Abstract
Car use has been identified as sedentary behavior, although it may enhance mobility, particularly in the older population. This cross-sectional study aimed to compare the time spent in objectively determined sedentary behavior (SB) and physical activity (PA) between older drivers and non-drivers. Four hundred and fifty Japanese older adults (74.3 ± 2.9 years) who had valid accelerometer data were included. They were asked to respond to a questionnaire and wear an accelerometer (HJA-350IT, Omron Healthcare) on their waist for 7 consecutive days in 2015. To compare activity time between drivers and non-drivers, we calculated estimated means using analysis of covariance, adjusting for sociodemographic, physical, and psychological factors and accelerometer wear time. Compared to non-drivers, drivers engaged in more light-intensity PA (LPA) (drivers: 325.0 vs. non-drivers: 289.0 min/day) and moderate-to-vigorous PA (drivers: 37.5 vs. non-drivers: 30.0 min/day) and less SB (drivers: 493.4 vs. non-drivers: 535.9 min/day) (all p < 0.05). After stratification by age, sex, and residential area, larger effect of driving on PA time was found in older-older adults, in men, and in rural residents. Older drivers were found to be more physically active than non-drivers, suggesting more access to outdoor activities or expanding social network.
Keywords: exercise, sedentary lifestyle, accelerometry, aging, mobility, automobiles, epidemiology
1. Introduction
Car use has been identified as sedentary behavior and a health risk in the adult population [1,2,3,4]. Initially, Morris et al. found that sedentary drivers of London’s double-decker buses who remain sedentary for a large amount of the day had higher risks of cardiovascular disease than the bus conductors who engaged in physically active jobs [3]. Recent longitudinal studies have also shown that frequent and longer car use is associated with higher cardiovascular disease mortality in men [5] and greater weight gain in adults [1]. Several interventions to replace car use with active transport have been conducted [6,7].
However, contrary to the adult population, car use may not be a health risk in the older population. One possibility is that car use enables mobility and freedom and enables older adults to be more physically active throughout the entire day. For older adults in Japan and other developed countries, driving is often the most preferred mode of transportation [8,9]. Previous studies have indicated that car ownership and driving are associated with independence and life satisfaction in older adults [10,11,12,13]. Driving cessation is likely to result in fewer out-of-home activities as they replace outside activities with indoor activities [14].
A previous questionnaire survey suggested that older adults with 1 or fewer cars were less likely than those with ≥2 cars to achieve the recommended levels of moderate-to-vigorous physical activity (MVPA) (i.e., 150 min/week MVPA) [15]. On the other hand, another recent study showed that there was no difference in accelerometer determined MVPA time between drivers and non-drivers in older American adults [16]. However, in these studies, driving status was evaluated based on assumption (e.g., car ownership). Therefore, direct assessment of whether these people drive or not is required to accurately compare physical activity (PA) time between drivers and non-drivers.
Recent studies report that older adults spend the majority of time in sedentary behavior (SB) and light-intensity PA (LPA) [17,18,19], which can be associated with mortality [20,21,22,23], cognitive decline [24], and cardiometabolic risk biomarkers [25,26,27]. To date, it remains unclear as to how daily activity patterns including SB and LPA differ between older drivers and non-drivers. Therefore, the purpose of this study was to compare the time spent in objectively measured activity classified by intensity and duration between drivers and non-drives in community-dwelling older adults. Also, we aimed to determine whether the impact of driving on each activity differs according to sociodemographic characteristics.
2. Materials and Methods
2.1. Study Design and Data Collection
Questionnaires were mailed to 1210 community-dwelling older adults aged 70–79 years from February through June 2015. They were originally randomly recruited from resident registries of three municipalities in Japan: Bunkyo city (urban) and Fuchu city (suburban) in Tokyo, and Oyama City (rural) in Shizuoka prefecture, and they responded to a population-based survey conducted in 2010. The details of the sampling process for the 2010 survey and the regional characteristics of each area are presented in a previous study [28]. We sent accelerometers and instructions to participants who agreed to wear an accelerometer. Ethical approval was obtained from the Tokyo Medical University Ethics Committee prior to the survey (No. 2898). Written informed consent was obtained from all participants.
2.2. Questionnaire Data
Date of birth, sex, and residential area were obtained from the residential registry of each municipality in 2010. A residential registry is a local government database including information on all the residents. Living arrangement (with others/alone), working status (working with income/not working), driving status (frequently/rarely/no driver’s license), self-rated health, and self-rated physical limitation were assessed by the questionnaire survey carried out in 2015. Older adults who frequently drive a car were defined as drivers whereas others were defined as non-drivers in this study, as we focused on the frequency of driving rather than the possession of a driver’s license. Body mass index (BMI) (kg/m2) was calculated by self-reported height and weight. Self-rated health was assessed using one question from SF-8 (Japanese version) that asked participants to rate their health. Participants chose the answer that most accurately described their health from a 6-point scale: excellent, very good, good, fair, poor, and very poor, to the question; “Overall, how would you rate your health during the past 4 weeks?” [29]. Self-rated physical limitation was also evaluated using one question from SF-8: not at all, very little, somewhat, quite a lot, could not do physical activities, to the question; “During the past 4 weeks, how much did physical health problems limit your physical activities (such as walking or climbing stairs)?” [29]. The answers were classified into “no” (not at all and very little) and “yes” (somewhat, quite a lot, and could not do physical activities).
2.3. Accelerometry
SB and PA were measured using a tri-axial accelerometer, the Active style Pro HJA-350IT (Omron Healthcare, Kyoto, Japan), which provides data comparable to the devices most commonly used in studies conducted in Western countries [30,31]. Its algorithm and validity have been presented in detail elsewhere [32,33,34]. Previous study reports that activity intensity measured by accelerometers used in this study is relatively accurate in older adults [34]. We obtained 60-s epoch data and calculated metabolic equivalents (METs) values using attached analysis software, BI-LINK PROFESSIONAL EDITION Ver1.0 (Omron Healthcare, Kyoto, Japan). METs-based cutoff was used to define each intensity of activities: ≤1.5 METs for SB, 1.6–2.9 METs for LPA, 3.0–5.9 METs for moderate-intensity PA (MPA), ≥6 METs for vigorous-intensity PA (VPA), and ≥3 METs for MVPA [35,36]. Active style Pro does not detect postural information and hence SB was determined by acceleration.
