA).
Although microsurgical excision provides the best chance for cure, if lesion's capsules are densely populated surrounding normal neural tissues, then they should be left in place to avoid increasing surgical/neurological dysfunction/morbidity.[2,4] Although some have reported a role for radiotherapy (RT) for treating recurrent IEC, RT is not an established treatment for these lesions.[3]
CONCLUSION
IECs are rare in adults without spinal dysraphism. Here, an adult presented with a 2-month history of a progressive paraparesis and an MR-documented T8-9 lesion. Six months following microsurgical subtotal excision of the IEC (e.g. residual posterior capsule densely adherent to the cord), the patient recovered 4+/5 motor function and, the MR documented no tumor recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Ajit M. Mishra, Email: drajitm@gmail.com.
A. R. Prabhuraj, Email: drprabhuraj@yahoo.co.in.
Nupur Pruthi, Email: pruthi_nupur@yahoo.co.in.
Shilpa Rao, Email: shilpagk.rao@gmail.com.
REFERENCES
- 1.Babayev R, Abbasov B, Eksi MS. Thoracic intramedullary epidermoid cyst—timely fashion diagnosis and treatment. Childs Nerv Syst. 2015;31:793–6. doi: 10.1007/s00381-015-2625-6. [DOI] [PubMed] [Google Scholar]
- 2.Bansal S, Ailawadhi P, Suri A, Kale SS, Sarat Chandra P, Singh M, et al. Ten years’ experience in the management of spinal intramedullary tumors in a single institution. J Clin Neurosci. 2013;20:292–8. doi: 10.1016/j.jocn.2012.01.056. [DOI] [PubMed] [Google Scholar]
- 3.Bretz A, Van den Berge D, Storme G. Intraspinal epidermoid cyst successfully treated with radiotherapy: Case report. Neurosurgery. 2003;53:1429–31. doi: 10.1227/01.neu.0000093828.70768.40. [DOI] [PubMed] [Google Scholar]
- 4.Chandra PS, Manjari T, Devi BI, Chandramouli BA, Srikanth SG, Shankar SK. Intramedullary spinal epidermoid cyst. Neurol India. 2000;48:75–7. [PubMed] [Google Scholar]
- 5.Graillon T, Rakotozanany P, Meyer M, Dufour H, Fuentes S. Intramedullary epidermoid cysts in adults: Case report and updated literature review. Neurochirurgie. 2017;63:99–102. doi: 10.1016/j.neuchi.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Kukreja K, Manzano G, Ragheb J, Medina LS. Differentiation between pediatric spinal arachnoid and epidermoid-dermoid cysts: Is diffusion-weighted MRI useful? Pediatr Radiol. 2007;37:556–60. doi: 10.1007/s00247-007-0463-8. [DOI] [PubMed] [Google Scholar]


