We reported a lack of association of presence, type, number, total volume, or largest diameter of fibroids with increased risk of miscarriage (1). The impetus for our prospective cohort was lack of data relevant to the general population. Prior publications were largely retrospective, clinically based, or small trials of myomectomy in subspecialty care. We sought evidence to inform care of patients like Ms. Doe, a 23-year-old without prior pregnancies who sought a second opinion about surgery for a 2.2-cm fibroid. She was advised it would grow, especially during pregnancy, and could cause problems including difficulty conceiving, miscarriage, and preterm birth.
To improve generalizability we enrolled women from the community across >72 practices in 3 states. A latent objective was to define which fibroid characteristics were strongly associated with miscarriage to lay the groundwork for a trial of myomectomy. We were surprised by the null findings and offer these considerations:
Fibroid classifications provide operational definitions and aid in aggregating data (2). The International Federation of Gynecology and Obstetrics classification system was designed to address abnormal uterine bleeding and was not derived from statistically relating fibroid characteristics to pregnancy outcomes. Literature about that relationship is sparse, and references were not provided to substantiate that claim by Nezhat et al. (3).
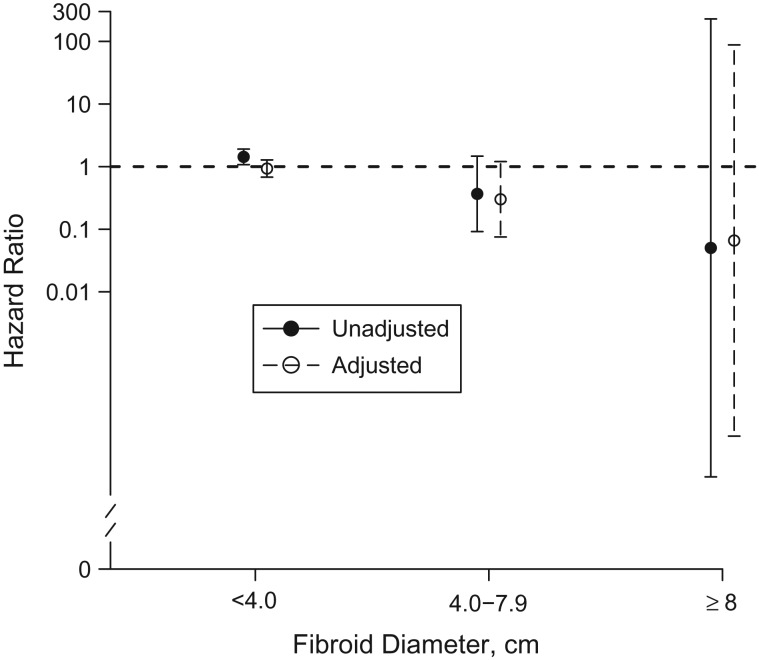
Our analyses (1, Table 2) do not reveal a dose-response pattern for largest diameter, total volume, or number of fibroids in relation to miscarriage. Most women with a fibroid of ≥8 cm diameter had a submucous component. Figure 1 restricts analysis to 403 women with 1 fibroid (79% of those with fibroids), to eliminate consideration of tumor number, and provides hazard ratios according to the sizes discussed in the letter. Joint effects of size and type of fibroid are also null and imprecise (not shown).
Clinical perception of a link between fibroids and miscarriage likely derives from failure to account for age and race. Advancing age increases miscarriage risk independent of fibroids status (1), and black women have greater fibroid prevalence and higher miscarriage risk than white women (4). Adjusting for these confounders reveals that fibroids are a correlate but not a candidate cause of miscarriage. Unadjusted associations for intramural and submucosal fibroids suggest increased hazard, but both are null with adjustment. Why was this not apparent in prior literature? In a recent review and meta-analysis of studies with women of typical reproductive potential, only one study constructed multivariable models to assess/adjust for confounding (5). That exception showed no association (6), while studies without analyses for confounding all reported elevated risk (risk ratios = 1.47–2.20) (5).