Participants were asked to wear the accelerometer on their waist for 7 consecutive days while awake, only taking it off for water-based activities (e.g., swimming and showering). No acceleration signal detected for longer than 60 consecutive minutes was defined as “non-wear” [37]. Wear time was calculated by subtracting non-wear time from 1440 min. Records from participants wearing the accelerometer for at least 10 h per day were considered valid [38]. Participants with data from at least 4 days were included in the analysis [37].
2.4. Statistical Analyses
The Chi-squared test or Fisher’s exact test was performed to compare participant characteristics between those who agreed to wear an accelerometer and those who did not. Descriptive analyses of the time spent in SB, LPA, and MVPA were conducted, stratified by driving status (drivers and non-drivers). Total MVPA was further classified into 2 types according to the duration of MVPA-bout: short-bout MVPA (<10 min) and long-bout MVPA (≥10 min). Long-bout MVPA was defined as 10 or more consecutive minutes above the moderate intensity threshold, with allowance for interruptions of 1 or 2 min below the threshold [37]. Regarding SB, a bout was considered as a specific duration of time in continuous sedentary time in which no interruption was allowed. In this study, we examined ≥30 min SB and ≥60 min SB, considering previous research on associations of sedentary bout durations with health outcomes [39,40,41].
As the multivariate analysis, we used the analysis of covariance (ANCOVA) to compare SB and PA classified by intensity and duration between drivers and non-drivers, adjusting for wear time, age, sex, residential area, working status, living arrangement, BMI, self-rated health, and physical limitation. Distributions of MVPA (total MVPA, short-bout MVPA, and long-bout MVPA) and prolonged SB (≥30 min SB and ≥60 min SB) were positively skewed and therefore the log transformation was applied when models were run. Estimated means and their 95% confidence intervals (CI) were then back-transformed for the purposes of reporting. To estimate the effect of size, partial eta squared (ηp2) was calculated after adjustment for covariates. Analyses were conducted first for the overall sample, and then separately for age group (younger-older adults [70–74 years]/older-older adults [75–79 years]), sex (men/women), or residential area (urban/suburban/rural). As sensitive analyses, models were rerun (1) excluding older adults with physical limitation (i.e., those who chose the answer: somewhat, quite a lot, and could not do physical activities, to the question; “During the past 4 weeks, how much did physical health problems limit your physical activities (such as walking or climbing stairs)?”; (2) stratified by “not at all” of physical limitation or the other; and (3) using the original 3 categories (frequently/rarely/no driver’s license) as exposure variable. All statistical analyses were performed using IBM SPSS Statistics version 21 software (IBM Corp., Tokyo, Japan) and R version 3.3.3. for Mac; a p-level of less than 0.05 was considered to indicate a statistically significant difference between groups.
3. Results
3.1. Participant Characteristics
Of the 1210 people surveyed, 988 older adults returned the questionnaire (response rate: 81.7%), and 478 of those agreed to wear the accelerometer. However, 28 were excluded owing to the following reason: not meeting the wearing time criteria (i.e., wearing at least four days of ≥10 h/day) (n = 7), refusal to wear or failure to return the accelerometer (n = 15), and system error (n = 6). Therefore, a total of 450 older adults (255 men, 56.7%) were included in this study. When participant characteristics were compared between those who agreed to wear an accelerometer and those who did not, significant differences were observed in sex (proportion of agreement; men: 55.6%, women: 47.7%, p = 0.015), self-rated health (proportion of agreement; excellent: 78.3%, very good: 66.0%, good: 59.4%, fair: 60.4%, poor: 50.0%, and very poor: 33.3%, p = 0.038), and physical limitation (proportion of agreement; not at all: 63.2%, very little: 55.1%, somewhat: 65.5%, quite a lot:54.2%, could not do physical actives: 17.6%, p = 0.001). No significant differences were found in driving status (proportion of agreement; drivers: 55.2%, non-drivers: 50.6%, p = 0.174).
The mean age of the participants was 74.3 ± 2.9 years. Fewer than half of the participants were drivers (n = 209, 46.4%), and most of the study population was living with others and had good self-rated health (Table 1). Most of the older adults categorized as non-drivers did not have driver license (n = 172, 71.4%).
Table 1.
Participant characteristics.
| Variables | Drivers (n = 209) | Non-Drivers (n = 241) | |
|---|---|---|---|
| n (%) | n (%) | p-Value | |
| Sex | <0.001 a | ||
| Men | 160 (76.6) | 95 (39.4) | |
| Women | 49 (23.4) | 146 (60.6) | |
| Age | 0.999 a | ||
| 70–74 years | 109 (52.2) | 125 (51.9) | |
| 75–79 years | 100 (47.8) | 116 (48.1) | |
| Residential area | <0.001 a | ||
| Urban | 28 (13.4) | 114 (47.3) | |
| Suburban | 59 (28.2) | 83 (34.4) | |
| Rural | 122 (58.4) | 44 (18.3) | |
| Living arrangement | 0.006 a | ||
| With others | 189 (38.3) | 197 (21.3) | |
| Alone | 19 (61.7) | 44 (78.7) | |
| (missing n = 1) | |||
| Working with income | <0.001 a | ||
| Working | 80 (90.9) | 51 (81.7) | |
| Not working | 129 (9.1) | 188 (18.3) | |
| (missing n = 2) | |||
| Body mass index (BMI) | 0.140 a | ||
| <25.0 kg/m2 | 165 (78.9) | 204 (84.6) | |
| ≥25.0 kg/m2 | 44 (21.1) | 37 (15.4) | |
| Self-rated health | 0.046 b | ||
| Excellent | 9 (4.3) | 8 (3.3) | |
| Very good | 50 (24.0) | 49 (20.5) | |
| Good | 121 (58.2) | 126 (52.7) | |
| Fair | 26 (12.5) | 42 (17.6) | |
| Poor | 2 (1.0) | 11 (4.6) | |
| Very poor | 0 (0.0) | 3 (1.3) | |
| (missing n = 3) | |||
| Self-rated physical limitation | 0.206 b | ||
| Not at all | 127 (61.1) | 125 (53.0) | |
| Very little | 41 (19.7) | 55 (23.3) | |
| Somewhat | 35 (16.8) | 42 (17.8) | |
| Quite a lot | 5 (2.4) | 11 (4.7) | |
| Could not do physical activities | 0 (0.0) | 3 (1.3) | |
| (missing n = 6) | |||
| Moderate to vigorous physical activity | 0.594 a | ||
| <150 min/week (not meeting guidelines) | 150 (71.8) | 179 (74.3) | |
| ≥150 min/week (meeting guidelines) | 59 (28.2) | 62 (25.7) |
p-values were calculated by the Chi-squared test a or Fisher’s exact test b bold indicates statistical significance (p < 0.05).
