Abstract
Background:
Small-diameter autograft hamstring grafts have been linked to graft failure after anterior cruciate ligament (ACL) reconstruction. The frequency of hamstring autografts that actually meet ideal size criteria remains unknown.
Purpose:
To examine a large cohort of patients to (1) evaluate sizing variability among a large cohort of surgeons and (2) identify patient factors most predictive of hamstring autograft size.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 1681 ACL reconstructions with hamstring autograft were analyzed as completed by 11 surgeons over a 13-year period. Patient demographics (age, height, weight, body mass index, sex) and intraoperative details (including graft diameter and strands) were extracted. Univariate and multivariate regression analyses were performed to correlate patient demographics with graft size and to develop a predictive model for hamstring graft size.
Results:
The mean height and weight of patients included in this study were 172.7 cm and 80.1 kg, respectively; 59% of patients were male. The mean diameters of hamstring autografts were 8.4 mm and 8.2 mm for the tibial and femoral ends of the graft, respectively. A total of 55.1% of grafts were ≤8 mm. Mixed-effects linear modeling revealed that height, weight, sex, and use of ≥5 strands correlated with graft size (P < .001), while age did not. The predictive multivariate model based on the statistically relevant factors demonstrated a moderate correlation (r = 0.39, R 2 = 0.150), illustrated a predictive equation, and proved height to be the greatest determinant of graft size.
Conclusion:
Marked variability in graft size distribution was found among surgeons, and more than half of all grafts did not reach the ideal size for hamstring autograft ACL reconstruction. A predictive equation including anthropometric factors may be able to provide the expected graft size. The risk of early graft failure may be mitigated with preoperative consideration of anthropometric factors—most importantly, height—in preparation for possible augmentation, additional strands, or alternative graft sources.
Keywords: hamstring, autograft, anthropometric, sizing, prediction, ACL reconstruction
The anterior cruciate ligament (ACL) is the most commonly reconstructed ligament of the knee, with more than 200,000 procedures performed a year in the United States.2 Graft selection in ACL reconstruction depends on many factors, including surgeon preference, patient age, and activity level.6 While allografts have been associated with a high failure rate following ACL reconstruction, hamstring autografts provide postsurgical patient-reported outcomes and failure rates similar to those of patellar tendon autografts. Some proponents of autograft hamstring ACL reconstruction cite decreased morbidity of hamstring autografts (ie, anterior knee pain and knee extension loss) as a reason for its use in ACL reconstruction.3–5,11,12,14,15 However, questions still exist with regard to ideal graft strand number and graft diameter.
Graft diameter, in particular, has become a topic of recent interest as a predictor of subsequent graft failure after ACL reconstruction with hamstring autograft. Magnussen et al16 retrospectively reviewed 256 patients who underwent hamstring autograft reconstruction and found hamstring autograft size ≤8.0 mm to correlate with subsequent failure among patients younger than 20 years, although only 17 revision surgery cases among 119 patients younger than 20 years were available for study. Treme et al23 prospectively evaluated 50 patients and found that those weighing <50 kg, measuring <140 cm in height, and having a thigh circumference <37 cm and a body mass index (BMI) <18 should be considered high risk for having a quadrupled hamstring graft diameter <7 mm. With a large cohort (N = 2240), Snaebjörnsson et al21 demonstrated that patients had a 0.86-times lower likelihood of revision surgery with every 0.5-mm increase in hamstring autograft. However, some results were mixed. In a level 4 retrospective case series of 786 patients, Wernecke et al25 found that increased autograft hamstring diameter did not significantly reduce revision risk after hamstring autograft.
As small-diameter grafts have been implicated as a potential cause of graft rupture following ACL reconstruction, preoperative knowledge of those prone to needing alternative graft sources, additional strands, or allograft augmentation is of interest to surgeons. Additionally, knowledge of the baseline prevalence of patients in practice who are predisposed to failure is necessary to understand the magnitude of addressing graft size challenges. Although the literature outlines the parameters for the ideal hamstring autograft size, no study to our knowledge has reported the trends of graft sizes or the prevalence of ideally sized grafts in a large cohort within the general population of patients requiring ACL reconstruction. The purpose of this study was to examine a large cohort of patients to (1) evaluate sizing variability among a large cohort of surgeons and (2) identify the patient factors that are most predictive of hamstring autograft size.
