Abstract
Background
Several nomograms were developed for predicting the potential recurrence and cancer death risk in renal cell carcinoma patients. The combination of TNM classification and appropriately selected clinical classifiers allows for the creation of simple and effective risk calculators.
Material/Methods
There were 230 patients with renal cell cancer enrolled in this study. Basic parameters of blood count, serum creatinine and sodium concentrations, and histopathological features of the tumors were analyzed. A determination of whether any of the tested parameters could be used to assess the prognosis of kidney cancer was performed.
Results
When the platelet cell count (PLT) increased by 10 thousand/μL, the risk of metastasis was higher by 5%, and cancer recurrence and death by 10%. A low-risk recurrence group was identified: T1b, PLT <230, Na of 140.6 mmol/L. A high-risk recurrence group was identified: T3a, PLT >280, Na of 143.4 mmol/L. A low-risk cancer specific mortality group was identified: T2a, absence of metastases, preoperative creatinine level of 85.6 μmol/L, and the value of PLT 227.0×103. A high-risk cancer specific mortality group was identified: T3a, the presence of metastases in the lungs (M), serum creatinine before treatment level of 97.9 μmol/L, and the value of PLT 299.5×103.
Conclusions
Preoperative PLT, serum sodium, and tumor staging were independent risk factors for local recurrence. Blood PLT, serum sodium, creatinine, and tumor staging were useful indicators for estimating 5-year cancer specific survival.
MeSH Keywords: Blood Cell Count, Creatinine, Kidney Neoplasms
Background
Despite advances in medicine, an increase in morbidity and mortality in renal cell cancer is still observed. The diversity of renal cell cancer does not allow unambiguous determination of prognosis. Given that 30% of patients with renal cell cancer confined to the organ after surgical treatment will develop disseminated disease, it is important to search for prognostic factors. Several nomograms were developed for predicting the potential recurrence and cancer death risk in long-term follow-up for both metastatic and local disease [1–5]. They are based mainly on the TNM classification. Molecular factors have not found so far had wider application due to the difficulty and cost of their determination. It seems that the combination of TNM classification and appropriately selected clinical classifiers could allow for the creation of simple and effective risk calculators.
Some studies have suggested that thrombocytosis, which can be defined as a platelet count (PTL) >400 000/μL, is a negative predictive factor for survival among patients with metastatic renal cell cancer. The purpose of this study was to determine if the PLT correlates with survival in patients with metastatic renal cell cancer as an independent prognostic factor and how it correlates with other well-known factors. In addition, serum sodium is a readily available, easily obtained, and routinely measured laboratory test. Recently, the predictive and prognostic role of low serum sodium has been recognized. It is known that hyponatremia is associated with poor outcomes in several medical conditions like liver cirrhosis, congestive heart failure, and infectious diseases as pneumonia, childhood meningitis, and necrotizing soft-tissue infection. Moreover, hyponatremia has recently been associated with poor overall survival in hepatocellular carcinoma, gastric cancer, and small cell lung cancer. In renal cell cancer, low serum sodium level has recently been associated with lower disease free and overall survival after nephrectomy.
The aim of this study was to analyze preoperative blood cell count parameters, serum sodium, and creatinine as independent risk factors of metastasis, local recurrence, and cancer specific survival in renal cell cancer; and to identify groups of patients at high risk of metastasis, local recurrence, and cancer specific survival based on the aforementioned parameters and tumor staging.
Material and Methods
The study was retrospective and used the medical records of 397 patients who underwent surgery due to kidney tumors at our center between the 2000 to 2006. During the five-year follow-up period, of the 397 patients, 230 patients with the postoperative diagnosis of non-metastatic renal cell carcinoma were enrolled in this study. The median follow-up was 3.98±0.99 years.
All patients in the study group underwent routine laboratory tests to qualify for their surgery at the time of admission to the hospital. Among the routine tests, the basic parameters of blood count, serum creatinine, and sodium were selected for our analysis. The study did not examine the documentation of patients with comorbidities that may have a direct impact on the analyzed parameters. We analyzed the data of histopathological material: histology, TNM, size and location of the removed tumor, and the positive margin in the case of the nephron sparing surgery (NSS). Histopathological tumor grade was rated according to the abbreviated three-grade Fuhrman scale. To determine clinical stage, data were analyzed according to the TNM classification available from 2010. This study was an attempt to determine whether any of the tested parameters could be used to assess the prognosis of kidney cancer so that a group of patients that require special oncological surveillance could be selected. All the information gathered were analyzed in relation to local recurrence, metastasis, and tumor-specific death.