3.2. Descriptive Data of Accelerometers
Time spent in objectively measured SB and PA in older drivers and non-drivers is presented in Table 2. Mean accelerometer wear time was 865.9 min/day in drivers and 880.8 min/day in non-drivers. Most of the wear time was spent in SB (57.9% in drivers, 61.4% in non-drivers), whereas the median time spent in MVPA was no more than 5% (5.0% in drivers, 4.1% in non-drivers).
Table 2.
Unadjusted data of objectively measured activity time (min/day) in older drivers and non-drivers.
| Variables | Drivers (n = 209) | Non-Drivers (n = 241) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Median | (25%, 75%) | Mean ± SD | Median | (25%, 75%) | |
| Wear time | 865.9 ± 86.8 | 875.6 | (806.3, 923.1) | 880.8 ± 93.1 | 876.1 | (819.3, 941.8) |
| SB | 501.5 ± 118.1 | 508.1 | (416.4, 580.3) | 539.3 ± 118.1 | 530.4 | (449.6, 608.8) |
| LPA | 315.0 ± 96.8 | 303.3 | (244.0, 374.2) | 300.7 ± 106.1 | 302.5 | (222.4, 371.5) |
| Total MVPA | 49.4 ± 33.0 | 42.6 | (23.4, 65.7) | 40.7 ± 29.2 | 34.8 | (19.0, 59.0) |
| Short-bout MVPA | 33.0 ± 22.1 | 27.6 | (16.8, 43.3) | 25.8 ± 17.9 | 21.9 | (12.7, 33.2) |
| Long-bout MVPA | 16.4 ± 20.4 | 9.1 | (2.0, 22.9) | 14.9 ± 18.2 | 7.8 | (1.2, 21.7) |
Abbreviations; SB: sedentary behavior, LPA: light-intensity physical activity, MVPA: moderate-to-vigorous physical activity. Short-bout: lasting <10 min, long-bout: lasting ≥10 min.
3.3. Results of Analysis of Covariance
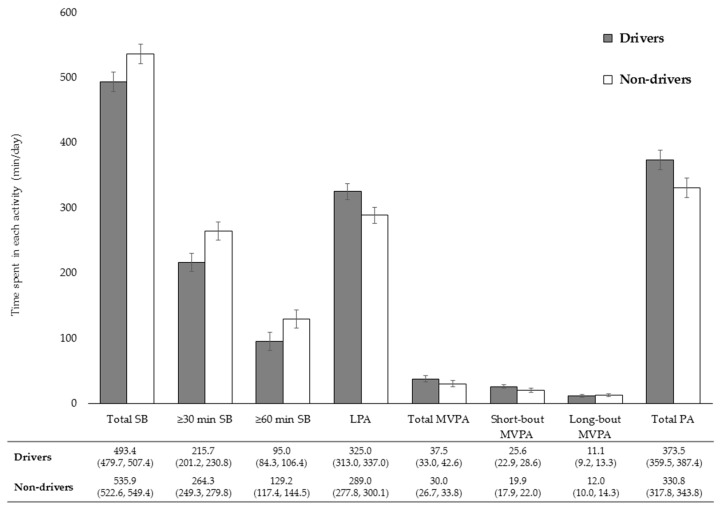
Comparisons of objectively measured SB and PA between drivers and non-drivers after adjustment for covariates are shown in Figure 1. Relative to non-drivers, drivers engaged in 42.7 min more total PA (i.e., LPA + MVPA) (p < 0.001) and 42.5 min less SB (p < 0.001) on account of 36.0 min more LPA (p < 0.001) and 7.5 min more total MVPA (p = 0.024). This difference in total MVPA time was mainly a result of not long-bout MVPA (p = 0.581) but short-bout MVPA (p = 0.003). Drivers engaged in 48.6 min less ≥30 min SB (p = 0.001) and less 34.2 min ≥60 min SB (p < 0.001).
Figure 1.
Comparisons of objectively measured sedentary and physical activity time between older drivers and non-drivers. Abbreviations; SB: sedentary behavior, LPA: light-intensity physical activity, MVPA: moderate-to-vigorous physical activity. Short-bout: lasting <10 min, long-bout: lasting ≥10 min. Estimated mean was adjusted for accelerometer wear time, age, gender, residential area, working status, living arrangement, body mass index, self-rated health, and physical limitation. Bars represent 95% CI of the mean. Values below the x-axis are adjusted means (95% CI).
In sensitivity analyses excluding those with physical limitation, the results are much the same. Differences in SB, ≥30 min SB, ≥60 min SB, LPA, short-bout MVPA, and total PA time between drivers and non-drivers were remained statistically significant, whereas differences in total MVPA time between them were no longer significant. For older adults who chose the answer “not at all” of physical limitation, the differences of each activity time between drivers and non-drivers were not statistically significant (Tables S3 and S4). The effect size of driving on SB and PA was larger in those with any physical limitation compared to those without physical limitation.
In sensitivity analyses using the original driving status categories (frequently/rarely/no driver’s license) as exposure variable, the results did not change (Tables S3 and S4). Older adults who drive a car frequently had the highest level of PA.