Methods
This study was approved by the Cleveland Clinic Institutional Review Board. We retrospectively reviewed all patients undergoing ACL reconstruction at our institution from January 1, 2000, to June 30, 2013. The patients were identified via the Current Procedural Terminology code 29888 for ACL reconstruction.
Inclusion and Exclusion Criteria
Patient records meeting the following criteria were included for analysis: (1) primary ACL reconstruction with a hamstring autograft with or without gracilis; (2) operation performed by a surgeon performing >5 ACL reconstructions annually; (3) available demographic data, including age, sex, height, and weight; and (4) available intraoperative details, including graft choice, graft diameter, and number of graft strands utilized.
Patient records were excluded for the following reasons: (1) ACL reconstruction with an allograft, bone–patellar tendon–bone autograft, quadriceps autograft, or any other autograft not including the gracilis or hamstring; (2) operation performed by a surgeon performing ≤5 ACL reconstructions annually; (3) records failing to identify patient age, sex, height, or weight; (4) records failing to include the number of strands in the graft; or (5) records failing to include graft size or both femoral and tibial tunnel diameters.
Study Data
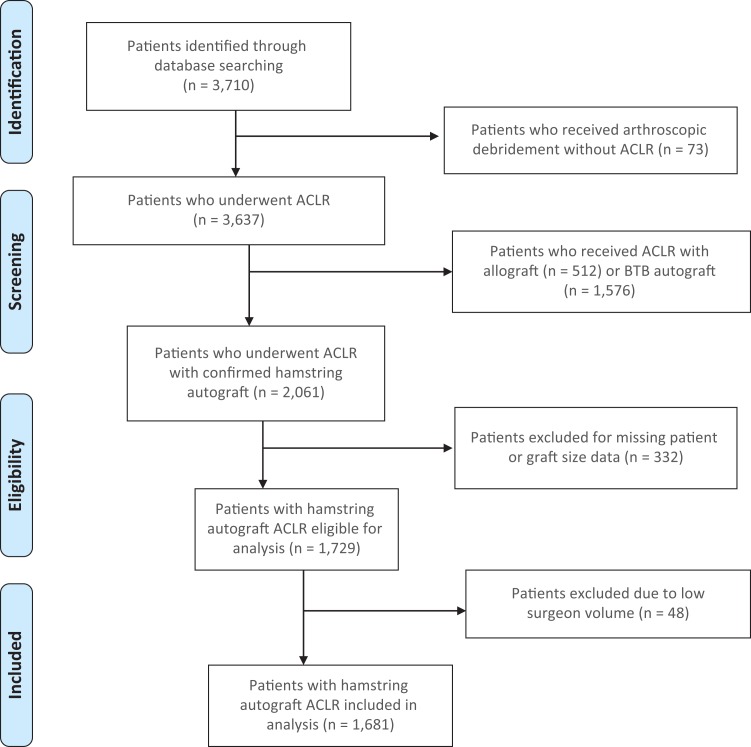
The following patient data were extracted from the electronic medical record: age, sex, weight, height, year of surgery, and the number of strands composing the autograft (4 vs ≥5). Graft size was determined through sizing guides with 0.5-mm increments. The force with which the graft was pulled through was with unknown tensioning force. If the graft size was not available, the femoral tunnel diameter was used as a surrogate to represent the size of the hamstring graft, given that it was considered reflective of the functional diameter of the graft since surgeons selected the smallest value at least as large as the actual graft. A modified PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart is depicted in Figure 1 for transparency of the patient record selection process.
Figure 1.
Modified PRISMA flow diagram of patient selection process. ACLR, anterior cruciate ligament reconstruction; BTB, bone–patellar tendon–bone.
Statistical Analysis
For the “unadjusted” (univariate) comparisons, levels of the binary categorical variables (sex, gracilis included, and number of strands) were compared on femoral tunnel diameter using the Welch two-sample t-test. A linear mixed-effects regression model was used to control for confounders. Categorical variables (surgeon, year of surgery) were compared with graft or femoral tunnel diameter via analysis of variance. Associations between numeric predictor variables (year of surgery, patient age, height, weight, and BMI) and graft or femoral tunnel diameter were tested with Pearson correlations. The unadjusted univariate analyses were built into a multivariate linear regression model for descriptive and prediction purposes, of which 20% of the observations were set aside as a test data set and the model was built on the remaining 80%. The descriptive multivariate regression model identified the factors affecting the graft size, and the predictive model identified the relationship (direct or indirect) and magnitude of each predictor. After the model based on the test data set was built and validated, the model coefficients were refit on the entire (training and test data recombined) data set to identify the predictors of graft size and to develop a predictive equation. All analyses were performed with the R statistical programming language (R 3.2.3; https://www.R-project.org/).20 All testing was 2-sided and considered significant at the 5% level.