Statistical analysis was performed using the program R [R Core Team (2012)]. The method of explaining the probability with which examined factors may contribute to the occurrence or not of an event (metastasis, recurrence or death) within 5-years of follow-up was based on the assumptions of logistic regression with an indication of the odds ratio. Based on the detected in multivariate logistic regression features coexisting with recurrence and death, a multidimensional classification of patients was performed, for which a taxonomic method “Wroclaw” was used that uses the metric taxonomic Marczewski-Steinhaus distance. The obtained two groups were compared based on the Wilcoxon and Student’s t-test. For all the tests, a statistically significant P value <0.05 was assumed.
The examination protocol was approved by the Bioethical Commission of Medical University of Silesia in Katowice, Poland, decision number KNW/0022/KB215/12.
Results
The study group included 123 males and 107 females. The average age was 60.9±10.5 years. Tumor size was 6.8±4.1 cm. Eighty-nine patients underwent NSS with mean tumor size of 4.16 cm, and 141 patients underwent radical nephrectomy with mean tumor size of 7.9 cm. Local recurrence during follow-up occurred in 25 patients (10.8%) and distant metastases were found in 22 patients (9.5%). Tumor-specific death was reported in 6 cases after NSS (2.6%) and in 43 cases (18.6%) after radical nephrectomy. In 7 patients with local recurrence (5 after nephrectomy and 2 after NSS) surgical removal of local recurrence was performed; despite this, in these patients, progression of the disease was observed. There was an almost identical distribution of neoplastic changes, taking into account the operated side, with 113 right kidneys and 117 left kidneys. We also evaluated the anatomical location of the tumor. The most frequently observed tumors were located on the dorsal side, followed by the lower pole and the upper pole. In the central part of the kidney, 7 tumors were detected. The lowest clinical stage T1 was observed in 112 patients (T1a in 48 patients, T1b in 64 patients), T2 in 60 patients (T2a in 33 patients, T2b in 27 patients), T3 in 54 patients (T3a in 50 patients, T3b in 4 patients) and the most advanced type of cancer, T4 was found in 4 patients.
The statistically significant results obtained in univariate analysis are presented in Table 1.
Table 1.
Monodimensional logistic regression: all statistically significant parameters predictive of metastasis, recurrence, and death specific for kidney cancer within five-years of observation.
| AE | AP | OR | CI 95% | P-value | |
|---|---|---|---|---|---|
| Metastasis | Tumor location | – C | 1.00 | Refer. | |
| – L | 0.07 | (0.012; 0.426) | 0.0039 | ||
| – U | 0.062 | (0.009; 0.408) | 0.0039 | ||
| – D | 0.128 | (0.025; 0.644) | 0.0127 | ||
| T | 1.7 | (1.26; 2.28) | <0.001 | ||
| PLT [thous/μL] | 1.005 | (1.001; 1.009) | 0.024 | ||
| Na [mmol/L] | 0.88 | (0.81; 0.95) | 0.002 | ||
| Recurrence | Tumor size | 1.11 | (1.03; 1.19) | 0.012 | |
| G | 3.3 | (1.43; 7.63) | 0.006 | ||
| T | 1.57 | (1.2; 2.05) | <0.001 | ||
| N | 4.74 | (1.66; 13.51) | 0.008 | ||
| HGB [g/dL] | 0.66 | (0.53; 0.83) | <0.001 | ||
| HCT [%] | 0.88 | (0.79; 0.99) | 0.035 | ||
| MCV [fL] | 0.88 | (0.83; 0.94) | <0.001 | ||
| MCH [pg] | 0.82 | (0.71; 0.94) | 0.007 | ||
| PLT [thous/μL] | 1.01 | (1.01; 1.02) | <0.001 | ||
| Na [mmol/L] | 0.83 | (0.77; 0.9) | <0.001 | ||
| Death | NSS/NF | 3.99 | (1.63; 9.77) | <0.001 | |
| Tumor size | 1.16 | (1.08; 1.25) | <0.001 | ||
| G | 3.29 | (1.72; 6.3) | <0.001 | ||
| T | 1.85 | (1.48; 2.31) | <0.001 | ||
| N | 11.2 | (4.38; 28.64) | <0.001 | ||
| M | 12.46 | (3.73; 41.65) | <0.001 | ||
| CREA [μmol/L] | 1.01 | (1; 1.02) | 0.018 | ||