Results of stratified analyses of SB and PA are shown in Table 3 and Table 4, respectively. Drivers engaged in less prolonged SB as well as total SB than non-drivers in older-older adults (total SB: 50.9 min, p = 0.002; ≥30 min SB: 48.0 min, p = 0.010; ≥60 min SB: 36.7 min, p = 0.004) and rural residents (total SB: 56.2 min, p = 0.002; ≥30 min SB: 43.9 min, p = 0.028; ≥60 min SB: 32.0 min, p = 0.019). In terms of PA, there were no significant differences in long-bout MVPA between drivers and non-drivers at any groups (younger-older adults: p = 0.976, older-older adults: p = 0.659, men: p = 0.443, women: p = 0.828, urban residents: p = 0.385, suburban residents: p = 0.781, rural resident: p = 0.689). On the other hand, drivers accumulated more short-bout MVPA than non-drivers in older-older adults (8.4 min, p = 0.004), women (9.7 min, p = 0.022), suburban residents (6.9 min, p = 0.010), and rural residents (10.4 min, p = 0.005). Except for women (p = 0.134), drivers engaged in more LPA in all groups (younger-older adults: 27.8 min, p = 0.023; older-older adults: 43.2 min, p = 0.003; men: 42.8, p < 0.001; urban residents: 39.2 min, p = 0.033; suburban residents: 29.9 min, p = 0.045, rural resident: 41.3 min, p = 0.007). Consequently, drivers spent longer time engaging in total PA time than non-drivers in all groups, (younger-older adults: 33.4 min, p = 0.023; older-older adults: 50.9 min, p = 0.002; men: 45.5, p = 0.001; suburban residents: 35.2 min, p = 0.037, rural resident: 56.3 min, p = 0.002) although no statistically significant differences were found between drivers and non-drivers in women (p = 0.050) and in urban residents (p = 0.065). The effect size of driving on SB and PA was larger in older-older adults, men, and rural residents, compared to in younger-older adults, women, and urban and suburban residents, respectively.
Table 3.
Comparisons of objectively measured sedentary time (min/day) between older drivers and non-drivers by sociodemographic characteristics.
| Independent Variables | Total SB | ≥30 min SB | ≥60 min SB | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | |
| Stratified by age group a | ||||||||||||
| Younger-older adults (70–74 years) | 0.023 | 0.023 | 0.020 | 0.034 | 0.012 | 0.113 | ||||||
| Drivers | 507.4 | (488.4, 526.5) | 216.8 | (198.6, 236.6) | 94.8 | (82.0, 109.6) | ||||||
| Non-drivers | 540.8 | (523.2, 558.4) | 250.0 | (230.7, 271.0) | 113.0 | (99.1, 129.1) | ||||||
| Older-older adults (75–79 years) | 0.048 | 0.002 | 0.033 | 0.010 | 0.043 | 0.004 | ||||||
| Drivers | 493.2 | (472.3, 514.2) | 194.1 | (173.8, 216.8) | 80.5 | (68.4, 95.1) | ||||||
| Non-drivers | 544.1 | (524.5, 563.8) | 242.1 | (217.8, 268.5) | 117.2 | (100.0, 137.1) | ||||||
| Stratified by sex b | ||||||||||||
| Men | 0.049 | 0.001 | 0.052 | <0.001 | 0.049 | 0.001 | ||||||
| Drivers | 532.0 | (517.8, 546.3) | 233.9 | (217.8, 250.6) | 98.6 | (87.9, 110.7) | ||||||
| Non-drivers | 577.5 | (558.3, 596.7) | 293.8 | (267.9, 322.8) | 141.9 | (121.6, 165.6) | ||||||
| Women | 0.022 | 0.050 | 0.007 | 0.272 | 0.004 | 0.392 | ||||||
| Drivers | 459.9 | (429.2, 490.7) | 178.2 | (152.4, 208.9) | 79.6 | (63.0, 100.5) | ||||||
| Non-drivers | 497.3 | (480.6, 513.9) | 198.6 | (182.4, 215.8) | 90.2 | (79.3, 102.3) | ||||||
| Stratified by residential area c | ||||||||||||
| Urban | 0.027 | 0.065 | 0.028 | 0.059 | 0.032 | 0.049 | ||||||
| Drivers | 528.2 | (491.9, 564.4) | 211.8 | (177.8, 252.3) | 80.5 | (58.6, 110.7) | ||||||
| Non-drivers | 567.4 | (550.2, 584.5) | 257.0 | (236.6, 279.9) | 116.1 | (100.0, 134.9) | ||||||
| Suburban | 0.033 | 0.037 | 0.025 | 0.073 | 0.014 | 0.180 | ||||||
| Drivers | 523.1 | (499.2, 547.0) | 221.8 | (198.2, 248.9) | 97.7 | (82.0, 116.4) | ||||||
| Non-drivers | 558.3 | (538.6, 578.0) | 256.4 | (233.3, 281.8) | 115.3 | (99.8, 133.0) | ||||||
| Rural | 0.058 | 0.002 | 0.031 | 0.028 | 0.035 | 0.019 | ||||||
| Drivers | 460.0 | (442.8, 477.2) | 188.4 | (172.2, 206.1) | 83.6 | (73.5, 95.1) | ||||||
| Non-drivers | 516.2 | (486.2, 546.3) | 232.3 | (198.6, 272.3) | 115.6 | (92.3, 145.2) | ||||||
a Adjusted for wear time, age, sex, residential area, working status, living arrangement, body mass index, self-rated health, and physical limitation; b Adjusted for wear time, age, residential area, working status, living arrangement, body mass index, self-rated health, and physical limitation; c Adjusted for wear time, age, sex, working status, living arrangement, body mass index, self-rated health, and physical limitation; Abbreviations; SB: sedentary behavior, EM: estimated mean, CI: confidence interval. Bold indicates statistical significance (p < 0.05).
Table 4.