Results
Table 1 depicts the full demographic and anthropometric data from the 1681 patients who underwent ACL reconstruction with hamstring autograft. A total of 1431 ACL cases measured graft size, and 250 documented only femoral and tibial tunnel diameters.
TABLE 1.
Anthropometric Data From Study Patients
| Mean ± SD or % | |
|---|---|
| Age, y | 28.7 ± 11.8 |
| Male | 59 |
| Height, cm | 172.7 ± 10.0 |
| Weight, kg | 80.1 ± 18.6 |
| Body mass index | 26.8 ± 5.1 |
| Graft diameter, mm | |
| Tibial | 8.4 ± 0.9 |
| Femoral | 8.2 ± 0.9 |
The mean graft diameters were 8.4 mm and 8.2 mm for the tibial and femoral ends, respectively. A total of 55.1% of grafts were ≤8 mm, with significant surgeon variability. Table 2 demonstrates the full distribution and variability of graft size by surgeon using the autograft.
TABLE 2.
Graft Size Distribution Among Surgeons
| Surgeon, % | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Graft diameter, mm | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
| >9 | 10.7 | 8 | 1.4 | 2.9 | 7.1 | 14.1 | 19.3 | 7.1 | 3.3 | 3.9 | 9.1 | 7.9 |
| 9 | 29.3 | 40 | 22.2 | 17.8 | 25.2 | 25.2 | 41.5 | 30.4 | 11.7 | 61.5 | 36.4 | 31.0 |
| 8.5 | 10.7 | 0 | 0 | 7.1 | 13.1 | 13.1 | 2.3 | 10.7 | 15.6 | 3.9 | 0 | 6.0 |
| 8 | 30.7 | 38 | 45.8 | 32.4 | 60.7 | 33.3 | 29 | 35.7 | 39 | 26.9 | 51.5 | 38.2 |
| 7.5 | 9.3 | 0.4 | 0 | 15.3 | 3.6 | 6.9 | 0.8 | 8.9 | 13 | 0 | 0 | 4.8 |
| 7 | 8 | 12.5 | 30.6 | 24.1 | 7.1 | 7.5 | 5.9 | 7.1 | 13.6 | 3.9 | 3 | 11.1 |
| <7 | 1.3 | 0.4 | 0 | 0.6 | 0 | 0 | 1.2 | 0 | 3.9 | 0 | 0 | 1.0 |
| Total >8 | 50.7 | 48.0 | 23.6 | 27.8 | 45.4 | 52.4 | 63.1 | 48.2 | 30.6 | 69.3 | 45.5 | 44.9 |
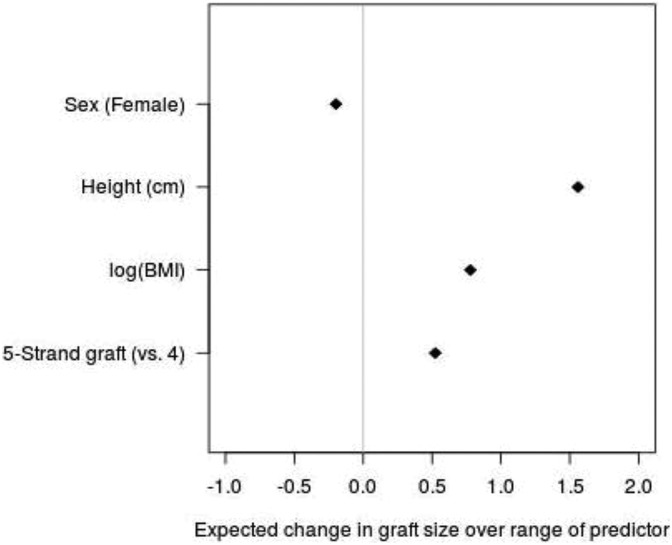
Table 3 depicts the descriptive multivariate regression model, which revealed that height, weight, sex (female), and use of ≥5 strands significantly correlated with graft size (P < .001), while age did not. After these 4 variables (sex, height, natural logarithm [ln] of BMI, and strands in the graft) were validated and applied to the predictive multivariate regression model, a moderate correlation (r = 0.39, R 2 = 0.150) was established. We used ln(BMI) for forecasting purposes in the regression analysis and to interpret changes in BMI as a linear percentage change to derive a clinically usable formula. Height was directly proportional to graft size and was the greatest predictor of graft size in this model. Increased BMI and 5-strand grafts resulted in increased graft size, as did male sex; however, sex as a whole was the least predictive factor. Figure 2 illustrates the effect of the 4 determinants of the autograft size prediction model.