| HGB [g/dL] | 0.68 | (0.57; 0.82) | <0.001 | ||
| HCT [%] | 0.89 | (0.81; 0.97) | 0.006 | ||
| MCV [fL] | 0.88 | (0.84; 0.93) | <0.001 | ||
| MCHC [g/dL] | 0.83 | (0.72; 0.96) | 0.014 | ||
| MCH [pg] | 0.8 | (0.71; 0.9) | <0.001 | ||
| RDW [%] | 1.19 | (1.03; 1.37) | 0.019 | ||
| PLT [thous/μL] | 1.01 | (1.01; 1.02) | <0.001 | ||
| MPV [fL] | 0.64 | (0.52; 0.8) | <0.001 | ||
| Na [mmol/L] | 0.78 | (0.72; 0.85) | <0.001 | ||
LR – logistic regression; AE – adverse event; AP – analyzed parameters; OR – odds ratio; CI – confidence interval; Location C – a central location of the tumor; Location l – tumor in the lower pole of the kidney; Location U – a tumor in the upper pole of the kidney; Location D – a tumor in the dorsal part of the kidney; T – tumor scale; G – Fuhrman scale; PLT – platelets count; HGB – hemoglobin level; HCT – hematocrit; MCV – mean corpuscular volume; MCHC – mean corpuscular hemoglobin concentration; MCH – mean corpuscular hemoglobin; RDW – red blood cell distribution width; MPV – mean platelet volume; NSS – nephron-sparing surgery; NF – nephrectomy; Na – preoperative sodium concentration; M – metastases; CREA – preoperative creatinine concentration.
In terms of a single interaction of risk factors, we can say that the location of the tumor had a strong statistical relationship with the occurrence of metastasis. In reference to “the C” location (centrally located tumors), all other positions (i.e., the “L”, lower pole, the “U”, upper pole, and the “D”, dorsal) there was a significant decrease in the chance of metastasis of cancer to almost minimum. This is probably related to a better penetration of tumor cells into the lumen of the small vessels. While interpreting this last result, a relatively small number of patients in the reference group must be considered and therefore its accuracy should be assessed carefully. The given result may be more helpful in identifying trends in the risk of metastasis. The obtained results indicated that with increased grading of the tumor (T) the risk of metastasis increases; in patients differing in one level of sophistication, e.g., T1a relative to T1b, differs in approximately 70%, and cancer specific mortality 85%. When the platelet count (PLT) was increase by 10 thousand/μL, the risk of metastasis was higher by (1.00510–1)*100%=5%, and the recurrence and death by 10%. Furthermore, the increase of sodium level in serum of 2 units resulted in a statistical decrease in the risk of metastasis by about (1–0.882)*100%=23%, the risk of local recurrence by 31%, and specific mortality by 39%. On the basis of these results, it should also be noted that with increasing levels of hemoglobin, hematocrit, mean red blood cell volume, the average weight of hemoglobin by 2 units, the risk of local recurrence drops respectively for individual factors by: 56%, 22%, 22% and 32%. The same increase in the aforementioned parameters resulted in a decrease in the risk of cancer specific mortality by 53%, 20%, 22%, and 36%, respectively. More than 3 times higher risk of local recurrence and 10 of specific mortality for patients with the presence of cancer cells in the regional lymph nodes. Death due to kidney cancer occurred more than 11 times more often in patients with known distant metastases at the time of diagnosis.
Feedback (interplay) of investigated risk factors occurs in the case of multivariate logistic regression. The results of this analysis are presented in Table 2. No interaction was observed in the range of examined characteristics in the case of metastasis. This analysis showed that the analyzed individual morphology parameters (except PLT) were not as important as biochemical parameters or data on the tumor itself.