Comparisons of objectively measured physical activity time (min/day) between older drivers and non-drivers by sociodemographic characteristics.
| Independent Variables | LPA | Total MVPA | Short-bout MVPA | Long-bout MVPA | Total PA (LPA + MVPA) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | EM | (95% CI) | ηp2 | p-Value | |
| Stratified by age group a | ||||||||||||||||||||
| Younger-older adults (70–74 years) | 0.023 | 0.023 | 0.003 | 0.397 | 0.006 | 0.271 | 0.000 | 0.976 | 0.023 | 0.023 | ||||||||||
| Drivers | 318.1 | (302.2, 334.0) | 36.3 | (30.3, 43.5) | 24.3 | (20.8, 28.3) | 12.3 | (9.4, 16.1) | 367.1 | (348.0, 386.1) | ||||||||||
| Non-drivers | 290.3 | (275.7, 305.0) | 32.3 | (27.4, 38.1) | 21.3 | (18.5, 24.5) | 12.2 | (9.4, 16.0) | 333.7 | (316.1, 351.3) | ||||||||||
| Older-older adults (75–79 years) | 0.045 | 0.003 | 0.025 | 0.026 | 0.042 | 0.004 | 0.001 | 0.659 | 0.048 | 0.002 | ||||||||||
| Drivers | 331.6 | (313.1, 350.1) | 38.3 | (31.9, 45.9) | 26.9 | (22.8, 31.8) | 10.3 | (8.0, 13.3) | 379.4 | (358.4, 400.4) | ||||||||||
| Non-drivers | 288.4 | (271.0, 305.8) | 28.0 | (23.6, 33.2) | 18.5 | (15.8, 21.6) | 11.3 | (8.8, 14.4) | 328.5 | (308.8, 348.2) | ||||||||||
| Stratified by sex b | ||||||||||||||||||||
| Men | 0.057 | <0.001 | 0.009 | 0.140 | 0.015 | 0.055 | 0.003 | 0.443 | 0.049 | 0.001 | ||||||||||
| Drivers | 277.9 | (265.5, 290.3) | 34.6 | (30.2, 39.6) | 21.5 | (19.1, 24.2) | 11.6 | (9.5, 14.2) | 322.4 | (308.1, 336.7) | ||||||||||
| Non-drivers | 235.1 | (218.4, 251.8) | 28.8 | (24.0, 34.6) | 17.5 | (14.9, 20.5) | 13.4 | (10.1, 17.7) | 276.9 | (257.8, 296.1) | ||||||||||
| Women | 0.013 | 0.134 | 0.017 | 0.079 | 0.029 | 0.022 | 0.000 | 0.828 | 0.022 | 0.050 | ||||||||||
| Drivers | 382.7 | (356.8, 408.7) | 43.0 | (33.0, 56.0) | 33.6 | (26.5, 42.6) | 11.0 | (7.5, 16.3) | 439.4 | (408.6, 470.1) | ||||||||||
| Non-drivers | 358.7 | (344.6, 372.7) | 32.2 | (27.9, 37.2) | 23.9 | (21.0, 27.2) | 10.4 | (8.5, 12.9) | 402.0 | (385.4, 418.7) | ||||||||||
| Stratified by residential area c | ||||||||||||||||||||
| Urban | 0.036 | 0.033 | 0.001 | 0.777 | 0.000 | 0.939 | 0.008 | 0.385 | 0.027 | 0.065 | ||||||||||
| Drivers | 304.9 | (273.6, 336.2) | 31.3 | (21.8, 44.9) | 19.1 | (13.9, 26.4) | 10.7 | (6.9, 16.6) | 347.1 | (310.9, 383.4) | ||||||||||
| Non-drivers | 265.7 | (250.9, 280.5) | 29.5 | (24.9, 35.0) | 18.9 | (16.2, 21.9) | 13.4 | (10.8, 16.6) | 307.9 | (290.8, 325.1) | ||||||||||
| Suburban | 0.031 | 0.045 | 0.027 | 0.063 | 0.050 | 0.010 | 0.001 | 0.781 | 0.033 | 0.037 | ||||||||||
| Drivers | 308.5 | (287.4, 329.6) | 34.9 | (27.9, 43.7) | 22.9 | (18.8, 27.8) | 11.2 | (7.8, 16.1) | 350.1 | (326.2, 374.0) | ||||||||||
| Non-drivers | 278.6 | (261.1, 296.0) | 26.0 | (21.6, 31.3) | 16.0 | (13.6, 18.7) | 12.1 | (8.9, 16.3) | 314.9 | (295.2, 334.6) | ||||||||||
| Rural | 0.045 | 0.007 | 0.031 | 0.027 | 0.051 | 0.005 | 0.001 | 0.689 | 0.058 | 0.002 | ||||||||||
| Drivers | 356.0 | (341.6, 370.5) | 44.4 | (38.5, 51.2) | 33.3 | (29.4, 37.6) | 10.8 | (8.6, 13.6) | 412.6 | (395.3, 429.8) | ||||||||||
| Non-drivers | 314.7 | (289.5, 339.8) | 31.7 | (24.7, 40.6) | 22.9 | (18.5, 28.4) | 9.8 | (6.5, 14.8) | 356.3 | (326.3, 386.4) | ||||||||||
a Adjusted for wear time, age, sex, residential area, working status, living arrangement, body mass index, self-rated health, and physical limitation; b Adjusted for wear time, age, residential area, working status, living arrangement, body mass index, self-rated health, and physical limitation; c Adjusted for wear time, age, sex, working status, living arrangement, body mass index, self-rated health, and physical limitation; Abbreviations; LPA: light-intensity physical activity, MVPA: moderate-to-vigorous physical activity, PA: physical activity, EM: estimated mean, CI: confidence interval; Short-bout: lasting <10 min, long-bout: lasting ≥10 min. Bold indicates statistical significance (p < 0.05).
4. Discussion
Our data provide new information on regarding the potential effect of driving status on detailed daily activity patterns in Japanese older adults. In summary, we found that older drivers were more physically active than non-drivers regarding total daily PA levels. These findings did not change after stratification by age, gender, and residential area, although no statistically significant differences were found between drivers and non-drivers in women and in urban residents.