TABLE 3.
Output of Multivariate Regression Model Identifying Predictors of Graft Size
| Fixed Effect | Coefficient | SE | 95% CI | P |
|---|---|---|---|---|
| Intercept | 3.428 | 0.483 | 2.481 to 4.375 | <.001 |
| Female | –0.202 | 0.052 | –0.303 to –0.100 | <.001 |
| Age | 0.003 | 0.002 | –0.001 to 0.006 | .122 |
| Height, cm | 0.025 | 0.003 | 0.020 to 0.030 | <.001 |
| Body mass index | 0.021 | 0.004 | 0.013 to 0.028 | <.001 |
| Gracilis includeda | 0.028 | 0.070 | –0.109 to 0.165 | .685 |
| 5-strand graft, vs 4b | 0.518 | 0.092 | 0.334 to 0.702 | <.001 |
aGracilis was included in the 4- or 5-strand graft as additional tissue or core strands.
bThree equal strands of the semitendinosus combined with a double-stranded gracilis.
Figure 2.
Depiction of the magnitude and relationship between predictors and graft size. Log(BMI), natural logarithm of body mass index.
The final coefficients of the 4 statistically significant predictors can be found in Table 4 and are interpreted as follows:
TABLE 4.
Coefficients for Determinants of Predictive Equation for Hamstring Autograft Size
| Predictor | Coefficient |
|---|---|
| Intercept | 2.074 |
| Sex, female | –0.198 |
| Height, cm | 0.025 |
| ln(BMI)a | 0.623 |
| 5-strand graft, vs 4 | 0.523 |
aNatural logarithm of body mass index.
Thus, a male 198 cm tall with a BMI of 25 and a 5-stranded graft would be predicted to yield a graft size of 9.5 mm.
Discussion
This retrospective study of 1681 ACL reconstruction cases with a hamstring autograft at a single institution over 13 years met several objectives with the application of a large cohort. The principal findings demonstrated baseline demographic and trends data in the form of anthropometric characteristics, and a mean graft size of 8.2 to 8.4 mm was established. More than half of the grafts encountered in our study cohort failed to have a graft >8 mm. Additionally, large surgeon variability was found in terms of the graft size used. Descriptive regression analysis identified height, weight, 5-strand grafts, and sex to be relevant anthropometric factors related to graft size, while age did not significantly contribute. Height was found to be the greatest predictor of graft size.
The mean graft size in this study was just below 8.5 mm. Magnussen et al16 retrospectively studied 256 consecutive patients with hamstring autografts and found that patients younger than 20 years of age with a graft size ≤8.0 mm had higher rates of graft failure as compared with patients with larger grafts, albeit in a group of 17 patients aged <20 years who were undergoing revision. While the number of patients and the mean graft size of 7.9 mm in that study were smaller than those of the present study, our findings reinforce the notion that the mean graft size may be insufficient. Nevertheless, other factors, such as sex and sport, may contribute to ACL failure rates.25
In a study of 20 fresh-frozen hamstring allografts, Cruz et al8,9 reported that graft sizes may be overestimated during preparation and that bone tunnels could be drilled up to 1.0 mm smaller. The authors suggested that graft diameter is merely an indicator of total collagen content and that the measured graft size is not necessarily as important as the fact that more collagen is being implanted to reconstruct the ACL. This biological model has not been studied to the extent of the biomechanical role of graft size. In a caprine model assessing the biomechanical role of graft width and laxity, 16 patellar tendon autografts demonstrated that the use of larger grafts does not provide greater biomechanical properties but may block extension.10 More study into the biological principles driving the relationship among graft size, age-related changes, and failure rate is necessary.