Table 2.
Multivariate logistic regression: statistically significant risk factors for recurrence and death, tumor specific.
| LR | AE | AP | OR | CI 95% | P-value |
|---|---|---|---|---|---|
| Multivariate | Metastasis | Not found | |||
| Recurrence | T | 1.37 | (1.02; 1.83) | 0.035 | |
| PLT [thous/μL] | 1.0079 | (1.0029; 1.013) | 0.001 | ||
| Na [mmol/L] | 0.9 | (0.82; 0.99) | 0.032 | ||
| Death | T | 1.5 | (1.09; 2.06) | 0.01 | |
| M | 16.05 | (3.37; 76.33) | <0.001 | ||
| CREA [μmol/L] | 1.02 | (1.00; 1.04) | 0.03 | ||
| PLT [thous/μL] | 1.01 | (1.01; 1.02) | <0.001 |
LR – logistic regression; AE – adverse event; AP – analyzed parameters; OR – odds ratio; CI – confidence interval; T – tumor scale; PLT – platelets count; Na – preoperative sodium concentration; M – metastases; CREA – preoperative creatinine concentration.
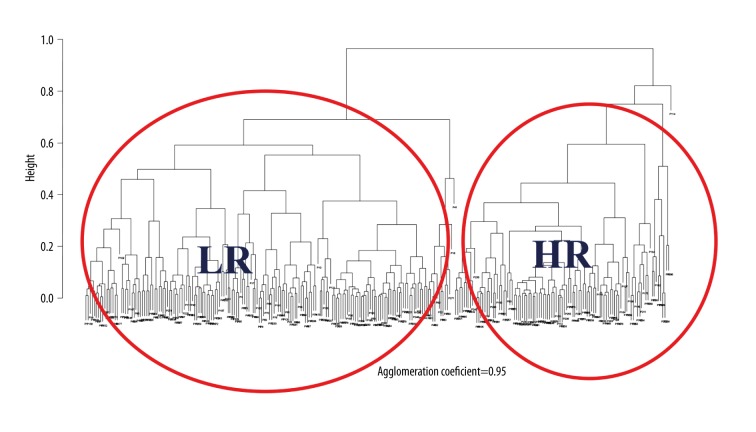
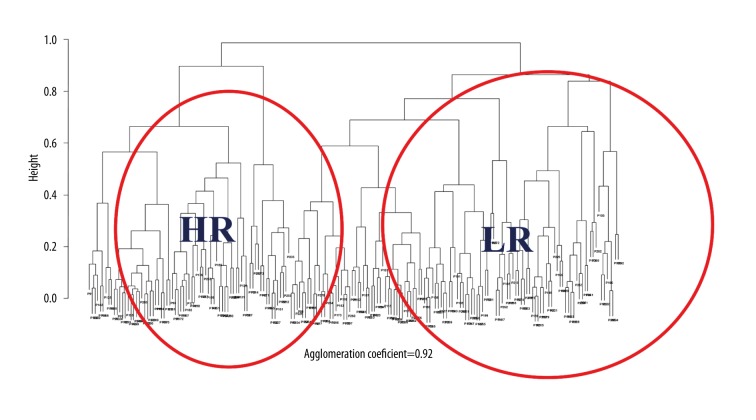
A multidimensional classification of patients performed on the basis of the detected in multivariate logistic regression features coexisting with recurrence and death allowed us to single out the “families” of the patients on the basis of the analyzed risk factors. Figures 1 and 2 represent suitable recurrence and death correlation characteristics classification dendrograms.
Figure 1.
Patients taxonomic dendrogram based on the tumor stage, the number of platelets, and the serum sodium concentration (LR – low risk; HR – high risk).
Figure 2.
Patients taxonomic dendrogram based on clinical stage of cancer, metastases, serum creatinine before treatment, and platelet counts (LR – low risk; HR – high risk).
Two main types of patients were distinguished for the characteristics interdependent with recurrence and with death. The results of the statistical analysis based on the Wilcoxon test and the Student’s t-test (for the median and average), belonging to the thus determined types of patients are presented (after prior identification) in Table 3.
Table 3.