The underlying reason older drivers are more active than older non-drivers may be enhanced mobility. Private car use may increase the mobility of older adults and make social inclusion and outside activities less difficult [42]. A previous study suggested that driving cessation was strongly associated with a decline in the amount of out-of-home activities [42]. Social inclusion among older adults, for example, is linked to more MVPA time [43,44] and less sedentary time [43]. In this study, a greater difference in MVPA time between drivers and non-drivers were found in rural residents compared with urban and suburban residents. This is probably because rural residents are more likely to rely on their private car for daily mobility [9].
Considering the accumulated line of evidence on the associations of SB and PA with health benefits [20,21,22,45,46,47,48,49], differences in the time spent in SB and PA between drivers and non-drivers may be significant. In this study, drivers had approximately 42 min shorter SB, 36 min longer LPA, and 8 min longer total MVPA, which were mainly owing to short-bout MVPA. A recent study, for example, showed that a greater PA was associated with lower all-cause mortality risk, estimating that replacing 30 min of SB with LPA reduces mortality risk (after 5 years of follow-up: hazard ratio [HR] = 0.80, 95% CI = 0.75–0.85) in adults age 50–79 years [45]. Another study found that replacing 10 min of SB with the same amount of MPA resulted in a significantly lower odds ratio (OR) for metabolic syndrome prevalence (OR = 0.89, 95% CI = 0.82–0.97), high waist circumference (OR = 0.94, 95% CI = 0.88–0.99), high triglyceride levels (OR = 0.91, 95% CI = 0.83–0.99), and high blood pressure (OR = 0.92, 95% CI = 0.85–0.99) [49]. Given these findings, drivers may be received more health benefits by PA than non-drivers, especially in older-older adults, in men, and in rural residents.
In this study, older drivers are more physically active than older non-drivers. Although it has been considered that car use accelerates sedentary lifestyle, older adults who drive a car for transportation do not always engage in more SB and less PA throughout the entire day. Findings of this study may suggest that policy and intervention which allow older adults to keep driving and mobility are effective to promote PA levels, independence, and health.
This study has several limitations to be considered. First, this is a cross-sectional design and there may be reverse causality. It may be that those people who are more active drive more. Second, physical performance and cognitive function can be an important confounding factors in our analyses. Although we adjusted for self-rated health and physical limitation as potential confounders, residual confounding needs to be considered for interpretation of these results. Third, an accelerometer cannot accurately detect postural information (i.e., sitting and standing) and using MET cut-points to define activity intensities may misclassify activity level for older adults. Besides, some types of activities such as swimming and cycling may be underestimated. Fourth, this study did not analyze driving time and consider the purpose for driving, which may affect a driver’s SB and PA. Fifth, our sample was limited to older adults aged 70–79 years. Further investigation including a wider range of the older population is warranted. Finally, the 3 locations included in the present study may not fully represent all rural, suburban, and urban cities. Although these cities were chosen based on their urbanization levels, it is necessary to consider the generalizability of these findings.
5. Conclusions
This study compared the time spent in objectively assessed SB and PA between drivers and non-drivers of community-dwelling older adults in Japan. Older drivers were found to be more physically active, suggesting more access to outdoor activities or expanding social network. The effect of driving on PA time was larger in older-older adults, men, and rural residents, compared to younger-older adults, women, and urban residents, respectively. Longitudinal studies are needed to verify directionality to make the case for physical activity policy and intervention effectiveness.
Supplementary Materials
The following are available online at http://www.mdpi.com/1660-4601/15/6/1094/s1. Table S1: Comparisons of objectively measured sedentary time (min/day) by driving status (frequently/rarely/no driver’s license). Table S2: Comparisons of objectively measured physical activity time (min/day) by driving status (frequently/rarely/no driver’s license). Table S3: Comparisons of objectively measured sedentary time (min/day) by physical limitation status. Table S4: Comparisons of objectively measured physical activity time (min/day) by physical limitation status.
Author Contributions
S.I. developed the study and all authors collected the data. S.A. conducted the statistical analyses and prepared the manuscript draft. N.F., H.K., T.T., Y.O., K.O., and S.I. interpreted the data, revised the manuscript drafts, and provided critical comments during the process. All authors read and approved the final version of the manuscript.
Funding
This study was founded by a Grant-in-Aid for Scientific Research (20500604 and 16H03249) from the Japan Ministry of Education, Culture, Sports, Science and Technology, MEXT-Supported Program for the Strategic Research Foundation at Private Universities, 2015–2019 from the Ministry of Education, Culture, Sports, Science and Technology (S1511017), and the Uehara Memorial Foundation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Sugiyama T., Ding D., Owen N. Commuting by car: Weight gain among physically active adults. Am. J. Prev. Med. 2013;44:169–173. doi: 10.1016/j.amepre.2012.09.063. [DOI] [PubMed] [Google Scholar]
- 2.Sugiyama T., Wijndaele K., Koohsari M.J., Tanamas S.K., Dunstan D.W., Owen N. Adverse associations of car time with markers of cardio-metabolic risk. Prev. Med. 2016;83:26–30. doi: 10.1016/j.ypmed.2015.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morris J.N., Heady J.A., Raffle P.A.B., Roberts C.G., Parks J.W. Coronary heart-disease and physical activity of work. Lancet. 1958;262:1111–1120. doi: 10.1016/S0140-6736(53)91495-0. [DOI] [PubMed] [Google Scholar]