Our study also reported on the distribution of autograft hamstring sizes available to 11 surgeons and found that 55.1% of grafts were ≤8 mm, with marked surgeon variability. Not including the decrease in size after preparation described by Cruz et al,9 this finding demonstrates that the average patient in need of an ACL reconstruction is at risk for insufficient hamstring autograft diameter when quadruple stranded grafts are utilized. With this knowledge, the surgeon should be prepared to add additional strands, augment with allograft, or consider an alternative graft choice altogether. These options can now be discussed with patients before surgery based on their demographic parameters. However, each of these options has limitations. As an example, Pennock et al,18 in a study of 26 adolescent patients with ACL ruptures necessitating hamstring autografts augmented with allograft, found that this did not reduce graft retear rates and may have contributed to earlier graft failure.
To preoperatively identify patients with insufficient hamstring autograft sizes, we used a regression model assessing the anthropometric clinical data and found height, weight, 5-strand grafts, and male sex to be predictors of graft size. Height had the greatest impact on the diameter of the hamstring graft. Our findings are consistent with other studies that correlated a relationship between anthropometric data and hamstring autograft size.1,7,13,17,19,21–24 In an observational study by Janssen et al13 of 725 patients, height and weight were most predictive of graft size in men, whereas only height was predictive for women; male sex was also predictive of autograft size. Similarly, Pinheiro et al19 analyzed 80 patients having ACL reconstruction with hamstring tendons in a quadruple graft and found that graft diameter was related to height, sex, leg and thigh length, weight, and thigh diameter.
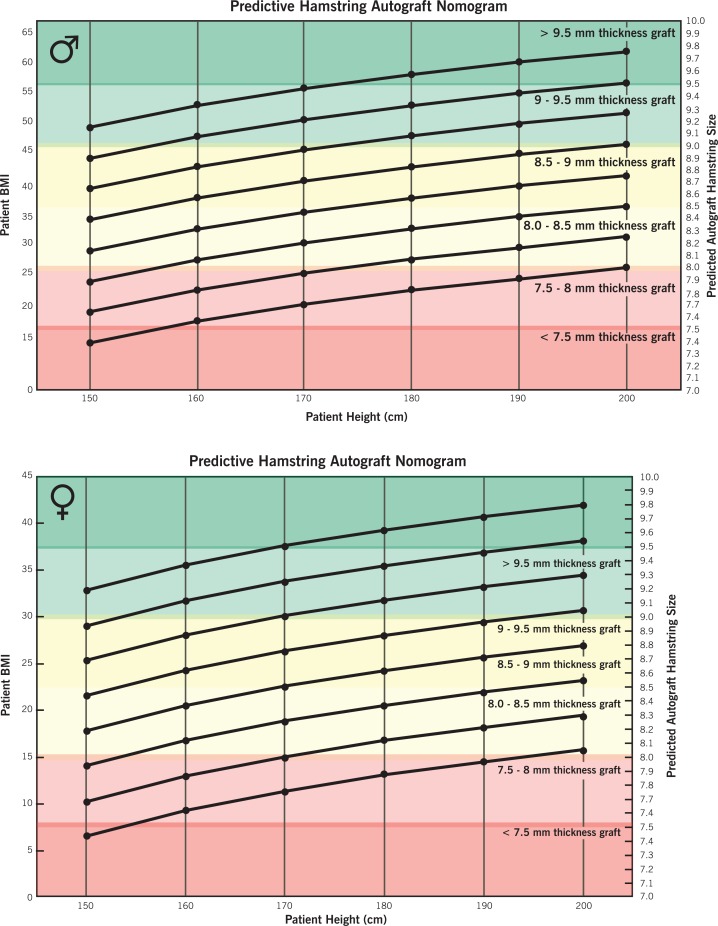
Another key finding from our study was the predictive equation with the coefficients from the multivariate regression analysis. In summary, all grafts start with a baseline value of 2 mm, are subtracted by 0.2 mm if female, are increased by 0.5 mm if using a 5-string graft, and require coefficient calculation with the patient’s height and natural logarithm of the BMI. In the Indian Journal of Orthopaedics, Asif et al1 reported the only other predictive equation based on multiple regression analysis coefficients in a population of 46 patients (44 males, 2 females) and used only height and thigh circumference as parameters. While the coefficients from our regression analysis equation require further prospective comparison and validation, it represents an important first step in preoperatively planning for those with potentially undersized autografts. A predictive nomogram for autograft hamstring size was developed with the height in centimeters and the natural logarithm of the BMI (Figure 3).