Multidimensional classification of patients into low risk and high risk of recurrence and death due to specific RCC.
| AE | AP | Stat. test | P-value | LR | HR |
|---|---|---|---|---|---|
| Recurrence | T | W=333 | <0.0001 | 1b | 3a |
| PLT [thous/μL] | t=−4.2539 | <0.0001 | 231.5 | 278.9 | |
| Na [mmol/L] | t=4.6661 | <0.0001 | 143.4 | 140.6 | |
| OR | W=7694 | <0.0001 | 2.8% | 19.2% | |
| Death | T | W=7691 | <0.0001 | 2a | 3a |
| M | W=5236 | <0.0001 | 0.0% | 20.5% | |
| CREA [μmol/L] | t=−4.2098 | <0.0001 | 85.6 | 97.9 | |
| PLT [thous/μL] | t=5.4487 | <0.0001 | 227.0 | 299.5 | |
| OR | W=5654 | <0.0001 | 10.9% | 41.1% |
AE – adverse event; AP – analyzed parameters; OR – odds ratio; T – tumor scale; PLT – platelets count; Na – preoperative sodium concentration; LR – low risk; HR – high risk; CREA – preoperative creatinine concentration.
The results of Wilcoxon and T-Student statistical tests shown in Table 3 demonstrate the significance of differences between median and average groups of patients for all risk factors correlative with recurrence and deaths. In the case of the characteristics coexisting with recurrence in patients, typically two groups occur predominantly in these cancer patients. They are characterized as follows: for severity of the disease (according to the TNM scale), relatively low risk was T1b and high risk was T3a; for PLT, relatively lower risk was about 230 units, and relatively high risk was about 280 units; for sodium concentration, relatively high risk with an average of 143.4 units and lower risk about 140.6 units.
There was a statistically significant difference in both groups in the fraction of patients who develop recurrence; group 1 (low risk) was characterized by a minimum number of patients with recurrence within 5-years of follow-up, which was 2.8%, while in the case of patients in group 2 (high risk), such events were recorded 19.2%.
A similar conclusion was made for the coexistence of death characteristics, obtaining two groups of patients differing statistically with regards to tumor-specific death in the postoperative follow-up period. The first group (low risk), the percentage of deaths was 10.9%, characterized by the following parameters: T2a, the absence of metastases, preoperative creatinine level of 85.6 μmol/L and the value of PLT of 227.0×103. The second group (high risk) where the tumor-specific death occurred in 41.4% of patients characterized by: T3a, the presence of metastases in the lungs (M), serum creatinine before treatment level of 97.9 μmol/L, and the value of PLT of 299.5×103.
Discussion
Erythropoietin (EPO) is the principal regulator of erythropoiesis in the tissues involved in the production of erythrocytes. In other tissues, especially in tumor cells, it inhibits apoptosis, promotes angiogenesis, and promotes cell proliferation. Many studies have confirmed the over-expression of EPO and its receptor (EPOR) in clear cell renal carcinoma. Predictive value of this remains still an unsolved problem [6–8].
It seems that in patients with renal cell carcinoma polycythemia this should be observed. As practice shows, this is not happening. Despite the increased expression of EPO and EPOR, up to 35% of patients with RCC develop anemia and only 1% to 5% develop paraneoplastic polycythemia. Weak activity of EPO produced by the tumor, and the low sensitivity to this factor of the tissues involved in the production of blood is the main explanation. An important role may also be played by low level and abnormal iron metabolism. Increase in inflammatory agents and antibodies that occurs during neoplasia may contribute to hemolysis by autoimmunity. This study demonstrated that lowering the values of the blood cell parameters below a specified cutoff point, except anisocytosis, resulted in increased risk of tumor-specific death during the 5-year follow-up period. Reduced value of preoperative hemoglobin, hematocrit; mean corpuscular volume, and mean corpuscular hemoglobin also predisposed patients to early recurrence of cancer.
Thrombocytosis in renal cell carcinoma is likely to be associated with the endocrine activity of tumor cells. Production of many types of cytokines, including IL-6, IL-11, thrombopoietin, granulocyte macrophage colony stimulating factor (GM-CSF) results in an increased production of thrombocytes. IL-6 plays a role by stimulating the maturation of megakaryocytes that stimulates platelet production [9]. The platelets may also affect tumor growth by producing growth factors such as VEGF, PDGF, hepatocyte growth factor, thrombospondin, or endostatins [10,11].