- 4.Wen L.M., Orr N., Millett C., Rissel C. Driving to work and overweight and obesity: Findings from the 2003 New South Wales Health Survey, Australia. Int. J. Obes. (Lond.) 2006;30:782–786. doi: 10.1038/sj.ijo.0803199. [DOI] [PubMed] [Google Scholar]
- 5.Warren T.Y., Barry V., Hooker S.P., Sui X., Church T.S., Blair S.N. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med. Sci. Sports Exerc. 2010;42:879–885. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mutrie N., Carney C., Blamey A., Crawford F., Aitchison T., Whitelaw A. “Walk in to Work Out”: A randomised controlled trial of a self help intervention to promote active commuting. J. Epidemiol. Community Health. 2002;56:407–412. doi: 10.1136/jech.56.6.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saunders L.E., Green J.M., Petticrew M.P., Steinbach R., Roberts H. What are the health benefits of active travel? A systematic review of trials and cohort studies. PLoS ONE. 2013;8:e69912. doi: 10.1371/journal.pone.0069912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collia D.V., Sharp J., Giesbrecht L. The 2001 National Household Travel Survey: A look into the travel patterns of older Americans. J. Saf. Res. 2003;34:461–470. doi: 10.1016/j.jsr.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Cabinet Office . Results of Survey on the Senior Citizens’ Lifestyle. Cabinet Office; Tokyo, Japan: 2015. [Google Scholar]
- 10.Choi M., Lohman M.C., Mezuk B. Trajectories of cognitive decline by driving mobility: Evidence from the Health and Retirement Study. Int. J. Geriatr. Psychiatry. 2014;29:447–453. doi: 10.1002/gps.4024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fonda S.J., Wallace R.B., Herzog A.R. Changes in driving patterns and worsening depressive symptoms among older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2001;56:S343–S351. doi: 10.1093/geronb/56.6.S343. [DOI] [PubMed] [Google Scholar]
- 12.Marottoli R.A., Mendes de Leon C.F., Glass T.A., Williams C.S., Cooney L.M., Jr., Berkman L.F., Tinetti M.E. Driving cessation and increased depressive symptoms: Prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J. Am. Geriatr. Soc. 1997;45:202–206. doi: 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 13.Ragland D.R., Satariano W.A., MacLeod K.E. Driving cessation and increased depressive symptoms. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60:399–403. doi: 10.1093/gerona/60.3.399. [DOI] [PubMed] [Google Scholar]
- 14.Edwards J.D., Lunsman M., Perkins M., Rebok G.W., Roth D.L. Driving cessation and health trajectories in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009;64:1290–1295. doi: 10.1093/gerona/glp114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frank L., Kerr J., Rosenberg D., King A. Healthy aging and where you live: Community design relationships with physical activity and body weight in older Americans. J. Phys. Act. Health. 2010;7(Suppl. 1):S82–S90. doi: 10.1123/jpah.7.s1.s82. [DOI] [PubMed] [Google Scholar]
- 16.Ding D., Sallis J.F., Norman G.J., Frank L.D., Saelens B.E., Kerr J., Conway T.L., Cain K., Hovell M.F., Hofstetter C.R., et al. Neighborhood environment and physical activity among older adults: Do the relationships differ by driving status? J. Aging Phys. Act. 2014;22:421–431. doi: 10.1123/JAPA.2012-0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Amagasa S., Fukushima N., Kikuchi H., Takamiya T., Oka K., Inoue S. Light and sporadic physical activity overlooked by current guidelines makes older women more active than older men. Int. J. Behav. Nutr. Phys. Act. 2017;14:59. doi: 10.1186/s12966-017-0519-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawkesworth S., Silverwood R.J., Armstrong B., Pliakas T., Nanchalal K., Jefferis B.J., Sartini C., Amuzu A.A., Wannamethee S.G., Ramsay S.E., et al. Investigating associations between the built environment and physical activity among older people in 20 UK towns. J. Epidemiol. Community Health. 2018;72:121–131. doi: 10.1136/jech-2017-209440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkemeyer K., Wijndaele K., White T., Cooper A.J., Luben R., Westgate K., Griffin S.J., Khaw K.T., Wareham N.J., Brage S. The descriptive epidemiology of accelerometer-measured physical activity in older adults. Int. J. Behav. Nutr. Phys. Act. 2016;13:2. doi: 10.1186/s12966-015-0316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jefferis B.J., Parsons T.J., Sartini C., Ash S., Lennon L.T., Papacosta O., Morris R.W., Wannamethee S.G., Lee I.M., Whincup P.H. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: Does volume of activity matter more than pattern of accumulation? Br. J. Sports Med. 2018 doi: 10.1136/bjsports-2017-098733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dohrn I.M., Kwak L., Oja P., Sjostrom M., Hagstromer M. Replacing sedentary time with physical activity: A 15-year follow-up of mortality in a national cohort. Clin. Epidemiol. 2018;10:179–186. doi: 10.2147/CLEP.S151613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmid D., Ricci C., Baumeister S.E., Leitzmann M.F. Replacing Sedentary Time with Physical Activity in Relation to Mortality. Med. Sci. Sports Exerc. 2016;48:1312–1319. doi: 10.1249/MSS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 23.Del Pozo-Cruz J., García-Hermoso A., Alfonso-Rosa R.M., Álvarez-Barbosa F., Owen N., Chastin S., Pozo-Cruz B. Replacing Sedentary Time: Meta-Analysis of Objective-Assessment Studies. Am. J. Prev. Med. 2018 doi: 10.1016/j.amepre.2018.04.042. in press. [DOI] [PubMed] [Google Scholar]