Figure 3.
Predictive nomogram for hamstring autograft sizing based on patient height and body mass index (BMI). For females, subtract 0.2 mm from the predicted thickness. For 5-strand grafts, add 0.5 mm to the predicted thickness.
Regarding the variability in graft size distribution among the studied surgeons, 3 of the 11 surgeons used grafts >8 mm with the following low frequences: 23.6%, 27.8%, 30.6%. Other surgeons reported using a graft >8 mm as high as 69% of the time. This variability introduces questions beyond general population variation. Surgeons may overestimate the graft or tunnel size. Tunnel size can be overestimated to facilitate easier graft passage, as certain suspensory fixation devices on the femoral side require easy graft passage into the femoral tunnel. Alternatively, other suspensory devices and interference screws permit line-to-line sizing of the femoral tunnel, as passage of the graft into the knee can still be accomplished even with a graft-tunnel interference fit. Notwithstanding interobserver measurement error, the advantage of studying the ACL patient population at a single institution is the theoretical equivalence of the population pool among surgeons, although surgeon preference was not accounted for and may result in an unaccounted selection bias. This stable population suggests that the surgeon variation found in a single institution might in fact parallel that found at the general level; however, further study from institutions throughout the country is required.
The most important limitation of this study was that sizing of the graft was not standardized among all studied surgeons. The retrospective nature of the study did not control for nonstandardized measurement standards, and we did not include additional surgery-specific information, including surgical technique and graft details such as fixation method and graft composition. These factors certainly affect the ACL retear rate from biomechanical and clinical perspectives, as graft size alone does not contribute to failure.
Another limitation was that not all surgeons recorded graft and/or tunnel diameter, which resulted in a loss of 16.5% of the available patients. Documentation of intraoperative measurements for all patients would have been ideal; however, only 85.1% of the patients had measurements of the actual graft recorded, and for the rest we depended on tunnel measurements. While the error for tunnel measurements was 0.5 mm from our surgeon group, this did result in imprecision. In addition, multivariate regression model demonstrated moderate correlation at r = 0.39, which suggests that other factors more predictive exist or the anthropometric measures themselves do not correlate strongly. Some factors that may contribute to graft size but were not studied include surgeon experience and technique. While the relationship between small graft size and rupture rate is well established in the literature, this study did not review the relationship between graft size and revision rate or patient-reported outcomes.
To our knowledge, the present study comprises the largest cohort to date to evaluate the relationship of patient anthropomorphic data to hamstring autograft size. With the prevalence of small autograft hamstring sizes representing over half the study population, increased suspicion is warranted for patients who may need increased intraoperative attention. While the graft sizes used by surgeons demonstrated great variability, such patients present to clinic with anthropometric characteristics that may predict the size of the graft harvested. Age should not factor into consideration for graft size, although younger grafts may result in early revision attributed to alternative reasons unrelated to the size of the autograft. With height validated in this larger cohort as a key predictor of autograft size, the next step in advancing predictive power would be correlating height-based strata with autograft sizes to establish clinical expectation guidelines. In doing so, we may be better prepared to counsel patients and preoperatively plan for augmentation, other graft sources, or additional strands in ACL reconstruction.
Conclusion
Marked variability in graft size distribution was found among surgeons, and more than half of all grafts did not reach the ideal size for hamstring autograft ACL reconstruction. The harvesting of a small hamstring graft may be mitigated with preoperative consideration of anthropometric factors—most importantly, height—in preparation for possible augmentation, additional strands, or alternative graft sources.
Acknowledgment
The authors acknowledge William Messner.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: L.D.F. has received research support from the Musculoskeletal Transplant Foundation and Zimmer Biomet.
Ethical approval for this study was obtained from the Cleveland Clinic (FWA 00005367).