Karakiewicz et al. revealed in single and multivariable analyses that preoperative anemia and thrombocytosis correlate with the increase of cancer specific mortality. The predictive value of these parameters (0.3%) was, however, lower than the factors associated with the tumor parameters or patient ECOG scale [12].
Our analyses showed that the increase in PLT was a negative prognostic factor in patients undergoing surgery for renal cell carcinoma. Statistical significance was confirmed in single and multidimensional analyses. In addition, the predictive value of the volume of platelets was confirmed to have statistical significance.
In many cases, patients with renal tumors develop a decrease in glomerular filtration rate. This is due to renal parenchyma damage caused by the expanding tumor mass. Prognostic value in estimated glomerular filtration rate decline (eGFR) associated with tumor size was also reported by Donin et al. [13].
A small number of publications have confirmed the predictive value of preoperative serum sodium levels in patients with kidney cancer. Single and multidimensional analysis confirm that the concentration of sodium <136 mmol/L correlates with short-term survival, as well as low response to immunomodulatory therapy of patients with renal cell carcinoma [14,15]. Our study confirmed by single and multidimensional analyzes that preoperative hyponatremia was an unfavorable prognostic factor in the treatment of renal cell carcinoma.
The cause of hyponatremia in patients with renal cell carcinoma is not fully understood. Paraneoplastic syndromes that manifest hyponatremia have been described most often in relation to small-cell lung cancer and are associated with worse prognosis. Similar symptoms can also occur in prostate cancer, cancers of the gastrointestinal tract, carcinoid tumors, lymphomas, and thymomas. Hyponatremia described in those cases is caused by an inadequate secretion of the antidiuretic hormone (SIADH syndrome). So far there is no proof of anomalies in the secretion of vasopressin in patients with renal cell carcinoma, but this hypothesis needs further investigation. A more likely cause of hyponatremia in advanced kidney cancer is substantial damage to the exchange mechanisms in the renal tubules by the burgeoning mass of the tumor.
The control of sodium is performed mainly in the distal tubules and collecting ducts of the nephron, where the capacity to reabsorb sodium is regulated by the renin-angiotensin-aldosterone system. It is known that serum sodium is a prognostic marker in patients with small cell lung cancer [16], where the cause of hyponatremia is inappropriate anti-diuretic hormone secretion. It is supposed that same situation is in patients with renal cell carcinoma, and one alternative possibility is that renal tumors may be inducing a subtle disturbance of the renin-angiotensin-aldosterone axis.
It should be emphasized that previous studies looking for new, easily accessible classifiers do not constitute a breakthrough and only improve the value of factors associated with the anatomy and severity of the tumor. It is estimated that the blood count and biochemical parameters can be independent prognostic factors for kidney cancer, but they do not exceed the quality of TNM classification. All the evaluated morphological and biochemical parameters of blood are characterized by low reproducibility and are dependent on many factors exobiotic and endobiotic, which is also worth mentioning. Nevertheless, we were able to identify a group of laboratory parameters which can be applied to forecast of patients with renal cell carcinoma treatment.
Further studies, preferably prospective, with larger numbers of patients are needed to validate the obtained results.
Conclusions
In conclusion, preoperative PLT, serum sodium levels, and tumor staging were found to be independent risk factors for local recurrence. Blood PLT, serum sodium level, creatinine level, and tumor staging may be useful for estimating 5-year cancer specific survival. The prognostic value of studied parameters in defining the risk of metastasis was not confirmed in this study; however, low-risk and high-risk groups for local recurrence and cancer specific death were identified by preoperative laboratory parameters analysis.