- 24.Stubbs B., Chen L.J., Chang C.Y., Sun W.J., Ku P.W. Accelerometer-assessed light physical activity is protective of future cognitive ability: A longitudinal study among community dwelling older adults. Exp. Gerontol. 2017;91:104–109. doi: 10.1016/j.exger.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 25.Jefferis B.J., Parsons T.J., Sartini C., Ash S., Lennon L.T., Wannamethee S.G., Lee I.M., Whincup P.H. Does duration of physical activity bouts matter for adiposity and metabolic syndrome? A cross-sectional study of older British men. Int. J. Behav. Nutr. Phys. Act. 2016;13:36. doi: 10.1186/s12966-016-0361-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Healy G.N., Dunstan D.W., Salmon J., Cerin E., Shaw J.E., Zimmet P.Z., Owen N. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007;30:1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 27.Healy G.N., Wijndaele K., Dunstan D.W., Shaw J.E., Salmon J., Zimmet P.Z., Owen N. Objectively measured sedentary time, physical activity, and metabolic risk: The Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- 28.Inoue S., Ohya Y., Odagiri Y., Takamiya T., Kamada M., Okada S., Oka K., Kitabatake Y., Nakaya T., Sallis J.F., et al. Perceived neighborhood environment and walking for specific purposes among elderly Japanese. J. Epidemiol. 2011;21:481–490. doi: 10.2188/jea.JE20110044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tokuda Y., Okubo T., Ohde S., Jacobs J., Takahashi O., Omata F., Yanai H., Hinohara S., Fukui T. Assessing items on the SF-8 Japanese version for health-related quality of life: A psychometric analysis based on the nominal categories model of item response theory. Value Health. 2009;12:568–573. doi: 10.1111/j.1524-4733.2008.00449.x. [DOI] [PubMed] [Google Scholar]
- 30.Kurita S., Yano S., Ishii K., Shibata A., Sasai H., Nakata Y., Fukushima N., Inoue S., Tanaka S., Sugiyama T., et al. Comparability of activity monitors used in Asian and Western-country studies for assessing free-living sedentary behaviour. PLoS ONE. 2017;12:e0186523. doi: 10.1371/journal.pone.0186523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murakami H., Kawakami R., Nakae S., Nakata Y., Ishikawa-Takata K., Tanaka S., Miyachi M. Accuracy of Wearable Devices for Estimating Total Energy Expenditure: Comparison With Metabolic Chamber and Doubly Labeled Water Method. JAMA Intern. Med. 2016;176:702–703. doi: 10.1001/jamainternmed.2016.0152. [DOI] [PubMed] [Google Scholar]
- 32.Ohkawara K., Oshima Y., Hikihara Y., Ishikawa-Takata K., Tabata I., Tanaka S. Real-time estimation of daily physical activity intensity by a triaxial accelerometer and a gravity-removal classification algorithm. Br. J. Nutr. 2011;105:1681–1691. doi: 10.1017/S0007114510005441. [DOI] [PubMed] [Google Scholar]
- 33.Oshima Y., Kawaguchi K., Tanaka S., Ohkawara K., Hikihara Y., Ishikawa-Takata K., Tabata I. Classifying household and locomotive activities using a triaxial accelerometer. Gait Posture. 2010;31:370–374. doi: 10.1016/j.gaitpost.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 34.Park J., Ishikawa-Takata K., Tanaka S., Bessyo K., Tanaka S., Kimura T. Accuracy of Estimating Step Counts and Intensity Using Accelerometers in Older People With or Without Assistive Devices. J. Aging Phys. Act. 2017;25:41–50. doi: 10.1123/japa.2015-0201. [DOI] [PubMed] [Google Scholar]
- 35.Haskell W.L., Lee I.M., Pate R.R., Powell K.E., Blair S.N., Franklin B.A., Macera C.A., Heath G.W., Thompson P.D., Bauman A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 36.Pate R.R., O’Neill J.R., Lobelo F. The evolving definition of “sedentary“. Exerc. Sport Sci. Rev. 2008;36:173–178. doi: 10.1097/JES.0b013e3181877d1a. [DOI] [PubMed] [Google Scholar]
- 37.Troiano R.P., Berrigan D., Dodd K.W., Masse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 38.Tudor-Locke C., Camhi S.M., Troiano R.P. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003–2006. Prev. Chronic. Dis. 2012;9:E113. doi: 10.5888/pcd9.110332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Judice P.B., Silva A.M., Sardinha L.B. Sedentary Bout Durations Are Associated with Abdominal Obesity in Older Adults. J. Nutr. Health Aging. 2015;19:798–804. doi: 10.1007/s12603-015-0501-4. [DOI] [PubMed] [Google Scholar]
- 40.Peddie M.C., Bone J.L., Rehrer N.J., Skeaff C.M., Gray A.R., Perry T.L. Breaking prolonged sitting reduces postprandial glycemia in healthy, normal-weight adults: A randomized crossover trial. Am. J. Clin. Nutr. 2013;98:358–366. doi: 10.3945/ajcn.112.051763. [DOI] [PubMed] [Google Scholar]
- 41.Thosar S.S., Bielko S.L., Mather K.J., Johnston J.D., Wallace J.P. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med. Sci. Sports Exerc. 2015;47:843–849. doi: 10.1249/MSS.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 42.Marottoli R.A., de Leon C.F.M., Glass T.A., Williams C.S., Cooney L.M., Jr., Berkman L.F. Consequences of driving cessation: decreased out-of-home activity levels. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000;55:S334–S340. doi: 10.1093/geronb/55.6.S334. [DOI] [PubMed] [Google Scholar]
- 43.Kikuchi H., Inoue S., Fukushima N., Takamiya T., Odagiri Y., Ohya Y., Amagasa S., Oka K., Owen N. Social participation among older adults not engaged in full- or part-time work is associated with more physical activity and less sedentary time. Geriatr. Gerontol. Int. 2017 doi: 10.1111/ggi.12995. [DOI] [PubMed] [Google Scholar]
- 44.Legh-Jones H., Moore S. Network social capital, social participation, and physical inactivity in an urban adult population. Soc. Sci. Med. 2012;74:1362–1367. doi: 10.1016/j.socscimed.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 45.Fishman E.I., Steeves J.A., Zipunnikov V., Koster A., Berrigan D., Harris T.A., Murphy R. Association between Objectively Measured Physical Activity and Mortality in NHANES. Med. Sci. Sports Exerc. 2016;48:1303–1311. doi: 10.1249/MSS.0000000000000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Loprinzi P.D., Loenneke J.P., Ahmed H.M., Blaha M.J. Joint effects of objectively-measured sedentary time and physical activity on all-cause mortality. Prev. Med. 2016;90:47–51. doi: 10.1016/j.ypmed.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 47.Lee I.M., Shiroma E.J., Lobelo F., Puska P., Blair S.N., Katzmarzyk P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Glazer N.L., Lyass A., Esliger D.W., Blease S.J., Freedson P.S., Massaro J.M., Murabito J.M., Vasan R.S. Sustained and shorter bouts of physical activity are related to cardiovascular health. Med. Sci. Sports Exerc. 2013;45:109–115. doi: 10.1249/MSS.0b013e31826beae5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ekblom-Bak E., Ekblom O., Bergstrom G., Borjesson M. Isotemporal substitution of sedentary time by physical activity of different intensities and bout lengths, and its associations with metabolic risk. Eur. J. Prev. Cardiol. 2016;23:967–974. doi: 10.1177/2047487315619734. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.