References
- 1. Asif N, Ranjan R, Ahmed S, Sabir AB, Jilani LZ, Qureshi OA. Prediction of quadruple hamstring graft diameter for anterior cruciate ligament reconstruction by anthropometric measurements. Indian J Orthop. 2016;50(1):49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bach BR, Boonos CL. Anterior cruciate ligament reconstruction. AORN J. 2001;74(2):152–166. [PubMed] [Google Scholar]
- 3. Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–1601. [DOI] [PubMed] [Google Scholar]
- 4. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37(12):2362–2367. [DOI] [PubMed] [Google Scholar]
- 5. Chang SK, Egami DK, Shaieb MD, Kan DM, Richardson AB. Anterior cruciate ligament reconstruction: allograft versus autograft. Arthroscopy. 2003;19(5):453–462. [DOI] [PubMed] [Google Scholar]
- 6. Chen L, Cooley V, Rosenberg T. ACL reconstruction with hamstring tendon. Orthop Clin North Am. 2003;34:9–18. [DOI] [PubMed] [Google Scholar]
- 7. Chiang ER, Ma HL, Wang ST, Hung SC, Liu CL, Chen TH. Hamstring graft sizes differ between Chinese and Caucasians. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):916–921. [DOI] [PubMed] [Google Scholar]
- 8. Cruz AI, Jr, Fabricant PD. Hamstring graft for ACL reconstruction: does size matter? Ann Transl Med. 2017;5(3):65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cruz AI, Jr, Fabricant PD, Seeley MA, Ganley TJ, Lawrence JT. Change in size of hamstring grafts during preparation for ACL reconstruction: effect of tension and circumferential compression on graft diameter. J Bone Joint Surg Am. 2016;98(6):484–489. [DOI] [PubMed] [Google Scholar]
- 10. Cummings JF, Grood ES, Levy MS, Korvick DL, Wyatt R, Noyes FR. The effects of graft width and graft laxity on the outcome of caprine anterior cruciate ligament reconstruction. J Orthop Res. 2002;20(2):338–345. [DOI] [PubMed] [Google Scholar]
- 11. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564–573. [DOI] [PubMed] [Google Scholar]
- 12. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. [DOI] [PubMed] [Google Scholar]
- 13. Janssen RP, van der Velden MJF, van der Besselaar M, Reijman M. Prediction of length and diameter of hamstring tendon autografts for knee ligament surgery in Caucasians. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1199–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:34–42. [DOI] [PubMed] [Google Scholar]
- 15. Lenehan EA, Payne WB, Askam BM, Grana WA, Farrow LD. Long-term outcomes of allograft reconstruction of the anterior cruciate ligament. Am J Orthop (Belle Mead NJ). 2015;44(5):217–222. [PubMed] [Google Scholar]
- 16. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 17. Mardani-Kivi M, Karimi-Mobarakeh M, Mirboolok A, et al. Predicting the hamstring tendon diameter using anthropometric parameters. Arch Bone Jt Surg. 2016;4(4):314–317. [PMC free article] [PubMed] [Google Scholar]
- 18. Pennock AT, Ho B, Parvanta K, et al. Does allograft augmentation of small-diameter hamstring autograft ACL grafts reduce the incidence of graft retear? Am J Sports Med. 2017;45(2):334–338. [DOI] [PubMed] [Google Scholar]
- 19. Pinheiro LF, Jr, de Andrade MA, Teixeira LE, et al. Intra-operative four-stranded hamstring tendon graft diameter evaluation. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):811–815. [DOI] [PubMed] [Google Scholar]
- 20. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2015. [Google Scholar]
- 21. Snaebjörnsson T, Hamrin Senorski E, Ayeni OR. et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D Values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med. 2017;45(9):2092–2097. [DOI] [PubMed] [Google Scholar]
- 22. Stergios PG, Georgios KA, Konstantinos N, Efthymia P, Nikolaos K, Alexandros PG. Adequacy of semitendinosus tendon alone for anterior cruciate ligament reconstruction graft and prediction of hamstring graft size by evaluating simple anthropometric parameters. Anat Res Int. 2012;2012:424158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Treme G, Diduch DR, Billante MJ, Miller MD, Hart JM. Hamstring graft size prediction: a prospective clinical evaluation. Am J Sports Med. 2008;36(11):2204–2209. [DOI] [PubMed] [Google Scholar]
- 24. Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(11):1945–1949. [DOI] [PubMed] [Google Scholar]
- 25. Wernecke GC, Constantinidis A, Harris IA, Seeto BG, Chen DB, MacDessi SJ. The diameter of single bundle, hamstring autograft does not significantly influence revision rate or clinical outcomes after anterior cruciate ligament reconstruction. Knee. 2017;24(5):1033–1038. [DOI] [PubMed] [Google Scholar]