Clinical trials align with our findings. A Cochrane review of randomized trials of myomectomy to improve pregnancy outcomes identified 3 studies (7). The trials enrolled women in subspecialty care with fibroids from 3–10 cm, >4 cm, or >5 cm. Myomectomy did not diminish the risk of miscarriage.
Figure 1.
Hazard ratios for miscarriage grouped by research ultrasound determination of maximum fibroid diameter among women with a single fibroid in the first trimester, Southern United States, 2000–2012. Model adjusted for maternal age, race/ethnicity, parity, prior termination of pregnancy history, and alcohol use. The reference group was women without fibroids. Upper confidence interval bounds for women with fibroids of ≥8 cm are truncated.
We agree with the American Society for Reproductive Medicine, whose guidance on removal of myomas in asymptomatic women concludes that evidence is insufficient to support the propositions that (8, pp. 419–422):
“…specific myoma size, number or location…is associated with an increased risk of early pregnancy loss.” (Evidence grade C = insufficient)
“…myomectomy reduces miscarriage rates.” (Evidence grade C = insufficient)
“…hysteroscopic myomectomy reduces likelihood of early pregnancy loss in women with infertility and submucous fibroids.” (Evidence grade C = insufficient)
We concur that our study does not address the circumstances of women with infertility or recurrent loss. We agree that our analysis is not able to dissect nuanced interactions of multiple factors such as exact position and size. However, we affirm that principles of informed medical decision-making warrant that women without an adverse reproductive history can be reassured of the overall high probability of a successful pregnancy without intervention. Given lack of evidence, careful scrutiny of myomectomy use remains warranted.
Acknowledgments
This work was funded by the National Institutes of Health (grants R01HD043883 and R01HD049675) and the American Water Works Association Research Foundation (grant 2579). Salary support for D.R.V.E. was provided in part by the National Institutes of Health Building Interdisciplinary Research Careers in Women’s Health career development program (grant K12HD04383); stipend support was provided in part by the National Institute of General Medical Studies for the Vanderbilt Medical-Scientist Training Program (grant T32GM07347). Additional infrastructure resources were provided by the National Institutes of Health National Center for Advancing Translational Sciences (grant UL1TR000445, a Clinical and Translational Science Award).
Conflict of interest: none declared.
References
- 1. Hartmann KE, Velez Edwards DR, Savitz DA, et al. . Prospective cohort study of uterine fibroids and miscarriage risk. Am J Epidemiol. 2017;186(10):1140–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Munro MG, Critchley HO, Fraser IS. The FIGO systems for nomenclature and classification of causes of abnormal uterine bleeding in the reproductive years: who needs them? Am J Obstet Gynecol. 2012;207(4):259–265. [DOI] [PubMed] [Google Scholar]
- 3. Nezhat CH, Pfeifer S, Bhagavath B, et al. . Re: “Prospective cohort study of uterine fibroids and miscarriage risk” [letter]. Am J Epidemiol. 2018;187(5):1133–1134. [DOI] [PubMed] [Google Scholar]
- 4. Mukherjee S, Velez Edwards DR, Baird DD, et al. . Risk of miscarriage among black women and white women in a US Prospective Cohort Study. Am J Epidemiol. 2013;177(11):1271–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sundermann AC, Velez Edwards DR, Bray MJ, et al. . Leiomyomas in pregnancy and spontaneous abortion: a systematic review and meta-analysis. Obstet Gynecol. 2017;130(5):1065–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benson CB, Chow JS, Chang-Lee W, et al. . Outcome of pregnancies in women with uterine leiomyomas identified by sonography in the first trimester. J Clin Ultrasound. 2001;29(5):261–264. [DOI] [PubMed] [Google Scholar]
- 7. Metwally M, Cheong YC, Horne AW. Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev. 2012;11:Cd003857. [DOI] [PubMed] [Google Scholar]
- 8. Practice Committee of the American Society for Reproductive Medicine; Practice Committee of the American Society for Reproductive Medicine Removal of myomas in asymptomatic patients to improve fertility and/or reduce miscarriage rate: a guideline. Fertil Steril. 2017;108(3):416–425. [DOI] [PubMed] [Google Scholar]