Footnotes
Source of support: Self financing
References
- 1.Zastrow S, Brookman-May S, Cong TA, et al. Decision curve analysis and external validation of the postoperative Karakiewicz nomogram for renal cell carcinoma based on a large single-center study cohort. World J Urol. 2015;33(3):381–88. doi: 10.1007/s00345-014-1321-6. [DOI] [PubMed] [Google Scholar]
- 2.Lee BH, Feifer A, Feuerstein MA, et al. Validation of a postoperative nomogram predicting recurrence in patients with conventional clear cell renal cell carcinoma. Eur Urol Focus. :2016. doi: 10.1016/j.euf.2016.07.006. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abel EJ, Masterson TA, Karam JA, et al. Predictive nomogram for recurrence following surgery for nonmetastatic renal cell cancer with tumor thrombus. J Urol. 2017;198(4):810–16. doi: 10.1016/j.juro.2017.04.066. [DOI] [PubMed] [Google Scholar]
- 4.Gu L, Wang Z, Chen L, et al. A proposal of post-operative nomogram for overall survival in patients with renal cell carcinoma and venous tumor thrombus. J Surg Oncol. 2017;115(7):905–12. doi: 10.1002/jso.24575. [DOI] [PubMed] [Google Scholar]
- 5.Abel EJ, Margulis V, Bauman TM, et al. Risk factors for recurrence after surgery in non-metastatic RCC with thrombus: A contemporary multicentre analysis. BJU Int. 2016;117(6B):E87–94. doi: 10.1111/bju.13268. [DOI] [PubMed] [Google Scholar]
- 6.Morais C, Johnson DW, Vesey DA, Gobe GC. Functional significance of erythropoietin in renal cell carcinoma. BMC Cancer. 2013;13:14. doi: 10.1186/1471-2407-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu P, Zhang N, Wang X, et al. The erythropoietin/erythropoietin receptor signaling pathway promotes growth and invasion abilities in human renal carcinoma cells. PLoS One. 2012;7(9):e45122. doi: 10.1371/journal.pone.0045122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minami T, Minami T, Shimizu N, et al. Identification of erythropoietin receptor-derived peptides having the potential to induce cancer-reactive cytotoxic T lymphocytes from HLA-A24(+) patients with renal cell carcinoma. Int Immunopharmacol. 2014;20(1):59–65. doi: 10.1016/j.intimp.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 9.Stone RL, Nick AM, McNeish IA, et al. Paraneoplastic thrombocytosis in ovarian cancer. N Engl J Med. 2012;366(7):610–18. doi: 10.1056/NEJMoa1110352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barata PC, Rini BI. Treatment of renal cell carcinoma: Current status and future directions. Cancer J Clin. 2017;67(6):507–24. doi: 10.3322/caac.21411. [DOI] [PubMed] [Google Scholar]
- 11.Di J, Gao K, Qu D, et al. Rap2B promotes angiogenesis via PI3K/AKT/VEGF signaling pathway in human renal cell carcinoma. Tumour Biol. 2017;39(7):1010428317701653. doi: 10.1177/1010428317701653. [DOI] [PubMed] [Google Scholar]
- 12.Karakiewicz PI, Trinh QD, Lam JS, et al. Platelet count and preoperative haemoglobin do not significantly increase the performance of established predictors of renal cell carcinoma-specific mortality. Eur Urol. 2007;52(5):1428–36. doi: 10.1016/j.eururo.2007.03.036. [DOI] [PubMed] [Google Scholar]
- 13.Donin NM, Suh LK, Barlow L, et al. Tumour diameter and decreased preoperative estimated glomerular filtration rate are independently correlated in patients with renal cell carcinoma. BJU Int. 2012;109:379–83. doi: 10.1111/j.1464-410X.2011.10331.x. [DOI] [PubMed] [Google Scholar]
- 14.Furukawa J, Miyake H, Kusuda Y, Fujisawa M. Hyponatremia as a powerful prognostic predictor for Japanese patients with clear cell renal cell carcinoma treated with a tyrosine kinase inhibitor. Int J Clin Oncol. 2015;20(2):351–57. doi: 10.1007/s10147-014-0713-3. [DOI] [PubMed] [Google Scholar]
- 15.Schutz FA, Xie W, Donskov F, et al. The impact of low serum sodium on treatment outcome of targeted therapy in metastatic renal cell carcinoma: Results from the International Metastatic Renal Cell Cancer Database Consortium. Eur Urol. 2014;65(4):723–30. doi: 10.1016/j.eururo.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simmonds P. Managing patients with lung cancer. New guidelines should improve standards of care. BMJ. 1999;319:527–28. doi: 10.1136/bmj.319.7209.527. [DOI] [PMC free article] [PubMed] [Google Scholar]